Abstract
Background
Surgical management is currently the most common treatment offered for ruptured Achilles tendon; however, the length of hospital stay varies among hospitals. The objective of our study was to compare the costs associated with hospital stay and safety in 2 groups of patients undergoing surgical treatment of Achilles tendon ruptures. The first group of patients represented the surgical arm of a randomized clinical trial, the Multicentre Achilles Tendon Treatment Study (MATTS), and the second group comprised surgically treated patients not included in that trial (non-MATTS).
Methods
We performed an observational analytical retrospective chart review of all patients surgically treated for acute Achilles tendon ruptures at all Calgary-area hospitals over a 3-year period (October 2002–September 2005) who met our inclusion criteria. We determined the costs associated with hospital stay, complications and readmissions for all patients.
Results
A total of 282 patients met our inclusion criteria. Hospital admission costs of patients enrolled in the MATTS trial were less than those of non-MATTS patients treated at each of the 3 Calgary adult hospitals. Non-MATTS patients remained in hospital for 1–4 days in contrast to MATTS patients, who were typically admitted and discharged the day of surgery. The complication rate was similar in both groups (MATTS 9% v. non-MATTS 8%). There were no readmissions in the MATTS group and 2 in the non-MATTS group. Between October 2002 and September 2005, an additional $236 436 was spent on non-MATTS patients who underwent surgery for Achilles tendon rupture.
Conclusion
Acute achilles tendon repair surgery is safe and less costly as an out-patient procedure.
Abstract
Contexte
À l’heure actuelle, on privilégie largement le traitement chirurgical dans les cas de rupture du tendon d’Achille. La durée de l’hospitalisation varie toutefois d’un hôpital à l’autre. Notre étude avait pour objectif de comparer les coûts associés à l’hospitalisation et la sécurité du traitement dans 2 groupes de patients soumis à une réparation chirurgicale de rupture du tendon d’Achille. Le premier groupe de patients représentait le volet chirurgical d’un essai clinique randomisé, l’étude MATTS (Multicentre Achilles Tendon Treatment Study) et le second groupe comprenait des patients traités par chirurgie mais non inscrits à cette étude (non-MATTS).
Méthodes
Nous avons étudié par observation et analyse rétrospective les dossiers de tous les patients traités chirurgicalement pour rupture du tendon d’Achille aiguë dans tous les hôpitaux de la région de Calgary sur une période de 3 ans (d’octobre 2002 à septembre 2005) qui répondaient à nos critères d’inclusion. Nous avons évalué les coûts associés à l’hospitalisation, les complications et les réadmissions pour tous les patients.
Résultats
En tout, 282 patients répondaient à nos critères d’inclusion. Les coûts d’hospitalisation ont été moins élevés pour les patients de l’étude MATTS que pour les patients non-MATTS traités dans chacun des 3 hôpitaux pour adultes de Calgary. Les patients non MATTS sont restés à l’hôpital de 1 à 4 jours, comparativement aux patients MATTS qui ont été admis à l’hôpital et sont repartis le jour même de la chirurgie. Les taux de complications ont été similaires dans les 2 groupes (MATTS 9 % c. non MATTS 8 %). On n’a eu aucune réadmission dans le groupe MATTS, tandis que 2 patients ont été réhospitalisés dans le groupe non-MATTS. Entre octobre 2002 et septembre 2005, on a consacré 236 436 $ de plus aux patients non MATTS soumis à une chirurgie pour rupture du tendon d’Achille.
Conclusion
La réparation chirurgicale de la rupture aiguë du tendon d’Achille est sécuritaire et moins coûteuse lorsqu’elle s’effectue en chirurgie ambulatoire.
The Achilles tendon is one of the most frequently ruptured tendons in the human body1 and has become the third most frequent major tendon injury behind those of the rotator cuff and knee-extensor mechanisms.2 Suchak and colleagues3 reported an incidence of 8.5 per 100 000 people in Edmonton, Alta. There has been an increase in incidence over the last half century,4 with studies reporting up to 18 per 100 000.1 The treatment of an Achilles tendon rupture is either surgical or nonsurgical. However, there is a lack of literature indicating which treatment leads to superior functional outcomes.5–10 Despite the reported surgical complications of adhesion, skin sloughing and infection,2,11 there is much debate surrounding the optimal method of treatment for these injuries.2,4,11 In a meta-analysis, Bhandari and colleagues10 reported a 68% reduction in the risk of rerupture with surgical treatment; however, a 4.7% incidence in postoperative infection suggests that there are benefits to nonoperative management. The functional superiority of one treatment over the other remains unknown.
To address this confusing literature, one of us (N.M.) agreed to participate in a multicentre randomized clinical trial (RCT) comparing surgical and nonsurgical treatments for acute Achilles tendon ruptures. The Multicentre Achilles Tendon Treatment Study (MATTS; ClinicalTrials.gov trial registration no. NCT00284648)12 originated at the University of Western Ontario, with Calgary being one of the major recruiting centres. From October 2002 to September 2005, patients were recruited into the MATTS trial. The treatment and admission algorithm for these patients differed from the existing practice pattern in Calgary. Eligible patients provided consented at the University of Calgary Sport Medicine Centre and were scheduled for urgent surgical repair and routinely treated on an outpatient basis as part of the MATTS study protocol.
As a direct result of participation in this trial, it was evident that surgically treated patients appeared to be treated effectively, safely and at less cost without overnight admission before surgery. There were no obvious negative trends or adverse effects observed in the MATTS patient population.
For patients with acute Achilles tendon ruptures who were not part of the MATTS trial (non-MATTS), the existing “standard of care” included confirming the diagnosis, orthopedic consultation, admission to hospital and surgical repair.13 The low-priority status for Achilles tendon surgery meant that patients waited in a hospital bed for several hours to a few days before an operating room became available. After surgery, patients were either discharged the same day or thereafter, depending on their postoperative status. At the time, there was no agreed-upon standard of care for the pre- and/or postoperative management of Achilles tendon ruptures in the Calgary area.
The observation that patients enrolled in the RCT were being treated effectively and safely allowed a natural comparison between the MATTS and non-MATTS patients. Therefore, we sought to determine whether there was a difference in hospital costs and safety of surgical repair of acute Achilles tendon ruptures, comparing patients enrolled in the MATTS trial with non-MATTS patients in the Calgary area during the same time period.
Methods
This observational analytical study involved the review of hospital charts for patients receiving Achilles tendon repair surgery over a 3-year period (October 2002–September 2005, inclusive) in Calgary, Alberta. The University of Calgary Conjoint Health Research Ethics Board approved the study protocol.
All patients had surgery at 1 of the 3 adult hospitals in Calgary (Peter Lougheed Centre, Rockyview General and Foothills Medical Centre) between October 2002 and September 2005.3 We identified the cohort using International Classification of Disease, version 10 (ICD-10) diagnostic (S860*) and procedure codes (1WT79, 1WT80*) for the repair of achilles tendon rupture. All patients were eligible for the final cost analysis if our inclusion and exclusion criteria were satisfied (Box 1). Inclusion and exclusion criteria defined for the present study were identical to those used in the MATTS so that the patients could be compared.
Box 1.
Inclusion and exclusion criteria
Inclusion criteria
Acute complete rupture of the Achilles tendon (≤ 14 days from injury to surgery date)
Age 18–70 years
Date of Injury between October 2002 and September 2005
Surgical repair
Exclusion criteria
Nonsurgical treatment
Clinically important ipsilateral injury (i.e., femur or tibia fracture)
Open injury of the Achilles tendon
Neurological disease (i.e., stroke, cerebral palsy)
Collagen disease (i.e., Ehlers–Danlos)
Pregnancy
Fluoroquinolone-associated rupture (rupture within 2 weeks of therapy)
Medical contraindications to surgery
Diabetes
Peripheral vascular disease
Clinical avulsion of Achilles tendon from calcaneus
Delayed repair of the Achilles tendon rupture (> 14 days from injury to surgery date)
Data extraction and identification of patient groups
We reviewed the patient charts at each hospital and transferred information onto a prescreened data extraction form. Hospital admission information included orthopedic consultation(s) dates, surgery dates and day or overnight stays, complications and readmissions. We established inter-rater reliability by comparing data extraction from individual patient charts until 100% agreement was obtained. This information was subsequently entered electronically for future storage and retrieval.
We classified patients in the MATTS group if they participated in the randomized clinical trial and in the non-MATTS group if they received surgical treatment outside of the trial. We identified patients in the MATTS group by cross-referencing the study data (i.e., birth, orthopedic consult and surgery dates) after data extraction was complete to avoid bias.
Calculation of time periods
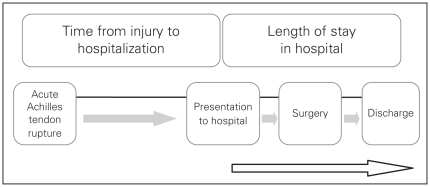
We used the data retrieved for each patient to calculate the length of stay in hospital (Fig. 1): the number of days between presentation to the hospital for definitive surgical treatment and the discharge date.
Fig. 1.
Calculated time periods for cost analysis of Achilles tendon surgery.
Categorization of patients
We categorized patients in each group based on the type of stay in hospital as follows.
Day surgery: patients who presented to the hospital, had surgery and were discharged on the same day.
ADOP-24 hours: patients who were admitted the day of the procedure (ADOP) and required a hospital bed for 1 night postsurgery.
ADOP-48 hours: patients who were admitted the day of the procedure and required a hospital bed for 2 nights postsurgery.
Admitted: patients who were admitted to the hospital for 1 or more days before surgery.
Cost calculations
We calculated individual hospital costs for each patient based on the length of stay in hospital stay and any additional orthopedic consultations. The average health care cost for a day surgery procedure was $660 at each hospital, and overnight costs varied among the hospitals: $909 and $1433 (unpublished data, 2006). The costs of the surgical procedure, anesthetic, nursing staff and surgical assistants were consistent between hospitals (unpublished data, 2006). We determined additional orthopedic consultation fees for weekday and weekend consultations and added these to the daily hospital costs. We calculated the average cost for day and overnight stays for each group of patients.
Complications
We recorded the intraoperative and perioperative complications for each patient. The perioperative complications were recorded if the event occurred within 6 weeks of the surgery. We defined hospital readmissions as those related to the Achilles tendon repair that occurred within 3 months of the initial surgery.
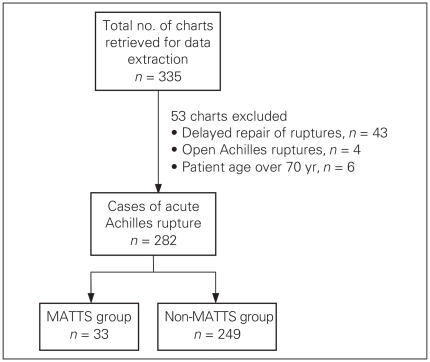
Results
We extracted a total of 335 charts from all Calgary adult hospitals. We excluded 53 charts from the analysis, resulting in a total of 282 charts for final analysis. There were 33 patients in the MATTS group and 249 in the non-MATTS group (Fig. 2).
Fig. 2.
Selection process for charts included in our review. MTTS = Multicentre Achilles Tendon Treatment Study.
Demographic information is summarized in Table 1. Table 2 outlines the activities at the time of injury for all patients.
Table 1.
Demographic and clinical characteristics for all patients undergoing Achilles tendon surgery at 3 adult hospitals in Calgary, Alberta, from October 2002 to September 2005
| Characteristic | Group | |
|---|---|---|
| MATTS, n = 33 | Non-MATTS, n = 249 | |
| Age, mean (range) [ 95% CI] yr | 38.5 (23–58) [35.5–41.5] | 41.2 (18–64) [40.0–42.3] |
| Sex, M:F | 27:6 | 205:44 |
| Side of injury, R:L | 19:14 | 105:144 |
| Anesthetic time, mean (95% CI) min | 0:58 (0:53–1:03) | 0:51 (0:49–0:54) |
CI = confidence interval; F = female; L = left; M = male; MATTS = Multicentre Achilles Tendon Treatment Study; R = right.
Table 2.
Activity at time of injury precipitating Achilles tendon surgery
| Activity | Group, no. patients | |
|---|---|---|
| MATTS | Non-MATTS | |
| Squash | 3 | 34 |
| Soccer | 7 | 28 |
| Volleyball | 2 | 25 |
| Baseball | 2 | 24 |
| Tennis | 1 | 21 |
| Basketball | 4 | 17 |
| Football | 3 | 19 |
| Walking/running | 0 | 16 |
| Badminton | 2 | 10 |
| Skiing/snowboarding | 1 | 5 |
| Hockey | 0 | 5 |
| Rugby | 0 | 3 |
| Other (sport related) | 5 | 14 |
| Falling | 1 | 2 |
| Pushing an object | 1 | 6 |
| Work related | 1 | 5 |
| Other (non–sport related) | 0 | 15 |
| Total | 33 | 249 |
MATTS = Multicentre Achilles Tendon Treatment Study.
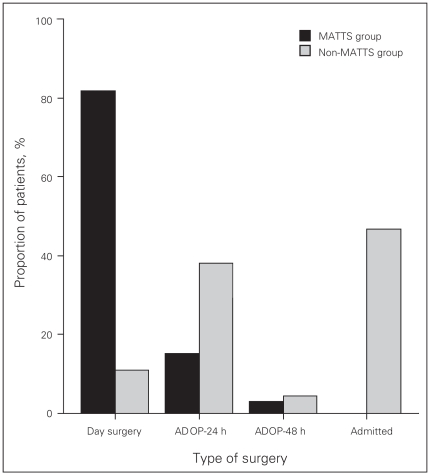
Day surgery, ADOP and admitted patients
Most of the MATTS patients (27 of 33; 82%) had day surgery. Of those remaining, 5 of 33 (15.2%) stayed in hospital overnight after surgery (ADOP-24 hours) and 1 patient (3%) stayed 2 days (ADOP-48 hours). None of the MATTS patients was admitted to the hospital before surgery (Fig. 3).
Fig. 3.
Distribution of patients based on type of surgery (day surgery v. overnight stays). ADOP = admitted on the day of procedure; MATTS = Multicentre Achilles Tendon Treatment Study.
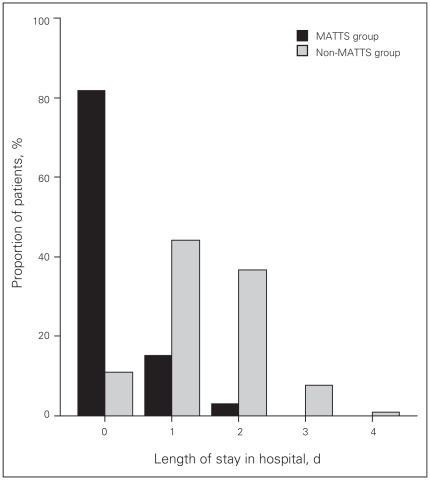
Only 11% (27 of 249) of patients in the non-MATTS group had day surgery. The remaining patients were admitted for 1 (95 of 249; 38%) or 2 nights (12 of 249; 5%) after surgery. However, most non-MATTS patients (115 of 249; 46%) were admitted to hospital to await surgical repair (Fig. 3). The length of stay in hospital for the non-MATTS group ranged from 1 to 4 days. For each length of stay, the proportion of non-MATTS patients was substantially greater than that of MATTS patients (Fig. 4).
Fig. 4.
Length of stay in hospital for Achilles tendon surgery, by group. MATTS = Multicentre Achilles Tendon Treatment Study.
Cost calculations
All patients had an initial orthopedic consultation; however, some patients required 1 or 2 additional consultations. The cost for a consultation was $83.57 on a weekday and $157.19 on the weekend.14 We determined the individual costs by adding the day surgery cost ($660) and the additional weekday or weekend orthopedic consultation fees. The average cost per patient in the MATTS group for a day surgery was $682, and the average for an overnight stay was $1237. In the non-MATTS group, the average day surgery cost per patient was $669, and the average overnight cost per patient admitted for 1 or more nights was $1709 (Table 3).
Table 3.
Cost of day surgery versus overnight stays in hospital for Achilles tendon surgery
| Group | Day surgery |
Overnight stay |
||
|---|---|---|---|---|
| Proportion of patients (%) | Total cost (mean) $ | Proportion of patients (%) | Total cost (mean) $ | |
| MATTS | 27/33 (82) | 18 408 (682) | 6/33 (18) | 7 419 (1237) |
| Non-MATTS | 27/249 (11) | 18 071 (669) | 222/249 (89) | 379 497 (1709) |
MATTS = Multicentre Achilles Tendon Treatment Study.
Anesthetic times, complications and readmissions
The type of anesthetic used was consistent for all patients, as most agreed to a general anesthetic. The anesthetic time for all patients undergoing Achilles tendon repair was similar (MATTS 58 min v. non-MATTS 51 min).
In the MATTS group, there was a 9% (3 of 33) peri-operative complication rate, including superficial infection (n = 1) and delayed wound healing (n = 2). The complications observed in the MATTS group fully resolved without any consequences. In the non-MATTS group, there was a 7% (18 of 249) perioperative complication rate, which occurred in only overnight patients and included increasing pain (n = 3), falling on the operative leg (n = 4), delayed wound healing (n = 3), swelling (n = 2), superficial infections (n = 5) and gout (n = 1). All complications resolved. Two patients (0.8%) in the non-MATTS group were readmitted: 1 for a pulmonary embolus and 1 for a delayed presentation of compartment syndrome.15
Discussion
Summary of main results
The patients were demographically similar and most patients in both groups were involved in sport at the time of injury. Most of the MATTS patients had day surgery (length of stay 0 d); however, a few remained in hospital overnight because of surgeon/patient preference. In contrast, non-MATTS patients were mostly admitted on the day of the procedure and required a bed for 1 night post-surgery (length of stay 1–4 d). The cost of an overnight stay in the MATTS group was $1237 per patient compared with $1709 per patient in the non-MATTS group. Although the average cost per patient is comparable between the 2 groups, the total cost is considerably higher (non-MATTS $379 497 v. MATTS $7419; Table 3). Complications and readmissions only occurred in the overnight patients, and the rate was nearly similar in both groups (non-MATTS 8% v. MATTS 9%). Both of the serious complications occurred in the non-MATTS group: a pulmonary embolus and an acute compartment syndrome. There were no deep infections and no reruptures up to 3 months postoperatively in either group.
Explanation of findings
The higher average cost per patient for day surgery in the MATTS group ($682) was a result of additional orthopedic consultations. Since not all Calgary surgeons were involved with the MATTS trial, an additional consultation by a participating surgeon was required in some cases to confirm eligibility or perform the surgery. If non-MATTS patients were scheduled for day surgeries without the requirement to assess for study eligibility, it is likely that only 1 orthopedic consultation was necessary; however, in some cases extra consultations occured with non-MATTS patients because the admitting surgeon on call was not always the treating surgeon. Patients admitted before the day of surgery also incurred costs, possibly owing to the type of referral centre and the acuity of orthopedic trauma. If all overnight patients in each group had received day surgery, the total savings would have been $3459 for the MATTS and $232 977 for the non-MATTS group. The cumulative savings would have amounted to $236 436 if all Achilles tendon repairs between October 2002 and September 2005 had been out-patient procedures. Furthermore, day surgery would have avoided the 365 hospital bed days used within the same period.
The complication rate in this study is perhaps more detailed than what is reported in literature. For example, a fall requiring a cast change or reactive gout are postoperative complications that are unlikely reported in the literature. Therefore, it is likely that a 9% complication rate is an overestimation. The infection rate reported in the literature is consistent with that of this study.10 Two non-MATTS patients were readmitted, 1 for compartment syndrome15 and 1 for a pulmonary embolus. Lapidus and colleagues9 quoted a 36% incidence of deep vein thrombosis with no pulmonary emboli in their trial of achilles tendon repairs.
Limitations
The nature of this observational analytical study limits our ability to capture reasons for prolonged admission times. The inconsistent detail recorded in the hospital charts did not allow for an analysis of comorbidities. Therefore, the effects of smoking status, concurrent medication or activity level on prolonged admission times could not be determined in this study. Future studies should prospectively analyze patients and stratify them according to risk factors that could potentially require admission or delay discharge after a surgical procedure.
Our study also excluded exact costs for nursing, medications and other potential direct and indirect costs to the patients and health care system. However, it is assumed that these costs would be similar between groups. By accounting for costs owing to hospital stays and complication rates, additional overnight stays appear to offer no benefit to the patient compared with day surgery. In addition, long-term benefits to the patient such as functional outcomes and a return to previous activity levels cannot be compared between the groups because it was not possible to follow up on patients in the non-MATTS group.
One of the main concerns of this comparison is whether patients in the MATTS group were representative of the available population and, therefore, whether the comparison was valid and generalizable. The MATTS group represented only 12% of the acute surgically treated patients. Other potential patients were treated nonsurgically and were not part of this analysis. Most patients were treated by surgeons not involved in the trial and therefore were not included. The limitations of retrospective data preclude in-depth comparisons between groups. However, the demographic characteristics and activities of the 2 groups were similar, and most patients in both groups were actively involved in sports at the time of their injuries. Therefore, we considered the 2 groups to be comparable.
Conclusion
Achilles tendon rupture is a common injury that frequently requires surgical repair. Our study has demonstrated that surgical treatment of acute Achilles tendon ruptures is both safe and less costly when performed as an outpatient procedure. Serendipitously, the impact of participating in the MATTS randomized clinical trial with its specific protocol has helped to define an improved and less costly standard of care for all patients.
Acknowledgements
The authors would like to acknowledge the investigators of the MATTS clinical trial. The investigators are Dr. A. Amendola and Dr. K. Willits and the Fowler Kennedy Sport Medicine Clinic, University of Western Ontario. The authors would also like to acknowledge Mrs. Heather Hannaford for her assistance with the data acquisition.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study, acquired and analyzed the data, wrote the article and approved its publication. Drs. Goel and Mohtadi and Ms. Chan reviewed the article.
This work was presented at the meetings of the Canadian Academy of Sport Medicine, March 29, 2007, in Québec City, Que., and the Canadian Orthopedic Association, Jun. 1–3, 2007, in Halifax, NS.
References
- 1.Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:277–9. doi: 10.3109/17453679608994688. [DOI] [PubMed] [Google Scholar]
- 2.Lesic A, Bumbasirevic M. Disorders of the Achilles tendon. Orthop Trauma. 2004;18:63–75. [Google Scholar]
- 3.Suchak AA, Bostick G, Reid D, et al. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26:932–6. doi: 10.1177/107110070502601106. [DOI] [PubMed] [Google Scholar]
- 4.Ufberg J, Harrigan RA, Cruz T, et al. Orthopedic pitfalls in the ED: Achilles tendon rupture. Am J Emerg Med. 2004;22:596–600. doi: 10.1016/j.ajem.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Cetti R, Christensen SE, Ejsted R, et al. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–9. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 6.Moller M, Movin T, Granhed H, et al. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83:843–8. doi: 10.1302/0301-620x.83b6.11676. [DOI] [PubMed] [Google Scholar]
- 7.Inglis AE, Scott WN, Sculco TP, et al. Ruptures of the tendo achillis. An objective assessment of surgical and non-surgical treatment. J Bone Joint Surg Am. 1976;58:990–3. [PubMed] [Google Scholar]
- 8.Nistor L. Surgical and non-surgical treatment of Achilles tendon rupture. A prospective randomized study. J Bone Joint Surg Am. 1981;63:394–9. [PubMed] [Google Scholar]
- 9.Lapidus LJ, Rosfors S, Ponzer S, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma. 2007;21:52–7. doi: 10.1097/01.bot.0000250741.65003.14. [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Guyatt GH, Siddiqui F, et al. Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res. 2002:190–200. doi: 10.1097/00003086-200207000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Rajasekar K, Gholve P, Faraj AA, et al. A subjective outcome analysis of tendo-Achilles rupture. J Foot Ankle Surg. 2005;44:32–6. doi: 10.1053/j.jfas.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Willits K, Mohtadi N, Keane C, et al. Operative versus non-operative treatment of Achilles tendon ruptures: a randomized controlled trial (SS-66) [(accessed 2009 Oct. 27)];Arthroscopy. 2009 25:e36. Available: www.arthroscopyjournal.org/article/S0749-8063(09)00306-5/abstract. [Google Scholar]
- 13.Ingvar J, Tagil M, Eneroth M. Nonoperative treatment of Achilles tendon rupture: 196 consecutive patients with a 7% re-rupture rate. Acta Orthop. 2005;76:597–601. doi: 10.1080/17453670510041619. [DOI] [PubMed] [Google Scholar]
- 14.Alberta Government. Alberta health care insurance plan schedule of medical benefits part C: price list. Calgary (AB): Alberta Health and Wellness; 2006. [Google Scholar]
- 15.Reed J, Hiemstra LA. Anterior compartment syndrome following an Achilles tendon repair: an unusual complication. Clin J Sport Med. 2004;14:237–41. doi: 10.1097/00042752-200407000-00007. [DOI] [PubMed] [Google Scholar]