Abstract
Purpose
Information on the use of complementary therapies in patients with advanced-stage cancer is limited. Given the disease and treatment complexities associated with the care of patients with metastatic cancer, oncology clinicians would benefit from having an appreciation of the extent of usage of unconventional, adjunctive therapies among these patients. This study evaluated the prevalence and demographic predictors of complementary therapy use in a sample of women with metastatic breast cancer.
Methods
Subjects with stage IV breast cancer were recruited from six treatment facilities in New England. A written, mailed survey assessing complementary therapy use and sociodemographic information was completed by each subject, while disease and treatment information was obtained from medical records. Descriptive statistics and multivariate logistic regression analyses were conducted.
Results
Of the 173 participants, 78% used at least one type of complementary therapy, 43% used two or more types, and 23% used three or more types, excluding spiritual practices and physical exercise. When including spiritual practices and physical exercise, 90% used at least one complementary therapy, 70% used two or more types, and 45% used three or more types. Visits to alternative health practitioners were predicted by younger age (P = .009) and higher education level (P = .002). Younger participants (P = .045) were more likely to use and spend more money on vitamins and herbal products (P = .02).
Conclusions
Use of unconventional therapies is pervasive among metastatic breast cancer patients, particularly among those who are younger and highly educated. Oncology providers need to assess patients' complementary therapy use and consider potential interactions with prescribed treatment protocols.
Introduction
Awareness of and interest in complementary therapies is increasing among patients with cancer.1–4 In general, these therapies are not used in isolation, but rather in addition to care prescribed by oncologists. Complementary therapy (CT) can be defined as unconventional therapeutic interventions used in conjunction with traditional Western allopathic medicine. The National Center for Complementary and Alternative Medicine (NCCAM) characterizes five major types of these nontraditional therapies: whole medical systems (eg, naturopathy, traditional Chinese medicine); mind-body medicine (eg, meditation, prayer); biologically based practices (eg, vitamins, herbal products, nutritional supplements); manipulative and body-based practices (eg, massage, chiropractic); and energy medicine (eg, reiki, qi gong).5
Documented use of CT among patients with cancer ranges from 45%6 to 88%,7 although the extent of use varies by diagnosis and patient characteristics.8 The major reasons for use include increasing one's chances of survival,9 alleviating adverse treatment effects,10 detoxifying the body,11 boosting immunity,8,12–14 enhancing quality of life,10–12,14 fostering a sense of control,12,14 and aiding conventional treatment.12 Bad experiences with conventional medicine and dissatisfaction with physicians have also been associated with CT use.9,15,14 Strikingly high CT use has been observed in patients enrolled onto cancer clinical trials,7,10 which is of concern because patients with cancer are oftentimes reticent to disclose their CT use to their oncologists, especially if not asked directly.1,12
While it is recognized that breast cancer patients, in general, are high users of CT, all but one published study16 were conducted in patients with early stage or mixed diagnoses.11,17,18 Given the complexities of medical management of patients with metastatic breast cancer, having an appreciation of CT use and its predictors in these patients would be valuable to oncology providers. This study evaluated the prevalence of CT use in a sample of patients with stage IV breast cancer and examined the association between specific patient characteristics and the use of these practices. Information gained from this study could propel oncologists to become more knowledgeable about different CT therapies and more astute in their assessments of CT use and related benefits and toxicities in their patients with metastatic breast cancer.
Patients and Methods
Participants
A convenience sample of women with stage IV breast cancer were recruited from six treatment facilities in New England, including two National Cancer Institute–designated comprehensive cancer centers, two tertiary care medical centers, one community hospital, and one community oncology practice, between April 2000 and March 2003. This was a secondary analysis of deidentified baseline data from a behavioral intervention randomized trial.19 Eligibility criteria included confirmed stage IV breast cancer diagnosis, the ability to read and write in English, and prognosis of at least 6 months (determined by an attending medical oncologist). On approval of the institutional review boards, potential subjects were identified by oncology providers or responded to flyer advertisements (for the parent study) posted within the institutions. Written informed consent was obtained.
Questionnaire
An eight-item questionnaire, designed by this study team, assessed particular CT practices. The questionnaire assessed CT practices within each of the major NCCAM categories: whole medical systems (visits to acupuncturists and naturopathic doctors), biologically based practices (visits to herbalists, use of herbal products and vitamin supplements), mind-body medicine (meditation, yoga, spiritual practices, and journal writing), manipulative and body-based practices (visits to massage therapists and participation in aerobic physical exercise), and energy medicine (visits to energy healers, including reiki and therapeutic touch practitioners). Herbal products and vitamin supplements were based on use in the last 3 months and the total amount of money spent on these products in the previous month. A checklist of specific alternative health practitioners assessed number of visits in previous 3 months to massage therapists, acupuncturists, naturopathic doctors, energy healers, herbalists, and other nontraditional healers. Meditation, yoga practice, aerobic physical exercise (at least 20 minutes per session), and spiritual practices were based on use in an average week, while journal writing was based on current use. Participant responses were based on their own interpretation of the CT terms as they were not prompted with definitions or examples.
Procedures
The self-administered written questionnaire as well as a sociodemographic form were mailed to participants and returned in preaddressed stamped envelopes. Disease and treatment information were obtained from medical record review. All study forms were numerically coded to ensure confidentiality of responses.
Analysis
Descriptive statistics were calculated on the use of specific CT therapies. General linear regression analyses were conducted to examine the relationships between the number of individual types of CT used and particular patient background characteristics (ie, age, marital status, education, income, and performance status), and between the amount of money spent and patient background characteristics. Multivariable logistic regression analysis was used to examine the relationships between patient background characteristics and the use of vitamins and herbal products.
Results
Sample
A total of 232 patients consented and 59 dropped out before data collection, resulting in 25% attrition rate and a final sample of 173. The reasons for attrition are changed mind (n = 52), too sick (n = 2), lost to follow-up (n = 2), data lost (n = 2), and deceased (n = 1).
Sociodemographic characteristics of the sample are summarized in Table 1. The mean age of the participants at study entry was 54 years (standard deviation [SD], 12.0), while the mean age of first breast cancer diagnosis was 47 years (SD, 10.3). All but nine participants (5.2%) were (in the last 4 weeks) receiving at least one type of conventional cancer treatment: chemotherapy (n = 95), hormone therapy (n = 83), radiation therapy (n = 11), and surgery (n = 4). Participants were diagnosed with stage IV breast cancer on an average of 36 months (range, 0.6 to 311.9) before study participation.
Table 1.
Sociodemographic Characteristics (N = 173)
| Characteristic | Patients | |
|---|---|---|
| No. | % | |
| Race/ethnicity | ||
| White | 165 | 95.3 |
| Hispanic | 2 | 1.2 |
| Other/mixed/unknown | 2 | 1.2 |
| Missing data | 4 | 2.3 |
| Marital status | ||
| Married | 121 | 70.0 |
| Single/divorced/widowed | 49 | 28.3 |
| Missing data | 3 | 1.7 |
| Education | ||
| High school graduate or less | 35 | 20.2 |
| Some college | 34 | 19.6 |
| College graduate | 65 | 37.6 |
| Advanced degree | 38 | 22.0 |
| Missing data | 1 | 0.6 |
| Annual family income, US$ | ||
| < 15,000 | 14 | 8.1 |
| 15,000-29,000 | 16 | 9.2 |
| 30,000-59,000 | 41 | 23.7 |
| 60,000-99,000 | 52 | 30.1 |
| > 100,000 | 36 | 20.8 |
| Missing data | 14 | 8.1 |
| Employment status | ||
| Full time | 40 | 23.1 |
| Part time | 39 | 22.5 |
| Work from home | 28 | 16.2 |
| Retired | 23 | 13.3 |
| Disabled | 42 | 24.3 |
| Student | 1 | 0.6 |
Patterns of CT Use
Seventy-eight percent of the sample used at least one type of CT, 43% used two or more types, and 23% used three or more types, excluding spiritual practices and physical exercise. When including spiritual practices and physical exercise, the results changed: 90% used at least one CT, 70% used two or more types, and 45% used three or more types.
Specific frequency of use of individual CT, based on NCCAM's five categories, is as follows: whole-body systems (traditional Chinese medicine with acupuncture, n = 7; naturopathy, n = 5; biologically based practices (vitamins, n = 107; herbal supplements, n = 48; visits to herbalist, n = 4); mind-body medicine (spiritual practices, n = 126; meditation and/or yoga, n = 57; journal writing, n = 45; manipulative and body-based practices (aerobic physical exercise at least 20 minutes once per week, n = 123 and two or more times per week, n = 99; massage, n = 23); and energy medicine (n = 9).
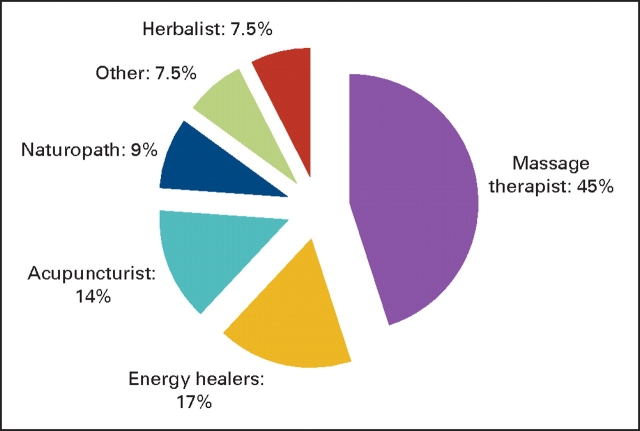
Fifty participants (29% of the sample) went to alternative health practitioners in the last 3 months, of which 16 went to more than one type of practitioner. Figure 1 illustrates the specific types and percentages of visits to these practitioners. Regarding herbal and vitamin supplements, the average amount of money spent per month was $48 (US dollars; range = $0 to $900; SD, $113.60), although information on specific herbal products and vitamin supplements was not obtained. Money spent on other CT was not assessed.
Figure 1.
Visits to alternative health practitioners.
Predictors of CT Use
General linear regression analyses show that younger participants (P = .009) with higher levels of education (P = .002) were more likely to use CT compared with older, less educated participants, excluding spiritual practices and physical exercise. When including spiritual practices and physical exercise, similar results were obtained (P = .010 for age, and P = .001 for education). Similarly, younger participants (P = .045) were more likely to spend more money on vitamins and herbal products than older participants. Logistic regression analysis shows that younger participants (odds ratio, 0.96; 95% CI, 0.93 to 0.99; P = .02) were also more likely to use herbal products. Other background variables (ie, functional status, income, and marital status) were not significant predictors of CT use in this sample.
Discussion
Our results indicate that CT use is clearly pervasive in our sample of patients with advanced-stage breast cancer, particularly those who are younger and more educated, which is consistent with studies of other cancer patients.2,6,20 The high use for these patients with metastatic disease can be explained by a myriad of reasons. These patients may feel vulnerable and be more willing to try anything given their poor prognosis. They may also use CT for management of symptoms from the disease itself or from conventional treatment toxicities, or to reduce anxiety and stress by making them feel more hopeful2 or more in control.10 They may also turn to CT if they perceive minimal risk in these therapies or if they are feeling dissatisfied with the quality of their conventional cancer care.9
More important than speculation about the reasons why patients with metastatic breast cancer use CT is the need for oncology clinicians to be aware that their patients are likely using CT. While many of the CTs are noninvasive with minimal likely adverse effects, some may have the potential to interfere with standard cancer therapies. Ninety-five percent of our sample was receiving conventional breast cancer treatment, while a remarkably high percentage was also using one or more CT, including vitamins and herbal supplements. Given the concomitant uses of CT in combination with conventional oncology treatment, the potential for drug-herb-vitamin interactions is a serious concern to the oncology community.21,22 Information about the toxicity and interactions of specific CT (particularly with ingested products) with conventional treatment is scarce, which highlights the need for thorough assessment of CT use and good communication between cancer patients and their oncology providers. The reluctance of oncology clinicians to initiate such open discussions with their patients could be due in part to the lack of reliable information on the safety and efficacy of these therapies, yet this lack of information has clearly not prevented patients from using these therapies. Therefore oncologists must maintain an open mind about their patients' treatment choices and encourage frank discussions about the potential risks and benefits of particular types of CT.23
Limitations of this study must be acknowledged. Despite our efforts to recruit a diverse sample of patients, the participants in the study were predominantly well-educated and white, limiting the generalizability of our results. Furthermore, a confounding factor is that this study was a secondary analysis whereby our sample was originally recruited to participate in a behavioral intervention trial. Therefore, there may be selection bias as the volunteers for the parent study may have been more inclined to use CT compared with a random sample of patients with metastatic breast cancer. Contributing to selection bias, some subjects were recruited through referral from oncology providers who likely had a predilection for referring patients who they may have perceived to be using or have an interest in CT. Furthermore, we are limited by the self-report nature of the questionnaire and the lack of details of some of the CT assessed; for example, we did not provide definitions nor obtain specific information on the types of vitamins, herbal products, or aerobic physical activities.
In conclusion, our results underscore that women living with metastatic breast cancer may be actively using a variety of CTs while also undergoing conventional cancer treatments. Given the disease and treatment complexities associated with the treatment of these patients, information related to CT use in these patients is of great importance to oncology clinicians.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Acknowledgment
This study was conducted at the Dana-Farber Cancer Institute, where Ms Gross and Dr Bauer-Wu had a previous affiliation in The Phyllis F. Cantor Center. The authors would like to acknowledge support from the Georgia Cancer Coalition Distinguished Scholars program as well as the Susan G. Komen Breast Cancer Foundation (who funded the parent study).
References
- 1.Yates J, Mustian K, Morrow G, et al: Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer 13:806-811, 2005 [DOI] [PubMed] [Google Scholar]
- 2.Richardson M, Sanders T, Palmer J, et al: Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol 18:2505-2514, 2000 [DOI] [PubMed] [Google Scholar]
- 3.Kelly K, Jacobsen J, Kennedy D, et al: Use of unconventional therapies by children with cancer at an urban medical center. J Ped Hematol Oncol 22:412-416, 2000 [DOI] [PubMed] [Google Scholar]
- 4.Patterson R, Neuhouser M, Hedderson M, et al: Types of alternative medicine used by patients with breast, colon, or prostate cancer: Predictors, motives, and costs. J Alt Comp Med 8:477-485, 2002 [DOI] [PubMed] [Google Scholar]
- 5.National Center for Complementary and Alternative Medicine: Definition and categories of CAM, http://nccam.nih.gov/health/whatiscam/
- 6.Molassiotis A, Scott J, Kearney N, et al: Complementary and alternative medicine use in breast cancer patients in Europe. Supportive Care in Cancer 14:260-267, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Dy G, Bekele L, Hanson L, et al: Complementary and alternative medicine use by patients enrolled onto phase I clinical trials. J Clin Oncol 22:4810-4815, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Morris K, Johnson N, Homer L, et al: A comparison of complementary therapy use between breast cancer patients and patients with other primary tumor sites. Am J Surg 179:407-411, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Boon H, Brown J, Gavin A, et al: Breast cancer survivors' perceptions of complementary/alternative medicine(CAM): Making the decision to use or not to use. Qualitative Health Research 9:639-653, 1999 [DOI] [PubMed] [Google Scholar]
- 10.Sparber A, Bauer L, Curt G, et al: Use of complementary medicine by adult patients participating in cancer clinical trials. Oncol Nurs Forum 27:623-630, 2000 [PubMed] [Google Scholar]
- 11.Tagliaferri M, Cohen I, Tripathy D: Complementary and alternative medicine in early-stage breast cancer. Semin Oncol 28:121-134, 2001 [DOI] [PubMed] [Google Scholar]
- 12.Boon H, Stewart M, Kennard M, et al: Use of complementary/alternative medicine by breast cancer survivors in Ontario: Prevalence and perceptions. J Clin Oncol 18:2515-2521, 2000 [DOI] [PubMed] [Google Scholar]
- 13.Hann D, Baker F, Robert C, et al: Use of complementary therapies among breast and prostate cancer patients during treatment: A multisite study. Integrative Cancer Therapies 4:294-300, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Henderson K, Daonatelle R: Complementary and alternative medicine use by women after completion of allopathic treatment for breast cancer. Alternative Therapies in Health and Medicine 10:52-57, 2004 [PubMed] [Google Scholar]
- 15.Lengacher C, Bennett M, Kip K, et al: Frequency of use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum 29:1445-1452, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Shen J, Andersen R, Albert P, et al: Use of complementary/alternative therapies by women with advanced-stage breast cancer: BMC Complementary and Alternative Medicine, 2002. http://www.biomedcentral.com/content/pdf/1472-6882-2-8.pdf [DOI] [PMC free article] [PubMed]
- 17.Burstein H, Gelber S, Guadagnoli E, et al: Use of alternative medicine by women with early-stage breast cancer. N Engl J Med 340:1733-1739, 1999 [DOI] [PubMed] [Google Scholar]
- 18.DiGianni L, Garber J, Winer E: Complementary and alternative medicine use among women with breast cancer. J Clin Oncol 20:34s-38s, 2002 [PubMed] [Google Scholar]
- 19.Bauer-Wu S, Liu Q, Hsieh C-C, et al: Expressive writing for metastatic breast cancer patients: Effects on symptoms, adjustment, and quality of life three months later, 8th National Conference on Cancer Nursing Research, Ft Lauderdale, FL, February 3-5, 2005
- 20.Navo M, Phan J, Vaughan C, et al: An assessment of the utilization of complementary and alternative medication in women with gynecologist or breast malignancies. J Clin Oncol 22:671-677, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Fugh-Berman A: Herb-drug interactions. Lancet 355:134-138, 2000 [DOI] [PubMed] [Google Scholar]
- 22.Izzo AA: Herb-drug interactions: An overview of the clinical evidence. Fundamental Clin Pharma 19:1-16, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Rosenthal D, Dean-Clower E: Integrative medicine in hematology/oncology: Benefits, ethical considerations, and controversies. Hematol: 491-497, 2005 [DOI] [PubMed]