Abstract
Every cellular process is likely to be regulated by microRNAs, and an aberrant microRNA expression signature is a hallmark of several diseases, including cancer. MicroRNA expression profiling has indeed provided evidence of the association of these tiny molecules with tumor development and progression. An increasing number of studies have then demonstrated that microRNAs can function as potential oncogenes or oncosuppressor genes, depending on the cellular context and on the target genes they regulate. Here we review our current knowledge about the involvement of microRNAs in cancer and their potential as diagnostic, prognostic, and therapeutic tools.
INTRODUCTION
After the initial discovery in 1993, when a small RNA encoded by the lin-4 locus was associated to the developmental timing of the nematode Caenorhabditis elegans by modulating the protein lin-14,1 microRNAs have undergone a long period of silence. It took indeed several more years to realize that these small (19 to 22 nucleotides [nts]) RNA molecules are actually expressed in several organisms, including Homo sapiens, are highly conserved across different species, are highly specific for tissue and developmental stage, and play crucial functions in the regulation of important processes, such as development, proliferation, differentiation, apoptosis, and stress response. In the last few years, microRNAs have indeed took their place in the complex circuitry of cell biology, revealing a key role as regulators of gene expression.
MicroRNA genes represent approximately 1% of the genome of different species, and each of them has hundreds of different conserved or nonconserved targets: it has been estimated that approximately 30% of the genes are regulated by at least one microRNA.2
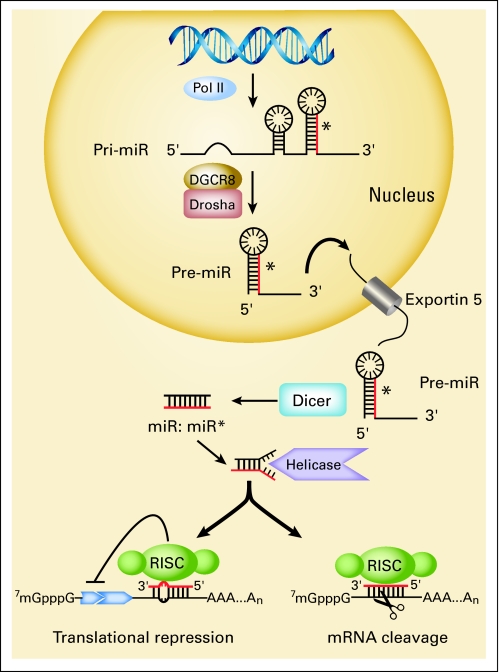
MicroRNAs are transcribed for the most part by RNA polymerase II as long primary transcripts characterized by hairpin structures (pri-microRNAs) and processed into the nucleus by RNAse III Drosha into 70- to 100-nts long premicroRNAs. These precursor molecules are exported by an Exportin 5-mediated mechanism to the cytoplasm, where an additional step mediated by the RNAse III Dicer generates a dsRNA of approximately 22 nts, named miR/miR*. The mature single-stranded microRNA product is then incorporated in the complex known as microRNA-containing ribonucleoprotein complex (miRNP), miRgonaute, or microRNA-containing RNA-induced silencing complex (miRISC), whereas the other strand is likely subjected to degradation. In this complex, the mature microRNA is able to regulate gene expression at the post-transcriptional level, binding through partial complementarity for the most part to the 3′UTR of target mRNAs, and leading at the same time to some degree of mRNA degradation and translation inhibition (Fig 1).
Fig 1.
Biogenesis, processing, and maturation of microRNAs (miRs). miRs are transcribed mainly by RNA polymerase II as long primary transcripts characterized by hairpin structures (pri-miRs) and processed in the nucleus by RNAse III Drosha in a 70-nucleotide-long pre-miR. This precursor molecule is exported by the Exportin 5 to the cytoplasm, where RNAse III Dicer generates a dsRNA of approximately 22 nucleotides, named miR/miR*. The mature miR product is then incorporated in the complex known as miRISC, whereas the other strand is likely subjected to degradation. As part of this complex, the mature miR is able to regulate gene expression binding through partial homology the 3′UTR of target mRNAs and leading to mRNA degradation in case of perfect matching or translation inhibition. RISC, RNA-induced silencing complex.
Our laboratory was involved in an attempt to identify tumor suppressors at chromosome 13q14, involved in the pathogenesis of chronic lymphocytic leukemia (CLL), the most common human leukemia in the Western world. Deletions of chromosome 13 at band q14 are detected by cytogenetic studies in approximatively 50% of CLLs, whereas loss of heterozygosity studies indicate deletions at 13q14 in approximatively 70% of CLLs. By taking advantage of chromosome translocations and small deletions, we found, however, that the critical region of 13q14 does not contain a protein-coding tumor suppressor gene, but rather two microRNA genes, miR-15a and miR-16-1, that are expressed in the same polycistronic RNA. This result indicated that the deletion of chromosome 13q14 caused the loss of these two microRNAs, representing the first evidence that microRNAs could be involved in the pathogenesis of human cancer.3 Study of a large collection of CLLs showed knockdown or knockout of miR-15a and miR-16-1 in approximatively 69% of CLLs. Because such alteration is present in most indolent CLLs, we speculated that loss of miR-15a and miR-16-1 could be the initiating event or a very early event in the pathogenesis of the indolent form of this disease.3
Immediately after these initial observations, we mapped all the known microRNA genes and found that many of them are located in regions of the genome involved in chromosomal alterations, such as deletion or amplification, in many different human tumors, in which the presumed tumor suppressor genes or oncogenes, respectively, failed to be discovered after many years of investigation.4
Here we will show that alterations in microRNA expression are not isolated, but the rule, in human cancer. After these early studies indicating the role of microRNA genes in the pathogenesis of human cancer, we and others have developed platforms to assess the global expression of microRNA genes in normal and diseased tissues and have carried out profiling studies to assess microRNA dysregulation in human cancer. This was an attempt to establish whether microRNA profiling could be used for tumor classification, diagnosis, and prognosis.
MicroRNAs PROFILING IN CANCER DIAGNOSIS AND PROGNOSIS
Profiling of different cell types and tissues indicated that the pattern of expression of microRNAs is cell type and tissue specific, suggesting that the program of expression of microRNAs is exquisitely cell-type dependent and tightly associated with cell differentiation and development. MicroRNAs aberrantly expressed in tumors are listed in Table 1.
Table 1.
MicroRNAs Aberrantly Expressed in Tumors
| Tumor Type | Upregulated MicroRNA | Downregulated MicroRNA | Target |
|---|---|---|---|
| CLL5–7 | miR-29, miR-181 | TCL1 | |
| miR-155 | |||
| miR-15a, miR-16-1 | BCL2 | ||
| AML8 | miR-29 | MCL1 | |
| DNMT | |||
| Lymphoma9–15 | miR-155 | ||
| miR-17-92 | PTEN, BIM,E2F1 | ||
| miR-106b-25 | E2F1 | ||
| MM16,17 | miR-21 | ||
| miR-19a, miR-19b | SOCS1 | ||
| Breast cancer18–27 | miR-21 | PTEN, PDCD4, TPM1 | |
| miR-125b | HER2, HER3 | ||
| miR-205 | HER3 | ||
| miR-10b (associated with metastasis) | HOXD10 | ||
| miR-373 | |||
| miR-200 | ZEB | ||
| Lung cancer28–32 | let-7 | RAS, HMGA2, C-MYC | |
| miR-155 | |||
| HCC28,34,35 | miR-122a | Cyclin G1 | |
| miR-221 | p27 | ||
| miR-34a | MET |
Abbreviations: CLL, chronic lymphocytic leukemia; AML, acute myelocytic leukemia; MM, multiple myeloma; HCC, hepatocellular carcinoma.
Leukemia/Lymphoma
CLL.
As mentioned, the first evidence of alterations of microRNA genes in human cancer came from studies of CLL. In a large study of indolent versus aggressive CLL, Calin et al6 discovered a signature of 13 microRNAs capable of distinguishing between indolent and aggressive CLL. Interestingly, it was found that miR-155, overexpressed in different lymphomas, including the activated B-cell–like type of diffuse large B-cell lymphoma, is also upregulated in aggressive CLLs, whereas members of the miR-29 family and miR-181 were found to be underexpressed and later demonstrated to directly regulate the TCL1 oncogene, which is overexpressed in the aggressive form of CLL.5 Because of the “wait and watch” approach to the treatment of CLL, a signature able to distinguish between CLL with good and bad prognosis was also found. Sequencing of many microRNAs, including those in the signature, allowed the identification of germline and somatic mutations of microRNA genes, including miR-15, miR-16-1, and miR-29 family members. Interestingly, mutations in the miR-15/16 precursor were also identified, affecting the processing of the pri-miR into the pre-miR. In two cases, the mutant was in homozygosity in the leukemic cells, whereas normal cells of the two patients were heterozygous for this abnormality, indicating a loss of the normal miR-15/16 allele in the leukemic cell.6 Thus miR-15a and miR-16-1 behave like typical tumor suppressors in CLL. Interestingly, Raveche et al36 have mapped a gene responsible for an indolent form of CLL in the New Zealand Black mouse strain on chromosome 14, in a region homologous to 13q14 in humans. Sequence analysis of this region showed a mutation in the precursor of miR-15/16 in the New Zealand Black mouse strain 6 nts 3′ to miR-16-1 (in the human cases, the mutation was 7 nts 3′ to miR-16-1), that also affected the processing of the miR-15/16 precursor. Thus germline mutation of miR-15/16 can cause the indolent form of CLL both in human and mouse. By using different algorithms to identify targets of miR-15a and miR-16-1, it was found that BCL2, an oncogene protecting cells from apoptosis, was a putative target of both miR-15a and miR-16-1. Knockdown experiments showed this to be the case.7 Thus loss of miR-15a and miR-16-1 leads to high constitutive level of the oncogene BCL2, contributing to the development of an indolent B-cell leukemia. In follicular lymphoma, another common indolent B-cell malignancy, the BCL2 gene becomes dysregulated as result of a t(14;18) chromosome translocation, because of its juxtaposition to immunoglobulin enhancers, indicating that constitutive overexpression of BCL2 causes an indolent B-cell tumor. More recently, it was also found that loss of miR-15a and miR-16-1 causes, although indirectly, overexpression of MCL1, another oncogene of the BCL2 family of inhibitors of apoptosis.37 Interestingly, a recent clinical trial of patients with CLL with ABT737, an inhibitor of BCL2 developed by Abbott Laboratories (Abbott Park, IL), showed partial resistance of the leukemic cells to the drug, because ABT737 is specific for BCL2 but not for MCL1. Thus treatment with either miR-15a or miR-16-1 may abrogate resistance to the drug and improve responsiveness. Additional experiments in vitro and in vivo also showed that miR-15a or miR-16-1 can be exploited to cause death of leukemic cells, suggesting the possibility of a microRNA-based therapeutic intervention.37
Acute myelocytic leukemia.
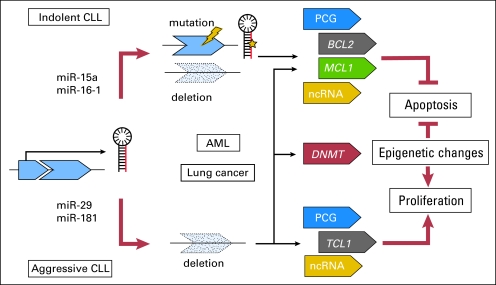
Acute myelocytic leukemia (AML) is a heterogeneous disease that includes several entities with different genetic abnormalities and clinical features. Garzon et al38 have reported unique microRNA profiles in the main molecular and cytogenetic subgroups of AML. In addition, a subset of these microRNAs was associated with overall and disease-free survival. The members of the miR-29 family are located in two clusters on two human chromosomes: miR-29b1/29a are located on chromosome 7q32, whereas miR-29b2/c are located on chromosome 1q23. Importantly, chromosome 7q is the region frequently deleted in myelodysplastic syndrome and therapy-related AML.39 Members of the miR-29 family have been shown to be downregulated in aggressive CLL,6 invasive breast cancer,18 lung cancer,40 and cholangiocarcinoma.8 Transfection of miR-29b induces apoptosis in cholangiocarcinoma cell lines and reduces the tumorigenicity of lung cancer cells in nude mice. Very recently, it was shown that rhabdomyosarcoma loses miR-29 expression because of an elevation of NFkB and YY1 levels, and introduction of miR-29s into the tumor delays rhabdomyosarcoma progression in mice.41 MiR-29s were also found to directly target MCL1,8 an oncogene overexpressed in AMLs, and the de novo DNA methyltransferases DNMT-3A and -3B, although indirectly, through regulation of the transactivator Sp1, the maintenance DNA methyl transferase DNMT1.40,42 Thus loss of miR-29 family members results in the constitutive overexpression of MCL1 and of DNMT, causing epigenetic changes characteristic of AML. These recent results suggest that loss of miR-29s may be important, perhaps critical, for the pathogenesis of a major group of myelodysplastic syndromes and AMLs (Fig 2).
Fig 2.
Molecular alterations in chronic lymphocytic leukemia (CLL) and acute myelocytic leukemia (AML). Deletion or downregulation of microRNA (miR)-15a/miR-16-1 cluster, located at chromosome 13q14.3 and directly involved in the regulation of BCL2 and MCL1 expression, represent an early event in the pathogenesis of CLL. During the evolution of malignant clones, other microRNAs (miRs) can be deleted (such as miR-29) or overexpressed (such as miR-155), contributing to the aggressiveness of B-cell CLL. Such abnormalities can influence the expression of other protein-coding genes (PCGs), as TCL1 oncogene, directly regulated by miR-29 and miR-181, or affect other noncoding RNAs (ncRNAs). The consequences of this steady accumulation of abnormalities are represented by the reduction of apoptosis and the induction of survival and proliferation of malignant B cells, leading to the evolution of more aggressive clones. Members of the miR-29 family, lost in AML and in other tumor types as lung cancer, have also been shown to directly target MCL1 and DNMT3A and B.
Lymphoma.
Early studies have shown that miR-155 is upregulated in a subgroup of Burkitt's lymphoma, diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, and Hodgkin's lymphoma.9,10 This microRNA is encoded by the terminal portion of the BIC (B-cell integration cluster) gene, which was originally identified as a common retroviral integration site in avian leukosis virus–induced B-cell lymphomas.43 Our group demonstrated that mice overexpressing miR-155 in B lymphocytes develop polyclonal preleukemic pre–B-cell proliferation followed by full-blown B-cell malignancy.11 More recently, two knockout mice models have demonstrated a critical role of miR-155 in immunity by showing that BIC/miR-155−/− have defective dendritic cell functions, impaired cytokine secretion, and TH cells intrinsically biased toward TH2 differentiation.44,45 Moreover, miR-155 could represent the connection between inflammation, immunity, and cancer, because its expression can be induced by mediators of inflammation and is involved in response to endotoxic shock.46
He et al12 reported that miR-17-92 polycistron was upregulated in 65% of patients with B-cell lymphoma and demonstrated in a mouse model that this microRNA cluster cooperates with the oncogene MYC in accelerating tumor development. More recently, a different group observed that the overexpression of miR-17-92 in lymphocytes caused a lymphoproliferative disease, autoimmunity, and premature death.13 The enhanced proliferation of the transgenic lymphocytes was mediated by direct regulation of pro-apoptotic phosphatase and tensin homolog gene (PTEN) and Bim. O'Donnell et al14 investigated the regulation of miR-17-92 in lymphoma, demonstrating that the expression of this cluster is directly activated by the oncogene c-Myc. Moreover, miR-17-92 cluster, as well as its paralog, miR-106b-25,15 establish with the transcription factor E2F1, a downstream target of c-Myc, a negative feedback loop: E2F1 indeed represents a direct target of the two microRNA clusters, but it also induces their expression. Thus MYC simultaneously activates E2F1 transcription and limits its expression, allowing a tightly controlled proliferative signal.
Multiple myeloma.
Few recent evidences have linked microRNAs to this plasma cell malignancy, as the aberrant expression of miR-335, miR-342-3p, and miR-561 in comparison with normal plasma cells47 or the Stat3-mediated activation of the oncogenic miR-21 in response to interleukin-6.16 More recently, Pichiorri et al17 described a microRNA signature characteristic of this neoplasia. They evaluated by both microarray analysis and real-time polymerase chain reaction the expression of microRNAs in multiple myeloma (MM) –derived cell lines, CD138+ bone marrow peripheral cells from subjects with MM or monoclonal gammopathy of undetermined significance, and normal donors, identifying the oncogenic miR-21 and miR-181 among the microRNAs aberrantly expressed. Two miRNAs, miR-19a and 19b, part of the miR-17-92 cluster, were also shown to downregulate expression of SOCS-1, a gene frequently silenced in MM that plays a critical role in inhibiting interleukin-6 growth signaling. Moreover, xenograft studies using human MM cell lines treated with miR-19a and b precursors or miR-181a and b antagonists resulted in significant suppression of tumor growth in nude mice, confirming the involvement of these microRNAs in the development of MM and supporting the idea of a possible use of these molecules as a therapeutic tool.
MicroRNAs in Solid Malignancies
Breast cancer.
One of the first solid tumors to be profiled for microRNA expression was, in 2005, breast cancer. Iorio et al18 described the first microRNA signature characteristic of breast carcinoma, identifying 13 microRNAs able to discriminate tumors and normal tissues with an accuracy of 100%. Among the most significant microRNAs differentially expressed, some were extensively studied since their initial discovery and revealed an important role on the biology of breast cancer: miR-21, overexpressed in breast carcinoma, has been demonstrated to mediate cell survival and proliferation directly targeting the oncosuppressor genes PTEN, PDCD4, and TPM1, and it has been associated with advanced clinical stage, lymph node metastasis, and poor patient prognosis.19,20 This microRNA, one of the first cancer microRNAs described, has been found overexpressed in a variety of other malignancies: glioblastoma,48,49 ovary,50 lung,28,51 and more.52 In colorectal cancer and pancreas endocrine and exocrine tumor, miR-21 overexpression is also associated with poor survival and poor therapeutic outcome.53–55
Conversely, downregulated microRNAs, as miR-125b and miR-205, regulate oncogenes as tyrosine kinase receptors HER-2 and HER-3, respectively.21,22 Ectopic expression of miR-205 in a breast cancer cell line decreases proliferation and improves the responsiveness to tyrosine kinase inhibitors as gefitinib or lapatinib.22 MicroRNA expression is also related to some histopathologic features of breast carcinoma, such as estrogen receptor (ER) and progesterone receptor expression, grade and stage, and presence of invasion.18 Further studies have investigated the correlation between microRNA expression and the classification in different subtypes of breast cancer.56 Very recently, few groups have reported experimental evidence supporting the correlation between microRNAs and ER status: miR-206 directly targets ERα, and miR-221 and -222 confer tamoxifen resistance regulating p2757 and ERα.58 Unpublished data from our laboratories 58a describe a regulatory loop between ERα and miR-221 and miR-222: the two microRNAs are able to directly target ERα receptor, which in turn negatively regulates their expression, binding estrogen-responsive elements on their promoter region.
Lung cancer.
Let-7, tumor suppressor microRNA initially discovered in C. elegans, where it induces cell cycle exit and terminal differentiation, has been described as a new regulator of self-renewal and tumorigenicity of breast cancer cells,59 targeting molecules originally described in lung cancer: RAS29 as well as the oncogene HMGA2,29,30 and even MYC itself.31 Overexpression of let-7 microRNA family can suppress tumor development in mouse models of breast and lung cancer.59,60 In the two most common forms of non–small-cell lung cancers (NSCLCs; adenocarcinomas and squamous cell carcinomas), high expression of miR-155 and low expression of oncosuppressor let-7 are correlated with poor prognosis.28 The association of let-7a with survival was also confirmed by an independent study performed by Yu et al,32 who identified an microRNA signature as an independent predictor of cancer relapse and survival of patients with NSCLC.
As in other tumor types, also in lung cancer microRNAs can represent accurate diagnostic markers: very recently, it has been described that squamous and nonsquamous NSCLCs can be distinguished according to the expression of miR-205.61
Hepatocellular carcinoma.
In hepatocellular carcinoma (HCC), Murakami et al62 reported that miR-222, miR-106a, and miR-17-92 clusters are associated with the degree of tumor differentiation, whereas high levels of the oncosuppressor miR-125b are correlated with good survival.63 MiR-125b has also been shown to induce growth inhibition in vitro in a model of human thyroid anaplastic carcinoma.64 Other studies focused on the identification of molecules targeted by microRNAs deregulated in HCC: miR-122a, downmodulated in HCC, directly regulates Cyclin G1,33 and miR-221, upregulated in this neoplasia, directly targets p27,34 as also shown in thyroid cancer,64 glioblastoma,65 prostate cancer,66 and melanoma.67 One of the first evidences proving miR alteration in human melanoma is a genomic study performed by Zhang et al,68 who reported DNA copy abnormalities in microRNA genes also in two other epithelial tumors, breast and ovary. Interestingly, the results obtained by this genomic analysis were largely overlapping with the expression profiles on the same tumor types.18,50
MicroRNAs IN INVASION, ANGIOGENESIS, AND METASTASIS
MicroRNAs have been implicated not only in the development of primary tumors, but also in affecting progression and the metastatic phase of the disease. Indeed, several evidences show how microRNAs are involved in the regulation of biologic processes leading to the acquisition of metastatic potential, as adhesion, migration and invasion, and angiogenesis.
One of the first studies reporting a prometastatic role for a microRNA was published by Ma et al.24 They observed that miR-10b was downmodulated in all the breast carcinomas from metastasis-free patients, as previously reported,18 but surprisingly, 50% of metastasis-positive patients had elevated miR-10b levels in their primary tumors. Induced by transcription factor Twist, miR-10b inhibits the translation of mRNA encoding homeobox D10 (HOXD10), releasing the expression of the prometastatic gene RHOC and thus leading to tumor cell invasion and metastasis.
Through a functional screen aimed to discover microRNAs promoting cell migration in vitro, Huang et al25 identified miR-373 and validated its metastatic potential in tumor transplantation experiments using breast cancer cells.
MiR-34a, lost in several tumor types and involved in the network mediated by the well-known “genome guardian” p53,35 inhibits migration and invasion by downregulation of MET expression in human HCC cells.69
Being the epithelial-mesenchymal transition (EMT) thought to promote malignant tumor progression, several groups have recently investigated whether microRNAs are involved in this process, and a number of evidences support this hypothesis. Indeed, members of the miR-200 family of microRNAs and miR-205 have been shown to reduce cell migration and invasiveness targeting ZEB transcription factors, known inducers of EMT,26,27 and PKCε, as recently demonstrated in prostate cancer.70 The oncogenic miR-21 stimulates invasion, extravasation, and metastasis in different tumor types, included colorectal cancer71 and breast cancer,72 whereas oncosuppressor miR-205 has opposite effects, reducing invasion in vitro and suppressing lung metastasis in vivo.23 With the same aim of searching for regulators of breast cancer metastasis, Tavazoie et al73 identified miR-126 and miR-335 as metastasis suppressors: reduced levels of the two microRNAs are associated with poor metastasis-free survival of patients with breast cancer, whereas their re-expression inhibits metastasis in a cell transplantation model.
Interestingly, it has been recently observed that primary tumors and metastasis from the same tissue show a similar pattern of microRNA expression.74 Being a more accurate classifier than mRNA expression studies, microRNA profiling has thus revealed the potential to solve one of the most demanding issues in cancer diagnostics: the origin of metastasis of unknown primary tumors.
In the metastatic process, neoangiogenesis is the crucial step allowing cells to reach and disseminate through the systemic circulation. microRNAs can also control tumor progression at this level, either promoting or inhibiting the proliferation of endothelial cells. miR-221 and miR-222 repress proliferative and angiogenic properties of c-Kit in endothelial cells,75 whereas hypoxic reduction of miR-16, miR-15b, miR-20a, and miR-20b, directly targeting vascular endothelial growth factor, supports the angiogenic process.76 On the other hand, vascular endothelial growth factor levels can be indirectly increased by miR-27b, through reduction of the zinc finger protein ZBTB10 and the consequent activation of Sp transcription factor,77 and by miR-126, through repression of Sprouty-related protein Spred-1 and phosphoinositol 3-kinase regulatory subunit 2.78 Angiogenesis can be also promoted by miR-210, activated by hypoxia and directly repressing endothelial ligand ephrin A3,79 and by miR-17-92 cluster, which sustains MYC angiogenic properties through repression of connective tissue growth factor and the antiangiogenic adhesive glycoprotein thrombospondin 1,80 also targeted by miR-27b and let-7f.81
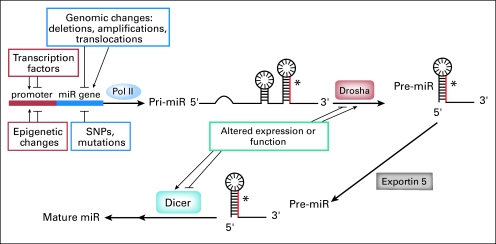
MicroRNA AND EPIGENETICS
MiRNA expression can be altered by several mechanisms in human cancer (Fig 3): chromosomal abnormalities, as suggested by the evidence that microRNAs are frequently located in regions of the genome involved in alterations in cancer,4 and recently confirmed by a genetic study in ovarian carcinoma, breast cancer, and melanoma68; mutations, as the inherited mutations in the primary transcripts of miR-15a and miR-16-1 responsible for reduced expression of the two microRNAs in vitro and in vivo in CLL36; and polymorphisms (SNPs), as described in lung cancer.82 The deregulated microRNA expression in cancer can also be due to defects in the microRNA biogenesis machinery, as supported by the changes in microRNA levels consequent to altered Drosha or Dicer activity in different tumor types,83–86 and epigenetic changes, as altered DNA methylation. An extensive analysis of genomic sequences of miRNA genes have shown that approximately half of them are associated with CpG islands, suggesting that they could be subjected to this mechanism of regulation.87 Several evidences have indeed proved that an altered methylation status can be responsible for the deregulated expression of microRNAs in cancer, as the silencing of putative tumor suppressor microRNAs: treating T24 bladder cancer cells and human fibroblasts with DNMT inhibitor 5-Aza-2′-deoxycytidine, Saito et al88 observed a strong upregulation of miR-127, microRNA characterized by a CpG island promoter, able to target the proto-oncogene BCL-6, and silenced in several cancer cells. With the same approach of unmasking epigenetically silenced microRNAs inducing chromatin-remodeling by drug treatment, it has been demonstrated that miR-9-1 is hypermethylated and consequently downmodulated in breast cancer,89 as well as the clustered miR-34b and miR-34c in colon cancer.90
Fig 3.
Mechanisms of microRNA (miR) regulation. The deregulated microRNA expression observed in cancer can be caused by chromosomal abnormalities, mutations, polymorphisms (SNPs), transcriptional deregulation, defects in the microRNA biogenesis machinery, and epigenetic changes.
Conversely, the upmodulation of putative oncogenic microRNAs in cancer can be due to DNA hypomethylation, as shown in lung adenocarcinoma for let-7a-391 or in epithelial ovarian cancer for miR-21.50
A different approach to identifying epigenetically regulated microRNAs was represented by the microRNA profiling of DNMT1- and DNMT3b-deficient colorectal cancer cells: among the 18 microRNAs upmodulated in comparison with wild-type cells, the only one resulting unmethylated in normal tissue but hypermethylated, and thus silenced, in tumor was miR-124a, embedded in a large CpG island and able to target cyclin D kinase 6, which mediates the phosphorylation of the RB tumor suppressor gene.92
Methylation is not the only epigenetic mechanism that can affect microRNA expression: Scott et al93 showed that in SKBR3 breast carcinoma cells, histone deacetylase inhibition is followed by the extensive and rapid alteration of microRNA levels.
The existence of epigenetic drugs, such as DNA demethylating agents and histone deacetylase inhibitors, able to reverse an aberrant methylation or acetylation status, raises the intriguing possibility of regulating microRNA levels, for example, to restore the expression of tumor suppressor microRNAs, thus reverting a tumoral phenotype.
To complicate the scenario connecting microRNAs and epigenetics, microRNAs themselves can regulate the expression of components of the epigenetic machinery, creating a highly controlled feedback mechanism: the miR-29 family directly targets the de novo DNA methyltransferases DNMT-3A and -3B, although indirectly, through regulation of the transactivator Sp1, the maintenance DNA methyl transferase DNMT1. Interestingly, introduction of miR-29s into lung cancers and AMLs results in reactivation of silenced tumor suppressors and inhibition of tumorigenesis.40,42 Loss of miR-290 cluster in Dicer-deficient mouse embryonic stem cells leads to the downregulation of DNMT3a, DNMT3b, and DNMT1 through upmodulation of their repressor, RBL-2, proven target of miR-29094,95; miR-1, involved in myogenesis and related diseases, directly targets HDAC4.96
MicroRNA/Anti-microRNAs IN CANCER TREATMENT
The evidences collected to date demonstrate how microRNAs could represent valid diagnostic, prognostic, and predictive markers in cancer. Indeed, the aberrant microRNA expression is correlated with specific biopathologic features, disease outcome, and response to specific therapies in different tumor types.
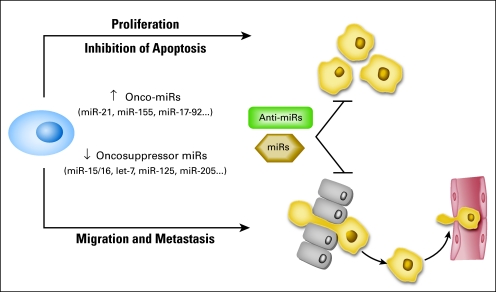
Considering the importance of microRNAs in development, progression, and treatment of cancer, the potential usefulness of a microRNA-based therapy in cancer is now being exploited, with the attempt to modulate their expression, reintroducing microRNAs lost in cancer, or inhibiting oncogenic microRNAs by using anti-microRNA oligonucleotides (Fig 4). For example, transfection of miR-15a/16-1 induces apoptosis in leukemic MEG01 cells and inhibits tumor growth in vivo in a xenograft model,37 whereas the inhibition of miR-21 with antisense oligonucleotides generates a proapoptotic and antiproliferative response in vitro in different cellular models and reduces tumor development and metastatic potential in vivo.97
Fig 4.
MicroRNAs (miRs) as therapeutic tools. The reintroduction by transfection of synthetic miRs lost during cancer development or progression or the inhibition of oncogenic miRs by using anti-miR oligonucleotides could contribute to counteract tumor proliferation, extended survival, and the acquisition of a metastatic potential, thus representing potential therapeutic tools.
Moreover, microRNAs involved in specific networks, as the apoptotic, proliferation, or receptor-driven pathways, could likely influence the response to targeted therapies or to chemotherapy: inhibition of miR-21 and miR-200b enhances sensitivity to gemcitabine in cholangiocytes, probably by modulation of CLOCK, PTEN, and PTPN12,98 whereas reintroduction of miR-205 in breast cancer cells can improve the responsiveness to tyrosine kinase inhibitors through HER-3 silencing.22
Beside targeted therapies and chemotherapy, microRNAs could also alter the sensitivity to radiotherapy, as recently reported by Slack et al99: in lung cancer cells, the let-7 family of microRNAs can suppress the resistance to anticancer radiation therapy, probably through RAS regulation.
Evidence described to date represents the experimental bases for the use of microRNAs as both targets and tools in anticancer therapy, but there are at least two primary issues to address to translate these fundamental research advances into medical practice: the development of engineered animal models to study cancer-associated microRNAs and the improvement of the efficiency of miRNAs/anti-microRNAs delivery in vivo. To this aim, modified microRNA molecules with longer half-lives and efficiency have been developed, such as anti-microRNA oligonucleotides,100 locked nucleic acid–modified oligonucleotides,101 and cholesterol-conjugated antagomirs.102 Interestingly, Ebert et al103 have recently described a new approach to inhibit microRNAs function: synthetic mRNAs containing multiple binding site for a specific microRNA, called microRNA sponges, are able to bind up the microRNA, preventing its association with endogenous targets.
To improve the in vivo delivery of either microRNAs or anti-microRNAs, the methods that have been tested in preclinical studies over the last decades for short-interfering RNAs (siRNA) or short heteroduplex RNA (shRNA)104 could be applied also to microRNAs. Moreover, the advantage of microRNAs over siRNA/shRNA is their ability to affect multiple targets with a single hit, thus regulating a whole network of interacting molecules.
In conclusion, 15 years ago, when microRNAs seemed just a peculiar discovery in C elegans, the scientific world probably did not even imagine that those small noncoding molecules would have a large impact on our understanding of cellular biology and gene regulation.
MicroRNAs contribute to maintaining the balance among genes regulating cells' fate, and their deregulation, a frequent hallmark in different human malignancies, can destabilize this equilibrium, thus contributing to cancer development and/or progression, from initiation to metastatic disease. However, despite the increasing and encouraging evidences linking microRNAs to cancer biology, many important questions remain to be addressed; in fact, although the identification and validation of microRNA targets greatly improved in the last few years, we still know very little about the cellular and molecular circuits where they are involved. The scenario is surely complicated by the ability of microRNAs to target multiple molecules, sometimes belonging to related pathways, and at the same time by the redundancy existing among microRNAs. This gives rise to a complex regulatory network in which biologic effects and properties of a particular microRNA do not always allow a linear explanation.
Improvement of computation programs of microRNA target prediction and experimental methods of validation will certainly contribute to elucidating their mechanisms of action, and genetically modified murine models will likely help in determining the oncogenic and tumor suppressor potential of individual microRNAs.
Data available to date clearly support the involvement of microRNA in cancer etiology and strongly suggest a possible use of these molecules as markers of diagnosis and prognosis and, eventually, as new targets or tools for a specific therapy. Stepping from the bench to clinical applications would be the next great challenge in cancer research.
Footnotes
Supported by grants from the National Cancer Institute (C.M.C.), and a My First AIRC Grant from Associazione Italiana per la Ricerca sul Cancro (M.V.I.).
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Carlo M. Croce
Manuscript writing: Marilena V. Iorio, Carlo M. Croce
Final approval of manuscript: Carlo M. Croce
REFERENCES
- 1.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-y. [DOI] [PubMed] [Google Scholar]
- 2.Bartel DP. MicroRNAs: Genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/s0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 3.Calin GA, Dumitru CD, Shimizu M, et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci U S A. 2002;99:15524–15529. doi: 10.1073/pnas.242606799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calin GA, Sevignani C, Dumitru CD, et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc Natl Acad Sci U S A. 2004;101:2999–3004. doi: 10.1073/pnas.0307323101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pekarsky Y, Santanam U, Cimmino A, et al. Tcl1 expression in chronic lymphocytic leukemia is regulated by miR-29 and miR-181. Cancer Res. 2006;66:11590–11593. doi: 10.1158/0008-5472.CAN-06-3613. [DOI] [PubMed] [Google Scholar]
- 6.Calin GA, Ferracin M, Cimmino A, et al. A MicroRNA signature associated with prognosis and progression in chronic lymphocytic leukemia. N Engl J Med. 2005;353:1793–1801. doi: 10.1056/NEJMoa050995. [DOI] [PubMed] [Google Scholar]
- 7.Cimmino A, Calin GA, Fabbri M, et al. MiR-15 and miR-16 induce apoptosis by targeting BCL2. Proc Natl Acad Sci U S A. 2005;102:13944–13949. doi: 10.1073/pnas.0506654102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mott JL, Kobayashi S, Bronk SF, et al. Mir-29 regulates Mcl-1 protein expression and apoptosis. Oncogene. 2007;26:6133–6140. doi: 10.1038/sj.onc.1210436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metzler M, Wilda M, Busch K, et al. High expression of precursor microRNA-155/BIC RNA in children with Burkitt lymphoma. Genes Chromosomes Cancer. 2004;39:167–169. doi: 10.1002/gcc.10316. [DOI] [PubMed] [Google Scholar]
- 10.Kluiver J, Poppema S, de JD, et al. BIC and miR-155 are highly expressed in Hodgkin, primary mediastinal and diffuse large B cell lymphomas. J Pathol. 2005;207:243–249. doi: 10.1002/path.1825. [DOI] [PubMed] [Google Scholar]
- 11.Costinean S, Zanesi N, Pekarsky Y, et al. Pre-B cell proliferation and lymphoblastic leukemia/high-grade lymphoma in E(mu)-miR155 transgenic mice. Proc Natl Acad Sci U S A. 2006;103:7024–7029. doi: 10.1073/pnas.0602266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He L, Thomson JM, Hemann MT, et al. A microRNA polycistron as a potential human oncogene. Nature. 2005;435:828–833. doi: 10.1038/nature03552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiao C, Srinivasan L, Calado DP, et al. Lymphoproliferative disease and autoimmunity in mice with increased miR-17-92 expression in lymphocytes. Nat Immunol. 2008;9:405–414. doi: 10.1038/ni1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Donnell KA, Wentzel EA, Zeller KI, et al. C-Myc-regulated microRNAs modulate E2F1 expression. Nature. 2005;435:839–843. doi: 10.1038/nature03677. [DOI] [PubMed] [Google Scholar]
- 15.Petrocca F, Visone R, Onelli MR, et al. E2F1-regulated microRNAs impair TGFbeta-dependent cell-cycle arrest and apoptosis in gastric cancer. Cancer Cell. 2008;13:272–286. doi: 10.1016/j.ccr.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Löffler D, Brocke-Heidrich K, Pfeifer G, et al. Interleukin-6 dependent survival of multiple myeloma cells involves the Stat3-mediated induction of microRNA-21 through a highly conserved enhancer. Blood. 2007;110:1330–1333. doi: 10.1182/blood-2007-03-081133. [DOI] [PubMed] [Google Scholar]
- 17.Pichiorri F, Suh SS, Ladetto M, et al. MicroRNAs regulate critical genes associated with multiple myeloma pathogenesis. Proc Natl Acad Sci U S A. 2008;105:12885–12890. doi: 10.1073/pnas.0806202105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iorio MV, Ferracin M, Liu CG, et al. MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 2005;65:7065–7070. doi: 10.1158/0008-5472.CAN-05-1783. [DOI] [PubMed] [Google Scholar]
- 19.Yan LX, Huang XF, Shao Q, et al. MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis and patient poor prognosis. RNA. 2008;14:2348–2360. doi: 10.1261/rna.1034808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qian B, Katsaros D, Lu L, et al. High miR-21 expression in breast cancer associated with poor disease-free survival in early stage disease and high TGF-beta1. Breast Cancer Res Treat. 2009;117:131–140. doi: 10.1007/s10549-008-0219-7. [DOI] [PubMed] [Google Scholar]
- 21.Scott GK, Goga A, Bhaumik D, et al. Coordinate suppression of ERBB2 and ERBB3 by enforced expression of micro-RNA miR-125a or miR-125b. J Biol Chem. 2007;282:1479–1486. doi: 10.1074/jbc.M609383200. [DOI] [PubMed] [Google Scholar]
- 22.Iorio MV, Casalini P, Piovan C, et al. MicroRNA-205 regulates HER3 in human breast cancer. Cancer Res. 2009;69:2195–2200. doi: 10.1158/0008-5472.CAN-08-2920. [DOI] [PubMed] [Google Scholar]
- 23.Wu H, Zhu S, Mo YY. Suppression of cell growth and invasion by miR-205 in breast cancer. Cell Res. 2009;19:439–448. doi: 10.1038/cr.2009.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma L, Teruya-Feldstein J, Weinberg RA. Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature. 2007;449:682–688. doi: 10.1038/nature06174. [DOI] [PubMed] [Google Scholar]
- 25.Huang Q, Gumireddy K, Schrier M, et al. The microRNAs miR-373 and miR-520c promote tumour invasion and metastasis. Nat Cell Biol. 2008;10:202–210. doi: 10.1038/ncb1681. [DOI] [PubMed] [Google Scholar]
- 26.Gregory PA, Bracken CP, Bert AG, et al. MicroRNAs as regulators of epithelial-mesenchymal transition. Cell Cycle. 2008;7:3112–3118. doi: 10.4161/cc.7.20.6851. [DOI] [PubMed] [Google Scholar]
- 27.Park SM, Gaur AB, Lengyel E, et al. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yanaihara N, Caplen N, Bowman E, et al. Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell. 2006;9:189–198. doi: 10.1016/j.ccr.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 29.Johnson SM, Grosshans H, Shingara J, et al. RAS is regulated by the let-7 microRNA family. Cell. 2005;120:635–647. doi: 10.1016/j.cell.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 30.Mayr C, Hemann MT, Bartel DP. Disrupting the pairing between let-7 and Hmga2 enhances oncogenic transformation. Science. 2007;315:1576–1579. doi: 10.1126/science.1137999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sampson VB, Rong NH, Han J, et al. MicroRNA let-7a down-regulates MYC and reverts MYC-induced growth in Burkitt lymphoma cells. Cancer Res. 2007;67:9762–9770. doi: 10.1158/0008-5472.CAN-07-2462. [DOI] [PubMed] [Google Scholar]
- 32.Yu SL, Chen HY, Chang GC, et al. MicroRNA signature predicts survival and relapse in lung cancer. Cancer Cell. 2008;13:48–57. doi: 10.1016/j.ccr.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 33.Gramantieri L, Ferracin M, Fornari F, et al. Cyclin G1 is a target of miR-122a, a microRNA frequently down-regulated in human hepatocellular carcinoma. Cancer Res. 2007;67:6092–6099. doi: 10.1158/0008-5472.CAN-06-4607. [DOI] [PubMed] [Google Scholar]
- 34.Fornari F, Gramantieri L, Ferracin M, et al. MiR-221 controls CDKN1C/p57 and CDKN1B/p27 expression in human hepatocellular carcinoma. Oncogene. 2008;27:5651–5661. doi: 10.1038/onc.2008.178. [DOI] [PubMed] [Google Scholar]
- 35.He L, He X, Lim LP, et al. A microRNA component of the p53 tumour suppressor network. Nature. 2007;447:1130–1134. doi: 10.1038/nature05939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raveche ES, Salerno E, Scaglione BJ, et al. Abnormal microRNA-16 locus with synteny to human 13q14 linked to CLL in NZB mice. Blood. 2007;109:5079–5086. doi: 10.1182/blood-2007-02-071225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calin GA, Cimmino A, Fabbri M, et al. MiR-15a and miR-16-1 cluster functions in human leukemia. Proc Natl Acad Sci U S A. 2008;105:5166–5171. doi: 10.1073/pnas.0800121105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garzon R, Volinia S, Liu CG, et al. MicroRNA signatures associated with cytogenetics and prognosis in acute myeloid leukemia. Blood. 2008;111:3183–3189. doi: 10.1182/blood-2007-07-098749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Le Beau MM, Albain KS, Larson RA, et al. Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: Further evidence for characteristic abnormalities of chromosomes no. 5 and 7. J Clin Oncol. 1986;4:325–345. doi: 10.1200/JCO.1986.4.3.325. [DOI] [PubMed] [Google Scholar]
- 40.Fabbri M, Garzon R, Cimmino A, et al. MicroRNA-29 family reverts aberrant methylation in lung cancer by targeting DNA methyltransferases 3A and 3B. Proc Natl Acad Sci U S A. 2007;104:15805–15810. doi: 10.1073/pnas.0707628104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang H, Garzon R, Sun H, et al. NF-kappaB-YY1-miR-29 regulatory circuitry in skeletal myogenesis and rhabdomyosarcoma. Cancer Cell. 2008;14:369–381. doi: 10.1016/j.ccr.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garzon R, Liu S, Fabbri M, et al. MicroRNA -29b induces global DNA hypomethylation and tumor suppressor gene re-expression in acute myeloid leukemia by targeting directly DNMT3A and 3B and indirectly DNMT1. Blood. 2009;113:6411–6418. doi: 10.1182/blood-2008-07-170589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tam W, Hughes SH, Hayward WS, et al. Avian bic, a gene isolated from a common retroviral site in avian leukosis virus-induced lymphomas that encodes a noncoding RNA, cooperates with c-myc in lymphomagenesis and erythroleukemogenesis. J Virol. 2002;76:4275–4286. doi: 10.1128/JVI.76.9.4275-4286.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thai TH, Calado DP, Casola S, et al. Regulation of the germinal center response by microRNA-155. Science. 2007;316:604–608. doi: 10.1126/science.1141229. [DOI] [PubMed] [Google Scholar]
- 45.Rodriguez A, Vigorito E, Clare S, et al. Requirement of bic/microRNA-155 for normal immune function. Science. 2007;316:608–611. doi: 10.1126/science.1139253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tili E, Michaille JJ, Cimino A, et al. Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J Immunol. 2007;179:5082–5089. doi: 10.4049/jimmunol.179.8.5082. [DOI] [PubMed] [Google Scholar]
- 47.Ronchetti D, Lionetti M, Mosca L, et al. An integrative genomic approach reveals coordinated expression of intronic miR-335, miR-342, and miR-561 with deregulated host genes in multiple myeloma. BMC Med Genomics. 2008;1:37. doi: 10.1186/1755-8794-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chan JA, Krichevsky AM, Kosik KS. MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res. 2005;65:6029–6033. doi: 10.1158/0008-5472.CAN-05-0137. [DOI] [PubMed] [Google Scholar]
- 49.Ciafrè SA, Galardi S, Mangiola A, et al. Extensive modulation of a set of microRNAs in primary glioblastoma. Biochem Biophys Res Commun. 2005;334:1351–1358. doi: 10.1016/j.bbrc.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 50.Iorio MV, Visone R, Di LG, et al. MicroRNA signatures in human ovarian cancer. Cancer Res. 2007;67:8699–8707. doi: 10.1158/0008-5472.CAN-07-1936. [DOI] [PubMed] [Google Scholar]
- 51.Markou A, Tsaroucha EG, Kaklamanis L, et al. Prognostic value of mature microRNA-21 and microRNA-205 overexpression in non-small cell lung cancer by quantitative real-time RT-PCR. Clin Chem. 2008;54:1696–1704. doi: 10.1373/clinchem.2007.101741. [DOI] [PubMed] [Google Scholar]
- 52.Volinia S, Calin GA, Liu CG, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci U S A. 2006;103:2257–2261. doi: 10.1073/pnas.0510565103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schetter AJ, Leung SY, Sohn JJ, et al. MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. JAMA. 2008;299:425–436. doi: 10.1001/jama.299.4.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roldo C, Missiaglia E, Hagan JP, et al. MicroRNA expression abnormalities in pancreatic endocrine and acinar tumors are associated with distinctive pathologic features and clinical behavior. J Clin Oncol. 2006;24:4677–4684. doi: 10.1200/JCO.2005.05.5194. [DOI] [PubMed] [Google Scholar]
- 55.Bloomston M, Frankel WL, Petrocca F, et al. MicroRNA expression patterns to differentiate pancreatic adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA. 2007;297:1901–1908. doi: 10.1001/jama.297.17.1901. [DOI] [PubMed] [Google Scholar]
- 56.Blenkiron C, Goldstein LD, Thorne NP, et al. MicroRNA expression profiling of human breast cancer identifies new markers of tumor subtype. Genome Biol. 2007;8:R214. doi: 10.1186/gb-2007-8-10-r214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miller TE, Ghoshal K, Ramaswamy B, et al. MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J Biol Chem. 2008;283:29897–29903. doi: 10.1074/jbc.M804612200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhao JJ, Lin J, Yang H, et al. MicroRNA-221/222 negatively regulates estrogen receptor alpha and is associated with tamoxifen resistance in breast cancer. J Biol Chem. 2008;283:31079–31086. doi: 10.1074/jbc.M806041200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 58a.Di Leva G, Gasparini P, Piovan C. A regulatory “miRcircuitry” involving miR-221&222 and ERα determines ERα status of breast cancer cells. J Natl Cancer Inst. in press. [Google Scholar]
- 59.Yu F, Yao H, Zhu P, et al. Let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell. 2007;131:1109–1123. doi: 10.1016/j.cell.2007.10.054. [DOI] [PubMed] [Google Scholar]
- 60.Kumar MS, Erkeland SJ, Pester RE, et al. Suppression of non-small cell lung tumor development by the let-7 microRNA family. Proc Natl Acad Sci U S A. 2008;105:3903–3908. doi: 10.1073/pnas.0712321105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lebanony D, Benjamin H, Gilad S, et al. Diagnostic assay based on hsa-miR-205 expression distinguishes squamous from nonsquamous non–small-cell lung carcinoma. J Clin Oncol. 2009;27:2030–2037. doi: 10.1200/JCO.2008.19.4134. [DOI] [PubMed] [Google Scholar]
- 62.Murakami Y, Yasuda T, Saigo K, et al. Comprehensive analysis of microRNA expression patterns in hepatocellular carcinoma and non-tumorous tissues. Oncogene. 2006;25:2537–2545. doi: 10.1038/sj.onc.1209283. [DOI] [PubMed] [Google Scholar]
- 63.Li W, Xie L, He X, et al. Diagnostic and prognostic implications of microRNAs in human hepatocellular carcinoma. Int J Cancer. 2008;123:1616–1622. doi: 10.1002/ijc.23693. [DOI] [PubMed] [Google Scholar]
- 64.Visone R, Pallante P, Vecchione A, et al. Specific microRNAs are downregulated in human thyroid anaplastic carcinomas. Oncogene. 2007;26:7590–7595. doi: 10.1038/sj.onc.1210564. [DOI] [PubMed] [Google Scholar]
- 65.le Sage C, Nagel R, Egan DA, et al. Regulation of the p27(Kip1) tumor suppressor by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J. 2007;26:3699–3708. doi: 10.1038/sj.emboj.7601790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galardi S, Mercatelli N, Giorda E, et al. MiR-221 and miR-222 expression affects the proliferation potential of human prostate carcinoma cell lines by targeting p27Kip1. J Biol Chem. 2007;282:23716–23724. doi: 10.1074/jbc.M701805200. [DOI] [PubMed] [Google Scholar]
- 67.Felicetti F, Errico MC, Bottero L, et al. The promyelocytic leukemia zinc finger-microRNA-221/-222 pathway controls melanoma progression through multiple oncogenic mechanisms. Cancer Res. 2008;68:2745–2754. doi: 10.1158/0008-5472.CAN-07-2538. [DOI] [PubMed] [Google Scholar]
- 68.Zhang L, Huang J, Yang N, et al. MicroRNAs exhibit high frequency genomic alterations in human cancer. Proc Natl Acad Sci U S A. 2006;103:9136–9141. doi: 10.1073/pnas.0508889103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li N, Fu H, Tie Y, et al. MiR-34a inhibits migration and invasion by down-regulation of c-Met expression in human hepatocellular carcinoma cells. Cancer Lett. 2009;275:44–53. doi: 10.1016/j.canlet.2008.09.035. [DOI] [PubMed] [Google Scholar]
- 70.Gandellini P, Folini M, Longoni N, et al. MiR-205 Exerts tumor-suppressive functions in human prostate through down-regulation of protein kinase Cepsilon. Cancer Res. 2009;69:2287–2295. doi: 10.1158/0008-5472.CAN-08-2894. [DOI] [PubMed] [Google Scholar]
- 71.Asangani IA, Rasheed SA, Nikolova DA, et al. MicroRNA-21 (miR-21) post-transcriptionally downregulates tumor suppressor Pdcd4 and stimulates invasion, intravasation and metastasis in colorectal cancer. Oncogene. 2008;27:2128–2136. doi: 10.1038/sj.onc.1210856. [DOI] [PubMed] [Google Scholar]
- 72.Zhu S, Wu H, Wu F, et al. MicroRNA-21 targets tumor suppressor genes in invasion and metastasis. Cell Res. 2008;18:350–359. doi: 10.1038/cr.2008.24. [DOI] [PubMed] [Google Scholar]
- 73.Tavazoie SF, Alarcon C, Oskarsson T, et al. Endogenous human microRNAs that suppress breast cancer metastasis. Nature. 2008;451:147–152. doi: 10.1038/nature06487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rosenfeld N, Aharonov R, Meiri E, et al. MicroRNAs accurately identify cancer tissue origin. Nat Biotechnol. 2008;26:462–469. doi: 10.1038/nbt1392. [DOI] [PubMed] [Google Scholar]
- 75.Poliseno L, Tuccoli A, Mariani L, et al. MicroRNAs modulate the angiogenic properties of HUVECs. Blood. 2006;108:3068–3071. doi: 10.1182/blood-2006-01-012369. [DOI] [PubMed] [Google Scholar]
- 76.Hua Z, Lv Q, Ye W, et al. MiRNA-directed regulation of VEGF and other angiogenic factors under hypoxia. PLoS One. 2006;1:e116. doi: 10.1371/journal.pone.0000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mertens-Talcott SU, Chintharlapalli S, Li X, et al. The oncogenic microRNA-27a targets genes that regulate specificity protein transcription factors and the G2-M checkpoint in MDA-MB-231 breast cancer cells. Cancer Res. 2007;67:11001–11011. doi: 10.1158/0008-5472.CAN-07-2416. [DOI] [PubMed] [Google Scholar]
- 78.Fish JE, Santoro MM, Morton SU, et al. MiR-126 regulates angiogenic signaling and vascular integrity. Dev Cell. 2008;15:272–284. doi: 10.1016/j.devcel.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pulkkinen K, Malm T, Turunen M, et al. Hypoxia induces miR-210 in vitro and in vivo ephrin-A3 and neuronal pentraxin 1 are potentially regulated by miR-210. FEBS Lett. 2008;582:2397–2401. doi: 10.1016/j.febslet.2008.05.048. [DOI] [PubMed] [Google Scholar]
- 80.Dews M, Homayouni A, Yu D, et al. Augmentation of tumor angiogenesis by a Myc-activated microRNA cluster. Nat Genet. 2006;38:1060–1065. doi: 10.1038/ng1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuehbacher A, Urbich C, Zeiher AM, et al. Role of Dicer and Drosha for endothelial microRNA expression and angiogenesis. Circ Res. 2007;101:59–68. doi: 10.1161/CIRCRESAHA.107.153916. [DOI] [PubMed] [Google Scholar]
- 82.Hu Z, Chen J, Tian T, et al. Genetic variants of miRNA sequences and non-small cell lung cancer survival. J Clin Invest. 2008;118:2600–2608. doi: 10.1172/JCI34934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thomson JM, Newman M, Parker JS, et al. Extensive post-transcriptional regulation of microRNAs and its implications for cancer. Genes Dev. 2006;20:2202–2207. doi: 10.1101/gad.1444406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nakamura T, Canaani E, Croce CM. Oncogenic All1 fusion proteins target Drosha-mediated microRNA processing. Proc Natl Acad Sci U S A. 2007;104:10980–10985. doi: 10.1073/pnas.0704559104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Karube Y, Tanaka H, Osada H, et al. Reduced expression of Dicer associated with poor prognosis in lung cancer patients. Cancer Sci. 2005;96:111–115. doi: 10.1111/j.1349-7006.2005.00015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Merritt WM, Lin YG, Han LY, et al. Dicer, Drosha, and outcomes in patients with ovarian cancer. N Engl J Med. 2008;359:2641–2650. doi: 10.1056/NEJMoa0803785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Weber B, Stresemann C, Brueckner B, et al. Methylation of human microRNA genes in normal and neoplastic cells. Cell Cycle. 2007;6:1001–1005. doi: 10.4161/cc.6.9.4209. [DOI] [PubMed] [Google Scholar]
- 88.Saito Y, Liang G, Egger G, et al. Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatin-modifying drugs in human cancer cells. Cancer Cell. 2006;9:435–443. doi: 10.1016/j.ccr.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 89.Lehmann U, Hasemeier B, Christgen M, et al. Epigenetic inactivation of microRNA gene hsa-mir-9-1 in human breast cancer. J Pathol. 2008;214:17–24. doi: 10.1002/path.2251. [DOI] [PubMed] [Google Scholar]
- 90.Toyota M, Suzuki H, Sasaki Y, et al. Epigenetic silencing of microRNA-34b/c and B-cell translocation gene 4 is associated with CpG island methylation in colorectal cancer. Cancer Res. 2008;68:4123–4132. doi: 10.1158/0008-5472.CAN-08-0325. [DOI] [PubMed] [Google Scholar]
- 91.Brueckner B, Stresemann C, Kuner R, et al. The human let-7a-3 locus contains an epigenetically regulated microRNA gene with oncogenic function. Cancer Res. 2007;67:1419–1423. doi: 10.1158/0008-5472.CAN-06-4074. [DOI] [PubMed] [Google Scholar]
- 92.Lujambio A, Ropero S, Ballestar E, et al. Genetic unmasking of an epigenetically silenced microRNA in human cancer cells. Cancer Res. 2007;67:1424–1429. doi: 10.1158/0008-5472.CAN-06-4218. [DOI] [PubMed] [Google Scholar]
- 93.Scott GK, Mattie MD, Berger CE, et al. Rapid alteration of microRNA levels by histone deacetylase inhibition. Cancer Res. 2006;66:1277–1281. doi: 10.1158/0008-5472.CAN-05-3632. [DOI] [PubMed] [Google Scholar]
- 94.Benetti R, Gonzalo S, Jaco I, et al. A mammalian microRNA cluster controls DNA methylation and telomere recombination via Rbl2-dependent regulation of DNA methyltransferases. Nat Struct Mol Biol. 2008;15:268–279. doi: 10.1038/nsmb.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sinkkonen L, Hugenschmidt T, Berninger P, et al. MicroRNAs control de novo DNA methylation through regulation of transcriptional repressors in mouse embryonic stem cells. Nat Struct Mol Biol. 2008;15:259–267. doi: 10.1038/nsmb.1391. [DOI] [PubMed] [Google Scholar]
- 96.Chen JF, Mandel EM, Thomson JM, et al. The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat Genet. 2006;38:228–233. doi: 10.1038/ng1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Si ML, Zhu S, Wu H, et al. MiR-21-mediated tumor growth. Oncogene. 2007;26:2799–2803. doi: 10.1038/sj.onc.1210083. [DOI] [PubMed] [Google Scholar]
- 98.Meng F, Henson R, Lang M, et al. Involvement of human micro-RNA in growth and response to chemotherapy in human cholangiocarcinoma cell lines. Gastroenterology. 2006;130:2113–2129. doi: 10.1053/j.gastro.2006.02.057. [DOI] [PubMed] [Google Scholar]
- 99.Weidhaas JB, Babar I, Nallur SM, et al. MicroRNAs as potential agents to alter resistance to cytotoxic anticancer therapy. Cancer Res. 2007;67:11111–11116. doi: 10.1158/0008-5472.CAN-07-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Weiler J, Hunziker J, Hall J. Anti-miRNA oligonucleotides (AMOs): Ammunition to target miRNAs implicated in human disease? Gene Ther. 2006;13:496–502. doi: 10.1038/sj.gt.3302654. [DOI] [PubMed] [Google Scholar]
- 101.Ørom UA, Kauppinen S, Lund AH. LNA-modified oligonucleotides mediate specific inhibition of microRNA function. Gene. 2006;372:137–141. doi: 10.1016/j.gene.2005.12.031. [DOI] [PubMed] [Google Scholar]
- 102.Krützfeldt J, Rajewsky N, Braich R, et al. Silencing of microRNAs in vivo with ‘antagomirs’. Nature. 2005;438:685–689. doi: 10.1038/nature04303. [DOI] [PubMed] [Google Scholar]
- 103.Ebert MS, Neilson JR, Sharp PA. MicroRNA sponges: Competitive inhibitors of small RNAs in mammalian cells. Nat Methods. 2007;4:721–726. doi: 10.1038/nmeth1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dykxhoorn DM, Palliser D, Lieberman J. The silent treatment: SiRNAs as small molecule drugs. Gene Ther. 2006;13:541–552. doi: 10.1038/sj.gt.3302703. [DOI] [PubMed] [Google Scholar]