Abstract
Purpose:
We systematically reviewed randomized and quasi-randomized clinical trials in the literature to assess the efficacy of neck stabilization and postural exercises on pain, neck range of motion, and time off work in adults with acute whiplash-associated disorders.
Methods:
Electronic databases, reference lists of relevant Cochrane reviews, reference lists of studies selected for inclusion, and tables of contents of relevant journals were systematically searched for randomized and quasi-randomized controlled trials. Two independent reviewers selected studies for inclusion, assessed methodological quality, and extracted data. Because of the heterogeneity of the interventions, a qualitative synthesis was performed using “levels of evidence” as recommended by van Tulder et al.
Results:
Eight studies representing five clinical trials were selected for inclusion. Two trials were graded as high quality, two as moderate quality, and one as low quality. Many of these studies had mixed results, demonstrating significant differences on some outcome measures but not on others.
Conclusions:
There is moderate evidence to support the use of postural exercises for decreasing pain and time off work in the treatment of patients with acute whiplash-associated disorders. However, no evidence exists to support the use of postural exercises for increasing neck range of motion. There is conflicting evidence in support of neck stabilization exercises in the treatment of patients with acute whiplash-associated disorders.
Keywords: exercise, motor vehicle accident, neck stabilization, posture, systematic review, whiplash
RÉSUMÉ
Objet :
Nous avons examiné systématiquement les essais cliniques aléatoires ou quasi aléatoires dans la documentation afin d’évaluer l’efficacité de la stabilisation cervicale et des exercices posturaux sur la douleur, l’amplitude articulaire cervicale et le temps de congé du travail chez les adultes atteints de troubles aigus associés au coup de fouet cervical.
Méthodologie :
Les bases de données électroniques, les listes de référence des examens pertinents de Cochrane, les listes de référence des études choisies pour l’inclusion ainsi que les tables des matières des revues scientifiques pertinentes ont fait l’objet de recherches méthodiques pour des essais cliniques aléatoires et quasi aléatoires contrôlés. Deux évaluateurs indépendants ont choisi des études pour leur inclusion, en ont évalué la qualité méthodologique et extrait les données. En raison de l’hétérogénéité des interventions, une synthèse qualitative a été effectuée à l’aide des « niveaux de preuves scientifiques », tel que recommandé par van Tulder et coll.
Résultats :
Huit études représentant cinq essais cliniques ont été choisies pour leur inclusion. Deux essais ont été classés comme étant de haute qualité, deux de qualité moyenne et un de qualité faible. Bon nombre de ces études avaient des résultats mixtes où des différences significatives étaient démontrées dans certaines mesures d'impact mais pas dans d’autres.
Conclusion :
Des preuves scientifiques modérées soutiennent l’utilisation d’exercices posturaux pour diminuer la douleur et le temps de congé du travail dans le traitement des patients atteints de troubles aigus associés au coup de fouet cervical. Cependant, aucune preuve scientifique ne soutient l’utilisation d’exercices posturaux pour augmenter l’amplitude articulaire cervicale. On fait état de preuves contradictoires dans le soutien des exercices de stabilisation cervicale pour le traitement des patients atteints de troubles aigus associés au coup de fouet cervical.
Mots clés: exercice, accident d’automobile, stabilisation cervicale, posture, étude méthodique, coup de fouet cervical
BACKGROUND
In 1995, the Quebec Task Force on Whiplash-Associated Disorders1 developed a definition of whiplash that has been widely adopted in the literature:
Whiplash is an acceleration–deceleration mechanism of energy transfer to the neck. It may result from rear-end or side-impact motor vehicle collisions, but can also occur during diving or other mishaps. The impact can result in bony or soft-tissue injuries, which in turn may lead to a variety of clinical manifestations (whiplash-associated disorders).
Whiplash is the most common type of injury in motor vehicle accidents (MVAs); the Insurance Corporation of British Columbia (ICBC) estimates that soft-tissue neck and back injuries account for approximately 60% of all bodily injury claims (J. Gane, personal communication, 9 May 2007). In 2007, it was estimated that whiplash-associated disorders (WAD) cost ICBC policyholders more than $600 million per year (J. Gane, personal communication, 9 May 2007).
The Quebec Task Force1 also developed a classification system to assign grades to WAD. Grade 0 implies no complaints and no physical signs of injury to the neck. Grade 1 includes complaints of neck pain, stiffness, or tenderness only, with no physical signs. Grade 2 describes a patient with a neck complaint as well as musculoskeletal signs that include decreased range of motion (ROM) and point tenderness. Grade 3 implies a neck complaint with neurological signs. Grade 4 is a neck complaint with a fracture or dislocation. A person with whiplash for more than 45 days is approaching chronicity, and at 6 months the person is deemed to have chronic whiplash.1
Symptoms of WAD can vary from one individual to another. They can include, but are not limited to, neck pain, neck stiffness, headaches, shoulder pain, arm pain/numbness, paraesthesias, weakness, dysphagia, visual disturbances, auditory symptoms, dizziness, cognitive disturbances, and jaw pain.1–3 These symptoms can vary in severity and can result in disability.
There is weak and inconsistent evidence available to support theories about the pathophysiology of whiplash.2 Conclusive evidence can be drawn from post-mortem studies; however, the injuries investigated in these studies are usually quite severe2 and are not representative of typical whiplash injuries, of which 90% are grades 1 and 2.3 It has been proposed that whiplash is a “systemic illness” with symptoms arising from pathology, psychological response, and social context;3 it is a complex injury with considerable variation in presentation and progression.
Ligaments contribute to 20% of neck stability, mostly in the end range of movement, and the damage they sustain is unclear in whiplash injuries below grade 4.4 Neck musculature accounts for the remaining 80% of stability and is primarily active through midrange, which corresponds to the range used for most functional activities.4 Dysfunction of the neck-stabilizing muscles after whiplash injury has been documented in the literature.5
There are many different treatment options for whiplash injury, with varying degrees of evidence to support them. These include exercise therapy, neck collars, prescribed rest, manipulation, mobilization, postural advice, traction, electrotherapies, local heat/ice, ultrasound, massage, surgical intervention, steroid injections, and pharmacology.1,6
Clinical practice guidelines from the Netherlands and British Columbia have summarized the available evidence to provide recommendations for the physiotherapy treatment of WAD.7,8 The Dutch “best treatment standards” include education, exercise, gradual return to activity and participation, and encouraging patients to take responsibility for their therapy.7 The British Columbia guidelines build and expand on the Dutch guidelines and focus on education, therapeutic exercise, manual therapy, and early return to activity.8 Because exercise is a common theme in current best practice, a systematic review on the effects of exercise on WAD was necessary.
RATIONALE AND REVIEW QUESTION
Treatment of adults with acute WAD is an area of interest because of the high incidence of WAD and the high compensation costs to victims.1 Dysfunction of the neck-stabilizing muscles after whiplash injury is common,5 as is postural dysfunction.9 Physiotherapists commonly treat these problems with neck-stabilization exercises (e.g., strengthening exercises for the deep cervical flexors) and postural exercises (e.g., stretches to lengthen tight sub-occipital muscles).9 We have defined neck stabilization as any exercise that strengthens the muscles surrounding the neck, whereas postural exercises include any correction, exercise, or advice with the aim of improving posture.
Two Cochrane reviews on topics related to WAD and treatment of WAD were identified.6,10 The quality of these reviews was assessed by two independent reviewers, using a seven-point scale adapted from Oxman et al.,11 which is included in the Appendix. Our interrater agreement in assessing these reviews was 85.7%. The review by Kay et al.6 received 7/7, while the review by Verhagen et al.10 scored 5/7, indicating that these are both high-quality reviews. Kay et al.6 examined the effects of exercise in the treatment of patients with mechanical neck disorders including, but not limited to, WAD, whereas Verhagen et al.10 reviewed the effects of all conservative treatments, including heat, ice, collars, ultrasound, traction, massage, electrotherapies, and exercise. Both reviews included studies that used multimodal treatments rather than limiting included studies to those examining the effects of exercise alone. As neither review looked specifically at the effects of exercise in the treatment of patients with WAD, we determined that there was a need for a systematic review to elucidate the specific effects of exercise in the treatment of WAD. In particular, there is a need for a review examining the effects of neck stabilization and postural exercises in the treatment of WAD, as these interventions are commonly employed by physiotherapists.9
Therefore, our purpose was to systematically review randomized and quasi-randomized clinical trials reported in the literature to answer the following focused question: In adults with acute WAD, do neck stabilization and postural exercises have an effect on pain, ROM, and time off work?
METHODS
We searched the following databases from their originating dates to 15 March 2007, using relevant MeSH terms and key words: MEDLINE, EMBASE, CINAHL, PEDro, the Cochrane Database of Systematic Reviews, the Cochrane Central Registry of Controlled Trials, and the National Research Register. The search strategy used for MEDLINE, including MeSH terms and key words, is detailed in Table 1. Where possible, we limited our electronic searches to humans and to studies published in English.
Table 1.
MEDLINE Search Strategy
| 1. whiplash injuries/ | 18. whiplash.mp. | 36. cervicalgia.mp. |
| 2. neck injuries/ | 19. whiplash associated disorder$.mp. | 37. cervicodynia.mp. |
| 3. exp cervical vertebrae/ | 20. WAD.mp. | 38. range of motion.mp. |
| 4. “sprains and strains”/ | 21. neck injur$.mp. | 39. ROM.mp. |
| 5. neck muscles/ | 22. neck hyperextension.mp. | 40. goniomet$.mp. |
| 6. or/1-5 | 23. neck hyperflexion.mp. | 41. return to work.mp. |
| 7. exercise/ | 24. cervical.mp. | 42. re-entry.mp. |
| 8. exercise therapy/ | 25. neck sprain.mp. | 43. reentry.mp. |
| 9. posture/ | 26. neck strain.mp. | 44. leave.mp. |
| 10. or/7-9 | 27. neck muscle$.mp. | 45. absen$.mp. |
| 11. pain/ | 28. or/18-27 | 46. illness day.mp. |
| 12. neck pain/ | 29. exercise$.mp. | 47. sick day.mp. |
| 13. “range of motion, articular”/ | 30. postur$.mp. | 48. time loss.mp. |
| 14. sick leave/ | 31. stabili$.mp. | 49. day loss.mp. |
| 15. absenteeism/ | 32. or/29-31 | 50. or/33-49 |
| 16. or/11-15 | 33. pain.mp. | 51. 28 and 32 and 50 |
| 17. 6 and 10 and 16 | 34. ache.mp. | 52. 17 or 51 |
| 35. neckache.mp. | 53. limit 52 to (humans and English language) |
Titles retrieved from our electronic database search were independently screened for exclusion by two of the first five authors (interrater agreement = 89.1%). A title was excluded if it was published in a language other than English; identified the study as a survey or case study; indicated that the study examined injury to a body part other than the neck; indicated that the study population did not include neck injuries sustained in an MVA (e.g., diving injuries); indicated that the study involved children, animals, or cadavers; identified specific neck pathologies other than whiplash (e.g., cancer, spondylosis); or indicated that the study involved a surgical intervention. Abstracts were retrieved for all articles selected by one or both reviewers.
Each abstract was again screened independently by two of the first five authors (interrater agreement = 90.5%). Studies were excluded if they included subjects with previous neck injuries or WAD grades 0 or 4; indicated that the injuries were not sustained in MVAs; or involved co-interventions of surgery, traction, electrotherapies, injections, manipulation, or passive mobilizations. Where there were disagreements between reviewers, the two authors discussed their reasoning until consensus was reached. Full-text articles were retrieved for all studies that were not excluded.
Full-text articles were independently screened for inclusion by two authors (interrater agreement = 86.1%). Studies were included if they were randomized controlled trials (RCTs) or quasi-randomized controlled trials (trials using date of birth or medical record number, for example, to assign participants to groups);6 if the study population consisted of adults (ages 18 and older) with acute (less than 6 months duration) grade 1, 2, or 3 WAD sustained in an MVA; if the intervention involved postural and/or neck-stabilization exercises; and if at least one of pain, ROM, or length of time off work was measured as an outcome. Again, where there were disagreements between reviewers, the two authors discussed their reasoning until consensus was reached.
The studies included were limited to RCTs and quasi-RCTs because these types of studies are considered to represent the highest levels of evidence, according to Sackett.12 Furthermore, the Editorial Board of the Cochrane Back Review Group recommends limiting systematic reviews to RCTs where five or more studies are eligible for inclusion.13
We also hand-searched the reference lists of relevant Cochrane reviews6,10 (interrater agreement = 86.3%), the reference lists of studies selected for inclusion (interrater agreement = 83.0%), and the tables of contents of the following journals from January 2003 to March 2007 (interrater agreement = 99.7%): Clinical Orthopaedics and Related Research, Physical Therapy, Physiotherapy, Physiotherapy Canada, and Spine. Titles, abstracts, and full-text articles were screened by the procedure described above. We also contacted experts in the field for relevant studies.
The methodological quality of the studies was assessed by two independent reviewers using the van Tulder et al. criteria13 (interrater agreement = 86.4%). These criteria were selected because they had been recommended by the Editorial Board of the Cochrane Back Review Group for use in the field of back and neck pain.13 Studies were considered to be of high quality if they received a quality score of 8 or higher, of moderate quality if they scored between 4 and 7, and of low quality if they scored 3 or less. In the case of pairs or triplets of studies, one quality score was assigned to each pair or triplet. Quality criteria were considered to have been met if they were described in at least one of the studies.
Data were extracted by two independent reviewers using a data-extraction form designed by the Cochrane Back Review Group.14 The extracted data included study methodology, sample characteristics, details of the intervention, outcome measures at baseline and follow-up, and details of the data analysis. In the case of pairs or triplets of studies, data were extracted from each study in a pair or triplet onto the same data-extraction form.
A meta-analysis was deemed inappropriate because of the heterogeneity of study interventions. While each study used exercise as an intervention, the exercise programmes varied widely. Instead, data were synthesized qualitatively using levels of evidence, as recommended by van Tulder et al.13 These levels of evidence were then graded according to a scale developed by van Tulder et al.13 This scale grades evidence as strong if it is supported by consistent findings among multiple high-quality RCTs, moderate if supported by consistent findings among multiple low-quality RCTs and/or one high-quality RCT, limited if supported by one low-quality RCT, and conflicting if supported by inconsistent findings among multiple RCTs.
RESULTS
Search Results
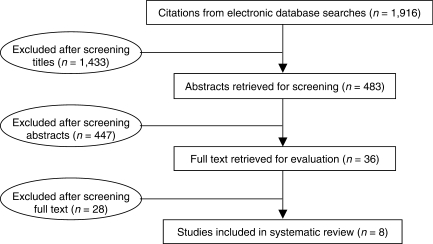
The results of our electronic database search are detailed in Figure 1. Eight studies were selected for inclusion as a result of this search. No additional studies were found through hand-searching reference lists and the tables of contents of selected journals or through contact with experts.
Figure 1.
Flow diagram of search results
Of the eight studies selected for inclusion,15–22 only three were stand-alone studies.15,16,22 Two of the remaining five constituted a pair, in which one study21 was a follow-up to the other.20 The three remaining studies constituted a triplet in which two of the studies18,19 were follow-ups to the first.17 Methods, study population, interventions, and outcome measures used in the included studies are presented in Table 2, while the methodological quality assessment of the included studies is presented in Table 3. Included studies are presented in alphabetical order in both tables.
Table 2.
Characteristics of Included Studies
| Study | Methods | Participants | Interventions | Outcomes |
|---|---|---|---|---|
| Bunketorp et al. 200615 | RCT; random allocation in blocks of 2 by flipping a coin; blinded outcome assessment | Sub-acute whiplash injury (6 weeks–3 months) after whiplash-type trauma; N = 47 (M:F = 17:30); mean age = 31 years |
|
Self-efficacy (Self-Efficacy Scale), fear of movement (Tampa Scale for Kinesiophobia), disability (Pain Disability Index), pain (VAS, Painometer), muscle tenderness (palpometer), grip strength (electronic grip-force instrument), cervical mobility (helmet equipped with goniometer), sick leave (five-point scale), use of analgesics (yes/no), frequency of analgesic use (four-point scale) |
| Crawford et al. 200416 | Quasi-RCT; random allocation based on casualty record number (even numbers allocated to experimental group, odd numbers allocated to control group); blinded outcome assessment | Acute whiplash injury within 48 hours of MVA; N = 108 (M:F = 40:68); mean age = 34 years |
|
Activities of daily living (five-item scoring tool designed by the authors), time taken to return to work (days), pain (VAS), neck ROM (goniometer) |
| Rosenfeld et al. 2000,17 2003,18 200619 (triplet of studies) | RCT; random allocation by opaque, sealed envelopes; blinded outcome assessment | Acute whiplash injury within 96 hours of MVA; N = 88 (M:F = 29:59); mean age = 35 years |
|
Cervical ROM (cervical measurement system composed of inclinometer and compass), pain (VAS), sick leave (days), physical therapy treatment costs (US$),19 costs of production loss (US$)19 |
| Schnabel et al. 2004,20 Vassiliou et al. 200621 (pair of studies) | RCT; random allocation by patient selection of opaque envelopes; unblinded | Acute whiplash injury within 48 hours of MVA; N = 200 (M:F = 77:123); mean age = 29 years |
|
Pain (VAS), disability (VAS), symptom prevalence (neck, head, shoulder, back, and limb pain; limb paresthesia; visual disturbance; tinnitus; dizziness) (yes/no) |
| Söderlund et al. 200022 | RCT; randomization procedure not described; blinding not described | Acute whiplash injury (average = 20 days) after MVA; N = 59 (M:F = 24:35); mean age = 34 years |
|
Disability (Pain Disability Index), self-efficacy (Self-Efficacy Scale), coping (Coping Strategies Questionnaire), pain (VAS), cervicothoracic posture (goniometer), cervical rotation ROM (goniometer), cervicocephalic kinaesthetic sensibility (helmet with laser pointer attached) |
C = control group; E = experimental group; M:F = ratio of male subjects to female subjects; MVA = motor vehicle accident; N = total number of subjects; n = number of subjects in experimental/control group; RCT = randomized controlled trial; ROM = range of motion; VAS = visual analogue scale
*The exercise advice sheet was not described in the paper. An attempt was made to contact the authors, but they did not respond to requests for details.
Table 3.
Results of Methodological Quality Assessment
| Study | |||||
|---|---|---|---|---|---|
| van Tulder et al. Quality Criterion13 | Bunketorp et al. 200615 | Crawford et al. 200416 | Rosenfeld et al. 2000,17 2003,18 200619 (triplet of studies) | Schnabel et al. 2004,20 Vassiliou et al. 200621 (pair of studies) | Söderlund et al. 200022 |
| Was the method of randomization adequate? | Y | N | Y | Y | U |
| Was the treatment allocation concealed? | Y | N | Y | Y | N |
| Were the groups similar at baseline regarding the most important prognostic factors? | Y | N | Y | Y | Y |
| Was the patient blinded to the intervention? | N | N | N | N | N |
| Was the care provider blinded to the intervention? | N | N | N | N | N |
| Was the outcome assessor blinded to the intervention? | Y | N | Y | U | U |
| Were co-interventions avoided or similar? | Y | Y | Y | U | Y |
| Was the compliance acceptable in all groups? | Y | U | U | Y | Y |
| Was the dropout rate described and acceptable? | Y | N | Y | N | Y |
| Was the timing of the outcome assessment in both groups comparable? | Y | Y | Y | Y | Y |
| Did the study include an intention-to-treat analysis? | Y | Y | Y | Y | U |
| Total score (/11) | 9 | 3 | 8 | 6 | 5 |
N = no (the study did not meet the criterion); U = unclear (not enough information was provided to determine whether the study did or did not meet the criterion); Y = yes (the study met the criterion)
Methodological Quality
Of the eight studies selected for inclusion, one stand-alone study15 and one triplet of studies17–19 were graded as high quality; one stand-alone study22 and one pair of studies20,21 were graded as moderate quality; and one stand-alone study was graded as low quality.16 Because of the nature of the interventions, none of the studies was able to incorporate blinding of patients or care providers. Many of the moderate- and low-quality studies did not fulfil the following criteria: adequate randomization, concealment of treatment allocation, blinding of outcome assessment, and dropout rate described and acceptable.
Effectiveness of Interventions
Postural Exercises
Two stand-alone studies15,22 and one triplet of studies17–19 used postural exercises as part of their intervention. One of the stand-alone studies15 was graded as high quality, while the other was graded as moderate quality.22 The triplet of studies17–19 was graded as high quality.
Both stand-alone studies15,22 used postural exercises with both intervention and control groups, meaning that between-group differences cannot be attributed to the postural exercises. However, the moderate-quality study22 did find significant improvements within groups on measures of pain and cervical ROM.
The high-quality triplet of studies17–19 provided postural exercises to both intervention groups but neither control group. A significant reduction in pain was reported for those patients who received postural exercises as compared to the control group, both at 6-month (p < 0.001)17 and at 3-year (p = 0.02) follow-up.18 While there was no significant difference in number of sick-leave days at 6 months,17 there was a significant difference at 3 years (p = 0.03).18 No significant difference was found for cervical ROM at either 6 months17 or 3 years.18 The authors also reported that although the initial cost of the postural exercise intervention was higher (multiple visits to a physiotherapist compared to a leaflet), the overall cost was lower when sick-leave days, loss of productivity, and the cost of other interventions eventually used by some of the control-group participants were taken into account.19
Based on one high-quality trial described in three studies,17–19 there is moderate evidence to support the use of postural exercise and advice for reducing pain and time off work in the treatment of acute WAD.
Neck-Stabilization Exercises versus Control
Two stand-alone studies15,22 and one pair of studies20,21 used neck-stabilization exercises as part of their intervention. One of the stand-alone studies15 was graded as high quality, while the other was graded as moderate quality.22 The pair of studies20,21 was also graded as moderate quality.
The high-quality stand-alone study15 had patients in both groups perform exercises, but only patients in the intervention group performed exercises specifically targeted at strengthening neck muscles. No statistically significant differences were found between or within the groups on pain measured using the visual analogue scale (VAS), cervical ROM, or time off work. However, the Pain Disability Index and analgesic consumption, along with several other outcome measures used in this study (e.g., Self-efficacy Scale, Tampa Scale for Kinesiophobia), showed a significant improvement in favour of the intervention group over the control group (p = 0.03) at 3-month follow-up.
The moderate-quality stand-alone study22 compared two different home exercise programmes in which the intervention group performed kinaesthetic sensibility and neck muscle coordination exercises that would also isometrically strengthen the neck muscles. No statistically significant differences were found between the groups with respect to pain or cervical ROM.
In the moderate-quality pair of studies,20,21 the intervention group performed exercises to strengthen the neck muscles. Significant differences were found between the groups at 6-week (p = 0.04)20 and 6-month (p = 0.02)21 follow-up on the pain VAS.
In summary, there is conflicting evidence on the use of neck-stabilization exercises in the treatment of acute WAD.
Neck Stabilization Exercises versus Soft Collars
One stand-alone study,16 one triplet of studies,17–19 and one pair of studies20,21 compared active exercise interventions with rest using a soft collar. The stand-alone study16 was graded as low quality, the triplet of studies17–19 as high quality, and the pair of studies20,21 as moderate quality.
In the low-quality stand-alone study,16 no significant between-group differences for pain scores or total neck ROM were noted either initially or at follow-up. The collar group took significantly more time to return to work (p = 0.03) compared to the active intervention group. There were no significant between-group differences for activities of daily living, either initially or at follow-up.
The high-quality triplet of studies17–19 found a significant reduction in pain at 6 months (p < 0.001)17 and at 3 years (p = 0.02) for the active intervention group as compared with the control group.18 There was no significant difference in number of sick-leave days or cervical ROM at 6-month follow-up;17 however, there was a significant reduction in number of sick-leave days in favour of the active intervention group at 3-year follow-up (p = 0.03).18
In the moderate-quality pair of studies,20,21 a significant difference in reduction of pain in favour of the active intervention group at 6 weeks (p = 0.04)20 and 6 months (p = 0.02)21 was found.
In summary, there is moderate evidence to suggest that active interventions are more effective than soft collars in the treatment of acute WAD.
DISCUSSION
Previous systematic reviews on this topic have found limited evidence in support of active ROM exercises in the treatment of acute WAD,6,10 and limited6 or conflicting10 evidence in support of active interventions (e.g., exercise) over passive interventions (e.g., soft collar). The efficacy of specific exercises, such as postural or neck-stabilization exercises, had not been evaluated in previous systematic reviews.
In agreement with previous systematic reviews,6,10 we found support for the use of active interventions over soft collars in the treatment of acute WAD. However, unlike previous systematic reviews, which found only limited or conflicting evidence,6,10 our systematic review found a moderate level of evidence.
A shortcoming of this review was the narrow focus that resulted in exclusion of studies with co-interventions, decreasing the number of included studies that might have strengthened our conclusions. This narrow focus was necessary, however, to elicit the specific effects of exercise on WAD. Another limitation was that only reviews from the Cochrane Database of Systematic Reviews were evaluated. Other review articles were excluded because Cochrane systematic reviews tend to have greater methodological rigour, making them less prone to bias, and tend to be updated more frequently than systematic reviews published by other sources.23 In addition, the sheer number of reviews on this topic published by other sources made it prohibitive to evaluate them all. A strength of this review was the exhaustive and systematic methodological approach, which minimized the likelihood of overlooked studies.
The practical and clinical implications of this review are that postural exercises should be of value, whereas soft collars should be used sparingly, in the treatment of persons with WAD; furthermore, although the initial cost of active intervention is high, the overall cost is less when time off work, reduced productivity, and the cost of other interventions are taken into account,19 suggesting that, economically, it would be best to invest in early exercise interventions for treating persons with WAD.
One question that the literature has left unanswered to date is which specific exercise interventions are beneficial in the treatment of WAD. In our review, the studies included were heterogeneous in terms of the types of exercises used for the treatment of WAD. For instance, in the study by Schnabel et al.,20 the prescribed exercises were mobilization and active elastic rubber-band exercises, whereas in the study by Rosenfeld et al.,17 the exercises were based on the McKenzie principle.24 Furthermore, description of the exercises was lacking in several of the studies, making it difficult for clinicians to use the findings of the studies in practice. The literature has yet to address the optimal frequency, intensity, and duration of the different exercises. Future research should focus on addressing these questions.
CONCLUSION
This systematic review found moderate evidence to support the use of postural exercise for reducing pain and time off work in the treatment of persons with acute WAD, conflicting evidence on the use of neck-stabilization exercises in the treatment of acute WAD, and moderate evidence to suggest that active interventions, such as postural and neck-stabilization exercises, are more effective than soft collars in the treatment of acute WAD. No evidence was found to support the use of postural or neck-stabilization exercises for increasing neck ROM in the treatment of persons with acute WAD.
KEY MESSAGES
What Is Already Known on This Subject
Two Cochrane reviews on topics related to the treatment of WAD had been previously published. Both reviews included studies that used multimodal treatments. As neither review looked specifically at the effects of exercise in the treatment of patients with WAD, we determined that there was a need for a systematic review to elucidate the specific effects of exercise in the treatment of WAD. In particular, there was a need for a review examining the effects of neck stabilization and postural exercises in the treatment of WAD, as these interventions are commonly employed by physiotherapists.
What This Study Adds
Based on the results of this systematic review, there is moderate evidence to support the use of postural exercises for decreasing pain and time off work in the treatment of patients with acute WAD. However, no evidence exists to support the use of postural exercises for increasing neck ROM. There is conflicting evidence in support of neck-stabilization exercises in the treatment of patients with acute WAD.
Acknowledgments
The authors would like to thank Tyler Dumont for providing consultation and review of this manuscript prior to submission and Charlotte Beck for her assistance in conducting the literature search.
Appendix: Quality-Assessment Tool for Evaluating Review Articles
Did the review address a focused clinical question?
Is it unlikely that important or relevant studies were missed? (i.e., was the search for evidence comprehensive?)
Were the criteria used to select articles for inclusion appropriate? Were the exclusion criteria appropriate?
Was the validity of the included studies appraised?
Were the assessments of studies reproducible?
Were the results combined appropriately?
Do the conclusions of the review reflect the results?
Drescher K, Hardy S, MacLean J, Schindler M, Scott K, Harris SR. Efficacy of postural and neck stabilization exercises for persons with acute whiplash-associated disorders: a systematic review. Physiother Can. 2008;60:215-223.
REFERENCES
- 1.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. 1995;20(8 Suppl):1S–73S. [PubMed] [Google Scholar]
- 2.Rodriquez AA, Barr KP, Burns SP. Whiplash: pathophysiology, diagnosis, treatment, and prognosis. Muscle Nerve. 2004;29:768–81. doi: 10.1002/mus.20060. [DOI] [PubMed] [Google Scholar]
- 3.Ferrari R, Russell AS, Carroll LJ, Cassidy JD. A re-examination of the whiplash associated disorders (WAD) as a systemic illness. Ann Rheum Dis. 2005;64:1337–42. doi: 10.1136/ard.2004.034447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Falla D. Unravelling the complexity of muscle impairment in chronic neck pain. Man Ther. 2004;9:125–33. doi: 10.1016/j.math.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. 2004;9:89–94. doi: 10.1016/S1356-689X(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 6.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G. Exercises for mechanical neck disorders. doi: 10.1002/14651858.CD004250.pub3. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: CD004250. [DOI] [PubMed] [Google Scholar]
- 7.Scholten-Peeters GGM, Bekkering GE, Verhagen AP, van der Windt DAWM, Lanser K, Hendriks E, et al. Clinical practice guideline for the physiotherapy of patients with whiplash-associated disorders. Spine. 2002;27:412–22. doi: 10.1097/00007632-200202150-00018. [DOI] [PubMed] [Google Scholar]
- 8.Leigh T. Clinical practice guidelines for the physiotherapy treatment of patients with whiplash associated disorders [PDF document on the Internet] Best Practices Task Force; 2004 [updated 2004 June; cited 2006 Jul 28]. Available from: http://www.bcphysio.org/app/pdfs/wad.pdf.
- 9.Kennedy CN. The cervical spine. In: Hall CM, Brody LT, editors. Therapeutic exercise: moving toward function. 2nd. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 582–609. [Google Scholar]
- 10.Verhagen AP, Scholten-Peeters GGM, de Bie RA, Bierma-Zeinstra SMA. Conservative treatments for whiplash. doi: 10.1002/14651858.CD003338.pub2. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No.: CD003338. [DOI] [PubMed] [Google Scholar]
- 11.Oxman AJ, Cook DJ, Guyatt GH. Users’ guides to the medical literature: VI. how to use an overview. J Am Med Assoc. 1994;272:1367–71. doi: 10.1001/jama.272.17.1367. [DOI] [PubMed] [Google Scholar]
- 12.Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. 1989;95(2 Suppl):2S–4S. [PubMed] [Google Scholar]
- 13.van Tulder M, Furlan A, Bombardier C, Bouter L,, Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine. 2003;28:1290–9. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 14.Cochrane Back Review Group [homepage on the Internet] Data extraction form. The Group; 2004 [updated 2004 Oct; cited 2006 Aug 1]. Available from: http://www.cochrane.iwh.on.ca/pdfs/data_extract_04.pdf.
- 15.Bunketorp L, Lindh M, Carlsson J, Stener-Victorin E. The effectiveness of a supervised physical training model tailored to the individual needs of patients with whiplash-associated disorders: a randomized controlled trial. Clin Rehabil. 2006;20:201–17. doi: 10.1191/0269215506cr934oa. [DOI] [PubMed] [Google Scholar]
- 16.Crawford JR, Khan RJ, Varley GW. Early management and outcome following soft tissue injuries of the neck: a randomised controlled trial. Injury. 2004;35:891–5. doi: 10.1016/j.injury.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Rosenfeld ME, Gunnarsson R, Borenstein P, Cassidy JD. Early intervention in whiplash-associated disorders: a comparison of two treatment protocols. Spine. 2000;25:1782–7. doi: 10.1097/00007632-200007150-00008. [DOI] [PubMed] [Google Scholar]
- 18.Rosenfeld M, Seferiadis A, Carlsson J, Gunnarsson R. Active intervention in patients with whiplash-associated disorders improves long-term prognosis: a randomized controlled clinical trial. Spine. 2003;28:2491–8. doi: 10.1097/01.BRS.0000090822.96814.13. [DOI] [PubMed] [Google Scholar]
- 19.Rosenfeld M, Seferiadis A, Gunnarsson R. Active involvement and intervention in patients exposed to whiplash trauma in automobile crashes reduces costs: a randomized, controlled clinical trial and health economic evaluation. Spine. 2006;31:1799–804. doi: 10.1097/01.brs.0000225975.12978.6c. [DOI] [PubMed] [Google Scholar]
- 20.Schnabel M, Ferrari R, Vassiliou T, Kaluza G. Randomised, controlled outcome study of active mobilisation compared with collar therapy for whiplash injury. Emerg Med J. 2004;21:306–10. doi: 10.1136/emj.2003.010165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vassiliou T, Kaluza G, Putzke C, Wulf H, Schnabel M. Physical therapy and active exercises: an adequate treatment for prevention of late whiplash syndrome? Randomized controlled trial in 200 patients. Pain. 2006;124:69–76. doi: 10.1016/j.pain.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Söderlund A, Olerud C, Lindberg P. Acute whiplash-associated disorders (WAD): the effects of early mobilization and prognostic factors in long-term symptomatology. Clin Rehabil. 2000;14:457–67. doi: 10.1191/0269215500cr348oa. [DOI] [PubMed] [Google Scholar]
- 23.Jadad AR, Cook DJ, Jones A, Klassen TP, Tugwell P, Moher M, et al. Methodology and reports of systematic reviews and meta-analyses: a comparison of Cochrane reviews with articles published in paper-based journals. J Am Med Assoc. 1998;280:278–80. doi: 10.1001/jama.280.3.278. [DOI] [PubMed] [Google Scholar]
- 24.McKenzie R. The cervical and thoracic spine: mechanical diagnosis and therapy. Waikane, New Zealand: Spinal Publications; 1990. [Google Scholar]