Abstract
Background:
Vision loss after spinal surgery is a rare and devastating complication. Risk factors include patient age, operative time, estimated blood loss, and intraoperative fluid management. Children with spinal cord injury often develop scoliosis that requires surgical correction.
Study Design:
Case report.
Methods:
Clinical and radiographic review was conducted of a 15-year-old boy who developed severe scoliosis after sustaining a C5 level injury at age 4 years from a motor vehicle crash.
Findings:
The patient underwent a posterior spinal fusion from T2 to the pelvis, and good correction of the spinal deformity was attained. During the 8-hour procedure, blood loss was 4,000 mL (approximately 1.2 blood volumes) and 17,000 mL of fluids were administered. On postoperative day 5, it was determined that the patient had complete visual loss. Neuro-ophthalmology consultation confirmed the diagnosis of posterior ischemic optic neuropathy.
Conclusions:
A significant number of children with spinal cord injury develop scoliosis requiring surgical correction. These procedures are often lengthy, with the potential for extensive blood loss and fluid shifts, factors that may increase the likelihood of postoperative vision loss. Patients should be counseled about this complication, and the surgical and anesthesiology teams should take all measures to minimize its occurrence.
Keywords: Blindness; Scoliosis; Spinal cord injuries; Spinal fusion; Neuropathy, optic, ischemic, posterior
INTRODUCTION
Skeletally immature children with paralysis secondary to spinal cord injury (SCI) are at a high risk for developing scoliosis. This spinal curvature may be due to a variety of factors, including asymmetric truncal weakness, injury to growth plates leading to asymmetric growth, postlaminectomy deformity, and chronic instability at the site of the injury (1). The incidence of scoliosis is close to 100% in children who sustain SCI before puberty (1,2). Typically, many of these children will develop a long C-shaped neuromuscular scoliosis, often requiring spinal fusion from the upper thoracic spine to the pelvis (3). These procedures are often lengthy and result in extensive blood loss (4), and patients can experience a significant number of perioperative complications (5).
Vision loss after spine surgery, first described by Hollenhorst and colleagues in 1954 (6), is a rare and devastating complication. Several more recent reports have attempted to establish the incidence of vision loss after spine surgery (7–11). Patil and colleagues (7) conducted a national population-based study of visual complications after spine surgery. Using ICD-9 codes, they identified 4,728,815 patients who had undergone spine surgery in the USA from 1993 to 2002. The incidence of postoperative visual loss in these patients was 0.087% (4,134 patients). In 2007, Baig and colleagues (8) performed an extensive review of the literature on visual loss after spine surgery and determined an incidence ranging from 0.028% to 0.2%. Chang and colleagues (9) reviewed the experience at Johns Hopkins Hospital and identified 4 patients with vision loss out of 14,102, for an incidence of 0.03%.
Spine surgery has replaced cardiac surgery as the leading cause of postoperative blindness (9,11). Risk factors include intraoperative anemia, hypotension, significant intraoperative hydration, and lengthy procedure (7–9,12), all of which are not infrequently encountered during spinal surgery for scoliosis in children with SCI.
In this report, we describe a 15-year-old boy with a C5 level SCI who suffered postoperative vision loss after a posterior spinal fusion. We discuss the potential pathophysiologic mechanisms and propose recommendations for minimizing the incidence of this occurrence.
CASE REPORT
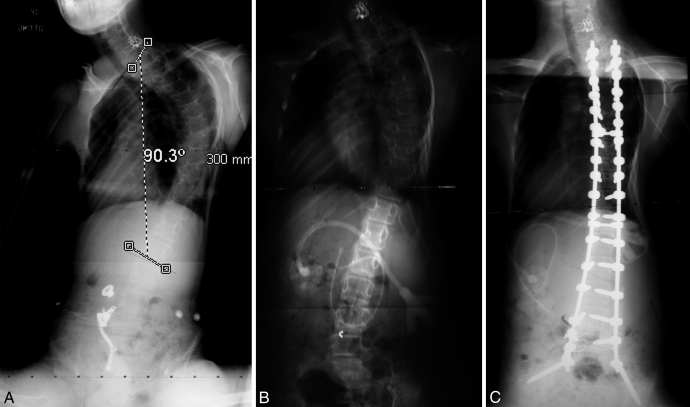
A 15-year-old boy developed a scoliosis measuring 90° after an ASIA A C5 level injury at age 4 years. Because of his poor sitting balance (Figure 1A) and the progressive nature of the curve, the decision was made to proceed with surgical correction. He was admitted to the hospital and placed in halo gravity traction for 8 weeks, where his curve decreased from 90° to 47°. He also underwent placement of a gastrostomy tube, and his weight increased from 65 to 82 pounds. Once maximal correction had been attained with traction (Figure 1B), he underwent a posterior spinal fusion from T2 to the pelvis.
Figure 1.
(A) Preoperative posteroanterior radiograph demonstrating a severe scoliosis measuring 90° from T1 to L2. (B) Post-traction film showing correction to 47°. (C) Postoperative radiograph showing curve correction after posterior spinal fusion from T2 to the pelvis.
Surgery
After intubation, femoral pins were placed to facilitate intraoperative halo-femoral traction as previously described (13). After positioning, the patient underwent exposure and pedicle screw instrumentation of his spine from T2 to the pelvis (Figure 1C). His blood pressure demonstrated variability throughout the procedure, ranging from a systolic of 70 to 125 mmHg. Preoperatively, his hemoglobin was 13.2 g/dL. At one point intraoperatively, his hemoglobin was 6.4 g/dL, at which time he was resuscitated with packed red blood cells. Upon admission to the intensive care unit, his hemoglobin was 11.6 g/dL. In addition, blood loss totaled 4,000 mL over an operating time of 479 minutes. He received a total of 17,280 mL of intraoperative fluids, including crystalloid (14,700 mL), 6 units of packed red blood cells (2,100 mL), and 2 units of fresh frozen plasma (480 mL). During the last 30 minutes of the procedure, the anesthesia team alerted the surgeons of difficulty in ventilating the patient due to high peak airway pressures. The surgery was completed, and the patient was taken to the intensive care unit.
Postoperative Course
In the intensive care unit, the patient required pressors and systemic diuresis, along with 3 units of packed red blood cells. Initially, the main concern was pulmonary function, and he remained intubated and sedated. With respect to motor function and cognition, he appeared to be at his neurologic baseline. On postoperative day 5 as he was extubated and his sedation decreased, he stated his inability to see. Neurology and ophthalmology consults were obtained, and he was diagnosed with posterior optic ischemic neuropathy.
At the 6-month follow-up visit, he reported partial return of vision with respect to differentiation of light and dark and peripheral vision. He demonstrated light perception with a pupillary response. He was able to discern shapes at short distances (<3 feet). He continues with neuro-ophthalmology follow up.
DISCUSSION
This child with SCI underwent a posterior spinal fusion and sustained postoperative vision loss. The surgical correction of scoliosis in these children requires lengthy, complex procedures, and practitioners should be aware of the potential for this dire complication.
Vision loss is a rare complication encountered after spinal surgery; there are 4 main etiologies (7,8,12,14). First, external ocular injury can occur with a corneal or scleral abrasion. Next, cortical blindness can occur from a vascular insult to the visual cortex or tracts. This is suspected in patients with normal papillary reflexes and is established by magnetic resonance imaging. Central retinal artery occlusion secondary to direct pressure on the globe often presents as unilateral vision loss with signs of periorbital swelling. Lee and colleagues (15) reported on 10 patients with central retinal artery occlusion and reported none in patients who were placed in cranial pins, because this floats the eyes. Because our patient was in a halo intraoperatively, direct global pressure is unlikely to be a major contributor to his visual loss. The most common cause of visual deficits after spine surgery is ischemic optic neuropathy, which results from decreased perfusion pressure of the optic nerve head (16,17). This is further subdivided into anterior and posterior, depending on the location of the insult on the optic nerve. The posterior variant is more common than anterior, possibly because the posterior optic nerve derives its blood supply from small end vessels from the ophthalmic artery, which lack autoregulatory control, making them vulnerable to anemia and hypotension (14,15).
Risk factors for the development of vision loss after spine surgery include lengthy procedure, intraoperative anemia and hypotension, and infusion of large amounts of crystalloid (7,8). Our patient met the criteria for all 3 of these risk factors. The length of the procedure was approximately 8 hours, which increases the risk of postoperative vision loss. Intraoperative anemia and hypotension were aggressively managed. The estimated blood loss was 4,000 mL, and episodes when the hemoglobin value was less than 10 g/dL or mean arterial blood pressure was less than 60 mmHg did occur. Last, our patient received 14,700 mL of crystalloid, another risk factor for postoperative vision loss.
Many of these risk factors are present in a significant percentage of children with SCI undergoing surgical correction of their scoliosis, the majority of whom do not develop postoperative vision loss. Thus, it is likely that a multitude of factors, some known and some not yet known, contribute to the development of this complication in a small subset of these patients. In any event, all patients and their parents should be counseled on the potential occurrence of this complication. This is now routinely listed on our preoperative consent forms.
CONCLUSION
Intraoperatively, hypotension and anemia must be aggressively managed with the avoidance of large amounts of crystalloid, when patient hemodynamics allow. In addition, patient positioning in 10° of reverse Trendelenberg during prone surgery should be considered to avoid venous congestion. The surgical team should consider staging procedures likely to extend beyond 8 hours, with the understanding that this is a multifactorial decision that needs to be tailored for each patient. Postoperatively, physicians and nursing staff should document a good visual examination. An urgent ophthalmology consultation is indicated for any suspicion of postoperative vision loss.
REFERENCES
- Dearolf WW, 3rd, Betz RR, Vogel LC.Effectiveness of spinal release and halo-femoral traction in the management of severe spinal deformity J Pediatr Orthop 1990102214–218.2312704 [Google Scholar]
- Mehta S, Betz RR, Mulcahey MJ. Effect of bracing on paralytic scoliosis secondary to spinal cord injury. J Spinal Cord Med. 2004;27(suppl 1):S88–S92. doi: 10.1080/10790268.2004.11753448. [DOI] [PubMed] [Google Scholar]
- Tsirikos AI, Lipton G, Chang WN, Dabney KW, Miller F. Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine. 2008;33(10):1133–1140. doi: 10.1097/BRS.0b013e31816f63cf. [DOI] [PubMed] [Google Scholar]
- Samdani AF, Torre-Healy A, Asghar J, Herlich AM, Betz RR. Strategies to reduce blood loss during posterior spinal fusion for neuromuscular scoliosis: a review of current techniques and experience with a unique bipolar electrocautery device. Surg Technol Internat. 2008;17:243–248. [PubMed] [Google Scholar]
- Mohamad F, Parent S, Pawelek J. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop. 2007;27(4):392–397. doi: 10.1097/01.bpb.0000271321.10869.98. [DOI] [PubMed] [Google Scholar]
- Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical operations. AMA Arch Ophthalmol. 1954;52(6):819–830. doi: 10.1001/archopht.1954.00920050825002. [DOI] [PubMed] [Google Scholar]
- Patil CG, Lad EM, Lad SP, Ho C, Boakye M. Vision loss after spine surgery: a population-based study. Spine. 2008;33(13):1491–1496. doi: 10.1097/BRS.0b013e318175d1bf. [DOI] [PubMed] [Google Scholar]
- Baig MN, Lubow M, Immesoete P. Vision loss after spine surgery: review of the literature and recommendations. Neursurg Focus. 2007;23(5):E15. doi: 10.3171/FOC-07/11/15. [DOI] [PubMed] [Google Scholar]
- Chang SH, Miller NR. The incidence of vision loss due to perioperative ischemic optic neuropathy associated with spine surgery: the Johns Hopkins Hospital experience. Spine. 2005;30(11):1299–1302. doi: 10.1097/01.brs.0000163884.11476.25. [DOI] [PubMed] [Google Scholar]
- Warner MA. Postoperative visual loss: experts, data, and practice. Anesthesiology. 2006;105(4):641–642. doi: 10.1097/00000542-200610000-00002. [DOI] [PubMed] [Google Scholar]
- Roth S, Barach P. Postoperative visual loss: still no answers—yet. Anesthesiology. 2001;95(3):575–577. doi: 10.1097/00000542-200109000-00006. [DOI] [PubMed] [Google Scholar]
- Farag E, Doyle DJ. Vision loss after spine surgery: a new hypothesis. Can J Anesthesiol. 2006;53(4):420. doi: 10.1007/BF03022516. [DOI] [PubMed] [Google Scholar]
- Mehlman CT, Al-Sayyad MJ, Crawford AH. Effectiveness of spinal release and halo-femoral traction in the management of severe spinal deformity. J Pediatr Orthop. 2004;24(6):667–673. doi: 10.1097/00004694-200411000-00014. [DOI] [PubMed] [Google Scholar]
- Stevens WR, Glazer PA, Kelley SD, Lietman TM, Bradford DS. Ophthalmic complications after spinal surgery. Spine. 1997;22(12):1319–1324. doi: 10.1097/00007632-199706150-00008. [DOI] [PubMed] [Google Scholar]
- Lee LA, Roth S, Posner KL. The American Society of Anesthesiologists Postoperative Visual Loss Registry: analysis of 93 spine surgery cases with postoperative visual loss. Anesthesiology. 2006;105(4):652–659. doi: 10.1097/00000542-200610000-00007. [DOI] [PubMed] [Google Scholar]
- Murphy MA. Bilateral posterior ischemic optic neuropathy after lumbar spine surgery. Ophthalmology. 2003;110(7):1454–1457. doi: 10.1016/S0161-6420(03)00480-9. [DOI] [PubMed] [Google Scholar]
- Williams EL. Postoperative blindness. Anesthesiol Clin North Am. 2002;20(3):605–622. doi: 10.1016/s0889-8537(02)00007-x. [DOI] [PubMed] [Google Scholar]