Peutz–Jegher syndrome (PJS) is a rare autosomal dominant disorder characterized by typical pigmented perioral macules, pigmented spots in the buccal mucosa and digits along with hamartomatous polyps in the gastrointestinal tract.1 The characteristic clinical course includes recurrent episodes of polyp-induced bowel obstruction, abdominal pain and gastrointestinal bleeding.
In addition to polyposis, the risk of gastrointestinal and extra-gastrointestinal malignancies is significantly increased in patients with PJS. The relative risk of dying from a gastrointestinal cancer is 13 times greater in patients with PJS than in patients without the condition. The risk of other cancers, especially of the reproductive organs, breasts, pancreas and lungs is 9 times greater among these patients than the general population.2 The Johns Hopkins University reported a 48% incidence of cancer, with 73% of these arising in the gastrointestinal tract.1 However, the occurrence of jejunal carcinoma is very rare. We present the unusual case of a patient with PJS and carcinoma of the jejunum.
Case report
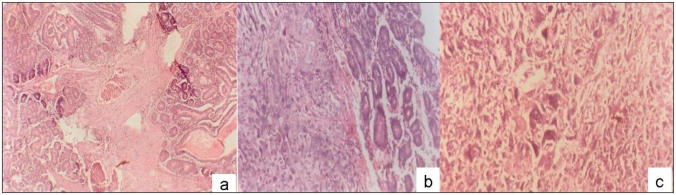
A 22-year-old man presented with repeated episodes of intestinal obstruction and had 30 cm of jejunum with 5 polyps and a 40-cm large intestine with 4 polyps removed surgically. The largest polyp was 5 cm in diameter. In addition, there was a large, pale creamy, necrotic and friable mass measuring 8 × 5 × 4 cm projecting into the lumen of the jejunum with mucosal ulceration. Mesenteric lymph nodes were also present. Microscopically, the polyps showed a Christmas-tree appearance with arborizing musculature and hyperplastic glands suggestive of hamartomatous polyps (Fig. 1A). The sections from the jejunal mass showed features of a poorly differentiated carcinoma with metastasis in 5 mesenteric lymph nodes (Fig. 1B and C). In retrospect, we found that the patient had mucocutaneous melanosis of the palms, soles and perioral region.
Fig. 1.
(A) Low-power view of a hamartomatous polyp showing arborizing musculature and hyperplastic glands (hematoxylin and eosin stain, original magnification ×100). (B) Low- and (C) high-power views of poorly differentiated carcinoma involving the jejunum (hematoxylin and eosin stains, original magnifications ×100 and ×400, respectively).
Discussion
PJS is a rare disease with an incidence of about 1 in 8300–29 000 live births. The hallmarks of PJS are multiple hamartomatous polyps of the gastrointestinal tract. Most of these are found in the small intestine, but they may also be found in the stomach and large intestine. The most distinctive clinical feature is melanosis of the lips, buccal mucosa and digits, which usually develops from infancy through childhood and often fades with age. Some patients may not show the full spectrum of the disease.
The diagnostic criteria for PJS proposed by Giardello and colleagues3 requires histopathological confirmation of hamartomatous gastrointestinal polyps and 2 of the following features: small bowel polyposis, family history and pigmented skin and/or mucosal brown macules. In our patient’s case, the polyps were hamartomatous and were present in the jejunum and large intestine. He had typical mucocutaneous pigmentation, although there was no family history of this condition. However, 50% of cases could be sporadic and may represent new mutations.4
Our patient also had a large, poorly differentiated adenocarcinoma in the jejunum. Although hamartomatous polyps commonly involve the jejunum, the colon is the most common site for gastrointestinal cancer in patients with PJS. The incidence of adenomatous and carcinomatous transformation in hamartomatous polyps is about 6%–12%. Carcinoma of the jejunum is rare.
Mehta and colleagues5 reported the case of a 25-year-old man with PJS in whom small intestinal adenocarcinoma developed. He presented with small bowel obstruction owing to jejuno-ileal intussuception.
A germline mutation in STK11, a tumour suppressor gene localized to chromosome 19p13.2–13.3, encodes a serine-threonine kinase enzyme involved in growth control regulation, which can occur sporadically with or can be inherited in an autosomal dominant pattern. The gene affects both sexes equally, with a 50% chance of PJS developing.
Recently, intraoperative endoscopy and endoscopic polypectomy, rather than segmental resections of the bowel, have been recommended for PJS polyps. Upper and lower gastrointestinal endoscopic surveillance for polyps or gastrointestinal cancer is recommended every 1–2 years from the age of 25 years.6
In PJS, hamartomatous polyps commonly involve the jejunum, but carcinoma of jejunum is distinctly rare. Our patient’s case demonstrates one of the rare sites for carcinomas in patients with PJS.
Footnotes
This case report was presented at APCON 2006, held Dec. 4–9, 2006, in Bangalore, India.
Competing interests: None declared.
References
- 1.Fenoglio-Preiser C, Lantz PE, Listrom MB, et al. Gastrointestinal pathology An atlas and text. 2nd ed. Philadelphia (PA): Lippincott - Raven publishers; 1999. Polyposis syndromes; pp. 717–45. [Google Scholar]
- 2.Spigelman AD, Murday V, Phillips RK. Cancer and the Peutz-Jeghers syndrome. Gut. 1989;30:1588–90. doi: 10.1136/gut.30.11.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giardiello FM, Welsh SB, Hamilton SR, et al. Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med. 1987;316:1511–4. doi: 10.1056/NEJM198706113162404. [DOI] [PubMed] [Google Scholar]
- 4.Kuramoto S, Kobayashi K, Mimura T. [Peutz-Jeghers syndrome] [Article in Japanese] Nippon Rinsho. 1994;(Suppl 6):49–52. [PubMed] [Google Scholar]
- 5.Mehta MV, Porecha MM, Mehta PJ. Small intestinal adenocarcinoma in Peutz-Jeghers syndrome. Indian J Gastroenterol. 2006;25:38–9. [PubMed] [Google Scholar]
- 6.Dunlop MG. Guidance on gastrointestinal surveillance for hereditary non-polyposis colorectal cancer, familial adenomatous polyposis, juvenile polyposis and Peutz-Jeghers syndrome. Gut. 2002;51(Suppl 5):V21–7. doi: 10.1136/gut.51.suppl_5.v21. [DOI] [PMC free article] [PubMed] [Google Scholar]