Abstract
Purpose:
To determine whether outcomes could be changed after poor response to non-specific exercise therapy when the prescription was changed to specific, directional-preference exercises (McKenzie method).
Methods:
Patients who participated in a randomized clinical trial (RCT) and the alternative care phase immediately following formed the cohort for this case series. In an earlier RCT, patients with directional preference were randomized to exercises/advice matched to their individual directional preference or to one of two unmatched protocols. The primary inclusion criterion for our case series was patient reports of being unchanged or worse following 2 weeks’ treatment in the RCT. The secondary inclusion criterion was patient requests for “a change to one of the other stretching protocols to see if I can achieve better pain control.” Patients meeting either of these criteria were offered matched exercises/advice if they had not previously received this intervention. Two-way repeated-measures ANOVA and McNemar tests compared outcomes during two consecutive time intervals: baseline to 2 weeks and 2 weeks to discharge. Dropouts were included in the intention-to-treat analysis.
Results:
Four patients from the matched group met the primary inclusion criterion of “unchanged” (none reported being worse); 10 additional patients requested alternative treatment for better pain control (secondary criterion). Eighty-five patients from the two unmatched treatment groups met all the inclusion criteria, and an additional 22 patients met only the secondary criterion. These patients were offered matched treatment, and 96 consented. Those reporting improvement or resolution of symptoms were 22 % in the first two weeks of unmatched care (during the RCT) compared to 84 % with matched care. Statistically significant and clinically meaningful changes occurred in all outcomes (p < 0.001) after receiving matched care, compared to clinically unimportant changes with previous unmatched care during the RCT.
Conclusions:
Poor outcomes from non-specific/unmatched exercise protocols appeared to reverse when patients with directional preference were given sub-group-matched, direction-specific exercises. Because of the limitations of our study design, replication with a control group and longer-term follow-up are required to validate the findings.
Keywords: centralization, directional preference, exercise, low back pain, McKenzie method, sciatica, sub-groups
RÉSUMÉ
Objet :
Déterminer si les résultats peuvent changer après une réaction médiocre à une thérapie par l’exercice non spécifique lorsque la prescription est changée à des exercices spécifiques à préférence directionnelle (méthode McKenzie).
Méthodologie :
Des patients qui ont participé à un essai clinique aléatoire (ECA) et à la phase de soins alternatifs suivant cet essai, ont formé la cohorte pour cette série de cas. Lors d’un ECA précédent, les patients ayant une préférence directionnelle s’étaient vus attribuer aléatoirement des exercices ou conseils correspondant à leur préférence directionnelle individuelle ou à un ou deux protocoles non assortis. Le critère d’inclusion principal pour notre série de cas était le choix de patients signalant qu’ils demeuraient inchangés ou devenaient pires après deux semaines de traitement en ECA. Le critère d’inclusion secondaire était le choix de patients demandant un changement à l’un des autres protocoles d’exercices d’étirement afin de savoir s’ils pouvaient exercer un meilleur contrôle sur la douleur. On a offert aux patients qui satisfaisaient à l’un de ces critères des exercices ou conseils assortis s’ils n’avaient pas déjà reçu cette intervention. Des mesures à deux critères de classification répétées ANOVA et des essais McNemar ont comparé les résultats durant deux intervalles de temps consécutifs : de la base de référence à deux semaines et de deux semaines au congé. Ceux qui avaient abandonné ont été inclus dans l’analyse du principe de vouloir traiter.
Résultats :
Quatre patients du groupe assortis satisfaisaient au critère principal d’inclusion d’« inchangés » (aucun n’était pire) ; 10 autres patients avaient demandé une forme différente de traitement pour arriver à un meilleur contrôle de la douleur (critère secondaire). Quatre-vingt-cinq patients des deux groupes de traitements non assortis satisfaisaient à tous les critères d’inclusion et 22 autres patients satisfaisaient seulement au deuxième critère. On a offert à ces patients des traitements assortis et 96 ont consenti. Ceux qui avaient signalé une amélioration ou une résolution des symptômes comptaient pour 22 % durant les deux premières semaines de soins non assortis (lors des ECA) par rapport à 84 % pour les soins assortis. Des changements importants des points de vue statistique et clinique se sont produits dans tous les résultats (p < 0,001) après que les patients ont reçu les soins assortis par rapport aux changements cliniques négligeables associés aux soins non assortis précédents durant les ECA.
Conclusion :
Les résultats médiocres des protocoles non spécifiques ou d’exercices non assortis semblaient se renverser lorsque les patients ayant une préférence directionnelle recevaient des exercices axés sur la direction et sur le sous-groupe assorti. En raison des limites du concept de notre étude, la reproduction avec un groupe témoin et une période de suivi à long terme sont requises pour valider ces résultats.
Mots clés: centralisation, exercice, lombalgie, méthode McKenzie, préférence directionnelle, sciatique, sous-groupes
BACKGROUND
Classifying persons with low back pain (LBP) into specific sub-groups to provide sub-group-specific treatment has been identified as a top research priority within the orthopaedic literature.1,2 As suggested in a number of trials, treating sub-groups with sub-group-specific interventions resulted in clearer differences in outcomes across the interventions studied.3–7 For example, clinical prediction rules have been developed to identify potential responders to manipulation3 and stabilization exercises.7 To determine whether classification led to more positive outcomes, a recent systematic review investigated treatment following classification into sub-groups based on patients’ responses to examination.8 The authors concluded that “the patient's response method of classification (i.e., change in pain location or intensity with specific movement testing) demonstrates a positive trend toward improving the likelihood of targeting the correct supervised exercises for patient intervention.”8(p.159) Conducting trials of specific sub-groups is important to determine which treatments are effective for a particular group of patients.
One sub-group of patients with LBP receiving increased attention in the literature are patients who demonstrate the centralization phenomenon and/or directional preference during an assessment and physical examination.8–20 Centralization, or the relief of local or distal pain emanating from the spine, occurs in response to repeated movements or sustained postures and is measured by patient self-report.11–13 First priority is given to relief of distal symptoms, if present. Experienced clinicians have demonstrated strong interrater chance-corrected agreement (i.e., kappa values 0.79 to 1) in eliciting centralization and determining whether it has or has not occurred.21–23 The presence of centralization has also demonstrated strong prognostic validity.9,10,13–19
Directional preference is the direction of movement or posture (flexion, extension, or side-glide/rotation) that produces the centralization phenomenon. Experienced clinicians have shown strong interrater chance-corrected agreement (κ = 0.90) in determining the direction of movement (directional preference) that produced centralization.22 While centralization can be described by the directional preference that produces it, directional preference does not always produce centralization (change in pain location). Directional preference may also produce a decrease in pain intensity without a change in location and/or an increase in previously limited movement; the therapist records directional preference while evaluating symptomatic and mechanical (e.g., range of motion) responses to the mechanical evaluation. Thus the two terms are not synonymous but closely allied.
Long et al.11 demonstrated that patients with a mechanically determined directional preference achieved superior outcomes when exercises and evidence-based advice matched the individual's directional preference compared to exercise protocols unmatched to directional preference and evidence-based advice.24,25 The latter included advice to remain active and education fashioned after Indahl et al.,24 aimed at minimizing fear-avoidance behaviour.
In that trial,11 direction-specific exercises matched to a patient's mechanically determined directional preference produced significantly better outcomes than non-specific exercises and evidence-based advice, even when this advice incorporated contemporary ideas on reassurance and remaining active. There were significantly greater improvements in every outcome for the matched group compared to the two unmatched groups (defined below): p-values varied from 0.016 to less than 0.001.
The present study is a case series that included two phases of analysis. First, secondary analysis of findings from the original randomized clinical trial (RCT) was conducted, excluding patients who reported that their symptoms were resolved or improved. The secondary analysis included only data from those patients reporting that they were worse or unchanged. The second phase of data collection occurred immediately after the RCT, when these patients were then offered direction-specific treatment. These latter data have not been reported previously.
Because of the equivocal or conflicting results of past trials, systematic reviews have been unable to recommend one form of exercise over the other, and the role of specific exercises remains controversial.26–29 More trials are needed before it is possible to recommend one form of exercise over another, or before the benefits of “individualized” exercise prescriptions can be convincingly demonstrated. The current study aims to contribute to the growing literature examining the role of direction-specific exercise.4–11
McKenzie12 introduced the concept of direction-specific exercises aimed at producing an analgesic effect for persons with LBP (often concurrent with restoration of range of motion). This pain-reduction effect was supported by Long et al.'s RCT.11 Two of the ethics board requirements for this RCT were that side effects (i.e., worsening or peripheralization of pain) be documented and that those patients failing to respond to treatment at 2 weeks be offered alternative care following completion of the trial. These requirements created an opportunity to collect data on this subset of patients immediately following the 2-week protocol of the original RCT.
Participation in the RCT followed by alternative care (i.e., direction-specific exercises) formed the framework for the current prospective case series. The aim of the present study was to conduct a secondary analysis of data from the original trial11 plus analysis of additional data collected during the following 2 weeks to determine whether outcomes could be changed after initial poor response to exercise therapy when patients were given alternative, direction-specific exercises.
METHODS
The current case-series investigation builds on a previously reported RCT.11 Before providing the details of the case-series methodology, we offer a brief review of the methodology associated with the clinical trial.
Background Details of Previous RCT
The purpose of the RCT11 was to determine whether patient-specific exercises concordant with the patient's directional preference would achieve better outcomes than non-concordant exercises. Consecutive patients with LBP aged 18–65 years, with or without lower-extremity symptoms and with no more than one neurological sign, and demonstrating directional preference during a single session mechanical assessment by McKenzie/MDT (Mechanical Diagnosis and Treatment) credentialed therapists were considered for inclusion. Patients were excluded for the following reasons: (1) signs or symptoms suggestive of serious pathology, (2) presentation post-surgery, (3) off work for one year or more, (4) currently pregnant, and (5) prior knowledge of the McKenzie (MDT) approach. Patients were recruited from 11 sites in five countries; 53 % were male; 70 % reported a history of prior episodes; and 39 % were off work. The median duration of LBP was 8.86 weeks. Approximately 50 % had simple LBP, and the remainder had additional referred symptoms (17 % with one neurological sign). A sub-group of 230/312 (74 %) consecutive patients demonstrated directional preference during a standardized mechanical assessment12 and were randomized into three different exercise and advice groups.
The exercise and advice groups are detailed in the appendices of the RCT.11 In brief, all three groups received evidence-based advice to remain active and to walk, cycle, or swim as tolerated. The three treatment groups received (1) matched exercises and advice consistent with directional preference and the McKenzie (MDT) method;12 (2) exercises opposite the directional preference that typically stretch the muscles over the painful area, plus advice aimed at minimizing fear and providing reassurance (fashioned after Indahl);24 and (3) common back exercises that do not favour one direction, do not go to end range, and include stretching of the hip/thigh muscles, as well as the advice fashioned after Indahl.24 Since the later two protocols did not match the patient sub-group classification and were not designed based on directional preference, these protocols will be referred to in this article as the “unmatched” treatment groups.
Primary outcome measures were back and leg pain intensity (0–10 numeric rating scales) and the Roland Morris Disability Questionnaire (RMDQ; 0–24 scale). Additional outcome measures were medication use, rating of activity interference at home and work (0–5 scale), Beck Depression Inventory (0–63 scale), and a questionnaire inquiring about patients’ self-rating of improvement and their beliefs regarding the need for further treatment.
During the planning stage of the RCT, it was proposed and supported by the Community Ethics Review Board of the Alberta Heritage Foundation for Medical Research that patients who failed to improve were to be provided an alternative treatment regimen. The sampling frame for this RCT11 formed the basis for the current case series sample.
Case-Series Methods
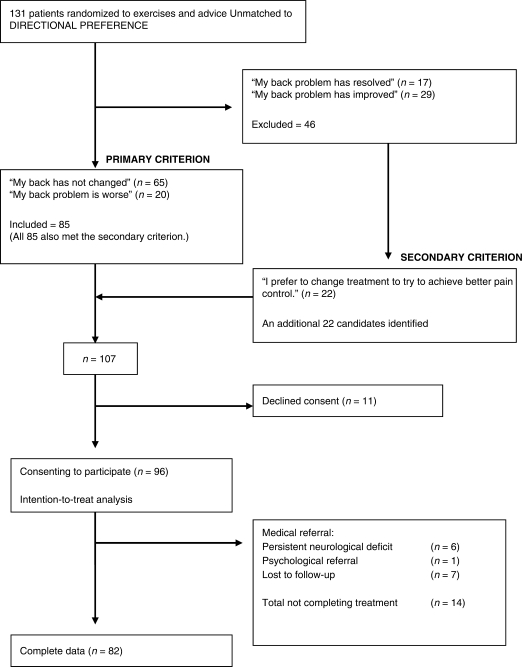
The current case series includes secondary analysis of data from the original 2-week RCT plus additional data collected when the participants received “alternative treatment” immediately following the RCT. Candidates for inclusion met one of two criteria. The primary criterion was a questionnaire item asking patients to “Please tick the phrase that best describes how you feel you have responded to treatment”: patients were included if they responded that they had “not changed much” or were “worse” upon completion of the RCT (see Figure 1). To ensure that individuals requiring further treatment were not missed, a secondary criterion was used as a cross-reference. Individuals who chose the item “I prefer to change to one of the other stretching routines to see if I could achieve better pain control” on the questionnaire regarding their wishes for further treatment were also offered alternative exercises. By these means, the ethics board requirement of identifying patients in need of alternative care was met and an additional 2 weeks’ treatment was offered.
Figure 1.
Inclusion/exclusion criteria for current case series
Outcome Measures
Outcome measures were the same as those used for the RCT. Data were collected at three time points: baseline, after a maximum of 2 weeks’ participation in the original RCT,11 and after a period of alternative care that immediately followed. The “global rating of subjective improvement” outcome was derived from the following questionnaire item:
Please tick the phrase that best describes how you feel you have responded to treatment:
(1) “My back problem has resolved and I no longer need treatment.”
(2) “My back problem has improved but I need a few more treatments.”
(3) “My back problem has not changed much.”
(4) “My back problem is worse.”
Obtaining patient feedback in treatment planning reflects common clinical practice.
Data Analysis
Analysis included two-way repeated-measures analysis of variance (ANOVA) for continuous variables, with the time effect used to address the current purpose. The factors were group (levels were Opposite and Non-directional) and time (levels were Pre and Post). McNemar tests were used for categorical variables. Outcomes were compared during the following two chronological intervals: (1) assigned RCT11 exercise protocol (change between baseline and the first 2-week interval) and (2) alternative care phase following the RCT (changes between week 2 and discharge). The sample-size calculations were based on the original RCT and used the RMDQ and low back and leg pain ratings as the primary outcomes. In addition, we included the same secondary outcomes used in the RCT. All patients who consented to participate in this second phase of treatment were included in an intention-to-treat analysis based on carry-forward of the last known data point.
RESULTS
The RCT protocol called for a maximum of six visits over 2 weeks. For participants who reported that they were unable/unwilling to continue their exercises because their pain was worsening or was not improving, the mean (SD) number of visits in the RCT was 2.55 (1.32). As stated in the consent form, participants were allowed to stop the trial at any time and were immediately offered alternative care. Those consenting to a change in exercise prescription received an average of 7.58 (7.22) visits of direction-specific exercises (more than the six intended in the protocol). It appears that inadequate instruction and/or poor wording on the data-entry forms affected the recording of the number of visits at some clinics: instead of recording the number of visits after 2 weeks of direction-specific exercises, the therapist recorded the number of visits at “discharge” from care, which may have included additional treatment. A number of clinics were obligated to provide conditioning-type programmes after the initial pain-control (direction-specific exercises) phase of treatment.
Phase 1: Randomized Controlled Trial11
Matched Care Group (n = 80) RCT Results
Four patients (5.6 %) met the primary inclusion criterion for the current case-series investigation, reporting that they were not changed as a result of participation in the RCT. Three of these were referred for medical evaluation (persistent neurological deficit), and one was referred for psychological intervention. None reported that they were worse. Ten (14.1 %) additional candidates were identified by the secondary inclusion criterion, reporting that they wished to “change treatment in order to achieve better pain control.” Six of these patients were referred for further medical investigations (one subsequently received a medical diagnosis of bone cancer and another one, who had experienced a fall, was told she had a “kidney infection/bruise”); three declined further “stretching exercises” and requested “strengthening” exercises, and the sixth was lost to follow-up. Because of these small numbers, no statistical analysis was completed on this group, and these patients are not included in the results.
Unmatched Care Groups (n = 131) RCT Results
Figure 1 illustrates the selection process and dropouts for the current case series. Of the 131 patients who received either of the two unmatched protocols in the original RCT,11 85 (65 %) met the primary criterion, reporting their symptoms as “not changed much” (65) or “worse” (20), and also met the secondary criterion by choosing the questionnaire item “I prefer to change to one of the other stretching routines to see if I could achieve better pain control.” An additional 22 candidates met only the secondary criterion (N = 85 + 22 = 107). Since we had anticipated that similar numbers of patients would meet both criteria, we took a closer look at the pain data of the additional 22 patients. While they had reported that their back problems had “improved” (mean decrease in LBP of 2.5/10), they did not have clinically meaningful decreases in leg pain (-1.1/10), which perhaps explains their desire for better pain control.
Of the 107 candidates identified, 11 declined consent, primarily because of time constraints. Baseline characteristics of the remaining 96 patients who formed the cohort for the current series appear in Table 1. Eighty-two completed treatment and provided complete data at all three time points: baseline, 2 weeks, and 4 weeks. The treating therapists recommended medical referral for six (persisting neurological deficit or patient preference) and psychological referral for one; seven were lost to follow-up. The 14 patients who did not complete treatment were more likely to be single (p < 0.001), to be younger (p = 0.043), to have higher depression scores (p = 0.002), to take medication (p = 0.010), and to take more pills per day (p = 0.045).
Table 1.
Baseline Characteristics (N = 96)
| Characteristic | n (%) |
|---|---|
| Male/female | 55/41 (57.3/42.7) |
| Current episode | |
| Acute (<7 days) | 12 (12.5) |
| Subacute (<7 weeks) | 25 (26.0) |
| Chronic (>7 weeks) | 57 (59.4) |
| Invalid data* | 2 (2.1) |
| History of prior episodes | 71 (74.0) |
| Pain location | |
| QTF 1 (back/buttock pain) | 46 (47.9) |
| QTF 2 (thigh) | 22 (22.9) |
| QTF 3 (below knee) | 15 (15.6) |
| QTF 4** (below knee plus mild neurological deficit) | 3 (13.5) |
| Off work because of LBP | 45 (46.9) |
| Mean (SD) age in years | 42.5 (10.2) |
| Length of current episode in weeks: 1st, 2nd (median), and 3rd quartiles | 3.0, 18.9, 37.3 |
QTF = Quebec Task Force; LBP = low back pain
*Data are unclear as to whether dates reflect current episode or first episode.
**Patients with two or more neurological signs were excluded.
All 96 patients were included in the intention-to-treat (ITT) analysis using the carry-forward of the last known data point. In Tables 2 and 3, the p-values for the ITT appear in italics under the boldface p-values for the 82. The data in Table 2 represent a secondary analysis of the RCT data, except that data for those who were reported that their symptoms were “resolved” or “improved” are excluded. Group and time effects, respectively, describe the significance accorded to treatment group and differences between baseline and follow-up points; interaction describes the significance between groups and outcomes in the two unmatched groups from the original RCT.
Table 2.
Secondary Analysis: Unmatched Treatment Groups—Outcomes after RCT
| Outcome Measures | Pre-Post | Unmatched Treatment | Group Effect | Interaction | Time Effect (n=82 with | |
|---|---|---|---|---|---|---|
| Groups | (F df) | (F df) | complete data) | |||
| (F df) | ||||||
| Opposite | EBC | Intention to Treat* (n=96) | ||||
| Mean | Mean | (F df) | ||||
| (SD) | (SD) | |||||
| Back pain/10 | Pre | 6.04 | 5.78 | 0.01 1,80 (p=0.98) | 1.31 1,80 (p=0.26) | 10.88 1,80 (p=0.001) |
| (2.22) | (2.02) | 101.72 1,94 (p<0.001) | ||||
| Post | 5.09 | 5.33 | ||||
| (2.28) | (2.18) | |||||
| Leg pain/10** | Pre | 3.66 | 2.75 | 0.70 1,75 (p=0.42) | 1.42 1,75 (p=0.24) | 0.02 1,75 (p=0.90) |
| (3.23) | (3.04) | 0.039 1,93 (p=0.94) | ||||
| Post | 3.27 | 3.11 | ||||
| (2.95) | (3.21) | |||||
| RMDQ: Total yes/24 | Pre | 15.61 | 19.65 | 8.36 1,78 (p<0.001) | 1.03 1,78 (p=0.31) | 2.76 1,78 (p=0.10) |
| (6.16) | (4.21) | 2.70 1,94 (p=0.10) | ||||
| Post | 15.09 | 17.76 | ||||
| (6.75) | (5.90) | |||||
| Medication: Total | Pre | 3.50 | 2.73 | 0.65 1,29 (p=0.43) | 0.12 1,29 (p=0.73) | 4.30 1,29 (p=0.047) |
| pills/day** | (2.90) | (2.02) | 0.050 1,48 (p=0.82) | |||
| Post | 2.56 | 2.06 | ||||
| (2.76) | (1.83) | |||||
| During the past week, | Pre | 3.37 | 3.34 | 0.42 1,79 (p=0.66) | 1.65 1,79 (p=0.20) | 2.17 1,79 (p=0.15) |
| pain interference | (1.06) | (0.91) | 4.461 1,94 (p=0.037) | |||
| with usual work, | Post | 3.13 | 3.34 | |||
| in and outside | (1.09) | (0.97) | ||||
| home: rating (0–5) | ||||||
| BDI-11/63 | Pre | 7.31 | 6.50 | 0.70 1,74 (p=0.41) | 1.19 1,74 (p=0.28) | 13.97 1,78 (p<0.001) |
| (7.24) | (6.33) | 25.10 1,94 (p<0.001) | ||||
| Post | 6.31 | 4.71 | ||||
| (7.16) | (4.17) | |||||
| Taking medication (Yes) | Pre | 12 | 8 | McNemar test used for time effect (p=0.63) | ||
| (63.2%) | (66.7%) | Groups collapsed due to small n (p=0.55) | ||||
| Post | 10 | 8 | ||||
| (52.6%) | (66.7%) | |||||
Opposite = evidence-based advice and exercises opposite to direction preference; EBC = evidence-based advice and common back exercises with no directional preference; RMDQ = Roland Morris Disability Questionnaire; BDI = Beck Depression Inventory
*Intention-to-treat analysis using carry-forward of last known data point
**Floor effect: those with no leg pain/no medication at baseline were excluded from analysis.
Table 3.
Outcomes after Crossover (N = 82 patients with complete data)
| Outcome Measures | Pre-Post | Unmatched Treatment | Group Effect | Interaction | Time Effect (n=82 with | |
|---|---|---|---|---|---|---|
| Groups | (F df) | (F df) | complete data) (F df) | |||
| Opposite | EBC | Intention to Treat* (n=96) | ||||
| Mean | Mean | (F df) | ||||
| (SD) | (SD) | |||||
| Back pain/10 | Pre | 5.09 | 5.33 | 0.05 1,80 | 1.41 1,80 | 125.11 1,80(p<0.001) |
| (2.28) | (2.18) | (p=0.83) | (p=0.52) | 14.62 1,94 (p<0.001) | ||
| Post | 2.41 | 2.33 | ||||
| (1.92) | (1.77) | |||||
| Leg pain/10** | Pre | 3.27 | 3.11 | 0.01 1,75 | 0.70 1,75 | 63.29 1,75 (p<0.001) |
| (2.95) | (3.21) | (p=0.91) | (p=0.41) | 55.12 1,93 (p=0.001) | ||
| Post | 1.00 | 1.28 | ||||
| (1.86) | (1.99) | |||||
| RMDQ: Total yes/24 | Pre | 15.09 | 17.76 | 3.18 1,78 | 0.01 1,78 | 34.61 1,78 (p<0.001) |
| (6.75) | (5.90) | (p=0.08) | (p=0.93) | 42.37 1,94 (p<0.001) | ||
| Post | 10.96 | 13.50 | ||||
| (7.74) | (8.20) | |||||
| Medication: Total | Pre | 2.56 | 2.07 | 0.001 1,29 | 1.38 1,29 | 8.24 1,29 (p=0.008) |
| pills/day** | (2.76) | (1.83) | (p=0.98) | (p=0.25) | 10.46 1,48 (p=0.002) | |
| Post | 0.81 | 1.33 | ||||
| (1.33) | (1.76) | |||||
| During the past week, | Pre | 3.13 | 3.34 | 1.01 1,79 | 0.04 1,79 | 78.12 1,79 (p<0.001) |
| pain interference | (1.09) | (0.97) | (p=0.32) | (p=0.85) | 70.88 1,94 (p=0.001) | |
| with usual work, in | Post | 2.17 | 2.34 | |||
| and outside home: | (0.85) | (0.99) | ||||
| rating (0–5) | ||||||
| BDI-11 | Pre | 6.31 | 4.71 | 1.51 1,74 | 0.23 1,74 | 34.19 1,74 (p<0.001) |
| (7.16) | (4.17) | (p=0.22) | (p=0.63) | 33.67 1,94 (p=0.001) | ||
| Post | 3.74 | 2.53 | ||||
| (5.22) | (3.18) | |||||
| Taking medication (Yes) | Pre | 10 | 8 | McNemar test used for time effect (p=0.040) | ||
| (52.6%) | (66.7%) | Groups collapsed due to small n (p=0.002) | ||||
| Post | 6 | 5 | ||||
| (31.6%) | (41.7%) | |||||
Opposite = evidence-based advice and exercises opposite to DP; EBC = evidence-based advice and common back exercises; RMDQ = Roland Morris Disability Questionnaire; BDI = Beck Depression Inventory
*Intention-to-treat analysis using carry-forward of last known data point
**Floor effect: those with no leg pain/no medication at baseline were excluded from analysis.
The data for those who reported that their symptoms were “worse” or “not changed much” after participation in the RCT demonstrated no statistically significant improvements in five of seven outcomes and showed statistically significant but not clinically meaningful changes in LBP and depression scores.
Phase 2: Alternative Care
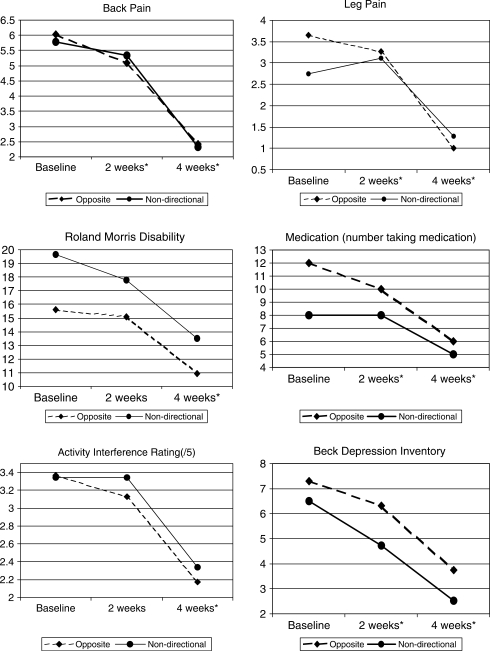
As stated above, the ITT analysis for the 96 patients given matched care appears in italics in Table 3 under the p-values for the 82 patients with complete data. The ITT analysis did not differ on the majority of variables from the p-values calculated for these 82 patients. Therefore, the data from patients with complete data at all three time points (baseline, after 2 weeks,11 and at discharge) were used to create Figure 2, which provides a visual summary of the six continuous outcomes reported in detail in Tables 2 and 3.
Figure 2.
Comparison of previously published RCT outcomes to the current series. Week 2 represents the point when treatment changed from unmatched exercises to matched exercises (current series). 2 weeks = difference from baseline to 2 weeks (end of original RCT,11 Unmatched care) 4 weeks = difference from 2 to 4 weeks (Matched care) *p ≤ 0.001; **p = 0.002; otherwise changes > 0.05
After the change to matched treatment, all outcomes demonstrated significant improvements: most p-values <0.001, and p = 0.039 for the number of patients taking medication (see Table 3 and Figure 2). Following the alternative treatment (matched, direction-specific exercises), the number of patients reporting that their pain had resolved or improved increased from 18 (22 %) to 69 (84 %) (see Table 4).
Table 4.
Subjective Global Rating of Improvement (N= 82)
| Responses after RCT with Unmatched | Responses after Change to |
|---|---|
| Treatment (Week 2)* | Matched Treatment (Week 4)** |
| My back pain is resolved | n/a |
| n=0 | |
| My back pain has improved | Resolved |
| n=15 (18%) | n=11/15 (73.3%) |
| Improved | |
| n=3/15 (20.0%) | |
| Not changed | |
| n=1/15 (6.7%) | |
| Worse | |
| n=0/15 (0.0%) | |
| My back pain has not changed much | Resolved |
| n=49 (60%) | n=23/49 (46.9%) |
| Improved | |
| n=20/49 (40.8%) | |
| Not changed | |
| n=5/49 (10.2%) | |
| Worse | |
| n=1/49 (2.0%) | |
| My back pain is worse | Resolved |
| n=18 (22%) | n=5/18 (27.8%) |
| Improved | |
| n=10/18 (55.6%) | |
| Not changed | |
| n=3/18 (16.7%) | |
| Worse | |
| n=0/18 (0.0%) | |
| Total improved or resolved | Total improved or resolved |
| n=15 (18%) | n=69 (84%) |
*Difference from baseline to 2 weeks (end of original RCT,11 Unmatched care)
**Difference from 2 to 4 weeks (Matched care)
DISCUSSION
In the initial trial11 from which this secondary analysis arose, patients with LBP, with or without lower extremity pain, were included if a baseline McKenzie/MDT assessment determined that they had a mechanical directional preference. These patients were randomly assigned to three different exercise and advice groups. While all participants received advice to remain active and to walk, cycle, or swim as tolerated, they were otherwise assigned either to exercises and advice that matched their individual directional preferences or to one of two unmatched exercise protocols, each of which included further evidence-based advice modelled after Indahl.24
Of interest in this case series were those patients who reported that their symptoms were unchanged or worse at completion of the RCT, a sub-group whose outcomes are typically “hidden” within group means and rarely studied separately. The new data reported here documents how these patients fared when offered alternative, direction-specific treatment immediately following the RCT.
Results indicated significant improvements in the second phase of treatment when patients received sub-group-specific treatment (matched/directional exercises and advice according to McKenzie/MDT principles12) compared to their outcomes in the first phase of treatment.11 In fact, their outcomes mirror very closely the outcomes achieved by the group that received matched, direction-specific exercises in the RCT,11 suggesting that their original failure to improve may have been related to inappropriate exercise prescription.
Whereas all four pain improvement scores (two groups each with back pain and leg pain scores) in these patients after termination of the RCT11 were <-1.0/10 on a numeric pain scale, by the end of the second, direction-specific phase, three of the four pain changes were >-2.0 points (-1.83 in the fourth), which represents a minimal clinically meaningful change in pain.30 Similarly, improvements in RMDQ after the first 2 weeks in the RCT were minimal, but after patients received direction-specific exercises, changes exceeded four points. The minimal level of detectable change is between four and five points for moderate disability.31 These data suggest that changes seen after direction-specific care were both statistically significant and clinically important.
Study Limitations
A number of important limitations should be recognized; these are discussed below.
Lack of Control Group
The fact that 90 % of the matched, direction-specific group reported resolution or improvement in the RCT11 effectively eliminated the option of a control group for the second phase of this series. Therefore, the possibility that changes may have occurred for some other reason (e.g., high patient expectations), or that other treatment might have been equally effective, cannot be ruled out.
While the lack of a control group in the second phase of the series was unfortunate, the mean length of the current LBP episode placed these patients outside the time frame within which good outcomes could be expected as a result of natural history (median 18.9 weeks). Two reviews of prognostic studies have shown improvement to be static after 12 weeks.32,33 The differences in outcomes between the earlier RCT and this case series were substantial, and we propose that these changes are unlikely to have arisen by chance. While these findings are promising, a study including a control group and longer-term follow-up is required to validate the results.
Unblinded Treatment
Unfortunately, it was not possible to blind therapists to the treatment they were prescribing, nor was it possible to blind patients to the fact that their exercises were being changed. The inability to blind clinicians and patients when active interventions are applied is a common challenge in physical therapy trials.34
Short-Term Follow-Up
Lack of long-term follow-up is a major limitation. Documentation of sustainability of results, recurrences, and future use of the health care system are needed to validate the current findings. This series was designed to be of short duration, with each phase of treatment limited to a 2-week interval, for two reasons. First, these limits were intended to control the number of treatments received by each group in each phase of the study (maximum of six). This maximum was exceeded (7.58) during the second phase of treatment because some sites inaccurately recorded the number of visits at discharge rather than the number of visits at 2 weeks. This data-collection error raises some questions about whether benefits were from the change in treatment or simply from receiving more treatment. Second, the short duration of treatment (2 weeks) was intended to reflect the existing literature suggesting that clinically meaningful changes can be achieved with MDT early in the course of care.9,13,17–19 This 2-week time frame met the pragmatic challenges of achieving the typical patient's primary goal of pain reduction and allowing therapists to move on to pursue strength, function, and other treatment goals.
Secondary Analysis
It should be recognized that secondary analysis of an RCT cannot depend on the sample-size calculation conducted for the original trial. However, we conducted a post-hoc sample-size calculation, with the Type I error probability set at 0.05 and a power of 0.95 to detect a mean difference of four points in the primary outcome (RMDQ), and found the sample size to be 19. This was further confirmed by the fact that we were able to reject the null hypothesis of no difference between the groups.
Future Considerations
This case series adds to the existing literature supporting an early analgesic effect from exercise prescription based on directional preference and/or centralization, resulting in improvements in self-reported disability.9–11,13,14 However, weaknesses in the study design must be recognized. Future research that compares directional preference exercises (McKenzie/MDT approach)12 to analgesics in the first 2 weeks of care might be useful. Further trials are needed to determine whether improved early pain control can create a “window of opportunity”20 that results in decreased overall use of the health care system, earlier return to work, and/or better performance with other aspects of rehabilitation.
CONCLUSION
The majority of patients with a directional preference who initially received an unmatched (inappropriate) exercise prescription and evidence-based advice reported unsatisfactory results in the RCT. This case series suggests that it may be possible to alter a patient's course from worse/not improving to improving/resolved if the treatment prescription is changed to “sub-group-specific” exercises and advice that match individuals’ directional preference (McKenzie/MDT method). In the present study, this approach appeared to provide patients with an active pain-management tool that also decreased medication use, disability, and depression scores in short-term follow-up. However, a number of weaknesses in the study design suggest that a study with longer follow-up and a control group is needed to fully validate these findings.
KEY MESSAGES
What Is Already Known on This Subject
Classification-based treatment has demonstrated improved outcomes for the management of back pain. Specific exercises based on mechanically determined directional preference have been shown to comprise a valid sub-group for classification-based treatment.
What This Study Adds
When patients with low back pain who were treated initially with exercises that were not matched to their directional preference and who failed to show improvement were prescribed exercises based on their directional preference, substantial improvements in pain and disability outcomes were obtained.
Long A, May S, Fung T. Specific directional exercises for patients with low back pain: a case series. Physiother Can. 2008;60:307-317
Footnotes
Funding: Physiotherapy Foundation of Canada, McKenzie Institute International, Cambridge Physiotherapy Associates.
Ethical Review: Community Ethics Review Board of the Alberta Heritage Foundation for Medical Research.
REFERENCES
- 1.Borkan JM, Koes B, Reis S, Cherkin DC. A report from the Second International Forum for Primary Care Research on Low Back Pain: re-examining priorities. Spine. 1998;23:1992–6. doi: 10.1097/00007632-199809150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Bouter L, Pennick V, Bombardier C. Editorial Board of Back Review Group. Cochrane Back Review Group. Spine. 2003;28:1215–8. doi: 10.1097/01.BRS.0000065493.26069.1C. [DOI] [PubMed] [Google Scholar]
- 3.Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulations: a validation study. Ann Intern Med. 2004;141:920–8. doi: 10.7326/0003-4819-141-12-200412210-00008. [DOI] [PubMed] [Google Scholar]
- 4.Delitto A, Cibulka MT, Erhard RE, Bowling RW, Tenhula JA. Evidence for use of an extension-mobilisation category in acute low back syndrome: a prescriptive validation pilot study. Phys Ther. 1993;73:216–28. doi: 10.1093/ptj/73.4.216. [DOI] [PubMed] [Google Scholar]
- 5.Erhard RE, Delitto A, Cibulka MT. Relative effectiveness of an extension program and a combined program of manipulation and flexion and extension exercises in patients with acute low back syndrome. Phys Ther. 1994;74:1093–100. doi: 10.1093/ptj/74.12.1093. [DOI] [PubMed] [Google Scholar]
- 6.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28:1363–71. doi: 10.1097/01.BRS.0000067115.61673.FF. [DOI] [PubMed] [Google Scholar]
- 7.Hicks GE, Fritz JE, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753–62. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 8.Cook C, Hegedus EJ, Ramey K. Physical therapy exercise intervention based on classification using the patent response method: a systematic review of the literature. J Manual Manip Ther. 2005;13:152–62. [Google Scholar]
- 9.Aina A, May S, Clare H. Centralization of spinal symptoms—a systematic review of a clinical phenomenon. Manual Ther. 2004;9:134–43. doi: 10.1016/j.math.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 10.George SZ, Bialosky JE, Donald DA. The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute low back pain: a preliminary investigation involving patients classified for specific exercise. J Orthop Sport Phys Ther. 2005;35:580–8. doi: 10.2519/jospt.2005.35.9.580. [DOI] [PubMed] [Google Scholar]
- 11.Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29:2593–602. doi: 10.1097/01.brs.0000146464.23007.2a. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie RA, May S. Lumbar spine mechanical diagnosis and therapy. 2nd. Waikanae: Spinal Publications NZ; 2003. [Google Scholar]
- 13.Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. Spine. 1999;24:676–83. doi: 10.1097/00007632-199904010-00012. [DOI] [PubMed] [Google Scholar]
- 14.Werneke M, Hart DL. Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine. 2001;26:758–65. doi: 10.1097/00007632-200104010-00012. [DOI] [PubMed] [Google Scholar]
- 15.Long AL. The centralization phenomenon: its usefulness as a predictor of outcome in conservative treatment of chronic low back pain (a pilot study) Spine. 1995;20:2513–21. [PubMed] [Google Scholar]
- 16.Karas R, McIntosh G, Hall H, Wilson L, Melles T. The relationship between nonorganic signs and centralization of symptoms in the prediction of return to work for patients with low back pain. Phys Ther. 1997;77:354–60. doi: 10.1093/ptj/77.4.354. [DOI] [PubMed] [Google Scholar]
- 17.Donelson R, Murphy K, Silva G. Centralisation phenomenon: its usefulness in evaluating and treating referred pain. Spine. 1990;15:211–13. [PubMed] [Google Scholar]
- 18.Donelson R, Grant W, Kamps C, Medcalf R. Pain response to sagittal end-range spinal motion: a prospective, randomized multicentered trial. Spine. 1991;16:S206–12. doi: 10.1097/00007632-199106001-00006. [DOI] [PubMed] [Google Scholar]
- 19.Sufka A, Hauger B, Trenary M, Bishop B, Hagen A, Lozon R, et al. Centralisation of low back pain and perceived functional outcome. J Orthop Sport Phys Ther. 1998;27:205–12. doi: 10.2519/jospt.1998.27.3.205. [DOI] [PubMed] [Google Scholar]
- 20.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/sub-acute “non-specific” low back pain. Spine. 2006;31:623–31. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 21.Fritz JM, Delitto A, Vignovic M, Busse RG. Interrater reliability of judgements of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil. 2000;81:57–61. doi: 10.1016/s0003-9993(00)90222-3. [DOI] [PubMed] [Google Scholar]
- 22.Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Inter-tester reliability of low back pain assessment using the McKenzie method. Spine. 2002;27:E207–14. doi: 10.1097/00007632-200204150-00016. [DOI] [PubMed] [Google Scholar]
- 23.Razmjou H, Kramer JF, Yamada R. Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. J Orthop Sport Phys Ther. 2000;30:368–89. doi: 10.2519/jospt.2000.30.7.368. [DOI] [PubMed] [Google Scholar]
- 24.Indahl A, Velund L, Reikeraas O. Good prognosis for back pain patients when left untampered: a randomized clinical trial. Spine. 1995;20:473–7. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 25.Waddell G, MacIntosh A, Hutchinson A, Feder G, Lewis M. Low back pain evidence review. London: Royal College of General Practitioners; 1999. [Google Scholar]
- 26.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain—what works? Pain. 2004;107:176–90. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 27.Hettinga DM, Jackson A, Moffet JK, May S, Mercer C, Woby SR. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for non-specific low back pain of at least 6 weeks duration. Physical Therapy Reviews. 2007;12:221–32. [Google Scholar]
- 28.Hubley-Kozey CL, McCulloch TA, McFarland DH. Chronic low back pain: a critical review of specific therapeutic exercise protocols on musculoskeletal and neuromuscular parameters. J Manual Manip Ther. 2003;11:78–87. [Google Scholar]
- 29.Van Tulder M, Malmivaara A, Esmail R, Koes B. Exercise therapy for low back pain. Spine. 2000;25:2784–96. doi: 10.1097/00007632-200011010-00011. [DOI] [PubMed] [Google Scholar]
- 30.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30:1331–4. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 31.Stratford PW, Binkley J, Solomon P, Finch E, Gill C, Moreland J. Defining the minimum level of detectable change for the Roland-Morris Questionnaire. Phys Ther. 1996;76:359–65. doi: 10.1093/ptj/76.4.359. [DOI] [PubMed] [Google Scholar]
- 32.Abbott JH, Mercer SR. The natural history of acute low back pain. NZ J Physiother. 2002;30:8–16. [Google Scholar]
- 33.Pengel LHM, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. Brit Med J. 2003;327:323–5. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mannion A, Müntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24:2435–48. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]