Abstract
Purpose:
The purposes of this study were to quantitatively examine hip abductor strength in patients presenting with iliotibial band friction syndrome (ITBFS) and to determine whether a multi-modal physiotherapy approach, including hip abductor strengthening, might play a role in recovery.
Method:
Our observational, pretest–posttest study is one of the first prospective studies in this area. Patients presenting to physiotherapy with unilateral ITBFS were recruited to participate. Participants followed a 6-week rehabilitation programme designed to strengthen hip abductors; strength was measured every 2 weeks using a hand-held dynamometer and compared bilaterally.
Results:
Sixteen subjects (five men, 11 women) aged 20 to 53 years participated. All but 2 reported running as one of their main physical activities. A trend toward a significant difference in hip abductor strength was found between the injured and uninjured sides at baseline, but this difference disappeared by 6 weeks. Hip abductor strength was significantly related to physical function at weeks 2, 4, and 6. Nine subjects were discharged from physiotherapy after the 6-week period, while the other 7 subjects continued attending for up to 5 months.
Conclusions:
Hip abductor strengthening appeared to be beneficial in the treatment of ITBFS, but further research on the use of hip abductor strengthening for treatment and prevention of ITBFS is needed.
Keywords: Physiotherapy, Physical Therapy, hip abduction, iliotibial band, injury, rehabilitation, strength
RÉSUMÉ
Objectif :
Cette étude a pour but d’examiner quantitativement la force de l’adducteur de la hanche chez les patients atteints du ressaut de la bandelette de Maissiat (ITBFS), et de déterminer si une approche de physiothérapie multimodale, incluant le renforcement de l’adducateur de la hanche, peut jouer un rôle dans le rétablissement.
Méthode :
Notre étude observationnelle avant et après le test est la première étude prospective dans ce domaine. On a recruté la participation de patients qui se présentaient en physiothérapie avec un ITBFS unilatéral. Les participants ont suivi un programme de réadaptation de six semaines conçu en vue de renforcer les adducteurs de la hanche. La force musculaire a été mesurée toutes les deux semaines, à l’aide d’un dynamomètre tenu à la main, et comparée bilatéralement.
Resultats :
Seize sujets (cinq hommes, 11 femmes) âgés de 20 à 53 ans ont participé. Tous sauf deux avaient signalé que la course était leur principale activité physique. Une tendance vers une différence importante dans la force de l’adducteur de la hanche s’est manifestée entre le côté blessé et le côté sain à la ligne de base, mais cette différence est disparue après six semaines. La force de l’adducteur de la hanche était considérablement liée à la fonction physique aux semaines 2, 4 et 6. Neuf sujets ont obtenu leur congé de la physiothérapie après la période de six semaines, tandis que les sept autres ont continué les traitements pendant un maximum de cinq mois.
Conclusions :
Le renforcement de l’adducteur de la hanche semblait être bénéfique dans le traitement de l’ITBFS mais on devra s’adonner à des recherches plus poussées sur le recours au renforcement de l’adducteur de la hanche pour le traitement et la prévention de l’ITBFS.
Mots clés: adduction de la hanche, bandelette de Maissiat, blessure, réadaptation, force
INTRODUCTION
Iliotibial band friction syndrome (ITBFS) is a common overuse injury of the knee that occurs as a result of repetitive soft-tissue trauma.1,2 The iliotibial band (ITB) is a thick strip of fascia that originates from the tubercle of the iliac crest, continues down the lateral side of the thigh, and inserts into the lateral tibial condyle (Gerdy's tubercle) and into the lateral proximal fibular head.3,4 ITBFS arises when friction occurs between the posterior edge of the ITB and the underlying lateral femoral epicondyle. When the knee is flexed to an angle greater than ∼30°, the ITB lies posterior to the lateral femoral epicondyle; when the knee is extended, however, the ITB moves anterior to this landmark. Therefore, friction occurs at or at slightly less than 30° of knee flexion, when the ITB crosses over the lateral femoral epicondyle.3 The cumulative effect of excess friction causes an inflammatory reaction within the iliotibial tract, underlying bursa, and/or periosteum of the lateral femoral epicondyle, inducing lateral knee pain.2–5
ITBFS seems to result from a combination of intrinsic and extrinsic factors, but there is much debate in the literature over its causes. Some intrinsic factors that have been implicated in its development include genu varum, tibial varum, subtalar varus, subtalar valgus, forefoot varus, discrepancies in leg length, increased Q angle, prominent lateral femoral condyles, cavus feet, and excessive pronation.3–7 ITB flexibility deficits and hip abductor weakness have also been found to play a role in the development of ITBFS.1,4 In addition, extrinsic factors including excessive running, a sudden increase in running mileage, downhill running, improper or worn footwear, and dual-density midsole shoes have been associated with ITBFS.2–9
ITBFS is commonly referred to as “runner's knee,” since it is most common in distance runners.2,4,10 It is also commonly seen in cyclists and military personnel.11 The incidence of ITBFS in runners seems to be on the rise. A study published in 1981 by McNicol et al.6 reported only 52 cases of ITBFS in 1,047 overuse running injuries (5.0%); single severe training sessions and functional overpronation were the most significant factors contributing to ITBFS in this study.6 Two more recent studies of running injuries by Taunton et al. and Macintyre et al., however, both found ITBFS to be the second most common cause of injury in runners, exceeded only by patellofemoral pain syndrome.7,9 In the Taunton et al. study, 168 of the 2,002 running injuries (8.4%) were diagnosed as ITBFS. Hip abductor weakness, leg-length discrepancies, and a history of downhill running were the most significant factors contributing to its onset.7 Overall, the incidence of ITBFS in runners has been found to be in the range of 1.6% to 12%.1,5
The purposes of this prospective, observational, pretest–posttest study were to quantitatively examine hip abductor strength in patients presenting with ITBFS and to determine whether a multi-modal physiotherapy approach, including hip abductor strengthening, might play a role in recovery from this overuse injury, allowing for successful return to activity. Little research has quantitatively examined the aetiology of ITBFS; most studies have been retrospective and suggest only possible causes of the condition. This study is meant to broaden our understanding of the relationship between hip abductor strength and rehabilitation outcomes in patients with ITBFS.
METHODS
Sixteen patients presenting to physiotherapy at the Allan McGavin Sports Medicine Centre in Vancouver, British Columbia, with unilateral ITBFS, were recruited to participate in the study. ITBFS was diagnosed in all participants by one of two qualified physiotherapists, each of whom has more than 10 years’ experience; 12 participants were diagnosed by one therapist and 2 participants by the other therapist based on patient history and presentation, including lateral knee pain with or without physical activity. Participants who displayed signs or symptoms of other knee pathologies (e.g., meniscal tears, degenerative joint disease, patellofemoral pain) were excluded from the study. Other knee pathologies were ruled out by the same physiotherapist, again based on patient history, presentation, and assessment. As well, any subject who had a history of knee surgery or knee trauma to the affected side or who had already received treatment for ITBFS was excluded from the study. This study was approved by the Clinical Research Ethics Board of the University of British Columbia. All subjects were required to sign an informed consent prior to taking part.
Bilateral hip abductor strength was measured at 0, 2, 4, and 6 weeks using a hand-held Nicholas Dynamometer (Lafayette Instrument Co., Lafayette, IN). This dynamometer reportedly measures static force with accuracy to 0.1 kg ± 2%.12 One investigator performed all dynamometer strength measurements. Hand-held dynamometry has been shown to be a reliable assessment technique, with a median test–retest correlation of 0.97 (p < 0.01), when practiced by a single investigator.13 Height, weight, leg length (anterior superior iliac spine to medial malleolus), and thigh length (anterior superior iliac spine to medial joint line) were also measured, and information regarding age, main activities, knee-injury history, and previous treatment for ITBFS was collected. As well, all subjects completed the Allan McGavin Health Status Index (AMI) each time the hip strength measurements were taken. The AMI, a quality-of-life tool designed specifically for sports medicine, contains items assessing physical function, activity level, emotional behaviour, and pain. Pain during daily living, pain during activity, and night pain are assessed on three separate five-point numeric rating scales (NRS). This index has been validated psychometrically and is in the process of publication.
Hip Abduction Testing Protocol
Participants were instructed to assume a side-lying position with top hips extended, slightly externally rotated, and abducted to 30° in order to isolate the gluteus medius, as described by Kendall.14 Bottom knees were flexed for stability. The dynamometer was applied just proximal to the lateral malleolus to obtain a longer lever, and pressure was applied downward toward adduction.14 To ensure that participants were not rolling backward, they were positioned to keep their backs flat against a wall during the test. Participants were instructed to resist movement by maintaining an isometric contraction, and peak hip abductor strength was measured with the hand-held dynamometer. Each subject performed five consecutive experimental trials bilaterally, with 10-second rest intervals between trials. The mean value of the five trials was calculated for each lower extremity (LE).15 Injured and uninjured hips (ITBFS vs. normal LE) were tested in random order.
The Rehabilitation Programme
The rehabilitation programme used in this study was designed by the same two experienced physiotherapists and focused on improving hip abductor strength. Participants attended physiotherapy one or two times per week for 6 weeks. All strength exercises and stretches were taught to the subjects during their regular physiotherapy visits. Exercises were supervised during therapy; however, subjects were not supervised while doing their exercises at home.
The rehabilitation programme included three strength exercises: a side-lying hip abduction exercise, a standing pelvic stabilization exercise, and forward-backward lunges. Table 1 summarizes the weekly progressions of these exercises. All strength exercises were performed for two consecutive days, followed by one day off.
Table 1.
Progression of Strength Exercises
| Exercise | Week | # Sets | # Reps | Hold | Rest | Resistance |
|---|---|---|---|---|---|---|
| Side-lying hip abduction exercise | Week 1 | 1 | 10 | 10 sec | 10 sec | ∼ |
| Week 2 | 2 | 10 | 10 sec | 10 sec | ∼ | |
| Week 3 | 2 | 10 | 15 sec | 10 sec | ∼ | |
| Week 4 | 2 | 10 | 10 sec | 10 sec | green theraband | |
| Week 5 | 2 | 10 | 15 sec | 10 sec | green theraband | |
| Week 6 | 2 | 12 | 15 sec | 10 sec | green theraband | |
| Standing pelvic stabilization exercise | Week 1 | 1 | 5 | 5 sec | 5 sec | green theraband |
| Week 2 | 1 | 10 | 5 sec | 5 sec | green theraband | |
| Week 3 | 2 | 10 | 5 sec | 5 sec | green theraband | |
| Week 4 | 2 | 10 | 8 sec | 5 sec | green theraband | |
| Week 5 | 2 | 10 | 10 sec | 5 sec | green theraband | |
| Week 6 | 2 | 10 | 10 sec | 5 sec | green theraband | |
| Forward-backward lunges | Week 4 | 1 | 5/side | ∼ | ∼ | ∼ |
| Week 5 | 1 | 8/side | ∼ | ∼ | ∼ | |
| Week 6 | 1 | 10/side | ∼ | ∼ | ∼ |
Reps = repetitions
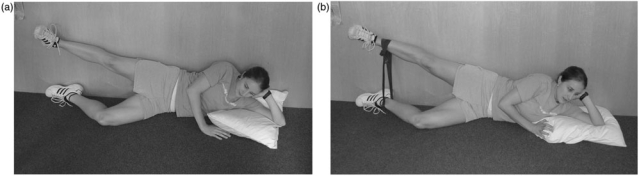
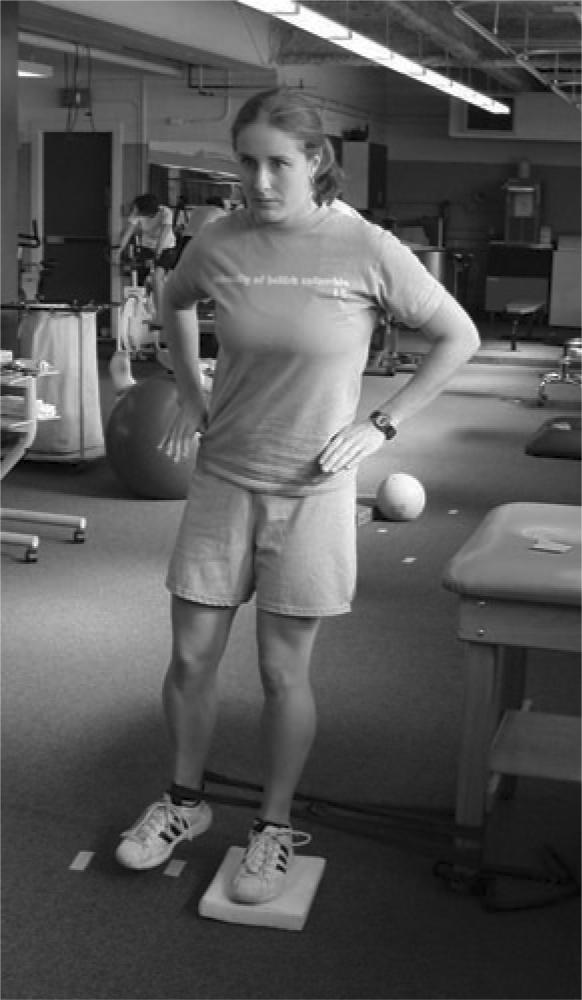
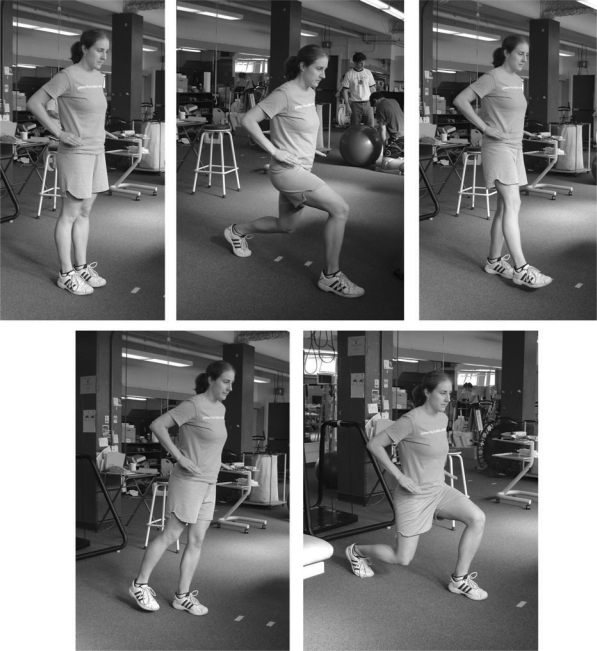
The side-lying hip abduction exercise (Figure 1a) was a gluteus medius isometric contraction held at approximately 30° of hip abduction with slight hip external rotation and neutral hip extension.14 This exercise was done with the back against a wall. In the fourth week, a 1-metre-long green theraband was added around the ankles (Figure 1b). The standing pelvic stabilization exercise (Figure 2) was another isometric contraction. Subjects stood on the affected leg and then abducted and held the unaffected LE using the same green theraband. They were instructed to stabilize the pelvis and to keep it level throughout the exercise. Finally, forward-backward lunges (Figure 3) were performed starting in the fourth week. Subjects were again told to keep the pelvis level while performing this exercise. Keeping one foot planted, subjects lunged forward with the other leg before rising and lunging backward with the same leg. This was considered one repetition.
Figure 1.
Side-lying hip abduction exercise (a) without theraband for first 3 weeks; (b) with theraband for last 3 weeks.
Figure 2.
Standing pelvic stabilization exercise.
Figure 3.
Forward-backward lunges.
The rehabilitation programme also involved two ITB stretches: a standing stretch (Figure 4) and a side-lying “pretzel” stretch (Figure 5). Stretches were maintained for 60 seconds each and conducted twice daily for the entirety of the programme. As well, ultrasound to the area of discomfort was used during regular physiotherapy visits. Continuous ultrasound at 0.5W/cm2 × 3mHz ×5 minutes was used during the first week; this was increased to 1.0W/cm2 × 3mHz × 5 minutes for the remaining 5 weeks. The programme also involved correcting any pelvic malalignment using muscle energy techniques and self-correction exercises. In addition, participants were educated to avoid painful activities (e.g., no running) until their pain was controlled, and then gradual reintroduction of activity was recommended.
Figure 4.
Standing iliotibial band stretch (for left side).
Figure 5.
Side-lying “pretzel” stretch (for right side).
Participants were asked to keep track of their daily rehabilitation exercises and activities in an activity log, which was used to help monitor and promote adherence to the rehabilitation programme.
Data Analysis
The hand-held dynamometer measured hip abductor strength in kilograms, which were converted to Newtons (N) [kg × 9.81] and then to moments (N*m) [N ×action length (leg length or thigh length)]. A formula was used to standardize hip abduction moments for differences in height and weight among subjects. The formula used to calculate these dimensionless moments was
% (BW × h) = Moment (N × m) × 100/BW × h
where BW is body weight in Newtons and h is height in metres.1
All data were entered into JMP Version 4.0 (SAS Institute Inc., Cary, NC). Regression analysis was used to examine hip abductor moments versus the different AMI domains at the four testing times. Paired t-tests were used to examine hip abductor moments of the injured and uninjured LE at the four testing times.
RESULTS
Nineteen participants were recruited for the study, but only 16 (5 men, 11 women) completed the protocol. There were three dropouts (all women): one was too busy to attend physiotherapy, one developed a hip injury and could not perform the rehabilitation exercises, and one stopped attending physiotherapy because it was too expensive. The subjects’ ages ranged from 20 to 53 years, with a mean age of 33.7 years (SD = 10.2 years). Height, weight, and body mass index (BMI) averages are summarized in Table 2. Based on BMI norms from the American College of Sports Medicine,16 one subject was underweight, with a BMI of less than 18.5 kg/m2 (18.2 kg/m2); four subjects were overweight, with BMIs between 25.0 kg/m2 and 29.9 kg/m2 (25.3, 25.7, 25.8, 28.2 kg/m2); and the rest were in the normal range, between 18.5 kg/m2 and 24.9 kg/m2. There were 10 injured left knees and 6 injured right knees. Four subjects had a leg length discrepancy of 2 cm or more; in 2 cases the affected side was longer and in 2 cases the unaffected side was longer.
Table 2.
Subject Anthropometric Characteristics
| Characteristic | Minimum–Maximum | Mean | SD |
|---|---|---|---|
| Weight (kg) | 54.5–83.2 | 68.0 | 9.5 |
| Height (m) | 1.6–1.9 | 1.7 | 0.1 |
| BMI (kg/m2) | 18.2–28.2 | 22.9 | 2.7 |
BMI = body mass index
All but two participants (87.5%) reported running as one of their main physical activities. Biking and gym workouts were the second most common activities, with five subjects (31.3% each) participating in each, while four (25.0%) listed skiing as a main physical activity. Walking, yoga/Pilates, swimming, golf, tennis, soccer, and volleyball were each listed as a main physical activity by two participants (12.5% each).
When hip abductor moments were examined using a paired t-test, a trend toward a significant difference in strength was found between the affected and unaffected limbs at 0 weeks, with the affected side being weaker (p = 0.05). At 6 weeks, however, this difference had disappeared (p = 0.29). After correction for multiple comparisons, the alpha level for 95% confidence was 0.013. See Table 3 for the means and standard deviations of each group.
Table 3.
Injured vs. Uninjured Hip Abductor Moments as Measured by Nicholas Dynamometer
| Hip Abductor Moment— Injured (N*m) |
Hip Abductor Moment—Uninjured (N*m) |
||||
|---|---|---|---|---|---|
| Testing Time | Mean | SD | Mean | SD | p* |
| 0 weeks | 25.5 | 7.7 | 28.9 | 8.7 | 0.05 |
| 6 weeks | 30.5 | 7.7 | 29.4 | 8.8 | 0.29 |
*α = 0.013 (95% CI)
Regression analysis was used to relate hip abductor moments of the affected side with the different domains of the AMI. A trend toward significance was found only between the physical function domain of the AMI and hip abductor moments of the affected side at weeks 2, 4, and 6 (see Table 4). After correction for multiple comparisons, the alpha level for 95% confidence was 0.003. The physical function domain of the AMI asked subjects about their limitations in 10 everyday activities: strenuous activity (e.g., lifting heavy objects, moving furniture), moderate activity (e.g., cleaning household, raking leaves), lifting or carrying groceries, dressing, bathing and self-care, sexual function, ascending/descending stairs, walking 2 km, walking one block, and crouching or kneeling.
Table 4.
Hip Abductor Moments of Injured Side by Allan McGavin Health Status Index (AMI) Domains
| AMI Domain | Testing Time | Mean AMI Score | Mean Hip Abductor Moment— Injured (N*m) | Regression Analysis |
|
|---|---|---|---|---|---|
| p* | r2 | ||||
| Physical Function | 0 weeks | 26.9 / 30 | 25.5 | > 0.05 | 0.01 |
| 2 weeks | 28.4 / 30 | 27.5 | 0.023 | 0.32 | |
| 4 weeks | 28.6 / 30 | 28.5 | 0.044 | 0.26 | |
| 6 weeks | 28.6 / 30 | 30.5 | 0.021 | 0.35 | |
| Emotional/Mental | 0 weeks | 19.1 / 25 | 25.5 | > 0.05 | 0.07 |
| 2 weeks | 18.9 / 25 | 27.5 | > 0.05 | 0.10 | |
| 4 weeks | 20.1 / 25 | 28.5 | > 0.05 | 0.04 | |
| 6 weeks | 20.4 / 25 | 30.5 | > 0.05 | 0.11 | |
| Pain | 0 weeks | 11.1 / 15 | 25.5 | > 0.05 | 0.00 |
| 2 weeks | 13.3 / 15 | 27.5 | > 0.05 | 0.11 | |
| 4 weeks | 13.3 / 15 | 28.5 | > 0.05 | 0.07 | |
| 6 weeks | 13.9 / 15 | 30.5 | > 0.05 | 0.13 | |
| Activity/Role | 0 weeks | 13.5 / 30 | 25.5 | > 0.05 | 0.13 |
| 2 weeks | 15.4 / 30 | 27.5 | > 0.05 | 0.00 | |
| 4 weeks | 17.3 / 30 | 28.5 | > 0.05 | 0.03 | |
| 6 weeks | 18.8 / 30 | 30.5 | > 0.05 | 0.00 | |
| Aggregate of All Domains | 0 weeks | 70.6 / 100 | 25.5 | > 0.05 | 0.10 |
| 2 weeks | 75.9 / 100 | 27.5 | > 0.05 | 0.11 | |
| 4 weeks | 79.2 / 100 | 28.5 | > 0.05 | 0.02 | |
| 6 weeks | 81.6 / 100 | 30.5 | > 0.05 | 0.10 | |
α = 0.03 (95% CI)
All participants were required to attend physiotherapy for at least 6 weeks, but many continued with their therapy beyond what was required for the study. At week 6, only four participants were completely pain free during physical activity (see Table 5). Adherence to the rehabilitation programme was good, based on the activity logs. No participant missed more than 5 days of exercise.
Table 5.
Bilateral Hip Abductor Torque Differences and Self-Reported Pain with Physical Activity
| Participant | Bilateral Hip Abductor Moment Differences, uninjured–injured (N*m) |
Lateral Knee Pain with Physical Activity on NRS (/5) |
# Weeks Attended PT‡ | ||||
|---|---|---|---|---|---|---|---|
| 0 weeks | 6 weeks | Change | 0 weeks | 6 weeks | Change | ||
| 1 | −0.2 | 0.4 | −0.6 | 2.1 | 0 | 2.1 | 6 |
| 2 | 3.9 | −2.4 | 6.3 | 1.4 | 0.3 | 1.1 | 21 |
| 3 | −1.2 | 3 | −4.2 | 4.8 | 4.9 | −0.1 | 6 |
| 4 | 1.1 | −2.9 | 4 | 4.8 | 0 | 4.8 | 9 |
| 5 | 5.3 | −2.3 | 7.6 | 4.1 | 0 | 4.1 | 11 |
| 6 | 2.9 | −3 | 5.9 | 3.5 | 2.7 | 0.8 | 11 |
| 7 | 3.5 | 3.4 | 0.1 | 4.2 | 0.6 | 3.6 | 13 |
| 8 | 0.8 | −8.8 | 9.6 | 4.8 | 0 | 4.8 | 6 |
| 9 | 8.4 | 0.2 | 8.2 | 0.3 | 0.8 | −0.5 | 6 |
| 10 | 1.5 | −4.5 | 6 | 4.8 | 1.1 | 3.7 | 8 |
| 11 | −0.2 | 1 | −1.2 | 4.3 | 3.9 | 0.4 | 7 |
| 12 | −1.5 | 6.2 | −7.7 | 3.2 | 0.2 | 3 | 8 |
| 13 | 3.3 | 3.2 | 0.1 | 2.8 | 1 | 1.8 | 8 |
| 14 | 11 | −1.6 | 12.6 | 3.9 | 0.1 | 3.8 | 6 |
| 15 | 3 | −4.1 | 7.1 | 4.3 | 0.8 | 3.5 | 6 |
| 16 | 3.5 | −4.1 | 7.6 | 1.9 | 1.9 | 0 | 7 |
| Mean | 2.82 | −1.02 | 3.84 | 3.45 | 1.14 | 2.31 | 8.7 |
| SD | 3.35 | 3.80 | 5.50 | 1.38 | 1.49 | 1.83 | 3.93 |
NRS = numeric rating scale; PT = physical therapy
DISCUSSION
Fredericson et al. found hip abductor weakness in people with ITBFS and concluded that improvement in hip abductor strength paralleled symptom improvement.1 These authors hypothesized that weak hip abductors increase the amount of thigh adduction, thigh internal rotation, and valgus stress at the knee while running.1 Together, these forces place added tension on the ITB, making it more vulnerable to impingement on the lateral femoral epicondyle at foot strike of the gait cycle.1
In our study, hip abductor weakness was also observed in the affected limb, which may have contributed to the lateral knee pain experienced. The injured side was weaker than the uninjured side at week 0; however, this difference only approached significance. It is possible, however, that the small sample size in this study may not have provided sufficient power to detect a difference. The strength difference seen at week 0 disappeared by week 6, suggesting that the rehabilitation programme was successful. It must be kept in mind that no control group was used in this study; the difference found between hip abductor strength of the injured and uninjured limbs at week 0 and the subsequent absence of a difference at week 6 could be attributed to extraneous factors that were not tested. It is possible that the other physiotherapy interventions (stretching, ultrasound, pelvic alignment corrections), or possibly even rest alone, contributed to correcting the strength imbalances. For instance, Verbunt at al. concluded that patients with chronic low back pain who reported higher levels of pain tended to have increased inhibition of muscle activity of the quadriceps, leading to sub-maximal performance.17 Hip abductor strength could be affected in a similar manner when people experience lateral knee pain from ITBFS. The effects of stretching, ultrasound, pelvic alignment corrections, and rest were not monitored in this study, but these factors may have played a role in reducing the pain and restoring strength to normal. More research in this area is needed.
The stretching exercises included in the rehabilitation programme may have contributed to the resolution of ITBFS symptoms in another way as well. It is thought that the ITB is under greater strain when there are flexibility deficits, facilitating impingement on the lateral femoral epicondyle.3 Further research is needed to examine the possible role of strength and flexibility training in the prevention of ITBFS.
Hip abductor moments were related to the physical function domain of the AMI at weeks 2, 4, and 6. This means that as hip abduction in the affected limb became stronger, subjects reported a higher level of physical functioning. Despite the fact that hip abductor moments were not related to physical function at week 0, the relationships at weeks 2, 4, and 6 further suggest efficacy of the rehabilitation programme.
Several study limitations should be mentioned. An a priori power analysis was not completed, and, after correction for multiple comparisons, the alpha levels needed for 95% confidence were quite low. This is a major limitation of the study; that is, there is legitimate risk of a type 1 error (false positive). However, this prospective case series provides only an introductory look at the relationship of quality of life to rehabilitation and resulting changes in hip abductor strength. We were interested solely in examining descriptive changes in strength over a 6-week rehabilitation period.
Fewer men (31.3%) than women (68.7%) participated in the study, mirroring the gender breakdown seen clinically. Whether this gender difference in injury rate is real or whether women seek therapy more often than men is not known.
None of the subjects was considered obese based on ACSM BMI normative data.16 Running was listed as the most common activity triggering ITBFS, in agreement with the literature.2,10 The repeated flexion and extension of the knee during running, which causes the ITB to continually cross over the lateral femoral epicondyle, is a likely contributing factor.
Extrinsic factors such as excessive training, a sudden increase in training volume, training terrain, and improper or worn footwear also seemed to contribute to ITBFS.2–9 Although we did not focus on these variables, they should be included in future research. It is possible that other factors caused both the symptoms of ITBFS and the hip abductor weakness seen in participants in this study.
Study participants attended physiotherapy for between 1.5 and 5 months. Their mean recovery time is similar to that reported by Barber and Sutker, who concluded that symptoms of ITBFS usually persist for 2 to 6 months.2 ITBFS often becomes chronic, and more successful treatments need to be developed. More research comparing control groups to different treatment combinations (e.g., no treatment vs. physiotherapy treatment without strengthening vs. physiotherapy treatment with strengthening) is needed. Inclusion of control groups would help increase internal validity, which was threatened in this one-group, pretest–posttest study.
CONCLUSION
ITBFS is a common overuse injury seen especially in runners, and its possible causes are debated in the literature. Although hip abductor weakness is often associated with this injury, whether this weakness is the cause of the lateral knee pain or the result of it cannot be determined from our data. In this study, increases in hip abductor strength were observed over the course of the 6 weeks during which the participants were taking part in the standardized rehabilitation programme, and these strength changes seemed to parallel decreases in the symptoms of ITBFS. Because of the study's design, however, it is unclear exactly how much of the symptom resolution was due to strength changes and how much may have been due to other factors. In addition, it is not known whether the observed strength changes resulted from the strengthening exercises or from symptom improvement. Despite its limitations, however, this study is of high clinical interest and appears to support the inclusion of hip abductor strengthening into a rehabilitation programme designed for treatment of ITBFS. This is one of the few prospective studies in this area. Additional prospective studies incorporating control groups are needed to examine whether hip abductor strengthening should be used for prevention and treatment of this common overuse injury.
KEY MESSAGES
What Is Already Known on This Subject
Iliotibial band friction syndrome (ITBFS) seems to result from a combination of intrinsic and extrinsic factors, but there is much debate in the literature over its causes. Until now, little research has quantitatively examined the etiology of ITBFS, and most studies have been retrospective; they can therefore only suggest possible causes of the condition.
What This Study Adds
Our prospective case series appears to support the inclusion of hip abductor strengthening into a rehabilitation programme designed for treatment of ITBFS, which is of high clinical interest to all physiotherapists treating this common overuse injury.
Acknowledgments
The authors thank the Nike Global Research Foundation for their financial support.
Beers A, Ryan M, Kasubuchi Z, Fraser S, Taunton JE. Effects of multi-modal physiotherapy, including hip abductor strengthening, in patients with iliotibial band friction syndrome. Physiother Can. 2008;60:180-188.
Footnotes
This study was approved by the Clinical Research Ethics Board of the University of British Columbia.
REFERENCES
- 1.Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10:169–75. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Barber FA, Sutker AN. Iliotibial band syndrome. Sport Med. 1992;14:144–8. doi: 10.2165/00007256-199214020-00005. [DOI] [PubMed] [Google Scholar]
- 3.Orchard JW, Fricker PA, Abud AT, Mason BR. Biomechanics of iliotibial band friction syndrome in runners. Am J Sport Med. 1996;24:375–9. doi: 10.1177/036354659602400321. [DOI] [PubMed] [Google Scholar]
- 4.Krivickas LS. Anatomical factors associated with overuse sports injuries. Sport Med. 1997;24:132–46. doi: 10.2165/00007256-199724020-00005. [DOI] [PubMed] [Google Scholar]
- 5.Messier SP, Edwards DG, Martin DF, Lowery RB, Cannon DW, James MK, et al. Etiology of iliotibial band friction syndrome in distance runners. Med Sci Sport Exerc. 1995;27:951–60. doi: 10.1249/00005768-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 6.McNicol K, Taunton JE, Clement DB. Iliotibial tract friction syndrome in athletes. Can J Appl Sport Sci. 1981;6:76–80. [PubMed] [Google Scholar]
- 7.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Brit J Sport Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKenzie DC, Clement DB, Taunton JE. Running shoes, orthotics, and injuries. Sport Med. 1985;2:334–47. doi: 10.2165/00007256-198502050-00003. [DOI] [PubMed] [Google Scholar]
- 9.Macintyre JG, Taunton JE, Clement DB, Lloyd-Smith DR, McKenzie DC, Morrell RW. Running injuries: a clinical study of 4,173 cases. Clin J Sport Med. 1991;1:81–7. [Google Scholar]
- 10.Sutker AN, Jackson DW, Pagliano JW. Iliotibial band friction syndrome in distance runners. Phys Sport Med. 1981;9(10):69–73. doi: 10.1080/00913847.1981.11711185. [DOI] [PubMed] [Google Scholar]
- 11.Kirk KL, Kuklo T, Klemme W. Iliotibial band friction syndrome. Orthopedics. 2000;23:1209–14. doi: 10.3928/0147-7447-20001101-24. [DOI] [PubMed] [Google Scholar]
- 12.Marino M, Nicholas JA, Gleim GW. The efficacy of manual assessment of muscle strength using a new device. Am J Sport Med. 1982;10:360–4. doi: 10.1177/036354658201000608. [DOI] [PubMed] [Google Scholar]
- 13.Bohannon RW. Test–retest reliability of hand-held dynamometry during a single session of strength assessment. Phys Ther. 1986;66:206–9. doi: 10.1093/ptj/66.2.206. [DOI] [PubMed] [Google Scholar]
- 14.Kendall FP, McGreary EK, Provance PG. Muscles: testing and function. 4th. Baltimore: Williams & Wilkins; 1993. [Google Scholar]
- 15.Whitley JD, Smith LE. Larger correlations obtained by using average rather than “best” strength scores. Res Q. 1963;34:248–9. [Google Scholar]
- 16.American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 7th. Baltimore: Lippincott Williams & Wilkins; 2006. [DOI] [PubMed] [Google Scholar]
- 17.Verbunt JA, Seelen HA, Vlaeyen JW, Bousema EJ, van der Heijden GJ, Heuts PH, et al. Pain-related factors contributing to muscle inhibition in patients with chronic low back pain: an experimental investigation based on superimposed electrical stimulation. Clin J Pain. 2005;21:232–40. doi: 10.1097/00002508-200505000-00006. [DOI] [PubMed] [Google Scholar]