Abstract
Most studies of decisions to curtail alcohol consumption reflect experiences of abusing drinkers. We employ an exploratory sequential research design to explore the applicability of this research to the experience of nonabusing drinkers advised to curtail alcohol consumption after a Hepatitis C diagnosis. A qualitative component identified 17 new decision factors not reflected in an inventory of factors based on synthesis of existing scales. We triangulated qualitative data by supplementing semi-structured interviews with Internet postings. A quantitative component estimated prevalence and association with current drinking of these new decision factors. Patients who quit drinking tended to attribute post-diagnosis drinking to occasional triggers, whereas patients who were still drinking were more likely to endorse rationales not tied to specific triggers.
Keywords: alcohol consumption, drinking decisions, nonabusing drinkers, hepatitis C, mixed methods
Introduction
Drinking even moderate amounts of alcohol is contraindicated for patients with a number of medical conditions that are not alcohol-related but may benefit from reducing alcohol consumption, e.g., patients with chronic hepatitis or other types of hepatic disease and gastrointestinal ulcers (Hobbs, Rall & Verdoorn, 1996). Additionally acute alcohol use can increase sedation associated with antihistamines, narcotic pain relievers, antidepressants, antipsychotic medications, and sleeping pills, whereas persistent use may decrease the effectiveness of anticoagulants such as warfarin, and in combination with antipsychotics may result in liver damage (National Institute on Alcohol Abuse and Alcoholism, 1995). Most research on alcohol consumption decisions has focused on patients with alcohol abuse or dependence. We do not know whether factors influencing alcohol consumption decisions among abusive drinkers adequately reflect consumption decisions among nonabusing drinkers advised to stop drinking for medical reasons not related to alcohol, or whether there are additional predictors unique to these nonabusing drinkers.
Our study is designed as an initial effort to address this gap. We selected an exploratory sequential design (Creswell, Clark, Gutmann & Hanson, 2003) to achieve a more comprehensive, elaborated and nuanced view of alcohol consumption among these nonabusing drinkers diagnosed with Hepatitis C (Lee & Greene, 2007). The qualitative component, with its inductive theoretical drive (Morse, 2003), generated insights into drinking behaviors that had not previously been reported in quantitative studies focusing primarily on abusing drinkers. The subsequent quantitative component provided estimates of the prevalence of new decision factors emerging from our qualitative analysis and explored the link between these factors and alcohol consumption. This use of quantitative data is consistent with the sequential exploratory design, in which the quantitative component assists in the interpretation of qualitative findings (Creswell, Clark, Gutman & Hanson, 2003). Morse (2003) diagrams this approach as QUAL → quan. Our integration of findings from both phases adds to our understanding of the impact of individual behavior on health, one of the dominant issues in health science research (Forthofer, 2003). We add to the mixed methods literature by illustrating two novel approaches. First, we used existing quantitative instruments as indicators of alcohol consumption decision factors already recognized by researchers, providing a comparison base with which to compare the experiences of informants in our qualitative component. Second, in identifying new decision factors encountered by nonabusing drinkers, we triangulated our qualitative data by supplementing transcripts of semi-structured interviews with comments posted by HCV+ patients on the Internet.
We examine drinking decisions among people diagnosed with chronic hepatitis C virus (HCV) infection who, at the time of data collection, were consuming alcohol at rates that would not be considered problematic in the absence of their HCV diagnosis, i.e., low risk drinkers whose consumption is generally within the ‘safe’ limits that are recommended by bodies such as the National Institute on Alcohol Abuse and Alcoholism. Nonabusing alcohol users do not have physical dependence, withdrawal symptoms or the complex psychosocial impairments that abusers experience as major impediments to limiting alcohol consumption.
We focus on chronic HCV infection for three reasons. First, HCV infection is prototypical of these non-alcohol-related conditions for which drinking is contraindicated. Curtailing alcohol intake among these patients is especially challenging, because HCV is generally asymptomatic throughout its course and moderate drinking does not predictably lead to symptoms that might influence subsequent consumption in nonabusing patients (CDC, 2007; Hoofnagle, 1990). Secondly, HCV constitutes a major public health challenge. An estimated four million Americans are currently infected (Armstrong, Wasley, Simard, McQuillan, Kuhnert & Alter, 2006) with projected medical costs from 2010 to 2019 of almost $11 billion and a societal cost of just over $54 billion due to years of life lost under the age of 65 (Wong, McQuillan, McHutchison & Poynard, 2000).
Even at low to moderate levels of intake, alcohol has been found to adversely influence the prognosis for HCV infection by aggravating histological lesions and increasing fibrosis, leading to cirrhosis and/or hepatic cancer/hepatoma (Hezode, Lonjon, Roudot-Thoraval, Pawlotsky, Zafrani, & Dhumeaux, D., 2003; Westin, Lagging, Spak, Aires, Svensson, Lindh, Dhillon, Norkrans, & Wejstal, 2002; Pessione, Degos, Macellin, Duchatelle, Njapoum, Martinot-Peignouz, Degott, Valla, Erlinger, & Rueff,. 1998). Thus, developing interventions that effectively encourage a reduction in even moderate amounts of alcohol consumption can potentially improve the course of HCV. A prerequisite for effective intervention is the ability to identify incentives and barriers to the elimination of alcohol within the context of a disease that may not be presently symptomatic and a pattern of alcohol consumption that is not producing personal or social problems in patients' lives. Our research illustrates the utility of a mixed methods design in addressing this goal.
Method
Overview of Research Design
Our objective in this exploratory research project was to identify factors impacting the initiation and maintenance of decisions to curtail alcohol consumption among nonabusing HCV+ patients not reflected in existing literature. Figure 1 summarizes our application of the exploratory sequential design (Cresswell et al., 2003). Our approach illustrates an assessment of Instrument Fidelity, which Collins, Onwuegbuzie and Sutton (2006) identified as one of four rationales for conducting mixed methods research. Although we are not designing a new instrument, our findings suggest areas in which existing instruments could be modified for use with nonabusing drinkers told to curtail alcohol consumption for medical reasons not related to alcohol. The research design was approved by the IRB of MetroHealth Medical Center, Cleveland, Ohio.
Figure 1.
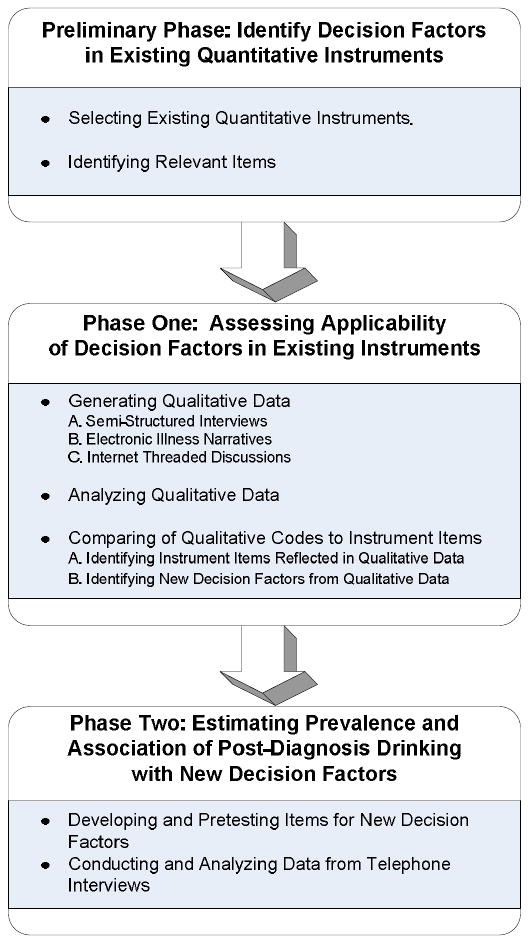
Research Design
Preliminary Phase: Identifying Decision Factors in Existing Quantitative Instruments
Introduction: Goals of Preliminary Phase
The Preliminary Phase was designed to summarize decision factors influencing alcohol consumption already identified by existing research. Our goal was to create a comprehensive summary of previously identified decision factors with which we could compare decision factors reported by our informants in Phase One.
Methods and Data Collection for Preliminary Phase
We examined previously tested scales and instruments developed to identify factors influencing the initiation and maintenance of decisions to curtail or eliminate alcohol consumption. We searched for instruments tapping the experiences of both abusing and nonabusing drinkers, but we were unable to locate any instruments that addressed nonabusing drinkers. We conceptualized these instruments as indicators of factors that researchers consider important in decisions about drinking, including barriers and incentives to implementing and maintaining decisions to reduce alcohol consumption. Examining an extensive inventory of instruments ensured that we were tapping a broad range of previously identified decision factors.
Five researchers, experts in alcohol research (ND, RM), psychometrics (KK, AP), and health education (SK), searched databases, reviewed bibliographies, and relied on their own expertise to identify instruments tapping decisions about alcohol consumption. We included self-report Likert-type instruments with a demonstrated ability to predict behavior change for abusing drinkers. Exact wording of items and published psychometric evaluations were available for all instruments. All instruments had been published and tested in English.
Results for Preliminary Phase
This process yielded 16 instruments comprised of 758 items (Table 1, Columns 1&2). Two experts in alcohol research, a physician (ND) and a clinical psychologist (RM), independently reviewed these 758 items to identify items addressing drinking decisions, eliminating items judged not relevant to nonabusing drinkers. Eliminated items generally referred to a degree of consumption not expected in nonabusing drinkers or to interventions (e.g., antabuse) that would not be used with nonabusing drinkers. After review, we retained 733 of the 758 items for analysis in Phase One (Table 1, Column 3).
Table 1. Comparison of Items in Existing Instruments and Qualitative Data.
| Column 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| Instrument | Items in the Instrument | Items Addressing Drinking Decisions or Patterns | Drinking Decision or Pattern Items Reflected in the Qualitative Data | Drinking Decision or Pattern Items NOT Reflected in the Qualitative Data | ||
| Total Number | Items ONLY Relevant for Abusing/ Problematic Drinkers | Items Relevant for Nonabusing Drinkers | ||||
| Drinking Self-Efficacy Questionnaire (DSEQ) (Young et al. 1991) | 31 | 31 | 31 (100%) | 0 | 0 | 0 |
| The Stages of Change Readiness and Treatment Eagerness Scale-Personal Drinking Questionnaire (SOCRATES 8A) (Miller and Tonigan 1996) | 19 | 19 | 19 (100%) | 0 | 0 | 0 |
| Alcohol and Drug Consequences Questionnaire (ADCQ) (Cunningham et al. 1997) | 28 | 28 | 27 (96%) | 1 | 1 | 0 |
| Drinking Expectancy Questionnaire (DEQ) (Young and Knight 1989) | 27 | 27 | 26 (96%) | 1 | 0 | 1 |
| The Drinker Inventory of Consequences (DrInc-2L or DrInc-2R) (Miller et al. 1995) | 50 | 50 | 48 (96%) | 2 | 2 | 0 |
| The Drinker Inventory of Consequences-Short Inventory of Problems (SIP-2L or SIP-2R) (Miller et al. 1995) | 15 | 15 | 13 (87%) | 2 | 2 | 0 |
| Alcohol Expectancy Questionnaire (AEQ) (Brown et al. 1987) | 120 | 120 | 119 (99%) | 1 | 1 | 0 |
| Perceived Benefit-of-Drinking Scale (Petchers and Singer 1987) | 5 | 5 | 5 (100%) | 0 | 0 | 0 |
| Reasons for Drinking Questionnaire (Zywiak et al., 1996) | 16 | 16 | 16 (100%) | 0 | 0 | 0 |
| Work Teams and Drinking Norms (Delaney and Ames 1995) | 18 | 18 | 18 (100%) | 0 | 0 | 0 |
| Alcohol Use Inventory (Horn et al. 1990) | 228 | 205 | 178 (87%) | 27 | 24 | 3 |
| Negative Alcohol Expectancy Questionnaire (NAEQ) (McMahon and Jones 1993) | 60 | 60 | 50 (83%) | 10 | 10 | 0 |
| Alcohol: Processes of Change (Cancer Prevention‥ 2001) | 65 | 63 | 46 (73%) | 17 | 10 | 7 |
| Alcohol: Decisional Balance (Cancer Prevention‥ 2001) | 16 | 16 | 15 (94%) | 1 | 1 | 0 |
| Alcohol Temptations (Cancer Prevention‥ 2001) | 21 | 21 | 21 (100%) | 0 | 0 | 0 |
| Alcohol: Self-Efficacy (Cancer Prevention‥ 2001) | 39 | 39 | 37 (95%) | 2 | 0 | 2 |
| TOTAL | 758 | 733 | 669 | 64 | 51 | 13 |
Inferences from Preliminary Phase
Researchers have identified a large number of factors influencing decisions about drinking. Although the 16 instruments were developed and validated with people identified as alcohol abusers, most items were judged as potentially relevant to the experiences of nonabusing drinkers. The 733 items provide a comprehensive baseline against which to compare the decision experiences captured in the qualitative data analyzed in Phase One.
Phase One: Assessing Applicability of Decision Factors in Existing Instruments
Introduction: Goals for Phase One
In Phase One we examined drinking decisions among HCV+ nonabusing drinkers as reflected in three sets of qualitative data. Our goals were to assess the extent to which the decision factors available in the quantitative instruments captured the experiences of these nonabusing drinkers advised to curtail alcohol consumption because of a Hepatitis C diagnosis and to identify any additional decision factors discussed by these nonabusing drinkers but not captured in the quantitative instruments.
Methods, Data Collection, and Analysis for Phase One
Generating Qualitative Data
Our first task was to provide a portrait of drinking decisions among this subset of drinkers. We began by analyzing textual data from three sources (semi-structured interviews, electronic illness narratives, and Internet threaded discussions) to understand factors affecting post-diagnosis alcohol consumption among nonabusing drinkers with Hepatitis C. Our goal was to maximize the range of potential responses.
We conducted 42 semi-structured interviews with HCV+ patients at MetroHealth Medical Center, an urban teaching hospital in Cleveland, Ohio. Respondents were recruited from patients who were being treated at the gastroenterology clinic and from emergency department patients who had not followed up with a doctor after an HCV diagnosis. Eligible patients were nonabusing drinkers (defined as a score of ten or less on the Alcohol Use Disorders Identification Test [AUDIT]) (Saunders, Aasland, Babor, DeLaFuente & Grant, 1993; Babor, T.F., de la Fuente, J.R., Saunders, J., and Grant, M., 1992). We used a sampling grid designed to ensure variability in gender, race/ethnicity (African American, Hispanic and White informants) and level of alcohol use (AUDIT scores between 1 and 7 (generally nonproblematic) and between 8 and 10 (potentially problematic)).
The interview guide, which consisted of guiding questions and structured probes, was developed by a multidisciplinary team (two sociologists, a psychologist, a nurse and a physician) and pretested with HCV patients not included in the study sample. The protocol included 12 questions about people's knowledge, experience, and management of HCV infection (Stoller, Hund, Webster, Blixen, Perzynski, McCormick, Kanuch & Dawson, 2006). The interview format enabled us to pursue new themes, encourage respondents to elaborate answers, and to explore the context of responses, while also giving us the opportunity to collect background information on the respondents. Interviews were recorded, transcribed verbatim, and typically lasted 30-90 minutes. Respondents received a $50 gift card and travel expenses.
Respondents were 36 to 74 years of age (mean=49.5, SD=8.1). Sixty-two percent were men, and the mean level of education was 12 years (SD=2.3). Thirty-eight percent identified themselves as African American, 26% as Hispanic, and 36% as White. The mean time since diagnosis was 8.0 years (SD=6.5).
We also sampled 2 types of electronic data: illness narratives and threaded discussions from 8 English-language websites (see Appendix for a listing of these websites). At the time of data collection, Google and Yahoo! maintained searchable digital archives of English-language website message boards and threaded discussions on HCV from which we identified electronic narratives and threaded discussions. In contrast to electronic narratives, which comprise a single post, threaded discussions consist of a series of linked postings that are created over time as people in an electronic discussion group read and respond to an initial post. These data minimized the reactivity that can emerge when people are interviewed in clinical settings in which they are also patients and tapped experiences of people not being treated in a teaching hospital affiliated with a medical center.
We identified and copied into electronic documents 307 HCV-related illness narratives from the 8 websites. Line-by-line coding by at least 2 researchers, supplemented by electronic text searching, identified 79 narratives that referred to alcohol consumption, which we analyze in this article. We could infer only limited demographic information about narrators from the posted text. Twenty-two percent were men, 40% were women, and 37% did not provide any indication of gender. We could infer years since diagnosis for 63% of the narratives, among whom 27% were diagnosed within the past year, 47% had been diagnosed 1-4 years earlier, and 27% more than 5 years ago.
We identified HCV-relevant Internet threaded discussions using 10 alcohol-related search terms synthesized from prior literature and an expedited review of 900 threaded discussions of HCV (Stoller, Webster, Blixen, McCormick, Perzynski, Kanuch & Dawson, in press). We collected over 600 HCV-relevant threaded discussions containing at least one of the alcohol-related search terms and selected a systematic sample of every third discussion (264 threads). Because multiple researchers collected the discussion data, we tested for inter-rater reliability in identifying alcohol-relevant discussions using Cohen's Kappa (Bernard, 2002). For identifying relevant discussions, Kappa = .93. Discussants rarely revealed information from which personal attributes could be inferred, so we are unable to provide discussant profiles.
Analysis of the Qualitative Data
Analysis of the qualitative data proceeded in two stages. We began with line-by-line coding. We did not code chunks of text that described drinking behaviors most likely in abusing drinkers, i.e., degrees of drinking not expected in a nondependent person or to interventions not used with nondependent drinkers. The Phase One qualitative team (CB, AH, ES & NW) independently reviewed each document and coded emergent themes, with an emphasis on alcohol consumption and drinking decisions among nonabusing drinkers. Our goal was to capture the full range of drinking decision factors reported by these informants, regardless of whether the factors were unique to nonabusing drinkers or shared with abusing drinkers. Each researcher read each document 3-5 times, recording initial thoughts and developing a preliminary set of themes or categories (Esterberg, 2002). Regular meetings were held to discuss emerging themes, to devise preliminary codes and to resolve discrepancies. We constructed a coding dictionary that was refined (e.g., new codes added, other codes deleted, definitions modified) through comparison, categorization and discussion of team members' interpretation of each code's properties and dimensions (Crabtree & Miller, 1999; Bernard, 2002). Using this dictionary, each document was coded by at least two researchers with coding decisions recorded electronically using NVivo, a computer program for managing and analyzing qualitative (text) data. We resolved all discrepancies between the two coders through discussion.
We then retrieved all segments of text attached to each code and further elaborated, refined and differentiated the initial codes. Emergent observations were recorded in theoretical memos, which provided the foundations for discussion at team meetings. We repeated this process of engagement with the data and subsequent team discussions until consensus was reached on coding decisions and no new insights emerged. Changes were incorporated into the coding dictionary, and the documents were recoded, with each document coded by different two researchers. Checks of inter-rater consistency using Cohen's Kappa (Bernard, 2002) were conducted at the beginning, middle and end of the coding process (Kappa > .90 for all checks). Results of this recoding generated a catalog of decision factors affecting consumption decisions among our samples of HCV+ nonabusing drinkers.
Comparison of Qualitative Codes and Items from Existing Instruments
The qualitative team independently compared the chunks of text attached to our final set of qualitative codes to the 733 alcohol-related items from the quantitative instruments, noting which instrument items were reflected in the qualitative data and compiling a list of new alcohol-related decision factors, with illustrative quotations, in the qualitative text not reflected in any of the indicators. Lists of new decision factors compiled by members of the qualitative team were merged, and each team member again reviewed the quantitative instruments searching for items matching the coded text. Results of this final search were reviewed by the Phase One quantitative team (ND, RM, AP), who eliminated two items they determined were encompassed by a combination of items from existing instruments. This process generated two outcomes, described below: (1) identification of items in each instrument represented in the qualitative data and (2) a catalog of new decision factors not reflected in the quantitative instruments.
Results for Phase One
Instrument Items Reflected in the Qualitative Data
Most (93.3%) of the 733 items from the quantitative instruments judged to be relevant to nonabusing drinkers appeared in our qualitative data (See Table 1, Col. 4). Six instruments were completely captured in the qualitative data: the DSEQ, the SOCRATES 8A, the Perceived Benefit-of-Drinking Scale, the Reasons for Drinking Questionnaire, the Work Teams and Drinking Norms inventory, and the Alcohol Temptations instrument. Six additional instruments had over 90 percent of their items reflected in the qualitative coding: the AEQ (99%), the ADCQ (96%), the DEQ (96%), the Drinc-2LI (96%), the Alcohol Self-Efficacy Inventory (95%), and the Alcohol Decision Balance instrument (94%). Only four instruments exhibited lower levels of overlap with the qualitative results: the SIP-2LI (87%), the Alcohol Use Inventory (87%), the NAEQ (83%), and the Alcohol Processes of Change Inventory (73%).
Identifying New Decision Factors from Qualitative Data
The qualitative data revealed a number of decision factors not included in the quantitative instruments. Informants described both reasons for quitting and reasons for continuing to drink, explaining that decisions to limit alcohol consumption were sometimes impeded by barriers to quitting or facilitated by strategies for quitting. In presenting the illustrative quotations, we refer to informants participating in semi-structured interviews as Respondents, informants posting electronic illness narratives as Narrators, and informants posted on Internet threaded discussions as Discussants.
Reasons for Quitting
The only reason for quitting not reflected in the quantitative instruments was Treatment Concerns. Several cautioned that evidence of recent alcohol consumption would remove a person from waiting lists for liver transplants. Others recognized that alcohol can undermine HCV drug treatment efficacy, like Discussant 6042, who compared drinking alcohol while on treatment to fighting a fire with gasoline.
Reasons for Continuing to Drink
Accompanying motivations not to drink are a range of perceived benefits from alcohol consumption that can undermine decisions to quit or cut back. We identified three Reasons for continuing to drink in the qualitative data that were not reflected in the quantitative instruments.
Some informants used alcohol as a Reward for positive behaviors. For example, Respondent 832DS related:
Recently I… had worked out real well… I said to myself, “You've been doing well, get you a beer and go home and sit down and get your buzz on …. You deserve a beer.”
Others used alcohol to reward themselves for positive test results or for completing treatment:
Only 6 months of enduring this treatment… I'm looking forward to celebrating after with a glass of wine! (Discussant 4028)
The quantitative instruments included items that described rewarding oneself for successfully abstaining from alcohol, but we did not find any items describing the use of alcohol itself as a reward.
Weather, especially hot summer days, generated a longing for cold alcoholic drinks among some informants:
I go into a store, it's scorching hot outside, 90 plus, and you got your mind set on getting some juice or pop or something. And then somebody walks up to the counter… like a commercial when you see… a crystal glass… and mist, cold mist coming off, ice cold 40 ounce Miller's. And I couldn't take it… I lost that battle that day. (Respondent 64DB)
Alcohol was also used for Health/Disease Management. Some drank to manage symptoms, particularly pain. Others believed that alcohol provided health-related benefits, often mentioning decreased risks of heart disease. Not all information was accurate, however, as illustrated by Respondent 802BB:
Some alcohol is healing to the body. I think it's gin they say thins the blood. Or is it rum? Rum, I think is good for the heart a little bit.
Barriers to Quitting
The likelihood that patients will implement and maintain decisions to cut back on alcohol can be reduced by barriers that operate at both the individual and contextual levels. Our informants described five barriers to quitting not reflected in the quantitative instruments:
Some described Hobbies involving alcohol. Respondent 294BJ is a wine aficionado who goes to wine tastings and prides himself on his extensive wine cellar and ability to talk knowledgably about wine. Discussant 6003 described making his own beer as a hobby.
A number of informants were aware of the risks of alcohol consumption but Discounted the Likelihood of Risks in their own case. Several reported drinking for some time after acquiring the disease, often before they knew or suspected they had been infected. After they were diagnosed, biopsies found no evidence of liver damage, and clinical tests results did not suggest (at least to the informants) that the disease had progressed. Therefore, they decided that they must be among the exceptions who can drink with minimal negative effects:
A good way to tell if alcohol will affect the course of your HCV is to drink a lot for about 25 years and see what happens! Now, I don't recommend that anyone do this, but a lot of us have already done this test, before we knew we had the HCV!… For those whose disease did not progress there simply is no compelling reason not to have an occasional drink. (Discussant 6002)
For others, statements by health care professionals that occasional alcohol use was acceptable opened the door to more frequent drinking (Blixen, Webster, Hund, Perzynski, Kanuch, Stoller, McCormick & Dawson, 2008). Expressing frustration at what they interpreted as ambiguous or conflicting medical advice, these informants said they needed stronger directives from health care professionals in order to quit drinking:
If [the doctor] said, “If you drink another drink it gonna kill you,” I could cut the recreational drinking that I do now. [Respondent 6GM].
Some informants saw Nothing to Lose if they continued drinking, because their disease was so advanced that they had little hope for an extended future. Others, diagnosed during the early stages of HCV awareness and told no treatment was available, saw no reason to forego drinking to extend the time line in a prognosis they understood as hopeless. For example, Narrator 207, diagnosed in 1978 with “non-A non-B Hepatitis” reports:
[The doctor] said… nothing could be done – just don't drink, I thought yea right! So I continued on drinking, smoking, eating fat, high stress job, but never felt like my old self
Countermeasures are strategies to counteract the negative effects of alcohol. Some respondents drink water or juice to dilute the alcohol; others drink only on a full stomach. Other countermeasures involved putting ice in beer (19GS) or eating mashed potatoes to absorb the alcohol (817SJ).
Stigma also shapes drinking decisions. Actual or anticipated responses from other people can make patients reluctant to disclose their diagnosis as an explanation for a change in previous drinking behavior (Lichtenstein, 2003). When drinking is central to socializing, not drinking can compromise efforts to keep their diagnosis secret. As Respondent 6GM explained, “Some things are best untold… because [people] tend to treat you a little bit different if you tell them.”
Strategies for Quitting
Only one strategy for quitting emerged from the qualitative data that was not reflected in the quantitative instruments. Substitution involves behaviors that enable informants to limit alcohol consumption, either quitting completely or cutting back on amount. Some switched the type of alcohol they consumed, most often from hard liquor to beer, wine or “coolers,” like Respondent 145RL, who explained “Now I'm just a beer man.” Others changed to a non-alcoholic alternative or eliminated alcohol from a favorite drink. Discussant 6006 “boiled margaritas” to remove the alcohol. Others maintained their drinking rituals (e.g., drinking out of the same mug, drinking at the same place and time of day) but substituted a non-alcoholic beverage. Finally, some informants sought to replace alcohol with other foods or beverages:
Instead of going and taking me a shot, instead I'll drink me some chocolate milk and eat me a couple of oatmeal cookies and smoke me a cigar. Something to replace what I would normally do with the alcohol. (Respondent 06GM)
Inferences from Phase One
The qualitative analysis in Phase One provides a fuller picture and deeper understanding of the experiences of these HCV+ nonabusing drinkers than that available from our synthesis of existing quantitative instruments in the Preliminary Phase. Standardized questionnaires constrain in advance the view of the phenomenon under study and can fail to capture the full range of relevant experience, especially experiences of segments of the population not represented in instrument development. In contrast, exploratory studies such as Phase One document the breadth of a phenomenon by mapping its extremes (Scott, Bergeman, Verney, Longenbaker, Markey & Bisconti, 2007). The new decision factors identified in our Phase One qualitative component constitute content areas that influence drinking behavior among nonabusing drinkers but would be overlooked by researchers relying on existing instruments.
Phase Two. Estimating the Prevalence of New Decision Factors
Introduction: Goals for Phase Two
Phase One revealed new decision factors surrounding alcohol consumption in our HCV+ nonabusing drinkers but did not provide estimates of the prevalence of these new factors, so we were unable to differentiate idiosyncratic or extreme cases from more typical examples. The goal of Phase Two was to address this gap by providing estimates of the prevalence and association with post-diagnosis alcohol consumption of the new decision factors identified in Phase One.
Methods, Data Collection and Analysis for Phase Two
The Phase Two quantitative team (ND, KK, RM, AP) developed survey items to tap each new decision factor that emerged from our analysis of Phase One qualitative data. For respondents who had quit drinking, items were framed in the past tense. Treatment concerns was excluded, because its importance would vary with time since diagnosis, i.e., people who had only recently been diagnosed might be unaware of treatment options and eligibility requirements, whereas people who had been diagnosed many years earlier may have already undergone treatment.
Members of the Phase Two qualitative team (CB, AH, ES, NW) reviewed these items to ensure that they captured the meaning of the new decision factors, and the items were piloted through telephone interviews with a convenience sample of medical patients from MetroHealth Medical Center. A separate sample of HCV patients were asked to complete a cognitive interview (Willis, 2005; Brennan, 2003). In the cognitive interviews, respondents were interviewed in person. After each question, an interviewer trained in cognitive interviewing reviewed each new item, the patient's response, and the reason for the response (“Why did you answer the way you did?”). Survey items were rewritten if the pilot or cognitive interviews indicated difficulties or ambiguities for respondents. The 17 items were incorporated into the schedule for telephone interviews (See Table 2).
Table 2. Frequency Distributions of Decision Factors not in Existing Instruments (N=386).
| Reasons for Continuing to Drink | None of the time | Little | Some | Most | All of the time | % Agreed/At least Some of the Time a | |||
|---|---|---|---|---|---|---|---|---|---|
| Quit Drinking? | |||||||||
| NO | YES | Sig. | |||||||
| Reward | |||||||||
| 1. You have a drink to reward yourself? b | 53.3% | 9.4% | 21.1% | 9.7% | 6.5% | 17.1% | 49.8% | <.001 | |
| Weather | |||||||||
| 1. When it's hot outside you can't resist a cold beer or cocktail? b | 22.1% | 44.4% | 2.6% | 4.9% | 19.2% | 6.8% | 17.0% | 39.5% | <.001 |
| Health/Disease Management | Strongly Disagree | Disagree | Slightly Disagree | Slightly Agree | Agree | Strongly Agree | |||
| 1. You drink alcohol to help when you are in pain or feeling ill? b | 22.3% | 41.8% | 2.6% | 7.3% | 17.1% | 8.8% | 26.5% | 37.3% | .015 |
| 2. In small amounts, alcohol can be good for you? | 21.1% | 47.0% | 5.0% | 9.2% | 15.6% | 2.1% | 44.0% | 16.8% | <.001 |
| Barriers to Quitting | |||||||||
| Hobbies | |||||||||
| 1. Studying and tasting various wines and/or beers is a hobby of yours? b | 25.4% | 55.7% | 0.8% | 5.4% | 10.4% | 2.3% | 13.6% | 20.9% | .123 |
| Discounted the Likelihood of Risks | |||||||||
| 1. When you feel ok, it is alright for you to have a drink? b | 18.2% | 29.6% | 3.7% | 11.9% | 28.0% | 8.7% | 55.2% | 44.5% | .121 |
| 2. Drinking every once in a while won't hurt you? b | 22.6% | 29.9% | 4.2% | 8.7% | 29.1% | 5.5% | 64.8% | 30.1% | <.001 |
| 3. When it is time to stop drinking your body will give you signals? b | 10.8% | 20.4% | 1.9% | 4.5% | 44.7% | 17.7% | 73.0% | 63.2% | .247 |
| 4. People who have low viral counts can still drink? | 23.8% | 56.9% | 5.0% | 7.0% | 6.7% | 0.6% | 27.7% | 7.3% | <.001 |
| Nothing to Lose | Strongly Disagree | Disagree | Slightly Disagree | Slightly Agree | Agree | Strongly Agree | |||
| 1. No matter what you do your hepatitis C is going to get worse? | 15.7% | 48.3% | 8.1% | 5.3% | 16.9% | 5.6% | 27.3% | 28.0% | .674 |
| 2. We all die eventually, so you might as well have a drink? | 28.8% | 57.1% | 3.1% | 4.7% | 4.9% | 1.3% | 19.1% | 5.8% | <.001 |
| Countermeasures | |||||||||
| 1. When you do choose to drink you make sure to have plenty of food or water with it? b | 6.7% | 28.5% | 2.6% | 8.3% | 41.2% | 12.7% | 80.3% | 51.0% | <.001 |
| None of the time | Little | Some | Most | All of the time | |||||
| 2. Drinking alcohol is ok as long as you live a healthy lifestyle (for example eating healthy, exercising, or taking vitamins)? | 65.8% | 11.6% | 12.6% | 8.9% | 1.1% | 40.8% | 11.7% | <.001 | |
| Stigma | |||||||||
| 1. You feel you need to keep your hepatitis C a secret? | 13.3% | 40.6% | 3.9% | 13.8% | 22.7% | 5.7% | 44.5% | 40.8% | .297 |
| 2. You feel you are at least partially to blame for your hepatitis C? | 11.8% | 15.5% | 1.6% | 6.6% | 41.2% | 23.4% | 69.1% | 72.4% | .310 |
| 3. You need to hide the fact you have hepatitis C? | 11.2% | 47.1% | 4.7% | 13.3% | 18.2% | 5.5% | 40.1% | 35.0% | .284 |
| Strategy for Quitting | |||||||||
| Substitution | |||||||||
| 1. People with hepatitis C should avoid hard liquor and stick to wine or beer? | 26.7% | 41.6% | 2.1% | 6.4% | 16.5% | 6.7% | 42.4% | 22.0% | <.001 |
Percent exhibiting some level of agreement (i.e., strongly agree, agree or slightly agree) or percent reporting behavior at least some of the time (i.e., some, most or all of the time). Complete distributions are available from the first author.
These items were reframed in past tense for respondents who indicated that had quit drinking sometime after their HCV diagnosis.
Significance tests are based on the nonparametric Mann-Whitney U test.
We conducted structured telephone interviews with a sample of 577 HCV+ patients from MetroHealth Medical Center. Eligible respondents were 21 years of age or older, were aware of their HCV diagnosis, had not cleared the virus, had consumed at least one alcoholic beverage in their lifetime, were not HIV+, were not pregnant, and had an AUDIT score less than or equal to 10, an indicator of nonabusive drinking (Saunders, Aasland, Babor, DeLaFuente & Grant, 1993).
We screened patients for eligibility from a randomized list of 2,931 potential subjects until we completed a sampling grid designed to ensure variability by race/ethnicity. We contacted 1,191 patients, of whom 783 met our eligibility criteria. The patient list included only 268 Hispanic patients and, although we contacted all of these patients, only 8.7% of the sample were Hispanic; 42.8% were White, 42.8% were Black, and 5.8% reported other ethnic backgrounds. Our 577 completed interviews constitute a participation rate of 74%. The interviews typically lasted 30-40 minutes. Participants received a $25 grocery store gift card.
In this article, we focus only on the 386 respondents who reported drinking after their HCV diagnosis; among these respondents, 147 reported that they were still drinking and 239 had quit drinking. Slightly under half (44.6%) of these 386 respondents were women; 44.7% were White, 42.6% were African American, and 12.7% reported another race/ethnicity. More than three-quarters (77.9%) reported annual incomes below $25,000; 11.2% reported incomes between $25,000 and $39,999, and the remaining 10.9% reported incomes of $40,000 or higher. The median level of education was high school graduate. The mean time since diagnosis was 8.0 years (SD=6.7).
In addition to estimating the prevalence of each of the 17 items, we compared responses to the 17 items of respondents who quit drinking sometime after their diagnosis with respondents who were still drinking (Table 2). We assessed significant differences between these distributions using the non-parametric Mann-Whitney U Test. Responses to the 17 items are distributed on an ordinal scale and therefore do not meet the parametric assumption of at least an interval level of measurement. The Mann-Whitney U test, as an analogue to the parametric independent sample t-test, does not impose this restriction on the data.
Results for Phase Two
Telephone survey data enabled us to examine the prevalence and association with current drinking behavior of the new decision factors identified in Phase One. Results of our analyses of responses to the 17 items reflecting the new decision factors are summarized in Table 2.
Prevalence
At least one-quarter of our telephone survey respondents expressed some level of agreement (i.e., strongly agree, agree or slightly agree) or reported a behavior at least some (i.e., some, most or all) of the time for 13 of the 17 new items, at least one-third expressed some level of agreement or frequency with 9 items, and at least two-fifths expressed some level of agreement or frequency with six items. None of the items generated agreement or reported frequency among fewer than 10%.
About one-third expressed some level of agreement or frequency for items tapping Reasons for Continuing to Drink. Thirty-seven percent used alcohol to reward themselves at least some of the time. One-third (33.2%) used alcohol to relieve symptoms, 26.9% agreed that small amounts of alcohol can enhance health, and 30.9% found it difficult to resist a drink in hot weather.
Decision factors involving Barriers to Quitting were among the most prevalent. Generating the highest levels of agreement were items that minimized the negative impact of alcohol consumption, either by discounting the risks or advocating countermeasures. Two-thirds (66.9%) expressed some level of agreement that people can rely on their bodies to give them signals “when it is time to stop drinking.” Almost one-half (48.6%) agreed that it is all right to have a drink “when you feel OK,” and 43.3% agreed that drinking “every once in a while won't hurt you.” Almost two-thirds (62.2%) agreed with the importance of “having plenty of food or water” when drinking, although fewer than one-quarter (22.6%) believed that alcohol consumption could be counterbalanced by living a healthy lifestyle.
Items tapping HCV as a stigmatized condition also generated fairly high levels of agreement. Almost three-quarters expressed some level of agreement that they were partially to blame for their HCV infection, and approximately two-fifths felt a need to keep their diagnosis a secret (42.4%) and to hide the fact that they have HCV (37.0%).
Substitution was the only Strategy for Quitting not reflected in the quantitative instruments. Almost three in ten respondents (29.6%) expressed some level of agreement that people with HCV should “avoid hard liquor and stick to wine or beer,” our indicator of substitution.
Association with Alcohol Consumption
We also examined the extent to which the new decision factors predicted post-diagnosis drinking. Respondents who were still drinking exhibited higher levels of agreement than respondents who had quit with decision factors providing a rationale for continued drinking. They were more likely to agree that occasional drinking is not harmful and that small amounts of alcohol can be good for you and were more likely to agree that people with low viral counts can still drink. Finally, these respondents were more likely to agree that one might as well drink since we all die eventually.
Respondents who were still drinking were also more likely to agree that countermeasures could mitigate the negative effects of alcohol. They were more likely to agree with the importance of food and water when one drank and to agree that alcohol damage can be offset by a healthy lifestyle. They were also more likely to advocate substituting wine or beer for hard liquor.
In contrast, respondents who quit drinking after their diagnosis exhibited more frequent reports of behaviors describing occasional drinking or drinking in response to intermittent triggers. They were more likely to report having used alcohol as a reward, more likely to drink in response to pain/illness, and more likely to drink in hot weather.
Inferences from Phase Two
Estimates of the prevalence of new decision factors among respondents to the Phase Two telephone survey suggest that the new factors are neither unique nor idiosyncratic but reflect the experiences of substantively significant proportions of these HCV+ patients. Our results documented differences in decision factors between respondents who were still drinking and respondents who had quit at some point after their diagnosis. Incorporating these new decision factors into existing instruments would enhance their generalizability to nonabusing patients advised to reduce alcohol consumption for medical reasons.
Conclusion
Summary
Our exploratory sequential design integrated analysis of qualitative data from semi-structured interviews and posting on Internet websites (Phase One) with quantitative data collected from telephone interviews (Phase Two) with people who had been diagnosed with Hepatitis C and who were consuming alcohol at levels that would be considered safe in the absence of their diagnosis. Our results enrich our understanding of similarities and differences in factors influencing decisions to curtail alcohol consumption between abusing drinkers and nonabusing drinkers advised to stop drinking for medical reasons not related to alcohol.
Most of the decision factors that have been found to predict alcohol consumption among abusers also influence the decision process of non-abusers faced with a medical need to stop drinking. Ninety-three percent of the items addressing drinking decisions identified in instruments examined in the Preliminary Phase appeared in the qualitative data.
Our Phase One qualitative analysis also identified a set of factors not included in existing instruments and seemingly specific to non-abusers faced with a medical necessity to curtail drinking. These included Reasons for Quitting (eligibility for and efficacy of treatment), Reasons for Continuing to Drink (reward, weather, health management), Barriers to Quitting (hobbies, discounting risks, nothing to lose, countermeasures, and stigma) and Strategies for Quitting (substitution).
Our quantitative analyses in Phase Two indicated that these factors were neither rare nor idiosyncratic. The majority of behaviors and attitudes identified as new decision factors were reported by one-quarter to one-third of a representative sample of HCV+ patients drinking at nonabusing levels at the time of their diagnosis. Decision factors addressing Barriers to Quitting were most prevalent, particularly efforts to discount the risks of alcohol consumption and relying on countermeasures to minimize the negative effects of drinking.
Phase Two results also suggested that these new decision factors are viewed differently by patients who are still drinking and patients who quit drinking after their diagnosis. In comparison with patients who were still drinking, patients who stopped drinking after diagnosis were more likely to attribute their post-diagnosis drinking to occasional triggers, such as a reward for non-alcohol-related behaviors, a source of symptom relief, or a response to hot weather. This intermittent drinking in response to specific triggers may be easier to modify than alcohol consumption associated with regular situations (e.g., socializing with family, friends or co-workers) or with chronic stressors.
In contrast, patients who had not been successful in implementing or maintaining decisions to curtail alcohol consumption were more likely to report rationales for drinking not tied to specific triggers. They were more likely to discount the risks of alcohol consumption and more likely to advocate countermeasures for alleviating the negative effects of drinking. Given our cross-sectional data, we do not know whether discounting risks and employing countermeasures encouraged these patients to continue drinking or whether they subsequently adopted these attitudes and behaviors to rationalize their failure to curtail drinking. In either case, our findings highlight the relevance of rationales among patients who are still drinking despite their diagnosis.
Mixed Methods Design: Strengths, Weaknesses and Directions for Future Research
Our integration of qualitative and quantitative research strategies capitalizes on complementary strengths and nonoverlapping weaknesses (Johnson, Onwuegbuzie & Turner, 2007). Analysis of Phase One qualitative data elaborated the understanding of drinking decisions among HCV+ nonabusing drinkers available in the existing instruments examined in the Preliminary Phase. Triangulating qualitative data sources enhanced the range of experiences reported by nonabusing patients who encountered medical advice to curtail alcohol consumption. Comparing our findings from Phase One with existing instruments examined in the Preliminary Phase revealed considerable overlap in decision factors but also identified new factors not previously documented. Our goal in Phase One was to cast a broad net to maximize the range of patient experiences captured in our data, and our results demonstrate the utility of multiple sources of qualitative data, including disease-specific Internet websites, for capturing a fuller range of patient responses to medical advice to change behaviors because of a medical diagnosis. Phase One did not provide prevalence estimates of these new factors, however, so we were unable to differentiate relatively common from extreme experiences (Scott et al., 2007). This weakness was addressed in the quantitative research in Phase Two, in which our analysis of data from the telephone interviews enabled us to estimate both the prevalence of new decision factors and their association with post-diagnosis alcohol consumption.
Our design leaves some unanswered questions. The cross-sectional nature of our quantitative data do not enable us to assess direction in the association between the new decision factors and current drinking behavior among these HCV+ nonabusing drinkers. The cross-sectional design also requires patients who quit drinking sometime after diagnosis to report retrospectively on previous alcohol consumption, responding to items framed in past rather than present tense. Although our goal in Phase One was to maximize the range of responses rather than to document their prevalence, we cannot determine the extent to which our data collection strategies tapped the full range of this experience. Indeed it is unlikely that patients recruited in the urban teaching hospital or posting on the Internet are representative of the larger population of persons diagnosed with HCV. Finally, we do not know the extent to which our Phase Two findings based on a sample of patients from one urban, Midwestern teaching hospital generalize to the larger population of HCV+ nonabusing drinkers.
Despite these limitations, we believe our exploratory study has yielded important new insights and suggests new directions for research. We encourage researchers working with nonabusing drinkers diagnosed with conditions that would benefit from a reduction in alcohol consumption to consider incorporating these content areas into existing instruments. Research is also needed to assess the potential relevance of the new decision factors to the experiences of alcohol abusers, particularly those diagnosed with a condition in which alcohol consumption is contraindicated. More generally, we believe that our research design can be used by other researchers concerned with testing the applicability and elaborating existing instruments for use with new populations.
Clinical Implications
Medical patients who are confronted with a disease that requires them to alter their intake of alcohol face many of the same challenges that patients with alcohol abuse face, but nonabusing patients differ from abusers in many important ways. They have not experienced a progressive deterioration of their vocational, social and physical health common in abuse. Few encounter the strong external pressure to quit drinking that an abuser faces from family, friends, employers and the legal system or receive the same pervasive and consistent external advice to terminate drinking. It is to be expected, therefore, that the factors influencing their decision to stop drinking in the face of a medical condition where drinking is contraindicated will differ somewhat from factors influencing abusers.
We categorized our new decision factors using a decisional balance framework emphasizing benefits (pros) and barriers (cons), as well as strategies for overcoming barriers. These factors can also be conceptualized as fitting into three broad categories that have heuristic explanatory value for clinicians: (1) the interaction of alcohol with the course of the medical illness and its treatment; (2) “tailoring” advice not to drink to make it fit better with the patient's life style (Wilson, Hutchinson & Holzemer, 2002); and (3) stigma.
Alcohol and Medical Illness/Treatment
As people face the prospect of change, they evaluate the pros and cons of the planned or recommended change for them, a process termed decisional balance in the Stages of Change Model (Prochaska, Velicer, Rossi, Marcus, Rakowski, Fiore, Harlow, Redding & Rosenbloom, 1994). This can be a complex and confusing process for non-abusers since the advantages of quitting may be long term and not readily evident in the present. This is especially true for HCV+ patients whose infection is asymptomatic and who do not experience immediate negative repercussions from drinking alcohol. Thus it is understandable that they would weigh factors such as the positive health impact of small daily consumption of alcohol and its use as a pain suppressant in deciding whether to drink post-diagnosis. When faced with the additional contingency that treatment for HCV may not progress unless they stop drinking, the decisional balance is further affected. The treatments for HCV can be stressful themselves, which may further affect the balance, and cause some to reward themselves with a drink after completing treatment or use alcohol to deal with this stress.
Tailoring Advice to Quit Drinking
Because the decisional balance equation for the non-abuser does not include the pervasive negative consequences of drinking common among abusers, it is understandable that the non-abuser may attempt to modify the advice to stop drinking. This can include drinking on special occasions, on very hot days, or in ways that accommodate other important aspects of their lives such as hobbies. They may also attempt to offset some of the negative impact of continued drinking by substituting a less potent spirit or developing countermeasures that they perceive will limit the risk. All of these can be seen as ways to “tailor” the medical recommendation to stop drinking to fit within their lifestyle. Discounting the risks of drinking then facilitates the tailoring of advice to quit.
Stigma
Medical conditions vary in the degree to which they are perceived by the population as stigmatizing. Diseases such as HCV which are communicable and commonly associated with socially undesirable behaviors (e.g. intravenous drug use) are most prone to stigma (Conrad, Garrett, Cooksley, Dunne & MacDonald, 2006). About two-fifths of the respondents to our quantitative survey expressed a desire to hide their diagnosis from others. This understandable concern enters the equation for HCV+ patients, particularly if they perceive that stopping drinking will open them up to scrutiny in social contexts. Fear of disclosure can also become a source of chronic stress (Link & Phelan, 2006) and can lead to a range of negative outcomes, including decreased psychological health and poor compliance (Jamison, 2006). The effects of stigma are not limited to patients who contracted HCV through intravenous drug use. Stigma has also been documented among patients who contracted HCV through iatrogenic disease cause by contaminated transfusions or anti-D products, suggesting that the diagnosis is stigmatized independent of actual etiology (Golden, Conroy, O'Dwyer, Golden & Hardouin, 2006).
Identification of these new decision factors should alert treating clinicians to these important additional factors that affect the compliance of nonabusing patients with advice to curtail drinking. Our quantitative results document the prevalence of these additional factors and suggest differences in the salience of specific barriers to quitting for patients who quit drinking at some point after their diagnosis versus those who are still drinking. Understanding the motivational challenges and reasons for ambivalence can help the clinician track compliance and suggest more effective ways to improve adherence to medical advice.
Acknowledgments
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism, NIH Grant #1 RO1 AA13302, Neal V. Dawson, M.D., PI.
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism, NIH Grant [deleted for confidentiality] PI.
Websites for Collection of Online Textual Data
We identified eight English-language websites, updated at least once since 1995, containing electronic information related to HCV and people's stories about HCV:
WebMD, http://www.webmd.com/ (Narratives no longer available online)
National Hepatitis C Coalition, http://nationalhepatitis-c.org/stories/index.htm
Hepatitis C Aware (Website no longer exists)
HepC.de http://hepatitis-c.de/ (Site is no longer published in English)
Janis & Friends Hepatitis C Support Web Site, http://janis7hepc.com/Shared%20Stories.htm
American Liver Foundation http://www.liverfoundation.org/ (Narratives no longer available online)
HCV Anonymous, http://www.hcvanonymous.com/stories.html
Of the eight websites identified in 2002, four continue to publish patients' HCV illness narratives, one is no longer available in English (HepC.de), two have removed the illness narratives (WebMD and American Liver Foundation), and one website is no longer in existence (Hepatitis C Aware).
Contributor Information
Eleanor Palo Stoller, Dept. of Sociology, Wake Forest University, Winston-Salem, North Carolina 27106
Noah J. Webster, Dept. of Sociology, Case Western Reserve University, Cleveland, Ohio 44106
Carol E. Blixen, Case Western Reserve University School of Medicine and Center for Health Care Research and Policy, Case Western Reserve University/MetroHealth Medical Center, Cleveland, Ohio 44109
Richard A. McCormick, Center for Health Care Research and Policy, Case Western Reserve University, Cleveland, Ohio 44106
Andrew J. Hund, Dept. of Sociology, Case Western Reserve University, Cleveland, Ohio 44106
Adam T. Perzynski, Center for Health Care Research and Policy, Case Western Reserve University, Cleveland, Ohio 44106
Stephanie W. Kanuch, Center for Health Care Research and Policy, Case Western Reserve University/MetroHealth Medical Center, Cleveland, Ohio 44109
Charles L. Thomas, Center for Health Care Research and Policy, Case Western Reserve University/MetroHealth Medical Center, Cleveland, Ohio 44109
Kyle Kercher, Dept. of Gerontology, University of Nebraska at Omaha, Omaha, Nebraska 68182
Neal V. Dawson, Case Western Reserve University School of Medicine and Center for Health Care Research and Policy, Case Western Reserve University/MetroHealth Medical Center, Cleveland, Ohio 44109
References
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The Prevalence of Hepatitis C Virus in the United States, 1999 through 2002. Annals of Internal Medicine. 2006;144:705–715. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT The Alcohol Use Disorders Identification Test Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Methods. Third. Walnut Creek, CA: Altamira Press; 2002. [Google Scholar]
- Blixen C, Webster N, Hund A, Perzynski A, Kanuch S, Stoller E, McCormick R, Dawson N. Communication about alcohol consumption between non-dependent drinkers with hepatitis C (HCV) and their health-care providers. Journal of General Internal Medicine. 2008;23(3):242–247. doi: 10.1007/s11606-007-0483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. Journal of Advanced Nursing. 2003;42:57–63. doi: 10.1046/j.1365-2648.2003.02579.x. [DOI] [PubMed] [Google Scholar]
- Brown SA, Christiansen BA, Goldman MS. The Alcohol Expectancy Questionnaire: An instrument for the assessment of adolescent and adult alcohol expectancies. Journal of Studies on Alcohol. 1987;48:483–491. doi: 10.15288/jsa.1987.48.483. [DOI] [PubMed] [Google Scholar]
- Cancer Prevention Research Center. University of Rhode Island; 2001. http://www.uri.edu/research/cprc/measures.htm#Alcohol. [Google Scholar]
- Center for Disease Control (CDC) Hepatitis C Fact Sheet. 2007 http://222.cdc.gov/hepatitis.
- Collins KMT, Onwuegbuzie AJ, Sutton IL. A model incorporating the rationale and purpose for conducting mixed-methods research in special education and beyond. Learning Disabilities: A Contemporary Journal. 2006;4(1):67–100. [Google Scholar]
- Conrad S, Garrett LE, Cooksley WGE, Dunne MP, MacDonald GA. Living with hepatitis C means ‘you just haven't got a normal life anymore.’. Chronic Illness. 2006:2121–131. doi: 10.1177/17423953060020020701. [DOI] [PubMed] [Google Scholar]
- Crabtree B, Miller W. Doing Qualitative Research. Second. Newbury Park, California: Sage Publications; 1999. [Google Scholar]
- Creswell JW, Plano Clark VL, Gutman ML, Hanson WE. Advanced Mixed Methods Research Designs. In: Tashakkori A, Teddlie C, editors. Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage Publications; 2003. pp. 209–240. [Google Scholar]
- Cunningham JA, Sobell LC, Gavin DR, Sobell MB. Assessing motivation for change: Preliminary development and evaluation of a scale measuring the costs and benefits of changing alcohol and drug use. Psychology of Addictive Behaviors. 1997;11:107–114. [Google Scholar]
- Delaney WP, Ames G. Work team attitudes, drinking norms, and workplace drinking. The Journal of Drug Issues. 1995;25(2):275–290. [Google Scholar]
- Esterberg KG. Qualitative Methods in Social Research. Boston: McGraw-Hill; 2002. [Google Scholar]
- Forthofer MS. Status of mixed methods in the health sciences. In: Tashakkori A, Teddlie C, editors. Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage Publications; 2003. pp. 527–540. [Google Scholar]
- Golden J, Conroy RM, O'Dwyer AM, Golden D, Hardouin JB. Illness-related stigma, mood and adjustment to illness in persons with hepatitis C. Social Science and Medicine. 2006;63:3188–3198. doi: 10.1016/j.socscimed.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Hezode C, Lonjon I, Roudot-Thoraval F, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of moderate alcohol consumption on histological activity and fibrosis in patients with chronic hepatitis C, and specific influence of steatosis: a prospective study. Alimentary Pharmacology & Therapeutics. 2003;17:1031–1037. doi: 10.1046/j.1365-2036.2003.01546.x. [DOI] [PubMed] [Google Scholar]
- Hobbs WR, Rall TW, Verdoorn TA. Hypnotics and Sedatives; Ethanol. In: Hardman JG, Limbard LE, editors. Goodman & Gilman's Pharmacological Basis of Therapeutics. 9th. Boston: McGraw-Hill; 1996. pp. 361–396. [Google Scholar]
- Hoofnagle JH. Hepatitis C: The Clinical Spectrum of Disease. Hepatology. 1990;27(3):15S–20S. doi: 10.1002/hep.510260703. [DOI] [PubMed] [Google Scholar]
- Horn JL, Wanberg KW, Foster FM. Guide to the Alcohol Use Inventory (AUI) Minneapolis, MN: National Computer Systems; 1997. [Google Scholar]
- Jamison KR. The many stigmas of mental illness. Lancet. 2006;367(9509):708–714. doi: 10.1016/S0140-6736(06)68187-7. [DOI] [PubMed] [Google Scholar]
- Johnson RB, Onwuegbuzi AJ, Turner LA. Toward a definition of mixed method research. Journal of Mixed Methods Research. 2007;1(2):112–122. [Google Scholar]
- Lichtenstein B. Stigma as a barrier to treatment of sexually transmitted infection in the American deep south: issues of race, gender and poverty. Social Science and Medicine. 2003;57(12):2435–2445. doi: 10.1016/j.socscimed.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Lee YJ, Greene J. The predictive validity of an ESL placement test: A mixed methods approach. Journal of Mixed Methods Research. 2006;1(4):366–389. [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- McMahon J, Jones BT. The Negative Alcohol Expectancy Questionnaire. Journal of the Association of Nurses in Substance Abuse. 1993;12:17. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Test Manual NIAAA Project MATCH Monograph Series Vol 4. Washington, DC: U.S. Government Printing Office; 1995. The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of alcohol Abuse; pp. 95–3911. NIH Pub. No. 95-3911. [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers' motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. [Google Scholar]
- Morse JM. Principles of mixed methods and multimethod research design. In: Tashakkori A, Teddlie C, editors. Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage Publications; 2003. pp. 189–208. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol-Medication Interactions. Alcohol Alert. 2007 Retrieved August 6, 2007. No 27. http://pubs.niaaa.nih.gov/publications/aa27.htm, 1995.
- Pessione F, Degos F, Macellin P, Duchatelle V, Njapoum C, Martinot-Peignouz M, Degott C, Valla D, Erlinger S, Rueff B. Effect of Alcohol Consumption on Serum Hepatitis C Virus RNA and Histological Lesions in Chronic Hepatitis C. Hepatology. 1998;27(6):1717–1722. doi: 10.1002/hep.510270635. [DOI] [PubMed] [Google Scholar]
- Petchers M, Singer M. Perceived benefit of drinking scale: Approach to screening for adolescent alcohol use. Journal of Pediatrics. 1987;110:977–981. doi: 10.1016/s0022-3476(87)80431-6. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi MG, Marcus BH, Rakowski W, Fiore C, Harlow LL, Redding CA, Rosenbloom D. Stages of Change and Decisional Balance for 12 Problem Behaviors. Health Psychology. 1994;13:39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Rhodes T. Risk theory in epidemic times: sex, drugs and the social organization of ‘risk behavior’. Sociology of Health & Illness. 1997;19:208–227. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection pf Persons with Harmful Alcohol Consumption- II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Scott SB, Bergeman CS, Verney A, Longenbaker S, Markey MA, Bisconti TL. Social support in widowhood: A mixed methods study. Journal of Mixed Methods Research. 2007;1(3):244–266. doi: 10.1177/1558689807302453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoller E, Hund A, Webster N, Blixen C, Perzynski A, McCormick R, Kanuch S, Dawson N. Alcohol consumption within the context of Hepatitis C: A qualitative study of non-problematic drinkers. Alcohol & Alcoholism. 2006;41(5):546–552. doi: 10.1093/alcalc/agl055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoller E, Webster N, Blixen C, McCormick A, Perzynski C, Kanuch S, Dawson N. Lay management of chronic disease: A qualitative study of living with Hepatitis C infection. American Journal of Health Behavior. doi: 10.5993/ajhb.33.4.4. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RMcD, Oei TPS, Crook GM. Development of a Drinking Self-Efficacy Questionnaire. Journal of Psychopathology and Behavioral Assessment. 1991;13(1):1–15. [Google Scholar]
- Young RMcD, Knight RG. The Drinking Expectancy Questionnaire: A Revised Measure of Alcohol-Related Beliefs. Journal of Psychopathology and Behavioral Assessment. 1989;11(1):99–112. [Google Scholar]
- Westin J, Lagging LM, Spak F, Aires N, Svensson E, Lindh M, Dhillon AP, Norkrans G, Wejstal R. Moderate alcohol intake increases fibrosis progression in untreated patients with hepatitis C virus infection. Journal of Viral Hepatitis. 2002;9:235–241. doi: 10.1046/j.1365-2893.2002.00356.x. [DOI] [PubMed] [Google Scholar]
- Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- Wilson HS, Hutchinson SA, Holzemer WL. Reconciling incompatibilities: A grounded theory of HIV medication adherence and symptom management. Qualitative Health Research. 2002;12:1309–1322. doi: 10.1177/1049732302238745. [DOI] [PubMed] [Google Scholar]
- Wong JB, McQuillan GM, McHutchison JG, Poynard T. Estimating future hepatitis C morbidity, mortality, and costs in the United States. American Journal of Public Health. 2000;90:1562–1569. doi: 10.2105/ajph.90.10.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Connors GJ, Maisto SA, Westerberg VS. Relapse research and the Reasons for Drinking Questionnaire: a factor analysis of Marlatt's relapse taxonomy. Addiction. 1996;91(Suppl):S121–30. [PubMed] [Google Scholar]


