Figure u1.
With a one in three chance of getting cancer in one's lifetime, Americans will either experience or know someone who has survived cancer. According to the Institute of Medicine report From Cancer Patient to Cancer Survivor: Lost in Transition, more than 10 million Americans live with a personal history of cancer; all are considered cancer survivors.
Some survivors experience few effects from their cancer treatment. Many survivors, however, manage psychological distress, sexual dysfunction, infertility, impaired organ function, cosmetic changes, and limitations in mobility, communication, and cognition. Others face risks from secondary cancers and such comorbidities as diabetes, cardiovascular disease, osteoporosis, or reproductive disorders. The good news is that with intervention, much can be done to avoid, ameliorate, or arrest these late effects of cancer, particularly if caregivers have access to key information regarding the patient's cancer, care, and treatment.
The transition from active treatment to post-treatment care is critical to long-term health. If care is not planned and coordinated, cancer survivors are left without knowledge of their heightened risks or a follow-up plan of action. Fragmented and poorly coordinated cancer care systems and poor communication mechanisms are among the hurdles cancer survivors often face.1 Remarkably absent from many survivors' care plans is a treatment summary containing critical information from the treating oncologist about the patient's cancer type and treatment.2 If a treatment summary were made available and exchanged in a secure electronic environment, it would enable the survivor and caregivers to effectively facilitate provider-to-provider and provider-to-patient communication.
This report (available at www.asco.org/ehr) identifies the unique communication issues for cancer patients and survivors, discusses the role of the treatment plan and treatment summary in continuity of care for cancer patients, and describes ASCO's position on the benefits of electronic medical record software for oncology practitioners and patients.
Background
Patients referred to an oncologist have almost always been recently dealt a sudden blow and usually restructure their everyday lives to focus on their health. By the time they present to an oncologist, patients typically have had visits with their primary care physician and other specialists, may have had surgery, and have had laboratory tests, x-rays, and other sophisticated radiological studies. When establishing a care plan, the oncologist analyzes reports from these encounters and, together with the patient, determines treatment methods, which may include chemotherapy, surgery, radiation therapy, or a combination of the three.
Chemotherapy Treatment Plan
A chemotherapy treatment plan is a synoptic document prepared at the initiation of a chemotherapy treatment course. Key elements of the treatment plan include diagnosis, goals and anticipated benefits of therapy, the regimen name, the planned duration and number of treatment cycles, a strategy for assessing response, and an assessment of major risks and benefits (available at www.asco.org/treatmentsummary). Ideally, the treatment plan should be reviewed with the patient and his or her family members when treatment is started. Because patients are often overwhelmed at the time of diagnosis, having a document that can be referred to later is valuable. Preparation of a plan at the start of treatment simplifies preparation of a summary at the conclusion of treatment (Fig 1).
Figure 1.
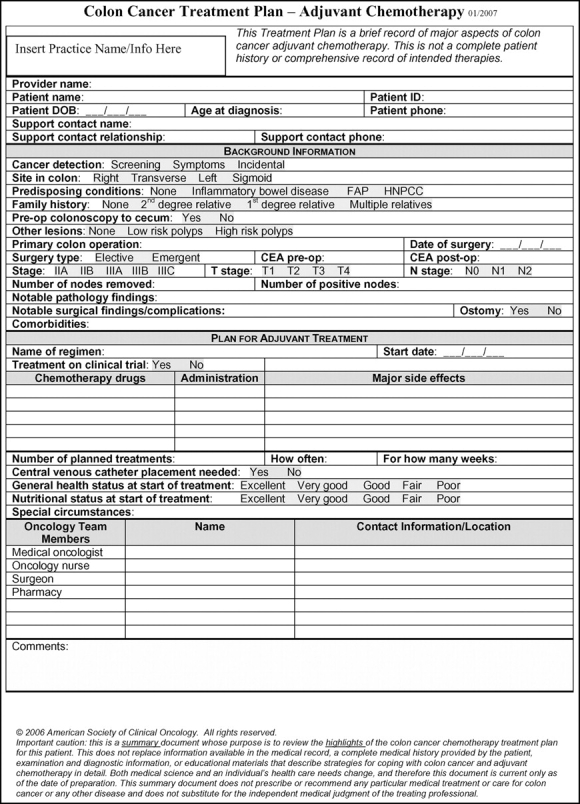
Sample treatment plan for colon cancer (available at www.plwc.org/ASCO/ArticleASCO/TabColonCancerTreatmentPlanandSummaryposting.pdf).
Chemotherapy Treatment Summary
The transition from active treatment to post-treatment care is daunting. The Institute of Medicine has identified four essential components of survivorship care:
Prevention of recurrent and new cancers and other late effects;
Surveillance for cancer spread, recurrence, or second cancers, as well as assessment of medical and psychosocial late effects;
Intervention for such effects of cancer and its treatment as lymphedema and sexual dysfunction, pain, fatigue, psychological distress of both cancer survivors and caregivers, and concerns related to employment, insurance, and disability; and
Coordination between specialists and primary care providers to ensure all of the survivor's health needs are met.1
Even though the long-term effects of cancer treatment vary by cancer type, survivors share commonalities. For example, many can name the location or type of cancer, yet few survivors recall clinical details. A breast cancer survivor knows which side was treated, but is unlikely to recall the size of the tumor, whether there were lymph node metastases, the names of chemotherapy drugs, starting or ending dosages, pathology findings, toxicities or adverse effects, or why treatment was interrupted.
Recognizing cancer survivorship as a distinct phase of cancer care, the Institute of Medicine's (Washington, DC) Lost in Transition report set forth 10 recommendations to improve survivors' health and well-being. Recommendations 1 and 2 are particularly pertinent:
Recommendation 1. Health care providers, patient advocates, and other stakeholders should work to raise awareness of the needs of cancer survivors, establish cancer survivorship as a distinct phase of cancer care, and act to ensure the delivery of appropriate survivorship care.
Recommendation 2. Patients completing primary treatment should be provided with a comprehensive care summary and follow-up plan that is clearly and effectively explained. This survivorship care plan should be written by the principal provider(s) who coordinated oncology treatment. This service should be reimbursed by third-party health care payors.1
An ASCO-commissioned study conducted by Harvard University (Boston, Massachusetts) and RAND Health (Santa Monica, California) confirmed the Institute of Medicine's findings. Researchers working on the National Initiative on Cancer Care Quality learned that patients with breast cancer received 86% of recommended care, and colorectal patients received 78% of care overall.3 But there was also room for improvement.
The most surprising finding of the National Initiative on Cancer Care Quality study was that it was difficult for chart reviewers to locate the patient's chemotherapy doses and administrative notes in the medical oncology records because there was no standard place to find them. Furthermore, the oncologist's record typically did not document all of the patient's oncology treatments, pointing to the need for oncologists to compile an easily accessible treatment summary.4
The chemotherapy treatment summary is a succinct document prepared at the end of a chemotherapy treatment course. Essential elements of a treatment summary include identifying the treatment that was planned and delivered, how treatment was tolerated, the patient's response to treatment, and next steps for the patient's care. The treatment summary is not intended to take the place of more detailed communication between the oncologist and the patient or the oncologist and other treating physicians, but is intended to be a communication tool and a resource for the patient (available at http://www.asco.org/treatmentsummary). As a further example, Figure 2 shows a sample treatment summary for colon cancer.
Figure 2.
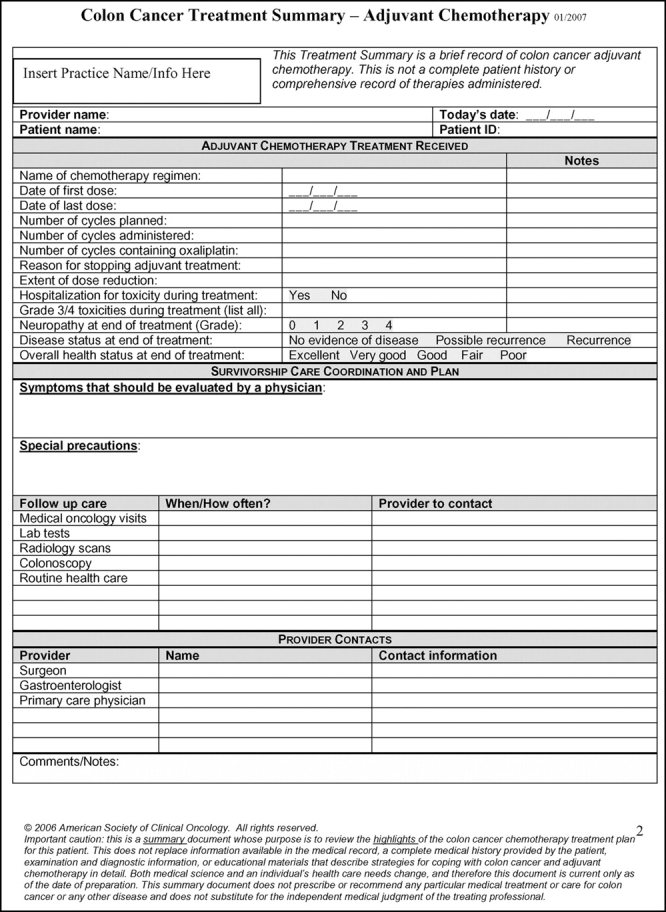
Sample treatment summary for colon cancer (available at www.plwc.org/ASCO/ArticleASCO/TabColonCancerTreatmentPlanandSummaryposting.pdf).
Patient Benefits From the Treatment Plan and Treatment Summary
The treatment plan and treatment summary are important tools toward care coordination and high-quality cancer care. The treatment summary is a synopsis of the actual treatment and is not intended to be a comprehensive report, but must include such information as serious complications and adverse effects of treatment. The treatment summary's most important function is to provide an outline of care that can be transmitted between providers or from provider to patient.
Patricia Ganz, MD, chair of ASCO's Electronic Health Record (EHR) Workgroup and a medical oncologist at the University of California at Los Angeles' Jonsson Comprehensive Cancer Center, has been instrumental in the development of ASCO's treatment plan and treatment summary. She recalls her own experience in opening a survivorship program and notes that the process of going through records of patients who have gone through treatment is very labor intensive, especially if those patients received multiple rounds of treatment. The treatment summary becomes most critical when a patient:
Completes curative treatment,
Faces treatment failure or a recurrence of cancer, and/or
Coordinates cancer treatment or survivorship care with multiple providers.
The treatment summary also is an essential tool when oncologists and other health care providers attempt to reconstruct medical records following a natural disaster, as demonstrated during the 2005 hurricane season. At that time, patients who had been dislocated from providers presented at new care facilities with little or no information about their stage of illness or treatment. Oncologists assuming care had tremendous difficulty taking on patients without such information and were forced to repeat testing, staging, and other services to ascertain appropriate next steps. The oncology treatment summary and its integration into an EHR provide an important opportunity to ensure continuity of care following natural or manmade disasters.
Promoting Industrywide Adoption of an Oncology Treatment Summary
As oncologists continue to assess ways to improve the quality of cancer care, they also seek answers about selection and implementation of electronic clinical information systems. ASCO has identified the EHR as an important vehicle for advancing quality and has established a series of initiatives that would advise and hasten adoption of EHRs among its members, as well as facilitate the adoption of treatment summaries. Working closely with members of its EHR Workgroup, ASCO hosted an EHR Roundtable in Washington, DC, on January 23-24, 2007.
The EHR Roundtable brought together senior thought leaders from government, academia, community-based oncology practices, and patient advocacy organizations. These 40 national thought leaders and practitioners invested 2 days exchanging firsthand knowledge of their experiences with EHR selection and implementation and developing recommendations to enable the effective exchange of health information between cancer patients and their caregivers.
Roundtable participants were asked to focus on the following objectives:
Achieve consensus and prioritize recommendations from key stakeholders about the functional elements needed to capture chemotherapy administration data in an EHR;
Identify interoperability challenges affecting development and implementation of EHRs for oncology; and
Challenge EHR vendors to incorporate functional elements of the ASCO-developed Chemotherapy Treatment Plan and Summary into EHR products.
Oncology Workflow Challenges
Roundtable Chair Robert Miller, MD, presented workflow in a medical oncology setting as a framework to engage participants to discuss their experiences with EHR planning, development, implementation, and process re-engineering. Table 1 presents the typical workflow, and Table 2 presents challenges that come with this complex workflow.
Table 1.
Typical Treatment Day Workflow for Infusion Visit
| Workflow | |
|---|---|
| 1. | Patient has blood drawn prior to or day of visit (generally a CBC; may include other laboratory tests as well). |
| 2. | Physician visits (generally includes history and physical as well as assessment of toxicity from prior therapy). |
| 3. | Physician orders chemotherapy treatment (may be single day or multiday therapy). |
| 4. | Patient proceeds to outpatient treatment room or center. |
| 5. | Drugs are mixed by RN, pharmacist or admixture technician. |
| 6. | Patient receives drug therapy (typically 15 minutes to > 6 hours); RN documents on flow sheet (includes drugs, doses, and patient response). |
| 7. | Patient is discharged home. |
Table 2.
Challenges of Oncology Workflow
| Challenges | Concerns |
|---|---|
| Treatment selection should be based on established guidelines and/or best practices. | 1. The oncologist's database for receiving information from pathology, labs, and other diagnostic studies may be incomplete. 2. There is no single authoritative source for verification of the drug regimen. 3. Patient assessment for eligibility for clinical trials may be incomplete. |
| Modification of treatment regimens should be based on accepted toxicity guidelines (National Cancer Institute's Common Terminology Criteria for Adverse Events). | 1. Access to guidelines may be limited. 2. Documentation of toxicity may be incomplete, inconsistent, and may not use standard terminology. |
| Physician drug ordering is usually done on an individual basis. | 1. This opens the risk of computational errors and drug interactions. |
| Patient handoff from physician to nurse or pharmacist increases the risk for errors. | 1. Handwriting can be misinterpreted. 2. Admixture errors occur (wrong drug, wrong dose, or wrong route). 3. Maximum drug dose and lifetime cumulative dose may be exceeded. 4. There can be infusion incompatibilities. |
| Drug administration errors may occur. | 1. Patients may be misidentified. 2. Documentation may be incomplete or inaccurate. 3. Charges may be missed. |
Abbreviation: EHR, electronic health record.
Functional and Clinical Elements in an Oncology EHR
A primary goal of the EHR Roundtable was to achieve consensus and prioritize recommendations from key stakeholders about the functional elements needed to capture chemotherapy administration data in an EHR. To maintain a focus on oncology, participants identified two defining facets of care provided by medical oncologists: the process of developing treatment plans and summaries for patients receiving chemotherapy, and the process by which patients undergo chemotherapy and their course of treatment in the chemotherapy chair. Presented with the following core elements for the Chemotherapy Treatment Plan and Treatment Summary, the group endorsed these as the essential elements for an oncology EHR:
Core elements of a chemotherapy treatment plan:
Diagnosis, including the cancer site, histology, and stage
Goals of therapy (may be specified by the type of template; eg, adjuvant chemotherapy plan)
Patient health status and comorbidities
Surgical history and notable pathology findings
Chemotherapy regimen and starting dosages
Duration of treatment and number of planned cycles
Major adverse effects of chemotherapy
Core elements of a chemotherapy treatment summary:
Chemotherapy treatment delivered, including number of cycles administered, duration, and extent of dose reduction
Reason treatment was stopped
Major toxicities and/or hospitalizations
Treatment response
Follow-up care and relevant providers
The Roundtable also recommended additional oncology-specific EHR core elements and functionality, such as the ability to generate a chemotherapy flow sheet and provide drug interaction alerts and dosing safety limits. A complete list of the EHR Roundtable's recommended core elements and functionality is presented in Table 3. Treatment plans and treatment summaries should be generated dynamically by the EHR. The expectation is, therefore, that the EHR software can extract data from relevant fields throughout the EHR to pull together a chemotherapy treatment plan and/or summary, and EHR products without this functionality should be viewed in a considerably less favorable light. The format and presentation of treatment plans and summaries need not be identical across different EHRs; however, the inclusion of these core elements is important and is what practitioners should come to recognize and expect as a standard in oncology EHRs.
Table 3.
Oncology EHR Core Functional Elements
| Element/Functionality | |
|---|---|
| Treatment plan core elements | Flow sheet: inclusive of all chemotherapy, |
| Demographics, including referring provider and PCP | non-chemotherapy medications, transfusions, tumor measurements, lab values |
| Diagnosis: ICD-9 or 10; possibly more clinically relevant system | |
| Flow sheet: physical findings, including tumor measurements, imaging, relevant procedures, nursing assessment* | |
| Stage | |
| AJCC for relevant diagnoses: tumor registry staging system for other diagnoses | |
| Oncology-specific review of systems | |
| Disease status at each course of therapy | Patient provided with copy of treatment plan and summary |
| Site/histology/pathology findings: menu-driven by disease | |
| Intent/goals of therapy: adjuvant/curative v palliative | Documentation of investigational drugs |
| Performance status | Capture date of death* |
| List of comorbid conditions expected to complicate chemotherapy, eg, hepatic insufficiency | Oncology-specific EHR functions |
| EHR-generated treatment plan | |
| Cancer surgical history | EHR-generated treatment summary |
| Chemotherapy/biotherapy regimen planned | Ability to update treatment summary |
| Body surface area and starting doses | EHR application to generate specific reports, eg, specific types of flow sheets |
| Duration of treatment and number of planned cycles | |
| Major toxicities associated with planned treatment | Mechanism to capture verbal orders* |
| Radiation therapy planned or previously delivered | Drug interaction alerts |
| Pain assessment and supportive care needs: advanced cancer | Basic safety limits for dosing |
| Body surface area safety monitoring | |
| Treatment on clinical trial | Lifetime cumulative chemotherapy dose |
| Sites of disease monitored: advanced cancer eligibility* | Clinical decision support, eg, guidelines or trial |
| Treatment summary core elements | |
| Patient demographics | Treatment preauthorization support* |
| Chemotherapy/biotherapy delivered: IV and oral | Drug inventory control* |
| Number of cycles planned and administered | Internal and external communications* |
| Duration: date of first and last dose | Import key external reports, eg, pathology, operative note, radiation |
| Extent of dose reduction | |
| Reason treatment stopped | Radiofrequency identification technology for patient/drugs given, eg, barcodes* |
| Major toxicities experienced | |
| Hospitalization required for toxicity | Open database with query capabilities* |
| Disease status at completion of treatment | Interoperability: health information exchange with labs, imaging centers, etc.* |
| Performance status at completion of treatment | |
| Coordination of follow-up care | Compliance safeguards |
| Provider contacts | Privacy and security safeguards in place |
| Other oncology-specific documentation | Disaster recovery plan in place |
Abbreviations: EHR, electronic health record; PCP, primary care physician; ICD-9, International Classification of Diseases, 9th Edition; AJCC, American Joint Committee on Cancer.
* Denotes elements characterized by Roundtable participants as desirable, not critical.
EHR vendor representatives were presented with the list of core elements and functionality as well as the treatment plan and treatment summary. The vendors agreed to take the Chemotherapy Treatment Plan and Summary back to their respective companies and determine whether they could incorporate ASCO's identified core elements into their software. Vendors meeting ASCO's selection criteria have been invited to participate in an EHR lab and demonstrate their application of the chemotherapy treatment plan and summary at ASCO's Annual Meeting in June 2007.
Next Steps
There is an urgent need for better tools to manage the highly complex clinical activities involved in treating cancer patients. The delivery of cancer care typically involves multiple physicians and other health professionals, as well as multiple sites of care. The National Initiative on Cancer Care Quality study highlighted the need for improved documentation to facilitate communication between caregivers and patients, and ultimately, to promote a higher quality of patient care. Patients on a course that includes surgery and radiation therapy benefit when the oncologist, surgeon, and radiation oncologist are in communication. “Snowbird” seniors who may see physicians in different parts of the country at different times of the year are at an advantage when this additional documentation occurs. For those patients who experience unanticipated separations from their health care team due to natural or other disasters, such a treatment record is critical. As the primary provider of chemotherapy, the medical oncologist plays a pivotal role in improving the communication between physicians, as well as between oncologists and patients, through the use of the treatment plan and treatment summary.
While the overall delivery of cancer care is distinctive, so are the data requirements for oncology EHRs. For example, stage of cancer is a core data element that is not always readily found in the cancer treatment record. An EHR for a patient with cancer must be able to integrate and keep up with multiple and evolving systems for cancer staging. In general, the body of knowledge around the science, technology, and treatment of cancer continues to increase at a rapid pace. Accordingly, there should be an expectation for continued innovation and refinement in oncology EHRs to adapt to these changes.
The Roundtable served to identify areas for future work by ASCO:
ASCO should continue the dialogue with members and EHR vendors to ensure that EHR products meet the requirements of this complex patient population.
ASCO should provide practical guidance and resources to address implementation and workflow issues for those practices who have already selected and purchased EHRs, as well as those considering a purchase in the near future.
The core functional elements for an oncology EHR should be further refined so that each of these elements are associated with a clear and standard definition, thereby facilitating adoption and integration into EHRs. ASCO should collaborate with other members of the cancer community as well as medical informatics and standards-developing organizations to pursue this effort.
ASCO should explore partnerships with the National Cancer Institute (NCI) and other groups who are working to enhance researchers' ability to access and use aggregated data collected through EHRs. The NCI, through the Cancer Biomedical Informatics Grid program, has made great strides in establishing an infrastructure for discussion around cancer-related data.
ASCO looks forward to continuing discussions with other stakeholders in the cancer community about the role of EHRs in advancing quality cancer care.
Appendix
Attendees included representatives from the following organizations:
American Society of Clinical Oncology; National Cancer Institute; Oncology Nursing Society; Administrators in Oncology/Hematology Assembly, Medical Group Management Asso ciation; Aetna; United Healthcare; Agency for Healthcare Research and Quality; Louisiana Health Care Review Inc; American Medical Informatics Association; American Cancer Society; Veterans' Administration Medical Center; American Academy of Family Physicians; National Coalition for Cancer Survivorship; EHR Vendor Association; IMPAC Medical Systems; Smart ID Works LLC; Eclypsis; Altos Solutions; MediNotes Corp; Intrinsiq; Emerging Meds; Epic Systems; DocComply; IKnowMed/US Oncology; e-MDs; Misys Healthcare Systems; NextGen; Varian.
References
- 1.Institute of Medicine Committee on Cancer Survivorship: From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC, National Academies Press, 2004, 1-7
- 2.National Initiative on Cancer Care Quality, American Society of Clinical Oncology, 2005
- 3.Malin JL, Schneider EC, Epstein AM, et al: Results of the National Initiative for Cancer Care Quality: How can we improve the quality of cancer care in the United States? J Clin Oncol 24:626-634, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Bailes JS: ASCO's groundbreaking study on cancer care quality: NICCQ. J Oncol Pract 2:48, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]


