Abstract
A role for the Notch signalling pathway in the formation of arteriovenous malformations during development has been suggested. However, whether Notch signalling is involved in brain arteriovenous malformations in humans remains unclear. Here, we performed immunohistochemistry on surgically resected brain arteriovenous malformations and found that, compared with control brain vascular tissue, Notch-1 signalling was activated in smooth muscle and endothelial cells of the lesional tissue. Western blotting showed an activated form of Notch-1 in brain arteriovenous malformations, irrespective of clinical presentation and with or without preoperative embolization, but not in normal cerebral vessels from controls. In addition, the Notch-1 ligands Jagged-1 and Delta-like-4 and the downstream Notch-1 target Hes-1 were increased in abundance and activated in human brain arteriovenous malformations. Finally, increased angiogenesis was found in adult rats treated with a Notch-1 activator. Our findings suggest that activation of Notch-1 signalling is a phenotypic feature of brain arteriovenous malformations, and that activation of Notch-1 in normal vasculature induces a pro-angiogenic state, which may contribute to the development of vascular malformations.
Keywords: Notch-1, AVM, human, brain, signalling, angiogenesis
Introduction
Brain arteriovenous malformations (AVMs) are abnormal vascular structures consisting of tortuous arteries and dilated veins, which arise from developmental failure of the intervening capillary beds, and are thought in most cases to be congenital. AVMs are distinct from other vascular malformations of the brain, including venous angiomas and cavernous haemangiomas. AVMs may be asymptomatic, or may cause intracerebral haemorrhage, seizures, headache or focal neurological deficits. The molecular mechanisms that underlie the formation and growth of brain AVMs are poorly understood.
Notch signalling, a fundamental pathway controlling cell fate acquisition in development (Artavanis-Tsakonas et al., 1999), plays a critical role during vascular development in zebrafish, mice and humans (Gridley, 2007). Mutations in Notch-3 or Jagged-1, a Notch ligand, lead to human cardiovascular disease: cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy, and Alagille syndrome (paucity of intrahepatic bile ducts with cholestasis, cardiac disease, skeletal abnormalities, ocular abnormalities and characteristic facies), respectively (Joutel et al., 1996).
A role for Notch signalling in the development of vascular malformations has been suggested based on abnormalities that result from Notch pathway mutations (Weinmaster and Kopan, 2006; Gridley, 2007). For example, Notch signalling-deficient zebrafish embryos lose expression of markers such as Ephrin B2 from arteries, where Eph B4, an Ephrin B2 receptor normally associated with veins, is ectopically expressed (Lawson et al., 2001). Changes in the arteriovenous gene expression profile of these animals are accompanied by arteriovenous shunts, a hallmark of AVMs, between the dorsal aorta and posterior cardinal vein (Lawson et al., 2001). Similar findings are observed in Notch-1–/– mouse embryos (Krebs et al., 2004). Although the survival of Notch-4-deficient mice shows that Notch-4 is dispensable for vascular development (Krebs et al., 2000), expression of an activated form of Notch-4 within the endothelium disrupts normal vascular development (Uyttendaele et al., 2001; Carlson et al., 2005). Interestingly, the inducible expression of an activated Notch-4 transgene in adult mice causes vascular malformations in an apparently tissue-specific fashion, along with vessel arterialization, ectopic venous expression of Ephrin B2 and increased numbers of vascular smooth muscle cells (Carlson et al., 2005). Mice with constitutively active Notch-4 in endothelial cells develop cerebral arteriovenous shunting and vessel enlargement by 3 weeks of age (Murphy et al., 2008). Surprisingly, these malformations are reversible if Notch-4 transgene expression is repressed (Carlson et al., 2005), suggesting that the involvement of Notch signalling in the development of dysplastic vasculature can extend to the post-natal period.
Although Notch signalling plays a critical role in arteriovenous cell fate determination during vascular development and is implicated in vascular malformations, its function in normal adult vascular physiology and in the pathogenesis of AVMs in humans has not been established. In this study, we found that Notch-1 signalling was activated in smooth muscle and endothelial cells of human brain AVMs. The Notch-1 ligands Jagged-1 and Delta-like 4, and the downstream Notch-1 target Hes-1, also showed increased abundance and activation in brain AVMs. Moreover, angiogenesis was increased in adult rats given a Notch-1 activator. Our findings suggest that activation of Notch-1 signalling is a phenotypic feature of brain AVMs, and that activation of Notch-1 in normal vasculature induces a pro-angiogenic state, which may contribute to the development of vascular malformations.
Material and methods
Human brain specimens
Thirteen brain specimens from patients with brain AVMs were obtained from the University of California, San Francisco Brain AVM Study Project and the First Affiliated Hospital, Wenzhou Medical College by surgical resection between 2005 and 2007. The patients ranged in age from 10 to 67 years with a mean of 40.6 years (median 40). Patient information is summarized in Table 1. Before surgery, three patients underwent embolization treatment. None underwent preoperative radiation therapy. Four normal human brain specimens without clinical or post-mortem evidence of neurological disease were obtained from the Brain and Tissue Bank for Developmental Disorders of the National Institute of Child and Health and Human Development (University of Maryland, Baltimore, MD, USA). All studies involving patients were conducted under protocols approved by the Institutional Research Review Board at Marin General Hospital, the University of California at San Francisco, and Wenzhou Medical College, China.
Table 1.
Summary of clinical data on patients with brain AVMs
| Case no. | Age (year) | Sex | Initial sign | Embolization | Cerebral AVM |
|
|---|---|---|---|---|---|---|
| Location | Diameter (cm) | |||||
| 1 | 24 | M | Haemorrhage | Yes | L O | 4.53 |
| 2 | 21 | M | Haemorrhage | Yes | NA | NA |
| 3 | 50 | F | Haemorrhage | Yes | L F | 2.84 |
| 4 | 44 | F | Headache | No | R P | 3.50 |
| 5 | 36 | F | Other | No | R F | 2.86 |
| 6 | 30 | M | Epilepsy | No | R P/O | 3.50 |
| 7 | 36 | M | Epilepsy | No | L T | 2.66 |
| 8 | 10 | M | Headache | No | L T | 1.50 |
| 9 | 56 | M | Haemorrhage | No | L F/T | 2.00 |
| 10 | 67 | M | Headache | No | L T | 4.00 |
| 11 | 66 | F | Haemorrhage | No | L T | 1.50 |
| 12 | 39 | M | Headache | No | R F | 2.00 |
| 13 | 50 | M | Haemorrhage | No | R P/T | 3.62 |
R = right; L = left; F = frontal; T = temporal; P = parietal; O = occipital; NA = not available.
Immunohistochemistry
Human and rat brain specimens were embedded in paraffin and cut in 6 µm sections, which were de-paraffinized with xylene and rehydrated with ethanol, following antigen retrieval with antigen unmasking solution (Vector Laboratories) according to the manufacturer's instructions. Endogenous peroxidase activity was blocked by incubation in 1% H2O2 at room temperature for 30 min. After several washes with phosphate buffered saline (PBS), sections were incubated in blocking solution for 1 h at room temperature. Primary antibodies used were (i) goat or rabbit polyclonal anti-Notch-1 (Santa Cruz Biotechnology, 1:100), (ii) rabbit polyclonal anti-NICD (intracellular domain of Notch; Abcam, 1:500), (iii) goat polyclonal anti-Jagged-1 (Santa Cruz Biotechnology, 1:100), (iv) rabbit polyclonal anti-Hes-1 (Chemicon, 1:500), (v) mouse monoclonal anti-Delta-like-4 (Dll4; R&D, 1:200), (vi) mouse monoclonal anti-BrdU (bromodeoxyuridine; Roche, 2 µg/ml), (vii) rabbit polyclonal anti-extracellular domain of Dll4 (Ab7280; Abcam, 1:500) and (vii) rabbit anti-smooth muscle α-actin (αSMC; Maine Biotechnology Service, 1:300). Primary antibodies were added in blocking buffer and incubated with sections at 4°C overnight. Sections were then washed with PBS and incubated with biotinylated goat anti-rabbit or anti-goat antibody (1:200, for polyclonal antibodies) or biotinylated horse anti-mouse antibody (1:200, for monoclonal antibodies) for 1 h at room temperature. Avidin–biotin complex (Vector Elite; Vector Laboratories) and a diaminobenzidine or nickel solution (Vector Laboratories) were used to obtain a visible reaction product. Controls for immunohistochemistry included pre-incubation of the antibodies with the corresponding antigens. The slide examiners were blinded to the source of the specimen (brain AVMs versus control). H9 human embryonic stem cells (H9, WiCell) and mouse brain tissue (E17) were used for additional controls. H9 cells were maintained on mouse embryonic feeder cells in proliferation medium consisting of Knockout Dulbecco's modified Eagle's medium (DMEM; Invitrogen) supplemented with 20% Knockout serum replacement (Invitrogen), pyruvate, glutamine, β-mercaptoethanol and human basic fibroblast growth factor. A Nikon microscope and a Nikon digital colour camera were used for examination and photography of the slides, respectively.
Double immunostaining
Double immunostaining was performed on brain sections as described previously (Jin et al., 2003). The primary antibodies used, in addition to those listed above, included mouse anti-CD31 (PECAM1; Dakocytomation, Denmark, 1:100). Fluorescein isothiocyanate (FITC)-labelled Lycopersicon esculentum (tomato) lectin (Vector, 1:300) was also used for vessel staining. The secondary antibodies were Alexa Fluor 488-, 594- or 647-conjugated donkey anti-mouse, anti-goat or anti-rabbit IgG (Molecular Probes, 1:200–500). Slides were mounted using proLong Gold antifade reagent with 4',6-diamidino-2-phenylindole (DAPI; Molecular Probes). Fluorescence signals were detected using a laser scanning microscope-510 non-linear optic confocal Scanning System mounted on an Axiovert 200 inverted microscope equipped with a two-photon Chameleon laser. Selected images were viewed at high magnification, and 3D images were constructed using IMARIS software. Controls included omitting either the primary or secondary antibody or pre-absorbing the primary antibody.
Western blotting
Tissues were dissected from frozen brains. Protein was isolated and western blotting was performed as previously described (Jin et al., 2003). The primary antibodies were: (1) anti-activated form of Notch-1 (NICD; Abcam, 1:500), (2) rat anti-Dll4 (R&D Systems, 1:500), (3) rabbit anti-Hes-1 (Chemicon, 1:1000), (4) rabbit polyclonal anti-Jagged-1 (Santa Cruz Biotechnology, 1:250) and (5) mouse monoclonal anti-actin (Oncogene Science, 1:20,000). Membranes were washed with PBS/0.1% Tween 20, incubated at room temperature for 60 min with horseradish peroxidase-conjugated anti-mouse, anti-rabbit or anti-goat secondary antibody (Santa Cruz Biotechnology; 1:3,000), and washed three times for 15 min. Peroxidase activity was visualized by chemiluminescence. Antibodies were removed with stripping buffer at 50°C for 30 min, followed by washing with PBS/Tween 20, and membranes were reprobed. Recombinant human Notch-1/Fc chimera, recombinant human Jagged-1/Fc chimera, recombinant human Dll4 and Hes-1 protein (all from R&D System) were used as positive controls. NICD antibody was mixed with activated Notch-1 peptide (Abcam) at 1:5 and pre-incubated for at 37°C 1 h prior to western blotting.
Administration of Notch signalling activator and inhibitor
Animal experiments were conducted according to National Institutes of Health guidelines after approval by the Buck Institute's Institutional Animal Care and Use Committee. Male Sprague-Dawley rats (2 to 3 months old) were anaesthetized with 4% isoflurane in 70% N2O/30% O2 and implanted with an osmotic minipump (Alzet 1003D; Alza Corporation). The cannula was placed in the right lateral ventricle 4.0 mm deep to the pial surface, +0.8 mm anteroposterior relative to bregma, and 1.3 mm lateral to the midline. Each rat was continuously infused for either 7 days or 28 days with 0.5 μl/h of either anti-Notch-1 antibody (hybridoma clone 8G10, Upstate Biotechnology) in artificial cerebrospinal fluid, Jagged-Fc/anti-Fc complex (2:1), anti-Fc antibody alone or artificial cerebrospinal fluid alone (n = 5–6 per group). Rats were killed on day 8 or 29 and brains were sectioned. Immunohistochemistry and double-label immunostaining were performed as described above.
Bromodeoxyuridine administration
BrdU (50 mg/kg) was dissolved in saline and given intraperitoneally, twice daily at 8 h intervals for 3 days, and rats were killed on day 8 or 29. To detect BrdU-labelled cells, brain sections were incubated in methanol at –20°C for 10 min and in 2 M HCl at 37°C for 50 min and rinsed in 0.1 M boric acid (pH 8.5). Immunohistochemistry and double-label immunostaining were otherwise performed as described earlier.
Quantification of blood vessel density
To quantify blood vessel density after administration of Notch-1 signalling activator or inhibitor, images of coronal brain sections on the cannula side (1 mm anterior and 1 mm posterior to the needle track) were acquired using a Nikon Eclipse-800 microscope and Nikon digital camera DXM1200. Three rectangular fields of interest in the cortex were randomly selected at 20× magnification. The intensity and total number of FITC-conjugated lectin-positive microvessels were measured using IMARIS 4.2 software (Bitplane AG Scientific Solutions, Zurich, Switzerland). Values were averaged and expressed as the mean percentage of stained vessel area per 100 μm2. The number of blood vessels was also counted manually in a blinded fashion.
Statistical analysis
Quantitative results were expressed as the mean ± SEM. The statistical significance of differences between means was evaluated using one-way analysis of variance (ANOVA) followed by a Bonferroni post hoc test. Statistical analyses were performed using GraphPad Prism 5.0 software for Windows (GraphPad, San Diego, CA, USA). Values of P < 0.05 were regarded as statistically significant.
Results
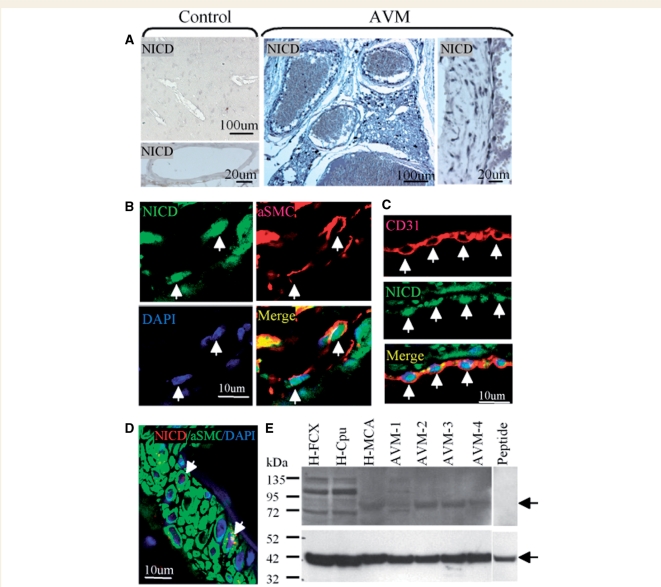
To assess the role of Notch-1 signalling in human brain AVMs, immunostaining was first performed using antibodies against Notch-1 as well as the activated form of Notch-1, the intracellular domain of Notch (NICD). Both Notch-1 and NICD were weakly expressed in vessels of normal human brain, but NICD was highly expressed in the nuclei of AVM vessel walls, suggesting activation of Notch-1 signalling (Fig. 1A). To determine the phenotype of NICD-expressing cells, double immunostaining was performed using anti-αSMA to label smooth muscle cells and anti-CD31 for endothelial cells. NICD was expressed in both smooth muscle and endothelial cells of AVMs (Fig. 1B and C). Normal human middle cerebral artery, which was comparable in caliber to AVM vessels, was used as an additional control. NICD was weakly expressed in smooth muscle cells of normal human middle cerebral artery (Fig. 1D). To confirm and extend these immunohistochemical studies, western blot analysis was performed. As shown in Fig. 1E, anti-NICD labelled a band of the predicted size (∼80 kDa), which could be abolished with an excess of immunizing peptide. This band was detected in all patients with brain AVM, irrespective of clinical presentation or embolization treatment, but not in normal human frontal cortex. The intensity of the NICD band varied across patients, which might reflect different stages of pathogenesis, different amounts of AVM in the brain samples studied or both.
Figure 1.
Activation of Notch-1 signalling in human brain AVMs. (A) NICD was barely detectable in normal human cerebral vessels (Control), but was highly expressed in cell nuclei of AVMs. (B) Double immunostaining of human brain AVM shows nuclear NICD (green) and cytoplasmic SMC (red) in the same (vascular smooth muscle) cells (arrows). DAPI (blue) was used to counterstain nuclei. (C) Double immunostaining of human brain AVM shows nuclear NICD (green) and cytoplasmic CD31 (red) in the same (endothelial) cells (arrows). DAPI (blue) was used to counterstain nuclei. (D) Double immunostaining of normal human middle cerebral artery shows abundant cytoplasmic SMC (green) but little nuclear NICD (red). DAPI (blue) was used to counterstain nuclei. (E) Protein was isolated from normal human frontal cortex (H-FCX), caudate-putamen (H-Cpu) and middle cerebral artery (H-MCA) and from four human AVMs (AVM 1–4). Western blotting was performed using an antibody against NICD (top panel). A band of the predicted size (arrow) was blocked after pre-incubating anti-NICD with an excess of immunizing peptide (Peptide). The membrane was re-probed with anti-actin as an internal protein loading control (bottom panel, arrow).
Next, we examined the expression of other components of the Notch-1 signalling pathway in brain AVMs. The Notch-1 ligand Jagged-1 was expressed in AVMs as well as in normal controls, whereas the ligand Dll4 was detected only in AVMs (Fig. 2A). Hes-1, a downstream target of Notch-1, was predominantly expressed in nuclei of both endothelial and smooth muscle cells in AVMs, but not normal vessels, although Hes-1 was expressed in some non-vascular cells in normal adult brain (Fig. 2A). To validate the antibodies used, immunostaining was performed on mouse embryonic tissues. We found that Notch-1, Jagged-1, Dll4, NICD and Hes-1 were expressed or activated in blood vascular cells of E17 mouse brain (Fig. 2B). In addition, immunostaining was also performed on positive control (H9 human embryonic stem) cells, which express Notch-1 signalling proteins including Notch-1, Jagged-1, Hes-1 and Dll4 (Yu et al., 2008). These proteins were expressed in H9 (Fig. 2C), but barely detected in mouse feeder cells (fibroblasts) (Fig. 2C).
Figure 2.
Immunohistochemical detection of Notch-1 ligands and Hes-1 in human brain AVMs. (A) Dll4, Jagged-1 and Hes-1 expression (black) was increased in human brain AVMs (left panels, low-magnification; middle panels, high-magnification) compared with normal human middle cerebral artery (right panels). A few non-vascular cells in normal control brain also expressed Hes-1 (arrow). (B) Notch1, Jagged-1, Dll4, NICD and Hes-1 were expressed or activated in vascular cells of E17 mouse brain. (C) Immunostaining was performed on H9 human embryonic stem cells using (left to right) anti-Jagged-1 (green) and anti-NICD (red); anti-Notch-1 (green); anti-Dll4 (green) and anti-Hes1 (green). DAPI (blue) was used to counterstain nuclei.
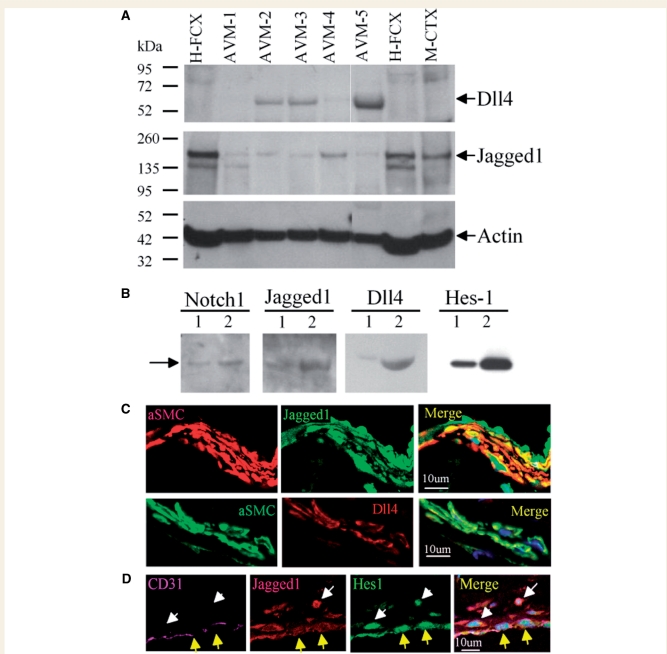
In agreement with data obtained by immunohistochemistry, western blotting showed a band corresponding to Jagged-1 in both controls and AVMs, whereas Dll4 was expressed only in AVMs (Fig. 3A). In contrast to our immunohistochemical results, Jagged-1 protein expression on western blots was greater in normal brain than in AVMs, which could be due to Jagged-1 expression in neural cells. To determine the specificity of the primary antibodies, recombinant human Notch-1, Jagged-1, Dll4 and Hes-1 were resolved by sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS–PAGE) and western blotting was performed using the corresponding antibodies. As shown in Fig. 3B, protein bands were detected in AVMs at the predicted sizes. The cell types that expressed Jagged-1 and Dll4 in human brain AVMs were determined by double-label immunostaining. Both Jagged-1 and Dll4 were expressed in smooth muscle cells (Fig. 3C) and Hes-1 was expressed predominantly in nuclei of endothelial cells (Fig. 3D).
Figure 3.
Western blot analysis and cell-type localization of Notch-1 ligands in human brain AVMs. (A) Protein was isolated from the sources listed in the legend to Figure 1, and from normal mouse cerebral cortex (M-CTX). Western blotting was performed using antibodies against the Notch-1 ligands Dll4 (top panel) and Jagged-1 (middle panel), with anti-actin to control for differences in protein loading (bottom panel). (B) Recombinant human Notch-1, Jagged-1, Dll4 and Hes1 were loaded on gels and probed with the indicated antibodies, showing that the antibodies used recognize authentic antigens. Each pair of gel lanes was loaded with 100 ng (lane 1) or 500 ng (lane 2) of total protein. (C) Double-label immunostaining of human brain AVM sections shows that αSMC-expressing vascular smooth muscle cells also express Jagged-1 (top panel) and Dll4 (bottom panel). DAPI (blue) was used to counterstain nuclei. (D) Triple-label immunostaining of human brain AVM shows co-expression of Jagged-1 (red) and Hes1 (green) in CD31-immunopositive (purple) endothelial cells. DAPI (blue) was used to counterstain nuclei.
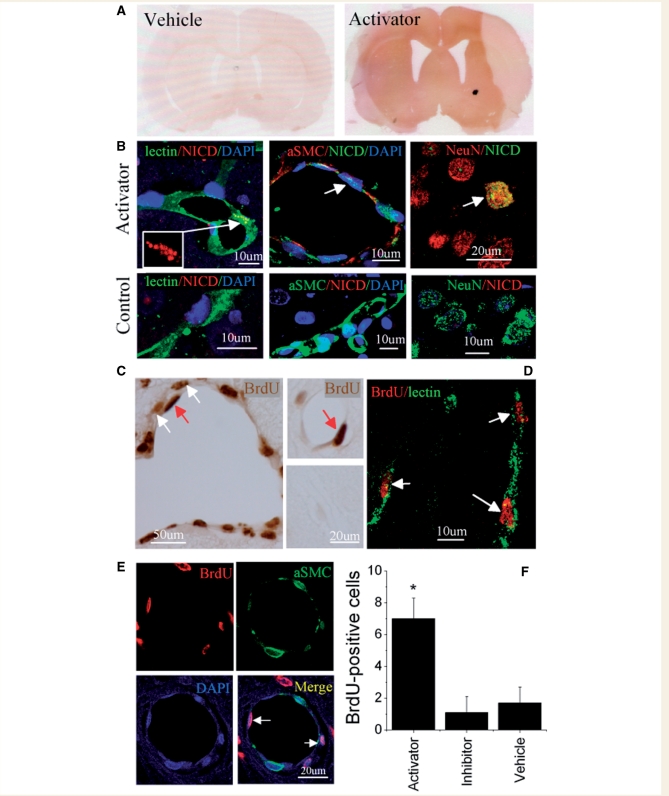
To investigate further whether Notch-1 signalling might mediate vascular proliferation in brain vascular malformations, we used a Notch-1-specific antibody to activate Notch-1 signalling and a soluble Jagged-1-Fc fusion protein (Hicks et al., 2002) to inhibit Notch-1 signalling (Conboy et al., 2003) in rats in vivo. Immunostaining with a hamster anti-mouse isotypic antibody showed that the Notch-1-activating mouse antibody entered the brain parenchyma (Fig. 4A). Double immunostaining for NICD and cell type-specific markers confirmed that Notch-1 signalling was activated in endothelial cells and smooth muscle cells after infusion of Notch-1-activating antibody, but not in the control group (Fig. 4B). As shown in Fig. 4C, BrdU-positive cells were detected in the walls of cerebral blood vessels after administration of Notch-1 activator for 7 days. Double immunostaining indicated that these BrdU-positive cells included endothelial (Fig. 4D) and smooth muscle (Fig. 4E) cells. The number of BrdU-positive cells in the cerebral vasculature was increased after activation of Notch-1 signalling (Fig. 4F). BrdU labelling was not reduced significantly below baseline by the Notch inhibitor, but this may be because baseline labelling was already so low.
Figure 4.
Effects of Notch-1 signalling activation in vivo on cerebral vessels of rat brain. (A) Vehicle (left panel) or Notch-1 activator (right panel) was infused into the lateral ventricle of adult rat brain for 7 days. BrdU was given by intraperitoneal injection for the first 3 days, and rats were killed on day 8. Notch-1-activating mouse antibody entered the brain parenchyma (right panel), as evidenced by immunostaining with a hamster anti-mouse isotypic antibody (brown). (B) Double-label immunostaining shows expression of activated Notch-1 (NICD) in lectin-labelled endothelial cells (left), αSMC-immunopositive vascular smooth muscle cells (middle) and neuron-specific nuclear protein (NeuN)-expressing neurons of Notch-1 activator-treated brain AVM (top panel) but not in vehicle-treated control brain (bottom panel). Insert in top left panel shows NICD immunoreactivity at higher magnification. DAPI (blue) was used to counterstain nuclei. (C) BrdU-positive cells were found in cerebrovascular endothelial (red arrows) and smooth muscle (white arrows) cells of Notch-1 activator-treated (right and middle top panels), but not control (middle lower panel) rat brains. (D) Double-label staining of sections from rat brain after administration of Notch-1 activator shows BrdU-immunopositive nuclei in lectin-labelled (vascular endothelial) cells. (E) Double-label immunostaining of rat brain vessels after administration of Notch-1 activator also shows BrdU-positive nuclei (red) in αSMC-expressing (green) smooth muscle cells. DAPI (blue) was used to counterstain nuclei. (F) The number of BrdU-positive cells per 400× field in rat cortex was increased by administration of Notch-1 activator, compared with Notch-1 inhibitor or vehicle. Asterisk indicates P < 0.05 relative to vehicle treatment (ANOVA and Bonferroni post hoc tests).
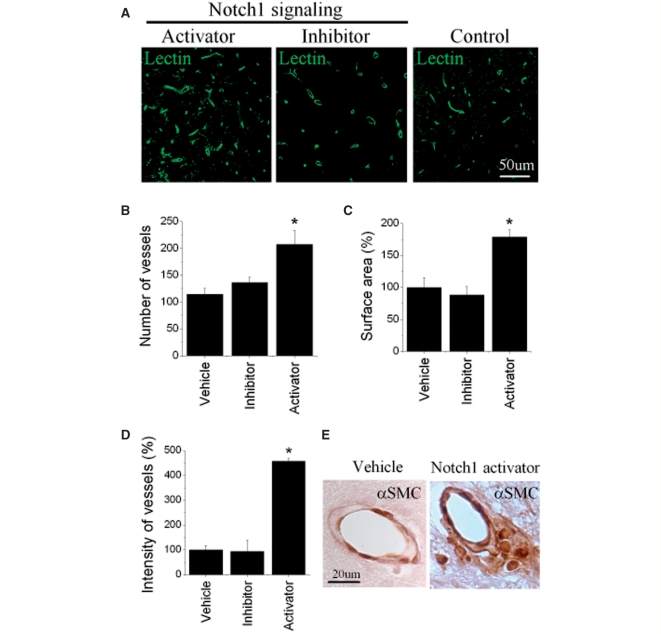
We also used FITC-labelled L. esculentum (tomato) lectin to label vessels in rat cerebral cortex for quantitation. Notch-1 activator treatment increased the number, area and intensity of vascular labelling, as well as the thickness of vessel walls (Fig. 5). Again the Notch-1 inhibitor had no effect.
Figure 5.
Effect of Notch-1 activator on rat brain blood vessels. (A) The number of FITC-lectin-positive cerebral cortical blood vessels was increased after 7 days in the Notch-1 activator- (left panel) compared with the Notch-1 inhibitor- (middle panel) and vehicle-treated control (right panel) groups. FITC-lectin-labelled blood vessels were counted manually (B) and the area (C) and intensity (D) of FITC-lectin staining was measured using IMARIS software, in cerebral cortex of rats given a Notch-1 activator, Notch-1 inhibitor or vehicle for 7 days. (E) Notch-1 activator was continuously infused into the lateral ventricle of adult rat brain for 28 days, and rats were killed 1 day later. Immunostaining with anti-αSMC (brown) shows that compared with vehicle-treated controls (left), cerebral vessels from rats given a Notch-1 activator (right) have thicker vessel walls. Asterisks indicate P < 0.05 (ANOVA and Bonferroni post hoc tests) relative to vehicle-treated controls.
Discussion
In this study, we found that NICD, the active form of Notch-1, is present in both endothelial and smooth muscle cells of human brain AVMs, but not in control human cerebral blood vessels. The Notch-1 ligands Jagged-1 and Dll4, and the downstream Notch-1 target (Hes-1), were also increased, suggesting that Notch-1 signalling is activated in human brain AVMs. This observation is consistent with the previously demonstrated role of Notch signalling in the developing circulation (Weinmaster and Kopan, 2006; Gridley, 2007) We also found that continuous intraventricular administration of a Notch-1 activator in normal rats stimulates the proliferation of both endothelial and vascular smooth muscle cells, suggesting that enhanced Notch-1 signalling can independently induce a pro-angiogenic state. However, it remains unclear whether more prolonged administration, or higher doses, of a Notch-1 activator would lead to the formation of arteriovenous shunts or vascular malformations. Our data imply that the enhanced Notch signalling in vascular malformations may have effects not only during development, but also in post-natal brain.
The significance of this work is several-fold. First, although the activation of Notch-1 signalling in surgical specimens cannot address the necessity or sufficiency of this pathway in the aetiology or pathogenesis of brain AVMs, it suggests that this pathway is involved at some stage of the natural history. The functional studies in rats are important in this regard because they establish that, in post-natal brain, there is a pro-angiogenic effect of Notch-1 signalling. Second, even if Notch signalling is not the primary cause of AVM development, its involvement at any stage of disease progression makes it a plausible target for therapy development. Other than surgical extirpation, endovascular embolization and radiotherapy, there is no treatment to prevent bleeding from cerebral AVMs, and each of these modalities carries the risk of disability or death. Approximately 20% of AVM patients cannot be offered these options because of excessive risk (Choi and Mohr, 2005).
The genesis of AVMs has been enigmatic, and we cannot determine from our findings whether Notch-1 signalling is necessary or sufficient for brain AVMs to occur. Brain AVMs may form independently of Notch-1 pathways, and haemodynamic stresses caused by high flow arteriovenous shunting may secondarily activate biomechanical responses that involve Notch-1 activation. Unlike the association of antecedent head trauma or other injuries with the pathogenesis of dural arteriovenous fistulae, overt environmental risk factors for AVMs are unknown. Considering the high utilization of pre-natal ultrasound, there is remarkably little evidence for the common belief that true AVMs—which do not include Vein of Galen lesions—arise during embryonic development. In fact, the mean age at detection is roughly 40 years, with a normal distribution (Kim et al., 2007). Furthermore, there have been multiple reports of AVMs that grow or regress, as well as of local re-growth of AVMs after treatment (Du et al., 2007). The scarce data available on longitudinal assessment of AVM growth after detection suggest that ∼50% of cases display interval growth (Hashimoto et al., 2001), but the relationship of such growth to clinical consequences remains unknown. Since post-natal growth of AVMs occurs, one plausible aim for therapy might be to reduce the rate of growth over time.
The Notch signalling pathway is activated through direct cell–cell interactions that facilitate binding between Notch ligands (Dll1, Dll3, Dll4, Jagged-1 and Jagged-2) on a signalling cell and the Notch receptor on a responding cell (Lai, 2004). Signals exchanged between these cells can amplify and consolidate molecular changes that eventually dictate cell fate. The importance of this signalling pathway is demonstrated by the fact that targeted disruption of Notch ligands in mice results in embryonic lethality with vascular defects (Xue et al., 1999; Gale et al., 2004). The importance of Jagged-1 in human disease is also suggested by its role in Alagille syndrome, a congenital disorder linked to mutations in the Jagged-1 gene (Oda et al., 1997). Additionally, Dll4 has emerged as the critical ligand in Notch signalling-mediated vascular malformations in mice (Gale et al., 2004; Gridley, 2007). Transgenic mice that conditionally overexpress Dll4 exhibit profound abnormalities in the developing vasculature, including fusion of large arteries and veins, enlargement of arteries with excess fibronectin accumulation and decreased vessel branching (Trindade et al., 2008). Similarly, vascular malformations in Notch4-overexpressing transgenic mice are reversible if expression of an activated Notch4 transgene is repressed (Carlson et al., 2005).
Notch signalling in adult endothelium is sufficient to confer arterial characteristics and lead to vascular malformations, since endothelial expression of constitutively active Notch-4 and Notch-1 causes hepatic (Carlson et al., 2005; Murphy et al., 2008) and cerebral (Murphy et al., 2008) vascular malformations. These findings suggest that brain vascular malformations might be treatable with Notch inhibitors. Our data indicate that both Jagged-1 and Dll4 are prominently expressed in the vasculature, and that Dll4 expression is increased in brain AVMs, suggesting that Dll4 may be a major ligand involved in Notch-1 signalling in human brain AVMs. Our finding that continuous intraventricular infusion of a Notch-1 activator in rat brain promotes angiogenesis further suggests such a link.
Upon ligand binding, Notch is proteolytically cleaved by γ-secretase to release NICD, which translocates to the nucleus, where it binds to the transcription factor CSL (Core binding factor-1 in humans, Suppressor of Hairless in Drosophila, LAG in Caenorhabditis elegans) (Kato et al., 1997). The NICD/CSL interaction converts CSL from a transcriptional repressor to a transcriptional activator by displacing the co-repressor complex and recruiting co-activators, which regulate expression of Notch target genes (Artavanis-Tsakonas et al., 1999). The most widely accepted Notch/CSL targets are members of the Hes (Kageyama and Ohtsuka, 1999) and HRT (Nakagawa et al., 1999) gene families. Although there are seven Hes and HRT genes, not all are clear Notch targets. As observed for Notch receptor- or ligand-deficient embryos, embryos deficient in Notch downstream signalling targets also display vascular defects. For example, RBP-Jk-null(−/−) embryos fail to express several artery-specific endothelial cell markers and exhibit vascular defects (Krebs et al., 2004). Both Hey1 and Hey2 knockout mice display a lethal vascular defect and recapitulate most of the known cardiovascular phenotypes of disrupted Notch pathway mutants, including defects in arteriovenous specification, septation and cushion formation (Fischer et al., 2004; Kokubo et al., 2005). Our data show that expression of Hes1 protein is increased in the nucleus of both endothelial and smooth muscle cells of human cerebral AVMs, suggesting that Hes-1 is a downstream target of Notch-1 signalling in this setting. Whether other Notch target genes are activated in human brain AVMs remains to be explored.
Taken together with previous observations, our findings that Notch-1 signalling is activated in human brain AVMs and that Notch-1 signalling may promote abnormal angiogenesis suggest that aberrant Notch-1 signalling may have a role in the pathogenesis of brain AVMs. Further study is essential to determine if this is the case. Another important area for future work will be to examine the overlap between Notch signalling and tumour growth factor (TGF)-β signalling in the context of brain AVMs. Hereditary haemorrhagic telangiectasia (Osler–Rendu–Weber disease), which is associated with AVMs in brain and other solid organs, is most commonly caused by loss-of-function mutations in endoglin or in activin A receptor-like kinase, both of which are involved in TGF-β signalling (Azuma, 2000).
Funding
Wenzhou Medical College (5010 grant, partial); National Institutes of Health grants (AG21980 to K.J., NS027713 to W.L.Y.).
Acknowledgements
Some human tissues were obtained from the NICHD Brain and Tissue Bank for Developmental Disorders at the University of Maryland, Baltimore, MD. The role of the NICHD Brain and Tissue Bank is to distribute tissue and, therefore, it cannot endorse the studies performed or the interpretation of results.
Glossary
Abbreviations
- AVM
arteriovenous malformations
- Dll4
anti-Delta-like-4
- NICD
intracellular domain of Notch
- TGF
tumour growth factor
References
- Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science. 1999;284:770–6. doi: 10.1126/science.284.5415.770. [DOI] [PubMed] [Google Scholar]
- Carlson TR, Yan Y, Wu X, Lam MT, Tang GL, Beverly LJ, et al. Endothelial expression of constitutively active Notch4 elicits reversible arteriovenous malformations in adult mice. Proc Natl Acad Sci USA. 2005;102:9884–9. doi: 10.1073/pnas.0504391102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi JH, Mohr JP. Brain arteriovenous malformations in adults. Lancet Neurol. 2005;4:299–308. doi: 10.1016/S1474-4422(05)70073-9. [DOI] [PubMed] [Google Scholar]
- Conboy IM, Conboy MJ, Smythe GM, Rando TA. Notch-mediated restoration of regenerative potential to aged muscle. Science. 2003;302:1575–7. doi: 10.1126/science.1087573. [DOI] [PubMed] [Google Scholar]
- Du R, Hashimoto T, Tihan T, Young WL, Perry V, Lawton MT. Growth and regression of arteriovenous malformations in a patient with hereditary hemorrhagic telangiectasia. Case report. J Neurosurg. 2007;106:470–7. doi: 10.3171/jns.2007.106.3.470. [DOI] [PubMed] [Google Scholar]
- Fischer A, Schumacher N, Maier M, Sendtner M, Gessler M. The Notch target genes Hey1 and Hey2 are required for embryonic vascular development. Genes Dev. 2004;18:901–11. doi: 10.1101/gad.291004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale NW, Dominguez MG, Noguera I, Pan L, Hughes V, Valenzuela DM, et al. Haploinsufficiency of delta-like 4 ligand results in embryonic lethality due to major defects in arterial and vascular development. Proc Natl Acad Sci USA. 2004;101:15949–54. doi: 10.1073/pnas.0407290101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gridley T. Notch signaling in vascular development and physiology. Development. 2007;134:2709–18. doi: 10.1242/dev.004184. [DOI] [PubMed] [Google Scholar]
- Hashimoto T, Mesa-Tejada R, Quick CM, Bollen AW, Joshi S, Pile-Spellman J, et al. Evidence of increased endothelial cell turnover in brain arteriovenous malformations. Neurosurgery. 2001;49:124–31. doi: 10.1097/00006123-200107000-00019. discussion 131–2. [DOI] [PubMed] [Google Scholar]
- Hicks C, Ladi E, Lindsell C, Hsieh JJ, Hayward SD, Collazo A, et al. A secreted Delta1-Fc fusion protein functions both as an activator and inhibitor of Notch1 signaling. J Neurosci Res. 2002;68:655–67. doi: 10.1002/jnr.10263. [DOI] [PubMed] [Google Scholar]
- Jin K, Sun Y, Xie L, Peel A, Mao XO, Batteur S, et al. Directed migration of neuronal precursors into the ischemic cerebral cortex and striatum. Mol Cell Neurosci. 2003;24:171–89. doi: 10.1016/s1044-7431(03)00159-3. [DOI] [PubMed] [Google Scholar]
- Joutel A, Corpechot C, Ducros A, Vahedi K, Chabriat H, Mouton P, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–10. doi: 10.1038/383707a0. [DOI] [PubMed] [Google Scholar]
- Kageyama R, Ohtsuka T. The Notch-Hes pathway in mammalian neural development. Cell Res. 1999;9:179–88. doi: 10.1038/sj.cr.7290016. [DOI] [PubMed] [Google Scholar]
- Kato H, Taniguchi Y, Kurooka H, Minoguchi S, Sakai T, Nomura-Okazaki S, et al. Involvement of RBP-J in biological functions of mouse Notch1 and its derivatives. Development. 1997;124:4133–41. doi: 10.1242/dev.124.20.4133. [DOI] [PubMed] [Google Scholar]
- Kim H, Sidney S, McCulloch CE, Poon KY, Singh V, Johnston SC, et al. Racial/ethnic differences in longitudinal risk of intracranial hemorrhage in brain arteriovenous malformation patients. Stroke. 2007;38:2430–7. doi: 10.1161/STROKEAHA.107.485573. [DOI] [PubMed] [Google Scholar]
- Kokubo H, Miyagawa-Tomita S, Nakazawa M, Saga Y, Johnson RL. Mouse hesr1 and hesr2 genes are redundantly required to mediate Notch signaling in the developing cardiovascular system. Dev Biol. 2005;278:301–9. doi: 10.1016/j.ydbio.2004.10.025. [DOI] [PubMed] [Google Scholar]
- Krebs LT, Shutter JR, Tanigaki K, Honjo T, Stark KL, Gridley T. Haploinsufficient lethality and formation of arteriovenous malformations in Notch pathway mutants. Genes Dev. 2004;18:2469–73. doi: 10.1101/gad.1239204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs LT, Xue Y, Norton CR, Shutter JR, Maguire M, Sundberg JP, et al. Notch signaling is essential for vascular morphogenesis in mice. Genes Dev. 2000;14:1343–52. [PMC free article] [PubMed] [Google Scholar]
- Lai EC. Notch signaling: control of cell communication and cell fate. Development. 2004;131:965–73. doi: 10.1242/dev.01074. [DOI] [PubMed] [Google Scholar]
- Lawson ND, Scheer N, Pham VN, Kim CH, Chitnis AB, Campos-Ortega JA, et al. Notch signaling is required for arterial-venous differentiation during embryonic vascular development. Development. 2001;128:3675–83. doi: 10.1242/dev.128.19.3675. [DOI] [PubMed] [Google Scholar]
- Murphy PA, Lam MT, Wu X, Kim TN, Vartanian SM, Bollen AW, et al. Endothelial Notch4 signaling induces hallmarks of brain arteriovenous malformations in mice. Proc Natl Acad Sci USA. 2008;105:10901–6. doi: 10.1073/pnas.0802743105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa O, Nakagawa M, Richardson JA, Olson EN, Srivastava D. HRT1, HRT2, and HRT3: a new subclass of bHLH transcription factors marking specific cardiac, somitic, and pharyngeal arch segments. Dev Biol. 1999;216:72–84. doi: 10.1006/dbio.1999.9454. [DOI] [PubMed] [Google Scholar]
- Oda T, Elkahloun AG, Pike BL, Okajima K, Krantz ID, Genin A, et al. Mutations in the human Jagged1 gene are responsible for Alagille syndrome. Nat Genet. 1997;16:235–42. doi: 10.1038/ng0797-235. [DOI] [PubMed] [Google Scholar]
- Trindade A, Kumar SR, Scehnet JS, Lopes-da-Costa L, Becker J, Jiang W, et al. Overexpression of Delta-like 4 induces arterialization and attenuates vessel formation in developing mouse embryos. Blood. 2008 doi: 10.1182/blood-2007-09-112748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uyttendaele H, Ho J, Rossant J, Kitajewski J. Vascular patterning defects associated with expression of activated Notch4 in embryonic endothelium. Proc Natl Acad Sci USA. 2001;98:5643–8. doi: 10.1073/pnas.091584598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinmaster G, Kopan R. A garden of Notch-ly delights. Development. 2006;133:3277–82. doi: 10.1242/dev.02515. [DOI] [PubMed] [Google Scholar]
- Xue Y, Gao X, Lindsell CE, Norton CR, Chang B, Hicks C, et al. Embryonic lethality and vascular defects in mice lacking the Notch ligand Jagged1. Hum Mol Genet. 1999;8:723–30. doi: 10.1093/hmg/8.5.723. [DOI] [PubMed] [Google Scholar]