Abstract
Background: Little is known about the effectiveness of behavioral strategies to prevent long-term weight gain among adolescents and young adults.
Objective: The objective was to assess the relation of dietary and physical activity weight-control strategies, alone and together, with subsequent weight change.
Design: This was a prospective study of 4456 female adolescents and young adults aged 14–22 y in the ongoing Growing Up Today Study. Weight-control behaviors, including dietary approaches and physical activity, were self-reported in 2001 and were used to predict weight change from 2001 to 2005.
Results: In 2001–2002, 23.7% of female adolescents and young adults were trying to maintain their weight and another 54.4% were trying to lose weight. Approximately 25% used each of the following weight-control strategies: not eating snacks, following low-calorie or low-fat diets, and limiting portion sizes. In addition, 47.7% reported exercising at least occasionally for weight control. During 4 y of follow-up, participants gained an average of 3.3 kg. None of the dietary approaches to weight control predicted less weight change; however, females who exercised ≥5 d/wk gained significantly less weight than did their peers (−0.9 kg; 95% CI: −1.4, −0.4). The most successful strategy for weight-gain prevention among the females was to limit portion sizes (−1.9 kg; 95% CI: −2.6, −1.1) combined with frequent exercise.
Conclusions: Our results suggest that physical activity is a necessary strategy for long-term weight control among adolescents and young adult females. Combining dietary weight-control approaches with physical activity is the most effective method for reducing weight gain.
INTRODUCTION
Although weight tends to increase with age from young adulthood through middle age (1), the prevalence of trying to lose weight is high among adolescent and adult females (2). For example, among high school students throughout the United States, Lowry et al (3; 2005) observed that 62% of females and 29% of males were trying to lose weight. In the 2001–2002 National Health and Nutrition Examination Survey (NHANES), 53% of female and 32% of male adults ≥20–29 y of age and 57% of women and 39% of men 50–59 y of age had tried to lose weight in the past year (4). Many approaches are used to lose or maintain weight, but little is known about how effective they are in free-living populations. Most studies have found that eating fewer calories or less fat and exercising are the most common weight-loss methods used (4, 5). However, a minority of people combine reducing calories with regularly engaging in physical activity (2, 4).
In several studies, dieting to lose weight has been found to predict greater weight gain (6–9); however, none of these studies have examined whether all types of self-reported diets or dietary weight-oss strategies were predictive of weight gain. Some dietary and behavioral approaches, such as increased exercise (10, 11), have been observed to promote weight loss, but because many weight-control attempts are of short duration (12), it is unknown which strategies promote prevention of weight gain over the long term.
The aim of the present study was to investigate the association of specific weight-control strategies to subsequent weight change during adolescence and young adulthood among 4480 females in the Growing Up Today Study (GUTS).
SUBJECTS AND METHODS
The GUTS was established in 1996 by recruiting children of women participating in the Nurses' Health Study II (NHS II). The NHS II was established in 1989 and consists of 116,608 female nurses aged 25–43 y at entry. Follow-up questionnaires have been sent to participants biennially since 1989. Using the NHS II data, we identified mothers who had children aged 9–14 y. We wrote a detailed letter to the mothers explaining the purpose of GUTS and seeking parental consent to enroll their children. Children whose mothers gave us consent to invite them to participate were mailed an invitation letter and a questionnaire. Additional details were reported previously (13). Approximately 68% of the females (n = 9039) and 58% of the males (n = 7843) returned completed questionnaires, thereby assenting to participate in the cohort. The participants have been sent questionnaires every 12–24 mo. The study was approved by the Human Subjects Committee at Brigham and Women's Hospital, and the analyses presented in this manuscript were approved by the Institutional Review Boards at Brigham and Women's Hospital and Children’s Hospital Boston.
Sample
The analysis was limited to the 6273 females who completed the 2001 questionnaire, which contained questions on weight-control behaviors. Because few males engaged in both regular exercise and dietary strategies to control their weight (n = 37–57 depending on the dietary strategy), the males were excluded from the analysis. Female participants were excluded from the analysis if they did not complete the 2005 questionnaire (n = 811); only completed the abbreviated version of the 2001 questionnaire (n = 962), which did not contain questions on weight-control behaviors; or who skipped the weight-control questions on the longer version of the questionnaire (n = 20), which left 4480 females for analyses. Participants who did not complete the 2005 questionnaire, and therefore were excluded from the analysis, were similar to their peers who completed the questionnaire in terms of the prevalence of overweight or obesity (P = 0.8).
Questionnaires completed by GUTS participants
In the fall of 1996 through 2005, the GUTS participants received a questionnaire every 12–24 mo that assessed a variety of factors. Self-reported weight and height were assessed on all questionnaires. Body mass index [BMI; weight (kg)/height2 (m)] was calculated by using self-reported weight and height. Children were classified as overweight or obese based on the International Obesity Task Force cutoffs (14), which are age- and sex-specific and provide comparability in assessing overweight and obesity from adolescence to adulthood.
Weight-control behaviors were assessed with questions adapted from the Youth Risk Behavior Surveillance System questionnaire (15). Exercising to control weight was assessed with the question, “During the past year, did you exercise to lose weight or keep from gaining weight?” Dieting was assessed with the question: “During the past year, did you go on a diet to lose weight or to keep from gaining weight?” In 2001, a detailed assessment of dieting was included. Participants were asked the duration of their diets, whether they lost weight on the diets, whether they regained weight lost on the diets, and the types of diets used (eg, low-calorie, low-fat, high-protein, and high-carbohydrate diets; diets devoid of snacks or desserts; meal skipping; limitations of portion sizes; weight-loss shakes; and Weight Watchers and other programs).
Maladaptive weight-control behaviors were assessed with 3 questions, which were based on the Youth Risk Behavior Surveillance System questionnaire (15). Participants were asked whether they had made themselves vomit, used laxatives, or fasted to lose weight or keep from gaining weight during the past year. Binge eating was assessed with a 2-part question. Participants were asked about the frequency during the past year of eating a very large amount of food. Adolescents who reported at least occasional episodes of overeating were asked whether they felt out of control during these episodes such that they could not stop eating even if they wanted to stop. Binge eating was defined as engaging in eating a very large amount of food in a short amount of time and feeling out of control during the eating episode. Both the binge eating and the questions on self-induced vomiting and laxative use have been validated in the GUTS cohort (16).
Physical activity was assessed with 18 questions on hours per week within each of the 4 seasons that a participant engaged in a specific activity (eg, volleyball and soccer). A summary score of average hours per week of physical activity was computed. Reports of an average of >40 h/wk were considered implausible and therefore set to missing and not used in the analysis. Inactivity was estimated by asking participants the average number of hours per week spent “watching TV,” “watching videos or VCR,” “reading/homework,” or “playing Nintendo/Sega/computer games (not homework).” Reports of an average of >80 h/wk of inactivity were considered implausible and therefore set to missing and not used in the analysis.
Reliability and validity of self-reported weight change
Although self-reported BMI, weight change, and BMI change have been used to predict the development of numerous chronic diseases (17–22), there has been some concern that self-reports are biased estimates of true weight and height, and, as a result, self-reported weight and BMI underestimate their true values. The validity of self-reported weight and height have been investigated in both adult populations (23, 24) and adolescent and young adult populations (25, 26), and the results support the use of self-report in epidemiologic studies of associations with weight and BMI. However, there is some evidence of a slight underestimation of the prevalence of overweight and obesity (25).
The validity of weight change based on serial self-reported measures of weight has been assessed by Field et al (27) using data from 1671 females and 1613 males in the National Longitudinal Study of Adolescent Health, a prospective study that has both measured and self-reported weights and heights at 2 time points ≈5 y apart. They observed that both males and females slightly underreported their weights, but they were quite consistent in their underreporting. As a result, weight change based on self-reported weights at Wave II and III underestimated weight change based on measured weights by only an average of 2.1 (females) to 2.6 (males) lb (1 lb = 0.45 kg). The study provided strong evidence that the use of repeated self-reported weights to estimate weight change is a valid approach for investigating weight change in epidemiologic studies.
Outcome measure
The outcome was weight change from 2001 to 2005. Weight change was modeled as weight reported on the 2001 questionnaire as a predictor and weight reported on the 2005 questionnaire as the outcome. Using Rosner’s outlier procedure (28), we identified 24 females as weight-change outliers and therefore excluded them from the analysis.
Statistics
All analyses were conducted with SAS software (SAS version 9.1; SAS Institute, Cary, NC). Because there are siblings within the data set, ordinary least-squares regression would not be appropriate. Therefore, we used SAS PROC MIXED with the repeated statement for all multivariate analyses. All models controlled for age, time spent watching television in 2001, recent weight change (2000–2001), and height change from 2001 to 2005. Effect modification by age (14–18.9 y compared with 19–21 y) and weight status (healthy weight compared with overweight or obese) were explored by including interaction terms and running stratified models.
RESULTS
In 2001–2002, the participants were 14–22 y of age; 23.7% were trying to maintain their weight and another 54.3% were trying to lose weight. Slightly more than half of the females reported that they had been on a diet at least once in the past year. Not eating snacks or desserts was the most popular dietary weight-loss strategy, followed by low-fat diets, low-calorie diets, and limiting portion sizes (Table 1). In addition to making dietary changes, many adolescents and young adult females reported that they exercised at least occasionally for weight control: 48% reported exercising at least weekly, and 14% reported exercising on ≥5 d/wk. Approximately 31% engaged in both dietary changes and at least weekly physical activity to control their weight. The combination approach was most common (48.6%) among females who were trying to lose weight. Among girls who reported using dietary approaches to control weight, 22% (no snacks or desserts) to 25.2% (low-calorie diets) reported exercising on ≥5 d/wk to control their weight.
TABLE 1.
Demographics and prevalence of weight-control strategies in 2001 among 4456 female adolescents and young adults in the Growing Up Today Study
| Value | |
| Age (y) | 17.6 ± 1.61 |
| BMI (kg/m2) | 22.1 ± 3.4 |
| Weight status (%) | |
| Overweight | 13.80 |
| Obese | 4.2 |
| Weight-change efforts (%) | |
| Trying to maintain | 23.7 |
| Trying to lose | 54.3 |
| Dietary weight-control strategies (%) | |
| Low-calorie diet | 24.7 |
| Low-fat diet | 25.2 |
| No snacks or desserts (%) | 32.5 |
| Limited portion sizes (%) | 23.1 |
| Skip meals (%) | 19.9 |
| Weight-loss shakes (%) | 7.8 |
| Commercial program (%) | 6.4 |
| Exercised to control weight (%) | |
| 1–4 d/wk | 33.7 |
| ≥5 d/wk | 14.0 |
Mean ± SD (all such values).
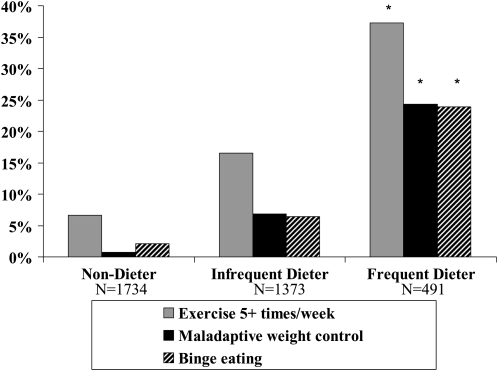
The prevalence of exercising on ≥5 d/wk increased with frequency of dieting. However, the use of maladaptive weight-control behaviors (self-inducted vomiting, use of laxatives, and fasting) and binge eating also increased with dieting frequency (Figure 1). Among frequent dieters, 37% exercised ≥5 times/wk, 24% engaged in binge eating, and 24% in maladaptive weight-control behaviors.
FIGURE 1.
Prevalence of weight-control behaviors and binge eating among dieting and nondieting adolescent and young adult females in the Growing Up Today Study. *P < 0.001.
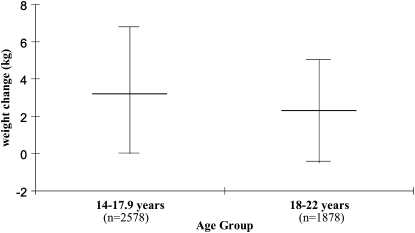
During 4 y of follow-up, the females gained an average of 3.3 kg. Twenty-five percent gained no weight, and 25% gained ≥6.4 kg. Weight change was greater among the 14–17.9-y-old participants (3.8 ± 5.7 kg) than among those who were ≥18 y (2.6 ± 5.7 kg) (Figure 2). Moreover, frequency of dieting to control weight was predictive of gaining more weight (data not shown). However, none of the dietary weight-control strategies was significantly associated with subsequent weight change. In contrast, exercise to control weight was predictive of less weight gain. Females who engaged in exercise ≥5 times/wk to control their weight gained 0.9 kg less than their less active peers.
FIGURE 2.
Distribution (25th, 50th, and 75th percentiles) of weight change over 4 y among adolescent and young adult females in the Growing Up Today Study. Middle bar indicates the median weight change, the upper bound equals the 75th percentile, and the lower bound equals the 25th percentile of weight change over 4 y.
The most successful strategies for weight gain prevention were to combine certain dietary strategies with frequent exercise. Females who combined a low-fat diet with exercising at least once a week to control weight gained ≈0.5 kg less than their peers over 4 y, whereas those who combined following a low-fat diet with exercising ≥5 times/wk to control weight gained ≈1.5 kg less (Table 2). The combination of limiting portion sizes with frequent exercise had the strongest protective effect against weight gain. Females who limited portion sizes and exercised ≥5 times/wk to control weight gained ≈1.9 kg less than their peers.
TABLE 2.
Association of dietary approaches to weight control with subsequent weight change among adolescents and young adult females in the Growing Up Today Study (2001–2005)1
| All females | Combined with exercising more than weekly | Combined with exercising ≥5 times/wk | |
| Low-calorie diet | −0.1 (−0.5, 0.4) | −0.3 (−0.9, 0.2) | −1.4 (−2.1, −0.7) |
| Low-fat diet | −0.4 (−0.8, 0.0) | −0.5 (−1.0, 0.0) | −1.5 (−2.3, −0.8) |
| No snacks or desserts | −0.1 (−0.5, 0.2) | −0.3 (−0.8, 0.2) | −1.1 (−1.8, −0.5) |
| Limited portion sizes | −0.3 (−0.7, 0.2) | −0.5 (−1.1, −0.0) | −1.9 (−2.6, −1.1) |
| Skip meals | −0.0 (−0.5, 0.5) | −0.3 (−0.9, 0.3) | −1.0 (−2.0, −0.1) |
| Exercise ≥1 time/wk | −0.2 (−0.6, 0.1) | ||
| Exercise ≥5 times/wk | −0.9 (−1.4, −0.4) |
The average weight change (converted from pounds to kilograms by dividing by 2.2) was measured in kilograms over 4 y, and the 95% CI (in parentheses) was obtained from mixed models that controlled for age, previous weight change, height change, and television time.
Many females engaged in multiple dietary strategies to lose or maintain weight. For example, among females who exercised ≥5 times/wk and followed a low-fat diet, 62% limited portion sizes and 76% eliminated snacks and desserts. When multiple approaches to weight control were included in the same model, only the combination of limiting portion sizes and exercising frequently remained significantly protective against weight gain. For example, when exercising daily and eating a low-fat diet are included in the same modeling as exercising daily and limiting portion sizes and exercising daily and eating a low-calorie diet, only exercising and limiting portion sizes appeared to be significantly protective against weight change over the 4 y (−1.3 kg; 95% CI: −2.3, −0.3).
All of the associations were strongest among 18–22-y-old women. For example, among the 14–17.9-y-old females, combining limiting portion sizes with exercising ≥5 times/wk predicted gains of 0.9 kg less over 4 y; whereas, among 18–22-y-old women, this weight-control combination predicted gains of 3.0 kg less over 4 y (Table 3). In addition, in both age groups, there was a suggestion that the associations were strongest among the overweight youth (Table 4); however, the differences were not significant. For example, nonoverweight 18–22-y-old women who combined portion control with exercise ≥5 times/wk gained 2.0 kg less over than their peers over 4 y; whereas, the overweight girls who used those weight-control strategies gained 6.0 kg less than their peers.
TABLE 3.
Age group–specific associations of dietary approaches to weight control with subsequent weight change among 4456 adolescents and young adult females in the Growing Up Today Study (2001–2005)1
| 14–17.9 y (n = 2578) |
18–22 y (n = 1878) |
|||
| Combined with exercising more than weekly | Combined with exercising ≥5 times/wk | Combined with exercising more than weekly | Combined with exercising ≥5 times/wk | |
| Low-calorie diet | −0.0 (−0.8, 0.7) | −0.7 (−1.8, 0.3) | −0.5 (−1.3, 0.2) | −2.1 (−3.1, −1.1) |
| Low-fat diet | −0.3 (−1.0, 0.4) | −0.8 (−1.8, 0.2) | −0.6 (−1.4, 0.1) | −2.4 (−3.5, −1.3) |
| No snacks or desserts | −0.0 (−0.7, 0.6) | −0.3 (−1.2, 0.6) | −0.5 (−1.2, 0.2) | −2.22 (−3.3, −1.2) |
| Limited portion sizes | −0.6 (−1.4, 0.1) | −0.9 (−1.9, −0.1) | −0.4 (−1.2, 0.4) | −3.03 (−4.2, −1.9) |
| Skip meals | −0.2 (−1.0, 0.6) | −0.5 (−1.7, 0.7) | −0.4 (−1.2, 0.5) | −2.1 (−3.6, −0.6) |
The average weight change (converted from pounds to kilograms by dividing by 2.2) was measured in kilograms over 4 y, and the 95% CI (in parentheses) was obtained from mixed models that controlled for age, previous weight change, height change, and television time.
P < 0.05 for interaction by age group.
P< 0.01 for interaction by age group.
TABLE 4.
Age and weight status group–specific associations of dietary approaches to weight control with subsequent weight change among 4456 adolescent and young adult females in the Growing Up Today Study (2001–2005)1
| 14–17.9 y (n = 2578) |
18–22 y (n = 1878) |
|||||||
| Combined with exercising more than weekly |
Combined with exercising ≥5 times/wk |
Combined with exercising more than weekly |
Combined with exercising ≥5 times/wk |
|||||
| Not overweight | Overweight | Not overweight | Overweight | Not overweight | Overweight | Not overweight | Overweight | |
| Low-calorie diet | −0.1 (−0.9, 0.6) | −0.5 (−1.7, 2.7) | −0.5 (−1.6, 0.6) | −2.0 (−4.9, 0.8) | −0.2 (−1.0, 0.3) | −0.3 (−2.9, 2.4) | −1.7 (−2.6, −0.8) | −3.0 (−6.3, −0.13) |
| Low-fat diet | −0.4 (−1.0, 0.3) | −0.3 (−1.9, 2.5) | −0.6 (−1.6, 0.4) | −1.8 (−4.5, 0.9) | −0.3 (−1.0, 0.4) | −1.7 (−4.3, 1.0) | −1.8 (−2.8, −0.9) | −4.3 (−7.8, −0.8) |
| No snacks or desserts | −0.04 (−0.7, 0.6) | −0.04 (−2.1, 2.0) | −0.1 (−1.0, 0.8) | −1.6 (−4.6, 1.3) | −0.2 (−0.8, 0.5) | −0.9 (−3.6, 1.8) | −1.7 (−2.6, −0.8) | −3.8 (−7.4, −0.3) |
| Limited portion sizes | −0.7 (−1.4, 0.0) | −0.2 (−2.7, 2.2) | −0.4 (−1.6, 0.4) | −2.0 (−4.9, 0.8) | 0.0 (−0.7, 0.7) | −0.5 (−3.2, 2.3) | −2.0 (−3.0, −1.0) | −6.02 (−9.6, −2.5) |
| Skip meals | −0.2 (−1.0, 0.5) | −0.1 (−2.7, 2.5) | −0.2 (−1.5, 1.0) | −1.5 (−6.2, 3.1) | −0.4 (−1.1, 0.4) | 0.6 (−2.4, 3.6) | −1.9 (−3.2, −0.5) | −2.5 (−6.4, 1.5) |
The average weight change (converted from pounds to kilograms by dividing by 2.2) was measured in kilograms over 4 y, and the 95% CI (in parentheses) was obtained from mixed models that controlled for age, previous weight change, height change, and television time.
P = 0.07 for interaction with weight status within age group.
DISCUSSION
We observed that, among 4456 adolescent and young adult females living throughout the United States, 24% were trying to maintain their weight and 54% were trying to lose weight. Despite their attempts to control their weight, females gained an average of 3.3 kg over the 4 y of the study. The rate of weight gain among those who were ≥18 y was similar to that observed among the white participants in the Coronary Artery Risk Development in Young Adults Study. Because we observed relatively little height change among the participants who were ≥18 y of age, it can be assumed that much of the observed weight gain was not related to healthy physical development.
The rates of attempting to lose or maintain weight in 2001 are similar to those reported by Lowry et al (3) in 2005 among high school students. Studies have found that children and adults who diet, which is a subset of those trying to lose or maintain weight, gain more weight than do their peers (6, 8, 10, 29–31). However, those studies did not investigate whether all types of diets are associated with weight gain or whether some dietary strategies are effective, nor did they study how the combination of dietary strategies coupled with regular physical activity, which is the strategy promoted by the National Institutes for Health (32), is related to long-term weight change among young adults. We observed that, on their own, none of the dietary approaches to control weight was protective against weight gain over 4 y. However, among females, portion control or limiting calories, fat, or snacks and sweets coupled with frequent exercise resulted in significantly less weight gain. Because we did not differentiate between weight due to fat mass compared with lean mass, it is possible that we underestimated the beneficial effect of exercise. Exercise could lead to increases in muscle mass, which would make weight changes smaller, whereas, none of the dietary changes would be expected to promote increases in muscle mass. It is also important to note that there is some speculation that behaviors that are associated with dieting, such as binge eating or other overeating episodes (8, 31, 33, 34), are at least partially responsible for the positive associations that have been observed between dieting and weight gain (6, 8, 31). The fact that we observed a strong association between dieting and binge eating and that dieting, but not the individual dietary approaches to weight control, predicted greater weight gain supports this line of speculation.
One limitation of our study is that it does not represent a random sample of all US adolescents and young adults. The participants are children of nurses, and the sample is >90% white; thus, we are unlikely to have children of low socioeconomic status in the sample, so it is unclear whether the results of the study are generalizable to economically disadvantaged populations or to nonwhite ethnic groups. However, there is no reason to believe that modifying dietary intake and engaging in regular physical activity would not benefit nonwhite populations. Although we studied a variety of dietary strategies to control weight, our list was not exhaustive. For example, modification of the energy density of meals, which some, but not all, studies have found effective for preventing weight gain (35–37), was not assessed in the present study. More research is needed to assess whether low-carbohydrate diets, substituting fruit and vegetables for more calorie-dense foods, and other strategies on their own and when coupled with frequent physical activity are effective weight-control strategies for adolescents and young adults. In addition, it is possible that adolescents and young adults who exercise to control their weight are more committed to losing or maintaining their weight and, thus, the associations with exercise may be partially explained by differences in dedication to control weight. Moreover, we used self-reported, not measured, weights to define our outcome. However, we found that weight change based on self-reported weights underestimated weight change based on measured weights by only an average of 1 kg among adolescent and young adult females in the Longitudinal Study of Adolescent Health, which is evidence that the use of repeated self-reported weights to estimate weight change is a valid approach for investigating weight change in epidemiologic studies (27).
Despite these limitations, the current study had many strengths. To our knowledge, this study was the first large investigation of adolescents and young adults to assess the relation of a variety of healthy and unhealthy weight-control practices to subsequent weight change. In addition, the study was sufficiently large to be able to look at associations among females by age group and weight status.
Our results suggest that a variety of approaches are used to “diet” and that few dietary approaches successfully prevent long-term weight gain unless they are coupled with regular physical activity. The most commonly used dietary approaches to weight control were to follow a low-fat or low-calorie diet, to eliminate snacks and desserts, and to limit portion sizes. Exercise was also used by many youth as a weight-control strategy. However, similar to Lowry et al (38; 2000), we observed that relatively few of the participants who were trying to lose weight engaged in both dietary strategies and frequent physical activity to control their weight. Our results support the recommendation to modify both diet and physical activity to make lasting changes in weight. The 2008 Physical Activity Guidelines for Americans suggests that children and adolescents engage in ≥60 min/d of moderate-to-vigorous physical activity and that adults engage in 30–60 min of moderate-to-vigorous physical activity on ≥5 d/wk (39). Our results suggest that if these recommendations are followed, much excessive weight gain could be avoided among adolescents and young adults.
Acknowledgments
We thank the GUTS research group for their comments on the results and the GUTS participants for providing information on weight, height, and weight-control behaviors.
The authors' responsibilities were as follows—AEF: contributed to the study design and participated in data collection; and AEF, JH, BR, and WCW: contributed to the statistical analyses, interpretation of the results, and manuscript preparation. None of the authors had any financial or personal interest in organizations sponsoring this research.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 2006;295:1549–55 [DOI] [PubMed] [Google Scholar]
- 2.Serdula MK, et al. Prevalence of attempting weight loss and strategies for controlling weight. JAMA 1999;282:1353–8 [DOI] [PubMed] [Google Scholar]
- 3.Lowry R, Galuska DA, Fulton JE, Burgeson CR, Kann L. Weight management goals and use of exercise for weight control among U.S. high school students, 1991-2001. J Adolesc Health 2005;36:320–6 [DOI] [PubMed] [Google Scholar]
- 4.Weiss EC, Galuska DA, Khan LK, Serdula MK. Weight-control practices among U.S. adults, 2001-2002. Am J Prev Med 2006;31:18–24 [DOI] [PubMed] [Google Scholar]
- 5.Kruger J, Galuska DA, Serdula MK, Jones DA. Attempting to lose weight: specific practices among U.S. adults. Am J Prev Med 2004;26:402–6 [DOI] [PubMed] [Google Scholar]
- 6.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol 1999;67:967–74 [DOI] [PubMed] [Google Scholar]
- 7.Field AE, Colditz GA. Frequent dieting and the development of obesity among children and adolescents. Nutrition 2001;17:355–6 [DOI] [PubMed] [Google Scholar]
- 8.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics 2006;117:1203–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Field AE, Aneja P, Austin SB, Shrier LA, de Moor C, Gordon-Larsen P. Race and gender differences in the association of dieting and gains in BMI among young adults. Obesity (Silver Spring) 2007;15:456–64 [DOI] [PubMed] [Google Scholar]
- 10.French SA, Jeffery RW, Forster JL, McGovern PG, Kelder SH, Baxter JE. Predictors of weight change over two years among a population of working adults: the Healthy Worker Project. Int J Obes Relat Metab Disord 1994;18:145–54 [PubMed] [Google Scholar]
- 11.Schmitz KH, Jacobs DR, Jr, Leon AS, Schreiner PJ, Sternfeld B. Physical activity and body weight: associations over ten years in the CARDIA study. Coronary Artery Risk Development in Young Adults. Int J Obes Relat Metab Disord 2000;24:1475–87 [DOI] [PubMed] [Google Scholar]
- 12.French SA, Jeffery RW, Murray D. Is dieting good for you?: prevalence, duration and associated weight and behaviour changes for specific weight loss strategies over four years in US adults. Int J Obes Relat Metab Disord 1999;23:320–7 [DOI] [PubMed] [Google Scholar]
- 13.Field AE, Camargo CA, Jr, Taylor CB, Berkey CS, Roberts SB, Colditz GA. Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics 2001;107:54–60 [DOI] [PubMed] [Google Scholar]
- 14.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kann L, Warren CW, Harris WA, et al. Youth risk behavior surveillance–United States, 1995. MMWR CDC Surveill Summ 1996;45:1–84 [PubMed] [Google Scholar]
- 16.Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. Int J Eat Disord 2004;35:86–92 [DOI] [PubMed] [Google Scholar]
- 17.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH, et al. The disease burden associated with overweight and obesity. JAMA 1999;282:1523–9 [DOI] [PubMed] [Google Scholar]
- 18.Field AE, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 2001;161:1581–6 [DOI] [PubMed] [Google Scholar]
- 19.Wannamethee SG, Shaper AG, Walker M. Overweight and obesity and weight change in middle aged men: impact on cardiovascular disease and diabetes. J Epidemiol Community Health 2005;59:134–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rexrode KM, et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA 1997;277:1539–45 [DOI] [PubMed] [Google Scholar]
- 21.Trentham-Dietz A, Newcomb PA, Egan KM, et al. Weight change and risk of postmenopausal breast cancer (United States). Cancer Causes Control 2000;11:533–42 [DOI] [PubMed] [Google Scholar]
- 22.Shoff SM, Newcomb PA, Trentham-Dietz A, et al. Early-life physical activity and postmenopausal breast cancer: effect of body size and weight change. Cancer Epidemiol Biomarkers Prev 2000;9:591–5 [PubMed] [Google Scholar]
- 23.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73 [DOI] [PubMed] [Google Scholar]
- 24.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr 2002;5:561–5 [DOI] [PubMed] [Google Scholar]
- 25.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics 2000;106:52–8 [DOI] [PubMed] [Google Scholar]
- 26.Strauss RS. Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. Int J Obes Relat Metab Disord 1999;23:904–8 [DOI] [PubMed] [Google Scholar]
- 27.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring) 2007;15:2357–64 [DOI] [PubMed] [Google Scholar]
- 28.Rosner B. Percentage points for a generalized ESD many-outlier procedure. Technometrics 1983;25:165–72 [Google Scholar]
- 29.Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ 1999;318:765–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Korkeila M, Rissanen A, Kaprio J, Sorensen TI, Koskenvuo M. Weight-loss attempts and risk of major weight gain: a prospective study in Finnish adults. Am J Clin Nutr 1999;70:965–75 [DOI] [PubMed] [Google Scholar]
- 31.Field AE, Austin SB, Taylor CB, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003;112:900–6 [DOI] [PubMed] [Google Scholar]
- 32.National Institutes of Health Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda, MD: National Institutes of Health, 1998 [PubMed] [Google Scholar]
- 33.Stice E, Akutagawa D, Gaggar A, Agras WS. Negative affect moderates the relation between dieting and binge eating. Int J Eat Disord 2000;27:218–29 [DOI] [PubMed] [Google Scholar]
- 34.Ackard DM, Neumark-Sztainer D, Story M, Perry C. Overeating among adolescents: prevalence and associations with weight-related characteristics and psychological health. Pediatrics 2003;111:67–74 [DOI] [PubMed] [Google Scholar]
- 35.Iqbal SI, Helge JW, Heitmann BL. Do energy density and dietary fiber influence subsequent 5-year weight changes in adult men and women? Obesity (Silver Spring) 2006;14:106–14 [DOI] [PubMed] [Google Scholar]
- 36.Savage JS, Marini M, Birch LL. Dietary energy density predicts women's weight change over 6 y. Am J Clin Nutr 2008;88:677–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vergnaud AC, Estaquio C, Czernichow S, et al. Energy density and 6-year anthropometric changes in a middle-aged adult cohort. Br J Nutr 2009;102:1–8 [DOI] [PubMed] [Google Scholar]
- 38.Lowry R, Galuska DA, Lowry R, Galuska DA, Fulton JE, Wechsler H, Kann L, Collins JL. Physical activity, food choice, and weight management goals and practices among US college students. Am J Prev Med 2000;18:18–27 [DOI] [PubMed] [Google Scholar]
- 39.US Department of Health and Human Services Physical Activity Guidelines Advisory Committee Report. Washington, DC: US Department of Health and Human Services, 2008 [Google Scholar]