Abstract
Background
In the technique of percuatenous pinning of proximal humerus fractures, the appropriate entry site and trajectory of pins is unknown, especially in the adolescent population. We sought to determine the ideal entry site and trajectory of pins.
Methods
We used magnetic resonance images of nonfractured shoulders in conjunction with radiographs of shoulder fractures that were treated with closed reduction and pinning to construct 3-dimensional computer-generated models. We used engineering software to determine the ideal location of pins. We also conducted a literature review.
Results
The nonfractured adolescent shoulder has an articular surface diameter of 41.3 mm, articular surface thickness of 17.4 mm and neck shaft angle of 36°. Although adolescents and adults have relatively similar shoulder skeletal anatomy, they suffer different types of fractures. In our study, 14 of 16 adolescents suffered Salter–Harris type II fractures. The ideal location for the lateral 2 pins in an anatomically reduced shoulder fracture is 4.4 cm and 8.0 cm from the proximal part of the humeral head directed at 21.2° in the coronal plane relative to the humeral shaft.
Conclusion
Operative management of proximal humerus fractures in adolescents requires knowledge distinct from that required for adult patients. This is the first study to examine the anatomy of the nonfractured proximal humerus in adolescents. This is also the first study to attempt to model the positioning of percutaneous proximal humerus pins.
Abstract
Contexte
Dans la technique du brochage transcutané des fractures de la partie proximale de l’humérus, on ne connaît pas le point d’entrée ou la trajectoire appropriés des broches, spécialement chez les adolescents. Nous avons cherché à déterminer le placement idéal du point d’entrée et de la trajectoire des broches.
Méthodes
Nous avons utilisé des images obtenues par résonance magnétique d’épaules non fracturées et des radiographies de fractures de l’épaule traitées par réduction fermée et par brochage afin de construire des modèles tridimensionnels générés par ordinateur. Nous avons utilisé un logiciel d’ingénierie pour déterminer l’emplacement idéal des broches. Nous avons aussi effectué une étude documentaire.
Résultats
L’épaule non fracturée de l’adolescent a une surface articulaire d’un diamètre de 41,3 mm et d’une épaisseur de 17,4 mm, et l’angle col-diaphyse s’établit à 36°. Même si l’anatomie squelettique de l’épaule est relativement semblable chez les adolescents et les adultes, ils subissent des types de fractures différents. Au cours de notre étude, 14 adolescents sur 16 avaient subi une fracture de Salter–Harris de type II. L’emplacement idéal des deux broches latérales dans la réduction anatomique d’une fracture de l’épaule se situe à 4,4 cm et 8,0 cm de la partie proximale de la tête de l’humérus dirigée à un angle de 21,2° sur le plan coronal par rapport à la diaphyse de l’humérus.
Conclusion
La prise en charge opératoire de fractures à la partie proximale de l’humérus chez des adolescents exige des connaissances distinctes de celles qu’il faut pour traiter des patients adultes. Cette étude est la première qui analyse l’anatomie de la partie proximale non fracturée de l’humérus chez les adolescents. Il s’agit aussi de la première étude où l’on essaie de modéliser le positionnement de broches transcutanées à la partie proximale de l’humérus.
The technique of percutaneous pinning of the proximal humerus has been described by several other authors.1–5 However, there are no studies exploring the appropriate entry point and trajectory of the pins in the adolescent population. The distinction between the adult and adolescent patient is important because the proximal humerus fracture occurs more proximally in adolescents than in adults. Adolescents mainly suffer Salter–Harris type II fractures, whereas adults have surgical neck fractures.6–13 Furthermore, the fracture line angle is different. Therefore, adolescents with proximal humerus fractures require special consideration. There are many potential pin configurations. Each of these pin arrangements is a balance between fixation into the humeral shaft and humeral head, and optimization of the biomechanical trajectory across the fracture line. The purpose of this study was to determine the appropriate starting point and trajectory of pins using computer-generated models of adolescent shoulders.
Methods
To determine these parameters, we carried out the following steps:
construct a 3-dimensional (3-D) computer-generated model of the nonfractured adolescent proximal humerus
determine the fracture pattern and the fracture geometry
determine the angle of insertion of the pins
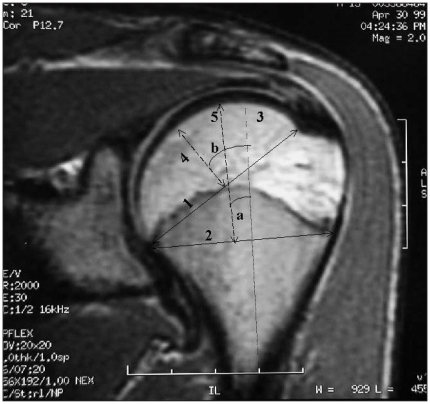
For the first step we reviewed magnetic resonance imaging (MRI) scans of nonfractured shoulders in an adolescent population. We reviewed all shoulder MRI scans carried out at our institution between 1999 and 2000. Six shoulder MRIs had been performed. Based on our review of the MRI scans, we gathered pertinent data to recreate 3-D models of the proximal humerus. We measured parameters based on studies of the adult proximal humerus anatomy (Fig. 1 and Fig. 2).14–16 We measured directly the magnetic resonance images and normalized the images to the actual size with the use of the centimetre calibration markers that were included in each imaging sequence. We used the midsagittal image to measure each parameter.
Fig. 1.
Coronal magnetic resonance images of a nonfractured shoulder with measured parameters. (1) Articular surface diameter; the diameter of the articular surface at the level of the margin of the cartilage. This parameter defines the epiphyseal sphere. (2) Physeal diameter; because the physis is curved, the distance between the 2 ends of the physis are used to measure this parameter. (3) Metaphyseal axis; a line at the midpoint of the metaphyseal width drawn parallel to the metaphysis. (4) Articular surface thickness; the perpendicular distance from the apex of the diameter of curvature to the articular margin. (5) The perpendicular line to the physeal diameter used in the measurement of the physeal shaft angle. (a) Physeal shaft angle; the angle between the metaphyseal axis and the perpendicular line to the physeal diameter. (b) Neck–shaft angle; the angle between the metaphyseal axis and the perpendicular line to the articular surface diameter (5). Not shown: humeral width; the narrowest part of the humerus in the coronal and axial planes. The narrowest part is measured because this is the critical parameter that defines the distance between the holes on the guide. Not shown: medial offset; perpendicular distance between the centre of the epiphyseal sphere and the central axis of the metaphyseal cylinder.
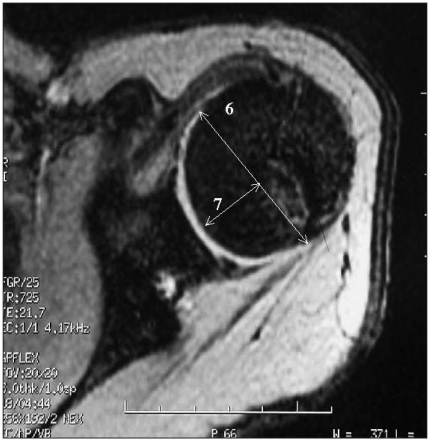
Fig. 2.
Axial magnetic resonance images of a nonfractured shoulder with measured parameters, including the (6) articular surface diameter and the (7) articular surface area.
The 3-D models are simplified to a cylinder to represent the humeral shaft and a sphere to represent the humeral head. Boileau and Walch14 suggested that the cylinder and the sphere are appropriate geometrical models to represent the proximal humerus. We used the humeral shaft diameter measurements to create the cylinder that represents the humeral shaft. We used the rest of the measurements to create the sphere that represents the proximal humerus and to establish the correct relation to the humeral metaphysis/diaphysis. In addition, we carried out a literature search to determine the dimensions of non-fractured humeri in adults for comparison.
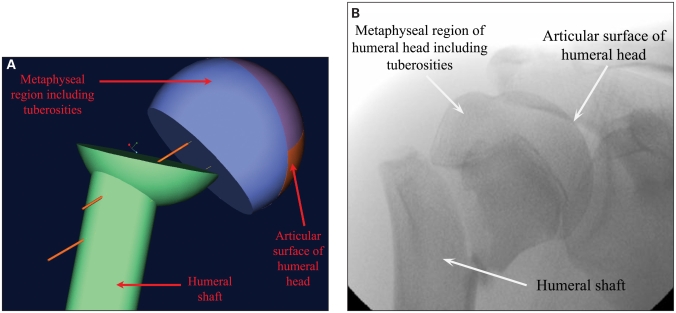
Next, we reviewed all cases at our institution of proximal humeral fractures that were treated by closed reduction and percutaneous insertion of internal fixation. We reviewed the charts as well as preoperative and postoperative radiographs of the patients whose care had been managed in this fashion. Finally, we used the Pro/Engineer software program (Parametric Technology Corp.) to create 3-D images of the proximal humerus, which we used to calculate the optimal point of entry and angle of insertion of the pins (Fig. 3 and Fig. 4).
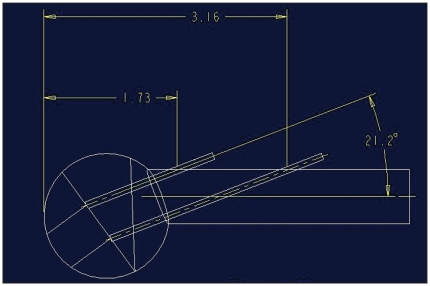
Fig. 3.
Diagram of the entry site and trajectory of pins in the anatomically reduced shoulder.
Fig. 4.
(A) Three-dimensional model of a proximal humerus fracture in an adolescent and (B) the corresponding radiograph.
Results
We identified 17 patients who had closed reduction and internal fixation at our institution between 1995 and 1999. One patient required immediate removal of the pins because the pins had been inserted into the intra-articular space; however, we still included this patient in the analysis. We could not locate 1 patient’s radiographs. This left 16 patients for analysis.
Fourteen patients had a Salter–Harris type II proximal humerus fracture, and 2 had a proximal metaphyseal humerus fracture. The mean age of the patients was 15.2 years, and there were 12 male and 4 female patients. Seven of the fractures were fixed with 2 Kirschner wires, 5 were fixed with 1 Kirschner wire, 2 were fixed with 3 Kirschner wires and 2 were fixed with 1 partially threaded Kirschner wire. There was no loss of fixation and all fractures united.
Modelling of pin site insertion and trajectory
The entry site and trajectory of the pins mainly depends on the reduction and the configuration of the head–shaft junction at the fracture site. Our approach to this problem has been to create and use 3-D computer-generated models of the shoulder. Review of the pediatric and adolescent orthopedic literature did not yield any studies that elaborated on position of pin placement. Within the adult literature, we found 2 studies that described the ideal position of the pins.3,17 Williams and Wong3 have recommended a starting point midway between the lateral and anterior surfaces of the arm above the insertion of the deltoid. They suggest angulation of the pins 45° to the shaft in the coronal plane and 30° to the shaft in the sagittal plane. The second pin is placed parallel to the first either proximally or distally. Rowles and McGrory17 have outlined guidelines for pin placement based on the proximity of pins to surrounding neurovascular structures. We summarize their recommendations later in the discussion.
Anatomy of the nonfractured shoulder
To construct the 3-D model of the adolescent proximal humerus, we used MRI scans from 6 patients (mean age 15.2, range 14–17 yr) (Table 1). The 3-D model used to represent the shoulder consists of a cylinder for the humeral shaft and a sphere for the proximal humerus. The sphere consisted of an “epiphyseal sphere,” which represents the articular surface, and a “metaphyseal sphere,” which represents the spherical portion of the head below the physis. These 2 have different radii of curvatures.
Table 1.
Important anatomic parameters measured from magnetic resonance images of nonfractured shoulders of adolescent patients
| Patients ID | Age, yr | Humeral head diameter, mm | Articular surface thickness, mm | Phyeal diameter, mm | Physeal angle, ° | Medial offset, mm | Neck shaft angle, ° | Humeral head diameter, mm | Articular surface thickness, mm | Humeral width, mm |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14 | 45.0 | 16.7 | 41.7 | 0.0 | 6.7 | 40.0 | 40.0 | 21.5 | 18.5 × 15.4 |
| 2 | 17 | 37.6 | 17.6 | 35.3 | 0.0 | 5.9 | 35.0 | 38.3 | 16.7 | 13.3 × 11.7 |
| 3 | 14 | 40.0 | 18.8 | 38.8 | 0.0 | 5.9 | 40.0 | 32.9 | 10.0 | 17.0 × 18.6 |
| 4 | 16 | 45.5 | 18.2 | 41.8 | 3.0 | 5.5 | 30.0 | 40.0 | 16.4 | 23.6 × 21.8 |
| 5 | 15 | 47.0 | 18.0 | 46.0 | 5.0 | 8.0 | 40.0 | 47.5 | 18.8 | 22.5 × 13.8 |
| 6 | 15 | 43.8 | 18.8 | 41.2 | 6.0 | 6.2 | 32.0 | 38.3 | 16.7 | 18.3 × 21.7 |
| Mean | 15.2 | 43.1 | 18.0 | 40.8 | 2.3 | 6.4 | 36.2 | 39.5 | 16.7 | 19.7 × 16.3 |
It is quite interesting to compare the shoulder anatomy of the adolescent with that of the adult. The anatomic parameters of the nonfractured adult shoulder are outlined in Table 2.14–16 The articular surface diameter is one of the important parameters for creating the 3-D model of the humeral head. The mean measurement is 41.3 mm in adolescents and 47.3 mm in adults (Table 3). The articular surface thickness was 17.4 mm in adolescents and 17.9 mm in adults. This parameter defines the width of the articular surface of the humeral head (Fig. 1). There was a slight discrepancy in the neck–shaft angle between the 2 groups. The adolescent group had an average measurement of 36.2° and the adults had an average measurement of 41.8°.
Table 2.
Summary of important anatomic parameters measured from nonfractured shoulders of adults
| Study | Mean age (SD) [range], yr | Humeral canal, mm | Humeral head offset, mm | Articular surface diameter, mm | Thickness of articular surface, mm* | Neck shaft angle, ° | Diameter of curvature of humeral head, mm | Retroversion (trans-epicondylar axis), ° (SD) |
|---|---|---|---|---|---|---|---|---|
| Iannotti et al.15 | 86 (13) [67–95] | — | — | 50 coronal 46 axial |
20 | 45 | — | — |
| Boileau and Walch14 | 75 (14) [26–104] | — | 6.9† | 43.3 | 15.2 | 39.6 | 46.2 | 17.9 (13.7) |
| Pearl and Kurutz16 | 72 [59–83] | 12 | 9.7 | 50.6 | 18.5 | 40.7 | — | — |
| Mean | 78 | 12 | 8.3 | 47.3 | 17.9 | 41.8 | 46.2 | 17.9 |
SD = standard deviation.
Coronal and axial planes.
Medial offset.
Table 3.
Comparison of important anatomic measurements of the proximal humerus in adolescents versus adults
| Parameter; mean | Adolescents | Adults |
|---|---|---|
| Articular surface diameter, mm | 41.3 | 47.3 |
| Articular surface thickness, mm | 17.4 | 17.9 |
| Neck–shaft angle, ° | 36.2 | 41.8 |
| Medial offset, mm | 6.4 | 8.3 |
| Physeal diameter, mm | 40.8 | — |
| Physeal–shaft angle, ° | 2.3 | — |
Biomechanical consideration
For proximal humerus surgical neck fractures in adults that would be fixed with percutaneous pins, most surgeons agree that 2 lateral pins are essential. The debate is whether additional pins such as antegrade pins through the greater tuberosity are necessary. Naidu and colleagues18 tried to answer this question by carrying out a cadaveric biomechanical study, and found that 2 lateral pins alone is the weakest biomechanical configuration. However, in our series, only lateral pins were used, and there was no failure of the internal fixation. Jiang and colleagues19 explored the biomechanical strength of 4 parallel pins versus 4 convergent pins. They did find that parallel pins were biomechanically stronger; however, the clinical relevance of this study is questionable as it is difficult to place 2 lateral pins into the humeral head, let alone 4. For the purposes of our study, we decided to model the pin configuration of 2 lateral retrograde pins.
Computer modelling of pin positions
The distal 2 pins are the most difficult to place. The proximal greater and lesser tuberosity pins are less challenging to place; therefore, we limited the modelling of pin placement to the distal 2 lateral pins. Initially, we simulated the pin site positioning to place pins in the centre of the head crossing the fracture at 90°. Because the majority of fractures were Salter–Harris type II fractures (14/16 patients), we modeled the pins to be perpendicular to the physis. However, it became apparent that this configuration is not realistic because there would be very little purchase in the distal limb of the humerus. Our next idea was to have both pins enter at the same level but to place them at the anterior and posterior aspects of the humeral head. Technically, this is a much more challenging operation as the humeral shaft is quite narrow. In our study, the average width of the humeral shaft was 19.7 mm × 16.3 mm (Table 2). Furthermore, it would be difficult to control for the coronal trajectory as well as the sagittal direction, as one has to account for the inherent retroversion of the proximal humerus.
Finally, we decided to model the pin placement to optimize the balance between the amount of humeral shaft fixation and humeral head fixation. Furthermore, to simplify the operation, we decided to model the construct such that both the proximal and distal pins would have a similar trajectory. The result (Fig. 3) is an entry site of 4.4 cm from the top of the humeral head for the proximal pin with a trajectory of 21.2° in the coronal plane relative to the humeral shaft. The distal pin would be placed 8.0 cm from the top of the humeral head with a trajectory of 21.2° in the coronal plane relative to the humeral shaft. With respect to this modelling philosophy, the above measurements define the safe proximal and distal boundaries of pin placement to prevent extrusion from the humeral neck.
Safety of pin placement
An important consideration in placement of percutaneous pins is the surrounding neurovascular structures. Unfortunately, there are no studies that have evaluated the anatomic location of the axillary nerve, radial nerve, anterior circumflex artery, posterior circumflex artery or the cephalic vein in the adolescent population. However, there has been some work done in the adult population. Rowles and McGrory17 carried out a cadaveric study to evaluate the proximity of the pins to the surrounding vital structures. Pins were placed into the proximal humerus, after which the specimens were dissected and the distance between the pins and the neurovascular structures were measured. Unfortunately, the authors did not specify or standardize the most important part of the study: the entry site and trajectory of the pins. Despite this grave shortcoming, the study still yielded valuable information. The distal lateral pins were on average 17 (range 13–25) mm from the anterior branch of the axillary nerve. The proximal lateral pins were on average 3 (range 1–10) mm from the anterior branch of the axillary nerve. The authors also evaluated greater tuberosity pins in this study but, unfortunately, there was no standardization nor clear criteria for the placement of these pins. The distal tip of these pins were at a mean distance of 8 (range 1–18) mm from the posterior humeral circumflex artery and 10 (range 0–22) mm from the axillary nerve. Based on their findings, the authors suggested that the starting point for the lateral pins should be, at minimum, twice the distance from the top of the humeral head to the most inferior margin of the articular cartilage. Pins should not be placed distal to the deltoid tuberosity because of risk of injury to the radial nerve. As for the greater tuberosity pins, the authors suggested that they should be aimed for a point at least 20 mm distal from the inferior extent of the humeral head to avoid injury to the axillary nerve and the posterior circumflex artery.
Indeed, the biggest concern during percutaneous pin placement is injury to the axillary nerve. Three studies have evaluated the anatomy of the axillary nerve by dissecting out the course of the nerve in cadaveric specimens (Table 4).20–22 The nerve is about 4 cm below the posterior border of the acromion and 6 cm below the anterior border of the acromion. Provided that these measurements are applicable to an adolescent population, our computer modelling of pin arrangement still places them in a safe zone.
Table 4.
Anatomic studies of the axillary nerve
| Study | No. specimens | Results |
|---|---|---|
| Cetik et al.20 | 24 adult shoulders | Mean (SD) distance from anterior edge of acromion was 6.08 (0.45) cm; from posterior edge of acromion was 4.87 (0.26) cm. |
| Kontakis et al.21 | 134 deltoids* | The vertical distance from the anterior upper border of the deltoid to the axillary nerve where it enters the deltoid muscle anteriorly was mean 4.5 (SD 1.2) cm. |
| Duparc et al.22 | 12 shoulders | The distance between the insertion of the deltoid muscle and the axillary nerve where it enters the deltoid muscle was mean 3.4 (range 3.0–4.8) cm. |
SD = standard deviation.
Median age of patients 63 (range 18–84) yr.
Discussion
Physeal fractures of the proximal humerus account for 0.45% of all pediatric fractures.23 Neer and Horowitz24 have classified these fractures from grades I to IV according to the severity of displacement: grade I refers to displacement of less than 5 mm shaft diameter; grade II is less than one-third; grade III is two-thirds; and grade IV is greater than two-thirds. Salter–Harris type I physeal fractures occur primarily in neonates and children younger than 5. Children aged between 5 and 11 primarily have metaphyseal fractures, whereas those older than 11 have Salter–Harris type II injuries.7,11–13 In our study, 14 of the 16 adolescent patients suffered a Salter–Harris type II fracture.
Traditionally, pediatric proximal humerus fractures have been treated nonoperatively. This is because roughly 80% of the longitudinal growth of the humerus occurs at the proximal humerus; therefore, there is great potential for remodelling at this site. Furthermore, the large arc of motion of this joint can compensate for a large degree of malunion and angulation. Clinical studies have confirmed this approach.6,8,11,12,25–28 However, these studies have comprised mainly younger patients and have included few older adolescent patients (≥ 15 yr). Studies that have evaluated the subset of older patients (≥ 14 yr) who have healed with a Neer III or IV grade of displacement, have found that these patients suffer more subjective symptoms and have more stiffness.7 This has led to some authors advocating surgical treatment of this subset of pediatric or adolescent patients to improve their long-term clinical outcome.6,7,9,29
Proximal humerus fractures in adolescents have to be distinguished from those in adults because of the location and angle of the fracture line. Adolescents suffer Salter–Harris type II fractures, which entail a more proximal fracture line with a steeper angle compared with fractures in adults. This translates into a different pin configuration as well as a different reduction manoeuvre. Based on our modelling scheme, we suggest that 2 parallel pins may be placed at about 4.5 cm and 8.0 cm from the top of the humeral head at a trajectory of 20°. We recognize that this is one of many pin configurations. The goal with each of these pin patterns is to optimize the amount of fixation in the humeral shaft and humeral head while optimizing the trajectory at which the fracture line is crossed.
Study limitations and strengths
In an effort to determine the ideal pin site entry and trajectory, we used MRI scans of nonfractured adolescent shoulders to measure important anatomic parameters. Next, we used this information to construct computer-generated 3-D models of the nonfractured shoulder. The anatomy of the nonfractured adolescent shoulder has been based on data collected from 6 MRI scans of nonfractured shoulders. Ideally, one would like to use more specimens; however, shoulder MRI is not frequently performed in this age group. Furthermore, there are not many cadaveric specimens in this age group. However, this is the only study that has outlined anatomy of the nonfractured adolescent shoulder.
To characterize the fracture geometry, we reviewed the radiographs of all patients who had their fractures treated with percutaneous pining at our institution. We combined this information with the 3-D models to evaluate various pin configurations. There are many different approaches to modelling of the placement of pins and each of them has certain drawbacks. This is the first study that has tried to determine the ideal entry site and trajectory of pins in shoulders of adolescents.
Lastly, pin placement also requires consideration of the surrounding neurovascular structures. Unfortunately, the position of the axillary artery and axillary nerve were not measured on the MRI scans.
Footnotes
Competing interests: None declared.
Contributors: Drs. R. Mehin, Wickham and Letts designed the study and reviewed the article. Dr. R. Mehin acquired the data, which Mr. A. Mehin analyzed; together, they wrote the article. All authors gave final approval for publication.
References
- 1.Jaberg H, Warner JJ, Jakob RP. Percutaneous stabilization of unstable fractures of the humerus. J Bone Joint Surg Am. 1992;74:508–15. [PubMed] [Google Scholar]
- 2.Herscovici D, Jr, Saunders DT, Johnson MP, et al. Percutaneous fixation of proximal humeral fractures. Clin Orthop Relat Res. 2000;375:97–104. doi: 10.1097/00003086-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Williams GR, Jr, Wong KL. Two-part and three-part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin North Am. 2000;31:1–21. doi: 10.1016/s0030-5898(05)70124-3. [DOI] [PubMed] [Google Scholar]
- 4.Chen CY, Chao EK, Tu YK, et al. Closed management and percutaneous fixation of unstable proximal humerus fractures. J Trauma. 1998;45:1039–45. doi: 10.1097/00005373-199812000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Kocialkowski A, Wallace WA. Closed percutaneous K-wire stabilization for displaced fractures of the surgical neck of the humerus. Injury. 1990;21:209–12. doi: 10.1016/0020-1383(90)90003-d. [DOI] [PubMed] [Google Scholar]
- 6.Curtis RJ., Jr Operative management of children’s fractures of the shoulder region. Orthop Clin North Am. 1990;21:315–24. [PubMed] [Google Scholar]
- 7.Dobbs MB, Luhmann SL, Gordon JE, et al. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003;23:208–15. [PubMed] [Google Scholar]
- 8.Larsen CF, Kiaer T, Lindequist S. Fractures of the proximal humerus in children. Nine-year follow-up of 64 unoperated on cases. Acta Orthop Scand. 1990;61:255–7. doi: 10.3109/17453679008993512. [DOI] [PubMed] [Google Scholar]
- 9.Schwendenwein E, Hajdu S, Gaebler C, et al. Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg. 2004;14:51–5. doi: 10.1055/s-2004-815781. [DOI] [PubMed] [Google Scholar]
- 10.Beringer DC, Weiner DS, Noble JS, et al. Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop. 1998;18:31–7. [PubMed] [Google Scholar]
- 11.Smith FM. Fracture-separation of the proximal humeral epiphysis; a study of cases seen at the Presbyterian Hospital from 1929–1953. Am J Surg. 1956;91:627–35. doi: 10.1016/0002-9610(56)90296-3. [DOI] [PubMed] [Google Scholar]
- 12.Baxter MP, Wiley JJ. Fractures of the proximal humeral epiphysis. Their influence on humeral growth. J Bone Joint Surg Br. 1986;68:570–3. doi: 10.1302/0301-620X.68B4.3733832. [DOI] [PubMed] [Google Scholar]
- 13.Bishop JY, Flatow EL. Pediatric shoulder trauma. Clin Orthop Relat Res. 2005;432:41–8. doi: 10.1097/01.blo.0000156005.01503.43<. [DOI] [PubMed] [Google Scholar]
- 14.Boileau P, Walch G. The three-dimensional geometry of the proximal humerus. Implications for surgical technique and prosthetic design. J Bone Joint Surg Br. 1997;79:857–65. doi: 10.1302/0301-620x.79b5.7579. [DOI] [PubMed] [Google Scholar]
- 15.Iannotti JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491–500. [PubMed] [Google Scholar]
- 16.Pearl ML, Kurutz S. Geometric analysis of commonly used prosthetic systems for proximal humeral replacement. J Bone Joint Surg Am. 1999;81:660–71. doi: 10.2106/00004623-199905000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Joint Surg Am. 2001;83:1695–9. doi: 10.2106/00004623-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Naidu SH, Bixler B, Capo JT, et al. Percutaneous pinning of proximal humerus fractures: a biomechanical study. Orthopedics. 1997;20:1073–6. doi: 10.3928/0147-7447-19971101-13. [DOI] [PubMed] [Google Scholar]
- 19.Jiang C, Zhu Y, Wang M, et al. Biomechanical comparison of different pin configurations during percutaneous pinning for the treatment of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16:235–9. doi: 10.1016/j.jse.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Cetik O, Uslu M, Acar HI, et al. Is there a safe area for the axillary nerve in the deltoid muscle? A cadaveric study. J Bone Joint Surg Am. 2006;88:2395–9. doi: 10.2106/JBJS.E.01375. [DOI] [PubMed] [Google Scholar]
- 21.Kontakis GM, Steriopoulos K, Damilakis J, et al. The position of the axillary nerve in the deltoid muscle. A cadaveric study. Acta Orthop Scand. 1999;70:9–11. doi: 10.3109/17453679909000948. [DOI] [PubMed] [Google Scholar]
- 22.Duparc F, Bocquet G, Simonet J, et al. Anatomical basis of the variable aspects of injuries of the axillary nerve (excluding the terminal branches in the deltoid muscle) Surg Radiol Anat. 1997;19:127–32. doi: 10.1007/BF01627959. [DOI] [PubMed] [Google Scholar]
- 23.Rose SH, Melton LJ, III, Morrey BF, et al. Epidemiologic features of humeral fractures. Clin Orthop Relat Res. 1982;168:24–30. [PubMed] [Google Scholar]
- 24.Neer CS, II, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24–31. [PubMed] [Google Scholar]
- 25.Dameron TB, Jr, Reibel DB. Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am. 1969;51:289–97. [PubMed] [Google Scholar]
- 26.McBride ED, Sisler J. Fractures of the proximal humeral epiphysis and the juxta-epiphysial humeral shaft. Clin Orthop Relat Res. 1965;38:143–53. [PubMed] [Google Scholar]
- 27.Kohler R, Trillaud JM. Fracture and fracture separation of the proximal humerus in children: report of 136 cases. J Pediatr Orthop. 1983;3:326–32. doi: 10.1097/01241398-198307000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Sherk HH, Probst C. Fractures of the proximal humeral epiphysis. Orthop Clin North Am. 1975;6:401–13. [PubMed] [Google Scholar]
- 29.Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA, et al. Fractures of the proximal humeral epiphysis. Int Orthop. 1993;17:16–9. doi: 10.1007/BF00195216. [DOI] [PubMed] [Google Scholar]