Abstract
Overall health status after a disaster may be associated with long-term physical morbidity and mortality. Little is known about factors associated with overall health status in the aftermath of disasters. We examined self-rated health in relation to disaster characteristics, social resources, and post-disaster outcomes in a sample of adults who experienced the 2004 Florida hurricanes. We interviewed a representative sample of 1,452 adults aged 18 years and older residing in the 33 Florida counties that were in the direct path of at least one of the 2004 hurricanes (Charley, Frances, Ivan, Jeanne). Overall health status was assessed using a self-rating format known to be predictive of mortality. Poor self-rated health was endorsed by 14.6% of the sample. Final multivariable models showed that poor self-rated health was associated with older age (p < 0.001), extreme fear during the hurricane (p = 0.03), low social support (p = 0.03), and depression (p = 0.003) since the hurricane. Self-rated health following the Florida hurricanes was strongly associated with two variables (social support and depression) that potentially can be mitigated through targeted interventions after disasters. Future work should evaluate secondary prevention strategies that can address general health-related concerns in the wake of a disaster.
Keywords: Disasters, self-rated health, PTSD, Depression
A substantial body of research has examined the mental health correlates of disasters and other major life stressors (1–3). Over 200 studies have examined psychosocial outcomes in the disaster literature alone, the vast majority focusing on mental health problems or health-risk behavior (4). Considerably less is known about the prevalence and risk factors associated with overall health status in disaster-affected communities. Overall health status—as assessed via self-rated health—is known to be related to long-term morbidity, mortality, economic burden, and impairment in occupational and social functioning (5–9) and it is important to understand its determinants among persons who experience disasters and other large-scale incidents. In particular, identification of potentially modifiable determinants of health status is important because this may provide insight into interventions and strategies that can mitigate the adverse health consequences of mass traumatic events.
Disasters (i.e., natural disasters, technological disasters, terrorist attacks, or other large-scale incidents that affect one or more communities) represent a unique set of stressors that have received increased research attention in recent years. However, existing research about the consequences of disasters is limited by the frequent use of non-representative samples, relatively small sample sizes, and assessment protocols that exclude measurement of overall health status and related outcomes (3, 10–11). Although few studies have overcome all of these limitations, several have identified factors that account for variability in overall health status following a disaster. First, psychopathology such as posttraumatic stress disorder (PTSD), depression, and anxiety (3, 12–13) may relate to health outcomes via a variety of biological [e.g., immune suppression, hypothalamic-pituitary-axis (HPA) axis dysregulation] or behavioral mechanisms (e.g., low levels of healthy activity, increased health-risk behavior). Indeed, depression has been associated with poor self-reported health (14). Second, in the post-disaster context, community and social resources may jointly influence mental and physical health. Social support in particular has been identified as a protective factor for post-disaster mental health problems (3, 12–13) and it may collaterally buffer the overall health effects of disasters. Third, health status may be affected by increases in health-risk behavior that occur in the aftermath of disasters, including alcohol and illicit drug use, cigarette consumption, risky sexual behavior, and poor sleep habits (3, 15–18). Fourth, individuals with pre-existing health conditions may encounter barriers to care (e.g., difficulty filling prescriptions, overburdened health care facilities) and experience increased symptoms post-disaster (19). As older adults are more likely to report poor self-rated health (7), they may be particularly at risk. However, it is notable that depression is more prevalent in younger than older adults (20–22), suggesting that associations between depression and overall health may differ as a function of age.
The 2004 Atlantic season devastated Florida, USA, with four hurricanes (Charley, Frances, Ivan, Jeanne), three of which made landfall as major hurricanes. These hurricanes were directly responsible for nearly 50 deaths and over $40 billion in damage (23) as well as substantial psychological distress in affected communities (12, 19). Psychological impairment was particularly evident among those with low social support and high hurricane exposure (12). Several post-hurricane experiences also may have contributed to an increased risk of physical health problems among vulnerable individuals. A report by the Centers for Disease Control and Prevention (CDC) found that, among persons with medical conditions, after the hurricanes 14% had difficulty obtaining medication, 5% indicated a worsening of their condition, and 9% had difficulty accessing essential medical equipment. In this study, we used data collected after the 2004 Florida hurricanes to examine self-rated health in relation to demographic factors, disaster characteristics, psychological stressors and stress reactions, and social resources.
Method
Data Collection and Sample
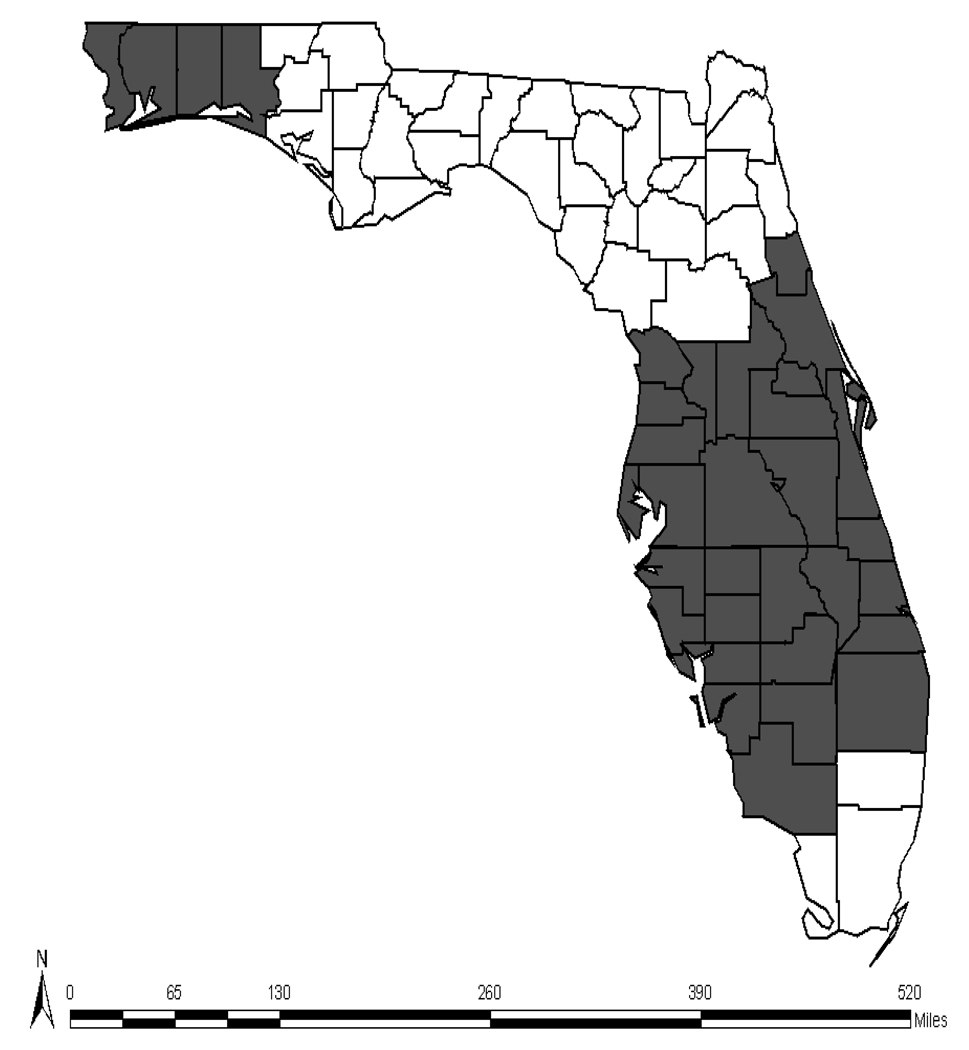
Data were collected from 1,452 adults aged 18 years and older residing in telephone households in Florida counties (n = 33) that were in the direct path of at least one of the 2004 hurricanes (12) (see Figure 1) and who provided complete data on age and gender. The sampling frame included an oversample of adults aged 60 years and over to address research questions specific to older adults (24). To correct for oversampling, data were weighted by gender and age to bring the sample in line with U.S. Census 2000 estimates of the population of Florida adults in the sampling frame. To accomplish this, sample frequencies were generated by gender and age cohort (18–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80+ years). Weightings were then generated for each gender × age-group cell based on comparisons between sample and population distributions using Census 2000 data from the 33 Florida counties in the sampling frame. No weighting by racial/ethnic status was necessary because sample distributions were highly comparable to Census-based population estimates for these counties.
Figure 1.
Shaded counties represent the sampling frame of only the 33 Florida counties found to be significantly affected by the 2004 hurricanes.
Random-digit-dial methods were used to screen households for eligibility. When multiple eligible participants were present within a household, the most recent birthday method was used to select the respondent. Land-line telephone interviews were conducted between April 5 and June 12, 2005. Informed consent was obtained verbally. Up to five attempts were made to contact an adult at each telephone number. Cooperation rate (i.e., [completes + screen-outs] divided by [completes + screen-outs + refusals before screen + qualified refusals]) was 70%. The cooperation rate among eligible individuals (i.e., completes divided by [completes + qualified refusals]) was 81%. The Institutional Review Board of the Medical University of South Carolina approved all study procedures.
Study Instruments
A structured computer-assisted telephone interview administered in English or Spanish included the following sections: demographics, hurricane exposure characteristics, social support, and post-hurricane mental health functioning and self-rated health. The interview averaged 26.5 minutes in length.
Hurricane exposure
Hurricane exposure was assessed with five important indicators identified in previous research on Hurricanes Hugo and Andrew on the basis of their relation to post-hurricane mental health functioning (25–26), and focused on peri- and post-hurricane effects on personal resources such as property and shelter. We assessed whether participants were physically present for hurricane-force winds, whether they experienced extreme fear during the hurricane, whether they had any damage to property, and whether they were displaced for at least a week. To characterize resource losses more fully, we also assessed whether total incurred losses (i.e., irrespective of insurance coverage) were greater than $10,000, and whether actual incurred out-of-pocket losses were greater than $1,000. We selected these levels of resource loss (displacement for more than a week, damage in excess of $10,000, and uninsured losses over $1,000) following review of archival data from Hurricane Hugo survivors (25–26) in which these approximate figures (adjusted for inflation) were associated with adverse outcomes.
Traumatic event history
Participants were asked if they had ever been exposed to a potentially traumatic event during which they experienced fear of being killed or seriously injured: natural disasters other than the 2004 hurricanes (“a natural disaster, such as a major earthquake, hurricane, flood, or tornado”), serious accidents (“a serious accident at work, in a car, or somewhere else”), being physically attacked (“been attacked with a gun, knife, or some other weapon;” “been attacked without a weapon, but with the intent to kill or seriously injure you”), and being in military combat (“have you ever been in military combat or in a war zone?”). This variable was coded dichotomously (yes/no).
Social support
Pre-disaster social support was assessed for the six-month period immediately prior to the hurricane using a modified 5-item version of the Medical Outcomes Study module (27). Five items measured three aspects of social support: emotional (e.g., “someone available to love you and make you feel wanted”), instrumental (e.g., “someone available to help you if you were confined to bed”), and appraisal (e.g., “someone available to give good advice in a crisis”). Answers ranged from “none of the time” to “all of the time” (4-point scale), and respondents were categorized in a manner consistent with our September 11 study (13), with scores divided into low (lowest 1/3 of the sample) or high (upper 2/3 of the sample) social support. This scale had good reliability (alpha = .85).
PTSD
We assessed PTSD since the hurricanes using the National Women’s Study PTSD module (NWS-PTSD; 28) a widely used measure in population-based epidemiological research originally modified from the Diagnostic Interview Schedule. Research on the NWS-PTSD has provided support for concurrent validity and several forms of reliability (e.g., temporal stability, internal consistency, diagnostic reliability) (2, 29–30). The NWS-PTSD was also validated against the SCID (31), a well-established diagnostic interview, in the DSM IV PTSD Field Trial (32). In the Field Trial, inter-rater kappa coefficient was .85 for PTSD and comparisons between the NWS-PTSD module and the SCID yielded a kappa coefficient of .71 for past-6-months and .77 for lifetime PTSD (32). We defined PTSD based on DSM-IV symptom requirements (i.e., three avoidance, one intrusion, and two arousal symptoms), including functional impairment. Among individuals completing the NWS-PTSD module, Cronbach’s alpha was .86.
Generalized Anxiety Disorder (GAD) since the hurricanes
was measured using a slightly modified version of the SCID-IV (31) structured interview questions that correspond directly to DSM-IV criteria using yes/no response options. The diagnosis required excessive and poorly controlled anxiety and worry occurring more days than not for a period of 6–9 months (“since the hurricanes”), as well as at least three of six hallmark GAD symptoms: restlessness, fatigue, concentration problems, irritability, tension, and sleep disturbance. This scale showed good internal consistency in the current sample among individuals screening into the module (Cronbach’s alpha = .85).
Major Depressive Episode (MDE) since the hurricanes
was measured using structured interview questions modified from the SCID-IV (31) that targeted MDE criteria using yes/no response formats for each DSM-IV symptom. Following DSM-IV guidelines, respondents met criteria for MDE if they endorsed five or more depressive symptoms occurring over at least a two-week period. Support for internal consistency and convergent validity exist for this measure (2, 33). Boscarino (33) compared the depression module (past-year time frame) against the depression scale of the Brief Symptom Inventory-18, yielding a sensitivity of 73% and specificity of 87% in detecting MDE as classified by our instrument. Receiver operating characteristic analysis using a BSI cutoff score of 65 or higher (clinical cutoff) optimally predicted depression (area under the curve = .89). Cronbach’s alpha in this sample for the MDE module was .82.
Substance use
We assessed cigarette smoking and alcohol consumption since the hurricanes using questions that were modified from our previous work with New York City-area residents after the September 11 attacks (18). Cigarette use was assessed with the question, “Since the 2004 hurricanes, have you smoked cigarettes every day, some days, or not at all?” Increased use of cigarettes was assessed by asking, “Since the 2004 hurricanes, have you been smoking more cigarettes than before the hurricanes?” Increased alcohol consumption was assessed with the following question: “Since the 2004 hurricanes, have you been drinking more alcohol than before the hurricanes?”
Self-rated health
Self-rated health was assessed with the question, “Compared to other people your age, is your health excellent, very good, good, fair, or poor?” Two general strategies of measuring self-rated health exist (34). One strategy entails the use of measures that consist of multiple items whose summation yields a total score reflecting overall health (e.g., General Health Questionnaire; 35), whereas the other involves the use of a single global item (6). The global self-rated health strategy is highly correlated with longer self-report measures of health (35), has demonstrated test-retest reliability (36), is a strong predictor of physical morbidity and mortality (7–8, 37), has been used in the post-disaster context (38), and is an increasingly popular method of subjective health assessment (34). Furthermore, the global self-rated health strategy has been used with individuals across the lifespan, including adolescents, middle-aged adults, and elderly adults, as well as among participants from a variety of ethnic and racial backgrounds (6, 37–39). Consistent with previous research using this measure (40), we dichotomized responses into good (response options of “excellent,” “very good,” or “good”) vs. poor (“fair” or “poor”) self-rated health.
Statistical Analyses
Weights were developed to account for differential probability of household and respondent selection. Predictor variables were selected on the basis of their relevance to overall health status based on prior research (3). Four separate logistic regression analyses were conducted to identify variables within each predictor set (i.e., demographic, hurricane-related, social support and traumatic event history, and psychopathology and substance use) that were associated with self-rated health. Significant predictors emerging from these analyses were entered into a final multivariable logistic regression analysis. Post-hoc descriptive analyses also were conducted to examine depression and self-rated health in relation to age group. The SUDAAN statistical package was used for all analyses to account for survey weighting. For significance testing, alpha was set a priori at 0.05.
Results
Sample characteristics are described in Table 1. The sample was approximately evenly divided between men and women. About three-fourths were European American, non-Hispanic; 11% were African American; and 9% were Hispanic. The most prevalent hurricane-related effects endorsed were damage from the hurricane (63.9%) and having out-of-pocket (i.e., uninsured) expenses of at least $1,000 (31.8%). A small but meaningful subset of participants met criteria for PTSD (3.6%), MDE (6.1%), and GAD (5.5%) since the hurricanes; over 1 in 10 met criteria for at least one of these mental health disorders. Increased cigarette and alcohol consumption since the hurricanes were endorsed by 7.4% and 8.6% of the sample, respectively. Poor self-rated health was endorsed by 1 in 7 adults (14.6%). Table 2 presents a correlation matrix of all variables.
Table 1.
Sample Characteristics (Weighted)
| n | % | |
|---|---|---|
| Gender | ||
| Male | 698 | 48.1 |
| Female | 754 | 51.9 |
| Ethnicity | ||
| Caucasian | 1102 | 76.6 |
| African American | 164 | 11.4 |
| Hispanic | 129 | 9.0 |
| Other | 43 | 3.0 |
| Income | ||
| <$15,000 | 149 | 12.0 |
| $15,000–$24,999 | 141 | 11.4 |
| $25,000–$49,999 | 468 | 38.8 |
| $50,000–$99,999 | 346 | 27.9 |
| 3 $100,000 | 135 | 10.9 |
| Age | ||
| <60 years | 987 | 68.0 |
| 3 60 years | 465 | 32.0 |
| Extremely afraid during hurricane | ||
| No | 1242 | 85.6 |
| Yes | 210 | 14.4 |
| Damage from hurricane | ||
| No | 524 | 36.1 |
| Yes | 928 | 63.9 |
| Displaced from home more than a week | ||
| No | 1397 | 96.2 |
| Yes | 55 | 3.8 |
| Amount of damage to home | ||
| <$ 10,000 | 1249 | 86.0 |
| 3 $ 10,000 | 203 | 14.0 |
| Out of Pocket Expense | ||
| <$ 1,000 | 990 | 68.2 |
| 3$ 1,000 | 683 | 31.8 |
| Prior trauma | ||
| No | 766 | 52.8 |
| Yes | 686 | 47.2 |
| Social support | ||
| High | 906 | 64.8 |
| Low | 491 | 35.2 |
| PTSD since hurricanes | ||
| No | 1399 | 96.4 |
| Yes | 53 | 3.6 |
| Depression since hurricanes | ||
| No | 1364 | 93.9 |
| Yes | 88 | 6.1 |
| Generalized anxiety disorder since hurricanes | ||
| No | 1372 | 94.5 |
| Yes | 80 | 5.5 |
| Cigarette smoking since hurricanes | ||
| Not at all | 1038 | 71.6 |
| Some days | 105 | 7.2 |
| Every day | 307 | 21.2 |
| Smoking more cigarettes than before the hurricanes | ||
| No | 1345 | 92.6 |
| Yes | 107 | 7.4 |
| Drinking more alcohol than before the hurricanes | ||
| No | 1328 | 91.4 |
| Yes | 124 | 8.6 |
Table 2.
Bivariate Correlations for all Variables
| Self-rated Health |
Gender | Hispanic | Black | Income | Age | Fear | Damage | Displaced | 10 K loss | Out of Expense |
Prior Trauma |
Social Support |
PTSD | MDD | GAD | Smoke | Increased Smoking |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | .04 | |||||||||||||||||
| Hispanic | −.02 | .04 | ||||||||||||||||
| Black | .05 | −.01 | .01 | |||||||||||||||
| Income | −.23*** | −.13*** | .06* | −.09** | ||||||||||||||
| Age | .11*** | .01 | .07** | −.11*** | −.26*** | |||||||||||||
| Fear | .13*** | .17*** | −.09** | .10*** | −.13*** | −.02 | ||||||||||||
| Damage | −.04 | −.01 | −.04 | −.01 | −.08** | .10*** | −.14*** | |||||||||||
| Displaced | .08** | .01 | −.02 | −.01 | −.05 | .03 | .13*** | −.18*** | ||||||||||
| 10 K loss | −.02 | −.05 | .05* | −.06* | .08** | −.004 | .06* | −.30*** | .24*** | |||||||||
| Out of Pocket Expense | .02 | .01 | −.04 | .03 | .13*** | −.07** | .15*** | −.41*** | .16*** | .39*** | ||||||||
| Prior Trauma | .08** | −.08** | −.09** | −.02 | .02 | −.19*** | .12*** | −.09*** | .04 | .01 | .05 | |||||||
| Social Support | −.16*** | .003 | .07* | −.05 | .19*** | .02 | −.08** | .03 | −.04 | .01 | −.04 | −.04 | ||||||
| PTSD | .14*** | −.02 | −.10*** | .05 | −.07** | −.04 | .13*** | −.05* | .09*** | .05 | .07** | .13*** | −.12*** | |||||
| MDD | .18*** | .04 | −.08** | −.01 | −.05 | −.07** | .06* | −.006 | .04 | .004 | −.02 | .11*** | −.15*** | .37*** | ||||
| GAD | .14*** | .08** | −10*** | .01 | −.08** | −.02 | .25*** | −.09*** | .14*** | .07** | .09** | .13*** | −.11*** | .23*** | .21*** | |||
| Smoke | −.08** | .03 | −.01 | .01 | .09** | .15*** | −.08** | .005 | −.03 | .02 | −.01 | −.11*** | .06* | −.05* | −.08** | −.07** | ||
| Increased Smoking | −.11*** | −.01 | .05* | .003 | .04 | .12*** | −.12*** | .03 | −.02 | −.02 | −.03 | −.08** | .09*** | −.13*** | −.21*** | −.14*** | .43*** | |
| Increased Drinking | .03 | .05* | .02 | −.02 | .03 | .09** | −.04 | .01 | −.01 | −.04 | −.03 | −.08** | .07** | −.11*** | −.09*** | −.09** | .10*** | .14*** |
p <.05.
p <.01.
p <.001
Table 3 describes results of logistic regression analyses within each predictor set: demographics, hurricane characteristics, social support and prior stressors, and mental health and substance use. First, in the analysis with demographic predictors, lower income and older age were associated with poor self-rated health. Second, analysis with hurricane characteristics revealed that extreme fear at the time of the hurricanes (OR = 2.0 vs. not extremely fearful) was the only variable associated with poor self-rated health2. Third, prior traumatic stressors (OR = 1.5 vs. no prior stressors) and low social support (OR = 2.5 vs. high social support) were associated with poor self-rated health. In the fourth analysis, MDE since the hurricanes (OR = 4.2 vs. no MDE) and GAD since the hurricanes (OR = 2.4 vs. no GAD) were associated with poor self-rated health; whereas PTSD and cigarette and alcohol consumption variables were unrelated.
Table 3.
Logistic Regressions Results: Risk Factors for Poor Health
| Predictor | OR | 95% CI | p-value |
|---|---|---|---|
| Model 1: Demographic Variables | |||
| Gender | |||
| Male | 1.00 | - | .46 |
| Female | 1.18 | 0.76–1.84 | |
| Hispanic | |||
| No | 1.00 | - | .99 |
| Yes | 0.99 | 0.30–3.22 | |
| Black | |||
| No | 1.00 | - | .33 |
| Yes | 0.60 | 0.21–1.69 | |
| Income | |||
| <$15,000 | 4.47 | 1.63–12.26 | .003 |
| $15,000–$24,999 | 3.37 | 1.22–9.33 | |
| $25,000–$49,999 | 2.54 | 1.00–6.46 | |
| $50,000–$99,999 | 0.98 | 0.33–2.85 | |
| ≥$100,000 | 1.00 | - | |
| Age | |||
| <60 years | 1.00 | - | .006 |
| ≥60 years | 1.88 | 1.20–2.95 | |
| Model 2: Hurricane-related Variables | |||
| Extremely afraid during hurricane | |||
| No | 1.00 | - | .005 |
| Yes | 1.96 | 1.22–3.14 | |
| Damage from hurricane | |||
| No | 1.00 | - | .56 |
| Yes | 1.14 | 0.73–1.78 | |
| Displaced from home more than a week | |||
| No | 1.00 | - | .07 |
| Yes | 2.08 | 0.95–4.54 | |
| Amount of damage to home | |||
| <$10,000 | 1.00 | - | .54 |
| ≥$10,000 | 0.84 | 0.47–1.48 | |
| Out of Pocket Expense | |||
| <$1,000 | 1.00 | - | .68 |
| ≥$1,000 | 0.90 | 0.53–1.51 | |
| Model 3: Prior Trauma and Social Support | |||
| Prior trauma | |||
| No | 1.00 | - | .045 |
| Yes | 1.50 | 1.01–2.23 | |
| Social support | |||
| High | 1.00 | - | <.001 |
| Low | 2.53 | 1.68–3.81 | |
| Model 4: Psychopathology and Substance Use Variables | |||
| PTSD since hurricanes | |||
| No | 1.00 | - | .15 |
| Yes | 2.29 | 0.74–7.10 | |
| Depression since hurricanes | |||
| No | 1.00 | - | .001 |
| Yes | 4.19 | 1.74–10.11 | |
| Generalized anxiety disorder since hurricanes | |||
| No | 1.00 | - | .04 |
| Yes | 2.38 | 1.05–5.37 | |
| Cigarette smoking since hurricanes | |||
| Not at all | 1.00 | - | .31 |
| Some days | 0.68 | 0.32–1.46 | |
| Every day | 1.34 | 0.73–2.45 | |
| Smoking more cigarettes than before the hurricanes | |||
| No | 1.00 | - | .83 |
| Yes | 0.90 | 0.36–2.30 | |
| Drinking more alcohol than before the hurricanes | |||
| No | 1.00 | - | .11 |
| Yes | 0.46 | 0.17–1.20 | |
A final multivariable analysis examined self-rated health in relation to variables that emerged as significant predictors via the aforementioned analyses. The majority of these variables were significant predictors in the final model (see Table 4). Factors associated with poor self-rated health included older age (OR = 3.1), extreme fear during the hurricane (OR = 1.9), low social support (OR = 1.7), and MDE since the hurricanes (OR = 5.0).
Table 4.
Logistic Regressions Results: Final Model of Risk Factors for Poor Health
| Predictor | OR | 95% CI | p-value |
|---|---|---|---|
| Income | |||
| <$15,000 | 2.48 | 0.93–6.59 | .07 |
| $15,000–$24,999 | 2.14 | 0.72–6.36 | |
| $25,000–$49,999 | 1.39 | 0.56–3.48 | |
| $50,000–$99,999 | 0.82 | 0.28–2.40 | |
| ≥$100,000 | 1.00 | - | |
| Age | |||
| <60 years | 1.00 | - | <.001 |
| ≥60 years | 3.06 | 1.90–4.93 | |
| Extremely afraid during hurricane | |||
| No | 1.00 | - | .03 |
| Yes | 1.87 | 1.08–3.24 | |
| Prior Trauma | |||
| No | 1.00 | - | .30 |
| Yes | 1.30 | 0.79–2.12 | |
| Social support | |||
| High | 1.00 | - | .03 |
| Low | 1.68 | 1.05–2.68 | |
| Depression since hurricanes | |||
| No | 1.00 | - | .003 |
| Yes | 5.02 | 1.75–14.40 | |
| Generalized anxiety disorder since hurricanes | |||
| No | 1.00 | - | .18 |
| Yes | 1.89 | 0.74–4.83 |
Secondary Analyses
Self-rated health was inversely related both to age cohort and depression in multivariable analyses. Yet, a significant body of research has shown that older adults are less likely than younger adults to have depression (20–22). Indeed, whereas older adults in this sample had a lower prevalence of depression than younger adults (3.4% vs. 7.4%) (24), they were more than twice as likely as younger adults to have poor self-rated health (24.1% vs. 10.1%). Post-hoc descriptive analyses examining depression and self-rated health in relation to age group revealed that among adults with poor overall health status, younger adults were more than four times as likely as older adults (33.0% vs. 8.0%) to meet criteria for depression since the hurricanes. Prevalence of depression was 4.5% and 2.0%, respectively, among younger vs. older adults in good health.
Discussion
Whereas a substantial body of research focuses on post-disaster mental health, little is known about the distribution and correlates of overall health status following disasters. The present study examined social and psychological predictors of self-rated health with a large population-based sample of adults affected by the 2004 Florida hurricanes. Analyses identified two potentially modifiable factors that were independently associated with poor self-rated health in the final model: low social support and depression. Two non-modifiable variables were also associated with self-rated health; older age (i.e., aged 60 years and over) and experiencing extreme fear during the hurricane. These findings have implications for the identification of at-risk populations after mass traumatic events and for interventions aimed at improving population health after these events.
The relation between depression and self-rated health was particularly strong: respondents with post-hurricane depression were five times more likely to endorse poor overall health status than their non-depressed counterparts. This relation is likely bi-directional and this study cannot determine temporal sequence of these two findings. In studies with older adults, health status has been identified as a predictor of depression (14). Changes in overall health status may precede depression in many cases, but in many others the temporal directionality may differ. For example, individuals experiencing sleep disturbance in the context of depressed mood may be likely to rate their health status negatively. Consistent with this suggestion, data indicate that dysregulation of neurobiologic systems in the thalamus and brainstem contributes to altered sleep in those who are depressed and that such sleep disturbances may lower immune system functioning and increase risk for poor health outcomes (41). Alternatively, a common factor, such as low physical activity, may play a role in both depression and overall health status.
Interpretation of the observed association between depression and poor health status is complicated by unknown temporal directionality. However, we suggest that the observed relation has implications for policy and practice, irrespective of directionality of association. These data strongly suggest that to enhance identification of at-risk individuals in the post-disaster context, disaster responders could screen for depression when individuals, particularly young adults, present with health-related concerns. For cases in which depressed mood has preceded changes in perceived health status, interventions that successfully treat depression after disasters and other large-scale incidents may collaterally improve perceived health. In other cases involving comorbid depression and poor overall health status, it may be particularly important to include intervention components that address behavioral outcomes that may relate closely both to depression and health outcomes, such as healthy sleep patterns, eating habits, and activity levels. These domains of health-risk behavior likely are associated with susceptibility to depression and poor overall health status, and disaster victims are at high risk for disruption of daily routines associated with each of these areas. Disaster victims who have property damage/loss, loved ones who were affected by the disaster, injury, or other circumstances requiring significant time, attention, money, and/or effort may experience major disruptions in their every day routines that can affect all three of these areas. Strategies consistent with principles of behavioral activation, such as encouraging pleasant and functional activities in the aftermath of a disaster, may serve to lower susceptibility. Alternatively, individuals for whom health problems are preceded by (and are related to) depression may benefit more directly from interventions that address relevant health issues and needs. Therefore, disaster responders should have the resources to address the needs of disaster victims on both of these levels.
PTSD was less strongly associated with overall health status. Bivariate analyses found that PTSD and poor health were significantly positively correlated. However, when examining all mental health variables in one multivariable regression, PTSD did not add predictive value, perhaps due to the high amount of shared variance between PTSD and MDD (r=.37, p<.001). Notably, peritraumatic fear, a component of PTSD, was predictive of poor health status, suggesting that threat perception may play an important role. This is consistent with research indicating that threat perception is related to behavioral changes (e.g., decreased activity), which may in turn, be related to poor health (43).
High levels of perceived pre-disaster social support were also found to be a protective factor in this study, consistent with past research (9). Although we did not measure post-disaster social support, help in the form of instrumental assistance (e.g., food, shelter), emotional support, and simple companionship delivered via churches, synagogues, mosques, senior centers, schools, and other public or semi-public institutions may well be among the best and most efficient approaches to community-based intervention following natural disasters such as hurricanes for the great majority of affected individuals (42). Ready access to these forms of assistance may be important both for mental health and positive overall health perceptions by addressing symptoms of depression and providing a natural environment that is supportive of healthy activities and routines.
This was one of the first studies to examine social and psychological correlates of self-rated health using a large, representative disaster-affected sample of adults. This study also had several limitations. First, findings are based strictly on retrospective self-report data. Although most of our interview questions referenced relatively short time frames with a clear anchor (e.g., “since the hurricanes”), the lack of supplementary forms of assessment prevented the identification of recall biases. In addition, because our sample consisted exclusively of disaster-affected adults, we were unable to account for the possibility that participants’ health ratings were skewed by self-comparisons to non-disaster victims. Second, our interview was necessarily brief because a lengthy interview would have been cost-prohibitive. Use of a brief interview prevented comprehensive assessment of health outcomes and hurricane exposure characteristics (such as injury resulting from the disasters) as well as the temporal directionality of mental health outcomes, health-risk behavior, and self-rated health. This includes an inability to determine the onset of mental health problems identified within our sample, which precluded an opportunity to control for pre-disaster mental health and social support in analyses. Third, participants were interviewed only once. A longitudinal component to the study would have provided better information about long-term perceived health for which post-disaster increases in cigarette, alcohol, and drug use may have emerged as more salient risk factors. Fourth, generalizability of our findings to communities affected by different types of disasters is unclear. Fifth, data are not available to characterize the pre-disaster functioning of the sample. The Behavioral Risk Factor Surveillance System (BRFSS), a state-based system of telephone health surveys supported by the Centers for Disease Control and Prevention, asks participants, “How is your general health?” Results from the 2004 BRFSS survey in Florida indicated that 16.5% of respondents self-rated their health status as poor (i.e., either “fair” or “poor,” as was defined in the present study). Although this percentage is comparable to the prevalence in the current study (14.6%), the different question structures between our study and the BRFSS survey preclude a direct comparison.
The present study identified two key potentially modifiable factors associated with poor self-rated health following a disaster: depression and social support. Post-disaster screening for the presence of these and other (non-modifiable) factors such as older age, low income, and extreme fear during the disaster may result in the identification of disaster victims at risk for poor overall health status. Identification of individuals who share these risk characteristics may allow for improved access to needed community resources that have the potential to accelerate the natural post-disaster recovery period, improve quality of life, and reduce the long-term direct and indirect economic burden at the individual and societal level.
Acknowledgments
This research was supported by National Institute of Mental Health RAPID Grant MH05220-01A2 (Principal Investigator: Ron Acierno, Ph.D.). Views in this article do not represent those of the funding agency.
Footnotes
An exploratory model of hurricane-related variables was conducted with the predictors described above, controlling for the total number of hurricanes the participant experienced. This analysis yielded the same pattern of results, and total number of hurricanes did not emerge as a significant predictor of health status.
References
- 1.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- 2.Kilpatrick DG, Ruggiero KJ, Acierno RE, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 3.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak, Part I: an empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 4.Norris FH, Elrod CL. Psychosocial consequences of disaster: A review of past research. In: Norris FH, Galea S, Friedman MJ, et al., editors. Methods for disaster mental health research. New York: Guilford; 2006. pp. 20–42. [Google Scholar]
- 5.Ullman SE, Siegel JM. Traumatic events and physical health in a community sample. Journal of Traumatic Stress. 1996;9:703–719. doi: 10.1007/BF02104098. [DOI] [PubMed] [Google Scholar]
- 6.Idler EL, Angel R. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. American Journal of Public Health. 1990;80:446–452. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant M, Piotrowski Z, Chappell R. Self-reported health and survival in the longitudinal study of aging, 1984–1986. Journal of Clinical Epidemiology. 1995;48:375–387. doi: 10.1016/0895-4356(94)00143-e. [DOI] [PubMed] [Google Scholar]
- 8.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 9.Ren XS, Skinner K, Lee A, Kazis L. Social support, social selection and self-assessed health status: results from the veterans health study in the United States. Social Science & Medicine. 1999;48:1721–1734. doi: 10.1016/s0277-9536(99)00069-6. [DOI] [PubMed] [Google Scholar]
- 10.Adams RE, Boscarino JA, Galea S. Alcohol use, mental health status and psychological well-being 2 years after the World Trade Center attacks in New York City. Am J Drug Alcohol Abuse. 2006;32:203–224. doi: 10.1080/00952990500479522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Norris FH. Range, magnitude, and duration of the effects of disasters on mental health: Review update. Dartmouth College: Research Education Disaster Mental Health; 2005. [Google Scholar]
- 12.Acierno R, Ruggiero KJ, Galea S, Resnick HS, Koenen K, Roitzsch J, de Arellano M, Boyle J, Kilpatrck DG. Psychological sequelae of the 2004 Florida hurricanes: Implications for post-disaster intervention. Am J Public Health 2007. 2002;97:S103–S108. doi: 10.2105/AJPH.2006.087007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galea S, Ahern J, Resnick H, Kilpatrick DG, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine. 346:982–989. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- 14.Berkman LF, Berkman CS, Kasl S, Freeman DH, Leo L, Ostfeld AM, Cornoni-Huntley J, Brody JA. Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Public Health. 1986;124:372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- 15.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 16.Rheingold AA, Acierno R, Resnick HS. Trauma, ptsd, and health risk behaviors. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 217–243. [Google Scholar]
- 17.Vlahov D, Galea S, Ahren J, Resnick HS, Kilpatrick DG. Sustained increased consumption of cigarettes, alcohol, and marijuana among manhattan residents after September 11, 2001. American Journal of Public Health. 2004;94:253–254. doi: 10.2105/ajph.94.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, Gold J, Kilpatrick DG. Increased use of cigarettes, alcohol, and marijuana use among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology. 2002;155:988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Epidemiologic assessment of the impact of four hurricanes --- Florida, 2004. Morbidity & Mortality Weekly Reports. 2005;54:693–697. [PubMed] [Google Scholar]
- 20.Henderson AS, Jorm AF, Korten AE, Jacomb P, Christensen H, Rodgers B. Symptoms of depression and anxiety during adult life: evidence for a decline in prevalence with age. Psychological Medicine. 1998;6:1321–1328. doi: 10.1017/s0033291798007570. [DOI] [PubMed] [Google Scholar]
- 21.Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychological Medicine. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush J, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (NCS-R) JAMA. 2003;23:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 23.National Oceanic and Atmospheric Administration. [Retrieved July 7, 2006];Hurricane history. 2006 from http://www.nhc.noaa.gov/HAW2/english/history.shtml.
- 24.Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults following the 2004 Florida Hurricanes. American Journal of Geriatric Psychiatry. 2006;14:1051–1059. doi: 10.1097/01.JGP.0000221327.97904.b0. [DOI] [PubMed] [Google Scholar]
- 25.Freedy J, Saladin M, Kilpatrick DG, Resnick HS, Saunders BE. Understanding acute psychological distress following natural disaster. Journal of Traumatic Stress. 1994;7:257–273. doi: 10.1007/BF02102947. [DOI] [PubMed] [Google Scholar]
- 26.Freedy J, Resnick H, Kilpatrick DG. Conceptual framework for evaluating disaster impact: Implications for clinical intervention. In: Austin LS, editor. Clinical response to trauma in the community. Washington, DC: American Psychiatric Press; 1993. pp. 3–23. [Google Scholar]
- 27.Sherbourne CD, Stewart AL. MOS Social Support Survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 28.Kilpatrick DG, Resnick HS, Saunders BE, Best CL. The National Women's Study PTSD Module. Charleston, SC: Medical University of South Carolina; 1989. [Google Scholar]
- 29.Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting & Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- 30.Ruggiero KJ, Rheingold AA, Resnick HS, Kilpatrick DG, Galea S. Comparison of two widely used PTSD-screening instruments: Implications for public mental health planning. Journal of Traumatic Stress. 2006;19:699–707. doi: 10.1002/jts.20141. [DOI] [PubMed] [Google Scholar]
- 31.Spitzer RL, Williams J, Gibbon M. Structured Clinical Interview for DSM-IV. Washington DC: American Psychiatric Press; 1995. [Google Scholar]
- 32.Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick PA, Roth S, van der Kolk B. The posttraumatic stress disorder field trial: Evaluation of the PTSD construct: Criteria A through E. In: Widiger T, et al., editors. DSM-IV sourcebook. Washington, DC: American Psychiatric Press; 1988. pp. 803–844. [Google Scholar]
- 33.Boscarino JA, Galea S, Adams RE, Ahern J, Resnick HS, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001 terrorist attack. Psychiatric Services. 2004;55:274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- 34.Sibthorpe B, Anderson I, Cunningham J. Self-assessed health among indigenous Australians: How valid is a global question? American Journal of Public Health. 2001;91:1660–1663. doi: 10.2105/ajph.91.10.1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ware J, Sherbourne C. The MOS 36-Item short form health survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 36.Lorig K, Stweart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome measures for health education and other health care interventions. Thousand Oakes, CA: Sage; 1996. [Google Scholar]
- 37.McCullum J, Shadbolt B, Wang D. Self-rated health and survival: A 7-year follow-up study of Australian elderly. American Journal of Public Health. 1994;84:533–539. doi: 10.2105/ajph.84.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deeg DJH, Huizink AC, Comijs HC, Smid T. Disaster and associated changes in physical and mental health in older residents. European Journal of Public Health. 2005;15:170–174. doi: 10.1093/eurpub/cki126. [DOI] [PubMed] [Google Scholar]
- 39.Ren XS, Amick BC. Racial and ethnic disparities in self-assessed health status: Evidence from the national survey of families and households. Ethn Health. 1996;1:293–303. doi: 10.1080/13557858.1996.9961798. [DOI] [PubMed] [Google Scholar]
- 40.Shetterly SM, Baxter J, Maxon LD, Hammon RF. Self-rated health among Hispanic vs non-Hispanic while adults: The San Luis Valley health and aging study. American Journal of Public Health. 1996;86:1798–1801. doi: 10.2105/ajph.86.12.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ressler KJ, Nemeroff CB. Role of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disorders. Depression & Anxiety. 2000;12:2–19. doi: 10.1002/1520-6394(2000)12:1+<2::AID-DA2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 42.National Child Traumatic Stress Network and National Center for PTSD. Psychological First Aid: Field Operations Guide. 2005 [Google Scholar]
- 43.Grieger TA, Fullerton CS, Ursano RJ, Reeves JJ. Acute stress disorder, alcohol use, and perception of safety among hospital staff after the sniper attacks. Psychiatric Services. 2002;54:1383–1387. doi: 10.1176/appi.ps.54.10.1383. [DOI] [PubMed] [Google Scholar]