Duodenocolic fistula (DCF) is a very rare entity characterized by fistulous communication between duodenum and transverse colon; DCF owing to metastatic lymph nodes is even rarer. Intractable explosive diarrhea is the most consistent and troublesome symptom in DCF. Treatment is mostly palliative. We present the case of a patient with malignant DCF owing to lymph node metastasis from carcinoma of the rectum. This patient’s diarrhea was successfully controlled with octreotide. We believe that this is the first reported case of malignant DCF arising due to metastatic lymph nodes and successfully palliated by octreotide.
Case report
A 61-year-old woman underwent low anterior resection 5 years earlier for a stage III C carcinoma rectum (AJCC TNM stage T4 N2 M0). Postoperatively, she had received adjuvant radiotherapy and chemotherapy. She was asymptomatic for 3 years, after which she started developing abdominal pain, urinary frequency and dysuria. Evaluation revealed left-sided hydro-ureteronephrosis owing to a large retroperitoneal lymph nodal mass. Computed tomography (CT)-guided fine needle aspiration cytology results suggested metastases from the previously treated cancer. Urinary obstruction was relieved by placement of a stent, and she was advised periodic stent replacement. A year later, she had an episode of intestinal obstruction. Laparotomy revealed dense adhesions between the retroperitoneal mass and proximal ileal loops which could not be released and she underwent bypass of this segment with an ileotransverse colon anastomosis. Furthermore, she received 6 courses of oxaliplatin-based chemotherapy.
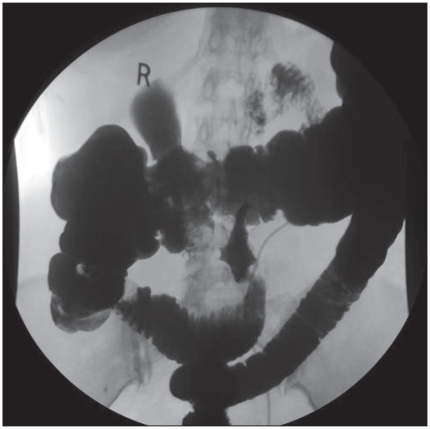
She now came to us with diarrhea (watery stools with a frequency of 10–12 times a day), weight loss, easy fatigability and anemia. Stool was positive for occult blood. A colonoscopic study was performed wherein the ileocolic anastomosis was normal. We saw a fistulous opening proximal to the site of anastomosis. Upper gastrointestinal endoscopy showed narrowing of the third part of duodenum (Fig. 1), and feculent material was aspirated. Part of a growth was seen in the lumen, a biopsy of which revealed adenocarcinoma, the features being identical to that of the previously resected rectal cancer. A malignant duodenocolic fistula was suspected. A barium meal evaluation showed rapid transit of barium into the colon. A barium enema revealed the fistulous communication between the proximal transverse colon and the third part of duodenum and confirmed the diagnosis.
Fig. 1.
Barium enema showing the flow of contrast into the duodenum through the fistulous communication.
We decided against any surgery after a detailed discussion with the patient because of the advanced nature of the disease. A trial of antibiotics was given with the intention of reducing the fecal contamination of small bowel, which may reduce diarrhea which was the most troublesome symptom for the patient. However, antibiotics offered little help. A trial with cholestyramine also proved futile. The patient was started on octreotide 50 μg three times a day, with an immediate reduction in the frequency of diarrhea by about 50% (4–6 times a day). The patient did not have any side effects of the drug, and she continued to take the same dose of the drug with a sustained response until her death from metastatic colon cancer.
Discussion
The first case of DCF was reported by Haldane in 1962.1 Subsequently, a report of 1400 cases of right-sided colon cancer observed duodenocolic fistula in only 2 cases.2 A review of literature shows few sporadic reports of DCF, emphasizing the rarity of the entity.
The causes of DCF can be benign or malignant. A few of the described benign causes include duodenal ulcer, Crohn disease, gallstones, ruptured pancreatic pseudocyst and stent migration.3 Malignant causes include3 colonic carcinoma, carcinoma of the gall bladder, carcinoma of the duodenum and even metastatic esophageal carcinoma.4 We believe that our case of malignant DCF has the rarest of the etiology. It was probably owing to metastatic lymph nodes infiltrating duodenum and colon resulting in a DCF.
Patients with malignant DCF can present with symptoms of the primary lesion, symptoms due to fistula or due to metastatic disease. Common symptoms include diarrhea, vomiting and weight loss. Some of the explanations given for diarrhea in DCF are:
fecal contamination of the stomach and duodenum leading to gastroenteritis5 and bacterial overgrowth in the entire small bowel,
direct emptying of the duodenal contents into the colon causing irritation of the colonic mucosa by bile salts and acid,6
reduced intestinal transit time and
fat malabsorption owing to reduction in concentration of conjugated bile acids.7
Diagnosis of DCF can be easily made by barium meal or barium enema.3 Endoscopic studies and CT scans help in evaluating the cause and operability of DCF.
Malignant DCF can be a difficult condition to treat. Treatment could be curative or palliative. Surgical treatment can be planned if the patient is reasonably fit to tolerate the procedure. Curative surgery can be offered in suitable patients with procedures like extended right hemicolectomy, hemicolectomy with excision and reconstruction of duodenum and hemicolectomy with pancreaticoduodenectomy.
The most troublesome symptom in DCF that mandates palliation is diarrhea. In fit patients, surgical palliation may be offered in the form of resection of underlying malignancy with fistulous communication or bypass of fistulous communication. Owing to the advanced nature of malignancy causing DCF and poor performance status, surgery may not be feasible in many patients. Conservative management of such patients includes correction of dehydration, electrolyte imbalance, correction of anemia and total parenteral nutrition to improve nutritional status. Various nonsurgical options have been described specifically to palliate diarrhea in DCF, including intraluminal antibiotics and cholestyramine.5
Octreotide has been tried in the treatment of refractory diarrhea in patients with AIDS, short-bowel syndrome,8 colonic adenomas, systemic sclerosis9 and carcinoid tumours. Being a somatostatin analogue, it has potent and nonspecific antisecretory and antimotility actions at multiple locations in the gastrointestinal tract. It inhibits gastric, pancreatic and intestinal secretions and release of vasoactive substances like vasoactive intestinal polypeptide and 5-hydroxytryptamine that are prokinetic. This may have a favourable effect by decreasing colonic mucosal irritation by hydrochloric acid and bile salts that are short circuited. It also reduces splanchnic blood flow to induce water and electrolyte absorption.8 Optimum dosage is yet to be determined and has ranged from 150 μg to 1500 μg per day.8 Our patient had an immediate favourable response to octreotide at a dose of 150 μg/day in 3 divided doses, with reduction in stool both frequency and volume after 2 days of therapy. We believe that a depot preparation of octreotide can offer similar benefits with better patient compliance. We could not try the depot preparation of octreotide because of its nonavailability in this part of our country.
Footnotes
Competing interests: None declared.
References
- 1.Haldane DR. Case of cancer of caecum accompanied by caeco duodenal and caeco colic fistulae. Edinburgh Med J. 1862;7:624–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Calmenson M, Black BM. Surgical management of carcinoma of the right portion of the colon. Surgery. 1947;21:476–81. [PubMed] [Google Scholar]
- 3.Soulsby R, Leung E, Williams N. Malignant colo-duodenal fistula; case report and review of literature. [(accessed 2009 Sept. 18)];World J Surg Oncol. 2006 4:86. doi: 10.1186/1477-7819-4-86. Available: http://wjso.com/content/4/1/86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reissman P, Steinhagen RM, Enright PF. Duodenocolic fistula: an unusual presentation of esophageal squamous cell carcinoma. Mt Sinai J Med. 1992;59:75–8. [PubMed] [Google Scholar]
- 5.Steer ML, Glotzer DJ. Colonic exclusion bypass principle. Its use in the palliative treatment of malignant duodenocolic and gastrocolic fistulas. Arch Surg. 1980;115:87–9. doi: 10.1001/archsurg.1980.01380010073017. [DOI] [PubMed] [Google Scholar]
- 6.Xenos ES, Halverson JD. Duodenocolic fistula: case report and review of literature. J Postgrad Med. 1999;45:87–9. [PubMed] [Google Scholar]
- 7.Ammon HV, Phillips SF. Inhibition of ileal water absorption by intraluminal fatty acids: influence of chain length, hydroxylation and conjugation of fatty acids. J Clin Invest. 1974;53:205–10. doi: 10.1172/JCI107539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried M. Octreotide in the treatment of refractory diarrhoea. Digestion. 1999;60(Suppl 2):42–6. doi: 10.1159/000051479. [DOI] [PubMed] [Google Scholar]
- 9.Soudah HC, Hasler WL, Owyang C. Effect of octreotide on intestinal motility and bacterial overgrowth in scleroderma. N Engl J Med. 1991;325:1461–7. doi: 10.1056/NEJM199111213252102. [DOI] [PubMed] [Google Scholar]