Abstract
This study investigated sudden gains, i.e., rapid and stable improvements, in posttraumatic stress disorder (PTSD) symptoms that may occur in cognitive–behavioral therapy. Twenty-nine of 72 participants (39.2%) experienced a sudden gain during treatment. Mixed model ANOVAs analyzed sudden gains impact on clinician-rated PTSD symptom severity, patient-rated PTSD symptom severity, and patient-rated depressive symptom severity. Sudden gains in PTSD symptomology were associated with greater reductions in PTSD symptom severity for the avoidance/numbing and hyperarousal symptom clusters at posttreatment. By 6-month follow-up, the sudden gains group had maintained those reductions in symptoms, but the nonsudden gains group had achieved equal reductions in symptom severity. Participants experiencing sudden gains on PTSD measures had lower depression severity at posttreatment and follow-up.
A number of studies have documented the effectiveness of cognitive–behavioral treatments (CBT) for posttraumatic stress disorder (PTSD). Intention-to-treat analyses reveal that 44–60% of clients show significant improvement in PTSD symptomatology, with approximately 50% no longer meeting diagnostic criteria for PTSD by the end of treatment and at follow-up (e.g., Bradley, Greene, Russ, Dutra, & Westen, 2005; Resick, Monson, & Gutner, 2007). There has been less research on treatment process factors that help elucidate mechanisms underlying treatment response and how the course of treatment is related to treatment outcome. Rather than assume that symptomatology declines at a steady rate over the course of treatment, clinical experience and some research suggest that PTSD symptoms may respond differentially depending on the targets of a given treatment session (Nishith, Resick, & Griffin, 2002). There are very few studies that have examined individual differences in the course of response to PTSD treatment (Gilboa-Schechtman & Foa, 2001; Nishith et al., 2002). To our knowledge, this is the first study to examine “sudden gains,” a form of treatment response that involves rapid and stable reduction in symptomatology in PTSD.
Comparatively more research exists on patterns of response during treatment for depression. Tang and DeRubeis (1999) documented a nonlinear treatment course for a sizeable percentage of treatment responders, that is, occurrences of large sudden improvements from one session to the next within CBT for depression. This phenomenon has been labeled a “sudden gain,” defined as a dramatic and stable reduction in symptom intensity that occurs between the beginning of one session and the beginning of the next, and has been operationally defined with a specific formula for calculation (detailed below). Tang and DeRubeis (1999) found that 37% of depressed patients experienced sudden gains that accounted for 50% of their total symptom improvement over the course of treatment. The study further demonstrated that although there were no differences between individuals who experienced sudden gains and those who did not immediately following treatment, the occurrence of sudden gains predicted more favorable outcomes 18 months posttreatment. These findings are particularly important given the high relapse rate in depression after treatment (Fava et al., 2004) because they suggest that treatment responders who experience a sudden gain have better long-term outcomes than those responders who do not experience a sudden gain.
Since Tang and DeRubeis’s (1999) study, a growing body of research has replicated and expanded upon their findings, revealing that sudden gains significantly predict better outcomes for individuals in a variety of psychotherapies for depression (Busch, Kanter, Landes, & Kohlenberg, 2006; Gaynor et al., 2003; Hardy et al., 2005; Kelly, Roberts, & Ciesla, 2005; Tang, DeRubeis, Beberman, & Pham, 2005; Tang, Luborsky, & Andrusyna, 2002). Moreover, sudden gains have been found to occur in cognitive–behavioral group therapy and exposure therapy for social phobia (Hofmann, Schulz, Meuret, Moscovitch, & Suvak, 2006) and in psychotherapy for a variety of disorders in routine clinic conditions (Stiles et al., 2003).
The present study aims to investigate whether sudden gains occur in CBT for PTSD, and whether they are relevant to treatment outcomes. Data were obtained from a larger study that investigated the efficacy of cognitive processing therapy (CPT) and its dismantled components (Resick et al., 2008). Consistent with the depression literature, we predicted that sudden gains would occur in PTSD treatment at similar rates. We further hypothesized that sudden gains would predict better symptom severity outcomes at posttreatment and at follow-up because cognitive–behavioral PTSD treatment has historically demonstrated continued improvements in symptom severity posttreatment and relatively low rates of relapse (Resick et al., 2007). In addition, previous research suggests different patterns of change in types of PTSD symptoms over the course of CBT for PTSD (Nishith et al., 2002). Nishith et al. (2002) found a quadratic symptom pattern for total PTSD symptomatology as well as reexperiencing and arousal symptom cluster scores. However, these authors found that the avoidance symptoms demonstrated a more linear pattern over the course of CPT treatment and a quadratic pattern in prolonged exposure (PE). In PE, there was an initial increase in symptoms in the early sessions that decreased in later sessions. Therefore, we also analyzed the association between sudden gains in the different symptom clusters comprising PTSD to better understand the nature of CBT effects on PTSD. We did not identify any hypotheses associated with the symptom clusters due to the lack of research in this area.
Finally, the comorbidity between PTSD and depression is well established (Oquendo et al., 2005), and existing PTSD treatments also improve levels of depression (Resick, Nishith, Weaver, Astin, & Feuer, 2002). Because sudden gains have been indicated as having a significant role in response to depression treatment and considering that PTSD sudden gains may also be related to depression outcomes, we hypothesized that sudden gains in PTSD would predict a greater decrease in depression severity at long-term follow-up.
METHOD
Participants
This study uses data from a treatment outcome study that dismantled the core elements of CPT (Resick et al., 2008). In this study, women who had PTSD from a sexual or physical assault were randomized to receive full CPT, CPT with cognitive therapy only and no written account (CPT-C), or written account only. Similar to Tang and DeRubeis (1999), we excluded all participants who did not complete at least 75% of the sessions, resulting in a sample of 90 women out of the original 150. Of the 90 potential participants in our study, a sufficient number of scores on the primary measure used to assess sudden gains and treatment outcome (see below) were not available for 16 individuals; thus, the analyses were completed with a total of 74 participants. Of these, 58% identified as Caucasian, 34% as African American, 2% as Asian, and 6% as other. The mean age was 35.4 years (SD = 12.4) and mean education level was 13.8 years (SD = 2.8). The 74 women did not differ significantly from the original 150 in terms of age, ethnicity, level of education, socioeconomic status, type of index trauma, or PTSD severity at pretreatment.
All participants in this study met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV ; American Psychiatric Association [APA], 1994) criteria for PTSD and were randomized to one of three treatment conditions: CPT (n = 24), CPT-C (n = 24), or written account only (n = 26) described in detail in Resick et al. (2008). Briefly, CPT includes both systematic cognitive therapy, focusing first on the traumatic event and then disruptions in beliefs more broadly, as well as written accounts in which they detail their worst traumatic event and read it to themselves daily. The CPT-C condition omits the written account component and has more time dedicated to cognitive errors and challenging beliefs. The written account only condition excludes cognitive work and focuses solely on the written account and reading it repeatedly to oneself and the therapist. Participants in CPT and CPT-C received 12 sessions of therapy, each 60 minutes long. Participants in the written account only group had two 60-minute sessions in the first week and then 5 weekly sessions, 2 hours in length, thus standardizing total hours of treatment to 12 hours over a 6-week period.
Measures
The Posttraumatic Stress Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) is a 49-item self-report measure that assesses trauma history and all DSM-IV criteria for the diagnosis of PTSD. Respondents rate the frequency of each symptom item on a scale from 0 to 3, with higher scores indicating greater frequency of symptoms. The PDS has demonstrated reliability and validity with a heterogeneous trauma group (Foa et al., 1997). The PDS has previously demonstrated high internal consistency and test-retest reliability for total PDS score (Foa et al., 1997). In the current study, the PDS was administered weekly throughout therapy, as well as at pretreatment, posttreatment, and 6-month follow-up assessments. The PDS total symptom severity score was used to determine the presence or absence of a sudden gain.
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990) is a widely used 22-item interviewer-administered diagnostic instrument. The CAPS yields frequency and intensity rating scales for all 17 symptoms identified in the DSM-IV (APA, 1994), as well as a total severity score. The CAPS has excellent psychometric properties (Blake et al., 1990, 1995). The CAPS can be used to assess either diagnosis or severity of PTSD. For each symptom, a clinician rates two separate dimensions, frequency, and intensity of symptoms. For the purposes of this study, the total PTSD symptom severity score and the diagnostic classification were used. Among raters, 100% diagnostic reliability was established and high inter-rater agreement on the three clusters was found with kappa values and percentages of agreement ranging from .69 to .87 and 77% to 90%, respectively (Resick et al., 2008). The CAPS was administered at pretreatment, posttreatment, and 6-month follow-up.
The Beck Depression Inventory-II (BDI-II, Beck, Steer, & Brown, 1996) is a 21-item self-report measure that assesses depressive symptoms. It is frequently used to assess depression and is well validated (Beck et al., 1996). Items are rated on a 4-point severity scale. Total scores are obtained by summing the items and are clinically evaluated using a cut-off score of 14 for clinical levels of depression symptoms. In the main treatment outcome study (Resick et al., 2008), the BDI-II was used to assess comorbid depression at the same weekly assessment points as the PDS. We primarily utilized the BDI-II in this study at pretreatment, post-treatment, and 6-month follow-up. However, we also used the weekly scores to calculate sudden gains in depression as part of our post hoc analyses (see Results section below). Cronbach’s alpha in the current sample was .93.
Data Analysis
We used an adapted version of Tang and DeRubeis’s (1999) sudden gain criteria to determine a sudden gain in this study. The first criterion for a sudden gain, absolute magnitude, states that there must be a significant decrease from the previous score. Specifically, the gain must represent a clinically significant change, operationalized as the primary measure’s reliable change index (RCI; for formulas see Jacobson & Truax, 1991). We calculated the RCI for the PDS using a 95% confidence interval, which resulted in a change of at least 12 points. The second criterion of comparative magnitude is operationalized as a 25% decrease in total score on the PDS from the prior score. The third criterion, relative symptom variation, specifies that the improvement should be large enough in comparison to symptom fluctuation before and after the gain. This criterion requires that the mean of the scores for the two sessions before the gain has to be significantly higher than the scores for the two sessions after the gain, using a two-sample t-test with an alpha level of .05. We modified this criterion from Tang and DeRubeis’s original criteria by calculating the mean scores weekly, which corresponded to every session for written account only and every other session for CPT and CPT-C. For the CPT and CPT-C conditions, session-by-session PDS scores were not collected as part of the main study and therefore not available for these secondary analyses. The sessions were held twice a week for two of the groups (CPT and CPT-C) and weekly for written account only (all three conditions had 2 hours of therapy per week). Because the purpose of the third criteria is to ensure that the sudden gain is maintained and is not a result of normal symptom fluctuation, the adaptation of using weekly, rather than session, scores appeared to be a viable alternative. Our change reflects the brief nature of the therapies included in this study (7–12 sessions over 6 weeks) and the fact that assessments were limited to eight time points (six weekly session scores, pretreatment, and posttreatment). As a result, sudden gains were calculated at four time points (weeks 2–5) to account for two sessions before and after the gain.
We used chi-square analyses to evaluate whether there were differences in the occurrence of sudden gains across treatment conditions. A series of 2 (sudden gain status) × 3 (time: pre-treatment, posttreatment, follow-up) mixed model ANOVAs were calculated to test whether there were differences in clinician-rated total PTSD symptom (CAPS) severity and the severity of each of the three CAPS symptom clusters, patient-rated PTSD symptom severity (PDS), and patient-rated depressive symptom severity (BDI-II) by each of the two factors and their interaction. Treatment type was not included as a factor in these analyses because there was no difference in the occurrence of sudden gains by treatment type (reported below) and because the sample size was too small to detect differences in a 3 × 2 × 3 analysis. In addition, we conducted post hoc analyses using Tang and DeRubeis’s (1999) criteria on the BDI-II to examine the association between sudden gains in depression and sudden gains in PTSD.
RESULTS
Based on our adapted sudden gain criteria, 29 of the participants (39.2%) experienced at least one sudden gain during the course of treatment. The occurrence of sudden gains did not significantly differ by treatment condition, χ2 < 1. Among participants who experienced a sudden gain, 37.9% were in the CPT treatment group, 27.6% were in the written account only treatment condition, and 34.5% were in the CPT-C condition. The average reduction in total PDS score per sudden gain was 16.72 (SD = 5.97, range = 12–39).
Clinician- and Patient-Rated Total PTSD Symptom Severity
The 2 (Sudden Gain) × 3 (Time) mixed ANOVAs with total CAPS and total PDS as the outcome variables revealed a significant interaction between sudden gain status and time (see Table 1 for details). Follow-up contrasts for the total CAPS and PDS revealed a significant quadratic pattern (i.e., curvilinear) on both measures, F (1, 72) = 11.83, p < .01 and F (1, 72) = 10.54, p< .01, respectively. There were no significant differences in pretreatment total CAPS or PDS scores between those with and without sudden gains during treatment. At posttreatment, those who experienced a sudden gain had significantly lower total CAPS and PDS scores than those who did not experience a sudden gain. However, at follow-up there was no significant difference in total CAPS or PDS scores between those who had a sudden gain and those who did not. The pattern of results in both measures is illustrated by the presentation of the CAPS data in Figure 1. There were no main effects for sudden gain status for total CAPS or PDS scores. Consistent with the primary outcomes reported, there was a main effect for time for total CAPS and PDS scores, as shown in Table 1.
Table 1.
Analysis of Variance for Symptom Severity in Clinician and Patient-Rated Posttraumatic Stress Disorder Symptomatology
| Main effect of sudden gain; F (1, 72) | Main effect of time; F (2, 144) | Interaction of time & sudden gain; F (2, 144) | |
|---|---|---|---|
| CAPS Total | <1 | 158.93** | 5.56** |
| CAPS Avoidance/numbing | <1 | 123.21** | 4.18* |
| CAPS Hyperarousal | 2.33 | 81.78** | 6.66** |
| CAPS Reexperiencing | 3.33 | 117.40** | <1 |
| PDS | <1 | 163.77** | 10.17** |
Note. CAPS = Clinician Administered PTSD Scale; PDS = Posttraumatic Diagnostic Scale.
p < .05.
p < .01.
Figure 1.
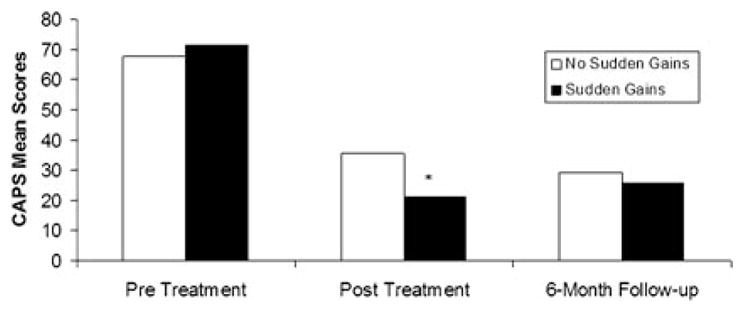
Clinician-Administered PTSD Scale (CAPS) total symptom severity of the sudden gain and nonsudden gain groups, * p < .05.
Clinician-Rated PTSD Symptom Cluster Severity
A significant interaction was found between sudden gain status and time for the CAPS cluster scores of avoidance/numbing and hyperarousal symptoms (see Table 1). Follow-up contrasts revealed a similar quadratic pattern to the interaction in these subscales to that found for total CAPS and PDS scores: for avoidance numbing, F (1, 72) = 14.48, p< .01 and for hyperarousal, F (1, 72) = 8.17, p< .01. There were no main effects for sudden gain status in these CAPS subscales but there were main effects for time (see Table 1).
Contrary to the pattern of findings found in total CAPS and the avoidance/numbing and hyperarousal CAPS clusters, there was no significant interaction between sudden gain status and time in CAPS cluster scores for reexperiencing symptoms. There was a main effect for time for CAPS reexperiencing symptom scores (see Table 1).
Patient-Rated Depression Symptom Severity
There was a significant interaction between PTSD sudden gain status and time for BDI-II scores, F (2, 144) = 3.08, p < .05. Follow-up contrasts revealed that the linear effect just failed to meet conventional levels of statistical significance, F (1, 72) = 3.92, p = .052. As shown in Figure 2, there were no differences between those with and without a sudden gain at pretreatment, but those experiencing sudden gains had lower BDI-II scores at posttreatment and follow-up assessments compared with those without sudden gains. The two groups continued to improve at follow up. There was no main effect for PTSD sudden gain status for BDI-II scores between subjects, F (1, 72) = 2.09, ns, but there was a main effect for time within subjects, F (2, 144) = 83.78, p < .01.
Figure 2.
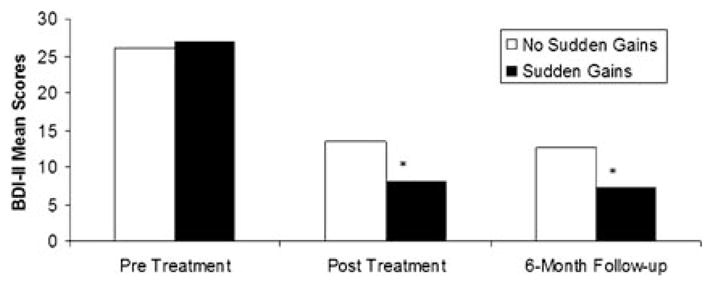
Beck Depression Inventory-II (BDI-II) symptom severity of the sudden gain and nonsudden gain groups, * p < .05.
To examine the possibility that sudden gains in PTSD symptomatology were accounted for by changes in depression, post hoc analyses were conducted to examine the prevalence of sudden gains in depression symptoms. Using the weekly BDI-II scores, and the Tang and DeRubeis (1999) criteria for determining sudden gains, we found only six participants (8%) had a sudden gain in depression symptomatology and only four participants (5.4%) had both a sudden gain in depression and PTSD.
DISCUSSION
This study examined the occurrence of sudden gains in psychotherapy for the treatment of PTSD. Consistent with our hypothesis, sudden gains do appear to occur in CBT for PTSD and happen at similar rates to sudden gains in the treatment of depression. There were no statistically significant differences in the frequency of sudden PTSD gains between the three treatment conditions most likely due to the small sample sizes per cell. However, the similarity across treatments may also be attributable to the presence of common therapeutic interventions found in the three cognitive–behavioral treatments, such as those targeting avoidance and directly addressing traumatic material. Further, consistent with current cognitive–behavioral theories of PTSD, different interventions with different routes to changing the same mechanisms may be at work, resulting in similar rates of sudden gains in the course of treatment (Foa, Rothbaum, Riggs, & Murdock, 1991). Future research should be conducted to clarify whether there are similar mechanisms in different therapies leading to sudden improved treatment outcome across therapeutic interventions.
This study also suggests that participants who experience a sudden gain during the course of PTSD treatment will have greater symptom reductions at the end of treatment compared with those who do not experience such a gain. However, the presence of a sudden gain during treatment does not appear to be associated with the amount of symptom reduction at follow-up. Although these findings call into question the importance of a sudden gain in predicting sustained response to PTSD treatment, they suggest that sudden gains may be important to the efficiency of therapies. In other words, those experiencing sudden gains may respond to treatment more quickly. However, a potential alternative explanation is simply that the PTSD results are an artifact of the definition of sudden gain and regression to the mean. Further, the timing of sudden gains in PTSD treatment may be different across therapies, but we were not able to compare when the sudden gains occurred in the three treatments due to limitations in the number of assessments given over the course of treatment and the small sample sizes. Therefore, more research is needed in this area, as it will be critical to better understand whether mechanisms at work in the beginning or end of treatment are more important to treatment outcome, both immediate and long-term (6-month follow-up).
In examining PTSD symptom clusters, this study indicates that sudden gains are similarly associated with change in avoidance/numbing and hyperarousal symptoms, i.e., sudden gains are associated with greater symptom reduction at the end of treatment, but not at follow-up. In contrast, a different pattern emerged in the reexperiencing symptom cluster. The results showed neither significant time by sudden gain group interaction nor a sudden gain group main effect. It appears that PTSD sudden gains, as measured by self-report PDS scores, are largely driven by changes in avoidance/numbing and hyperarousal symptoms, and not by changes in reexperiencing symptoms. There is some evidence that high levels of reexperiencing symptoms make it more difficult to be cognitively flexible, given the amount of cognitive resources taken up by these symptoms (Hellawell & Brewin, 2002; Shipherd & Salters-Pedneault, 2008; Vasterling & Brailey, 2005). Thus, patients with these significant cognitive intrusions may be less able to experience a cognitive shift or sudden gain during treatment.
Although sudden gains may not be uniquely predictive of longer-term PTSD outcomes, our study indicates that sudden gains are important in comorbid depression outcomes. We found that participants who had sudden gains in PTSD symptoms during treatment had significantly lower levels of depression at the end of treatment and at 6-month follow-up compared with those who did not evidence a sudden gain. Moreover, post hoc analyses suggest that the effects were not due to sudden gains in depression symptoms. This pattern of findings reinforces the notion that there are different processes underlying PTSD and depression, and that cognitive shifts may, in turn, be more or less relevant to these mechanisms. These findings are particularly relevant to better understanding the possible differences in mechanisms of action in PTSD treatment compared with depression treatment, but more research is needed to determine the differences of therapy process in PTSD and co-occurring depression.
As with other studies of sudden gains, a potential limitation of this study was the reliance on a self-report measure to determine sudden gains. However, because the study of sudden gains requires the use of repeated measurements, a more thorough interview-based assessment is not practical. The nature of the sample (i.e., exclusively female, PTSD from sexual or physical assault) requires that this study be replicated with more diverse samples to assess the generalizability of the findings. Another limitation of this study, in comparison with other sudden gain studies, is that only PDS scores from every other session were available for two of the three treatment conditions. As a result, we altered the sudden gain criteria in this study. This change may have inflated the number of individuals meeting the criteria because these sudden gains calculations are based on differences between two therapy sessions instead of one. On the other hand, the PDS was administered weekly, thus allowing for the calculation of sudden gains based on weekly measurements, which is comparable to other studies (Gaynor et al., 2003; Tang et al., 2002; Vittengl, Clark, & Jarrett, 2005). Additionally, only a limited number of sudden gains were possible, given the criteria and the duration of the therapies (i.e., 6 weeks). Thus, it is possible that the percentage of sudden gains found in this study may be an overestimate of the percentage of participants who will experience a sudden gain in more natural treatment settings. Because this is the first study of its kind, it is important that this be a launching point for more research in this area.
Future research is also needed in the area of mechanisms of change in cognitive–behavioral psychotherapies for PTSD. Although this article outlines the relationship between sudden gains and PTSD treatment outcome, further research is needed to examine the process of sudden gains in PTSD treatment. It seems important to identify what specifically occurs in treatment just prior to a sudden gain so that overall therapy can be enhanced. This objective was beyond the scope of this study. Future research may ultimately lead to briefer, more efficient therapies, and greater knowledge gained about potential critical sessions could lead to more effective evidence-based therapies for PTSD.
Acknowledgments
We would like to thank Dr. Suzanne Pineles for helpful thoughts and comments on the manuscript.
Contributor Information
Kacie A. Kelly, Women’s Health Sciences Division, National Center for PTSD, VA Boston Healthcare System, Boston, MA
Shireen L. Rizvi, Department of Psychology, New School for Social Research, New York, NY
Candice M. Monson, Women’s Health Sciences Division, National Center for PTSD, VA Boston Healthcare System, and Department of Psychiatry, Boston University, Boston, MA
Patricia A. Resick, Women’s Health Sciences Division, National Center for PTSD, VA Boston Healthcare System, and Departments of Psychiatry and Psychology, Boston University, Boston, MA
References
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. 2. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, et al. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. The Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Busch AM, Kanter JW, Landes SJ, Kohlenberg RJ. Sudden gains and outcome: A broader temporal analysis of cognitive therapy for depression. Behavior Therapy. 2006;37:61–68. doi: 10.1016/j.beth.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Fava GA, Ruini C, Rafanelli C, Rinos L, Conti S, Grandi S. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. American Journal of Psychiatry. 2004;161:1872–1876. doi: 10.1176/ajp.161.10.1872. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Gaynor ST, Weersing VR, Kolko DJ, Birmaher B, Heo J, Brent DA. The prevalence and impact of large sudden improvements during adolescent therapy for depression: A comparison across cognitive-behavioral, family, and supportive therapy. Journal of Consulting and Clinical Psychology. 2003;71:386–393. doi: 10.1037/0022-006x.71.2.386. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Foa EB. Patterns of recovery from trauma: The use of intraindividual analysis. Journal of Consulting and Clinical Psychology. 2001;110:392–400. doi: 10.1037//0021-843x.110.3.392. [DOI] [PubMed] [Google Scholar]
- Hardy GE, Cahill J, Stiles WB, Ispan C, Macaskill N, Barkham M. Sudden gains in cognitive therapy for depression: A replication and extension. Journal of Consulting and Clinical Psychology. 2005;73:59–67. doi: 10.1037/0022-006X.73.1.59. [DOI] [PubMed] [Google Scholar]
- Hellawell SJ, Brewin CR. A comparison of flashbacks and ordinary autobiographical memories of trauma: Cognitive resources and behavioural observations. Behaviour Research and Therapy. 2002;40:1143–1156. doi: 10.1016/s0005-7967(01)00080-8. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Schulz SM, Meuret AE, Moscovitch DA, Suvak M. Sudden gains during therapy of social phobia. Journal of Consulting and Clinical Psychology. 2006;74:687–697. doi: 10.1037/0022-006X.74.4.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kelly MA, Roberts JE, Ciesla JA. Sudden gains in cognitive behavioral treatment for depression: When do they occur and do they matter? Behavior Research Therapy. 2005;43:703–714. doi: 10.1016/j.brat.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Nishith P, Resick PA, Griffin MG. Pattern of change in prolonged exposure and cognitive-processing therapy for female rape victims with post-traumatic stress disorder. Journal of Consulting and Clinical Psychology. 2002;70:880–886. doi: 10.1037//0022-006x.70.4.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo M, Brent DA, Birmaher B, Greenhill L, Kolko DJ, Stanley B, et al. Posttraumatic stress disorder comorbid with major depression: Factors mediating the association with suicidal behavior. American Journal of Psychiatry. 2005;162:560–566. doi: 10.1176/appi.ajp.162.3.560. [DOI] [PubMed] [Google Scholar]
- Resick PA, Galovski T, Uhlmansiek M, Scher C, Clum G, Young-Xu Y. A randomized clinical trial to dismantle cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Gutner C. Psychosocial Treatments for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. PTSD: Science and practice–a comprehensive handbook. New York: Guilford Press; 2007. pp. 330–358. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipherd JS, Salters-Pedneault K. Attention, memory, intrusive thoughts and acceptance in PTSD: An update on the empirical literature for clinicians. Cognitive and Behavioral Practice. 2008;15:349–363. [Google Scholar]
- Stiles WB, Leach C, Barkham M, Lucock M, Iveson S, Shapiro DA, et al. Early sudden gains in psychotherapy under routine clinic conditions: Practice-based evidence. Journal of Consulting and Clinical Psychology. 2003;71:14–21. [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73:168–172. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Tang TZ, Luborsky L, Andrusyna T. Sudden gains in recovering from depression: Are they also found in psychotherapies other than cognitive-behavioral therapy? Journal of Consulting and Clinical Psychology. 2002;70:444–447. [PubMed] [Google Scholar]
- Vasterling JJ, Brailey K. Neuropsychological findings in adults with PTSD. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: Biological, cognitive, and clinical perspectives. New York: Guilford Press; 2005. pp. 178–207. [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Validity of sudden gains in acute phase treatment of depression. Journal of Consulting and Clinical Psychology. 2005;73:173–182. doi: 10.1037/0022-006X.73.1.173. [DOI] [PubMed] [Google Scholar]


