Short abstract
The collaboration between oncologists and clinical pharmacists seems destined to grow.
Why do we need our own pharmacist? That's what Barbara McAneny, MD, wondered. As chief executive officer of New Mexico Oncology Hematology Consultants in Albuquerque, New Mexico, a practice that includes 10 medical oncologists at five sites, she wasn't sure such an addition could be justified. After all, oncology nurses can mix chemotherapy and the typical salary package of a clinical pharmacist generally exceeds six figures.1 So, to determine the possible impact a pharmacist might make on the practice, she conducted an informal, internal, time-and-motion study. A review of it led her to predict a “break-even” cost for the hire, she recalls. Still, it confirmed that a clinical pharmacist was a tangible idea—it wasn't going to take money away from the practice.
The group ran a local advertisement, listing some carefully researched job requirements, including specifying an oncology pharmacist. McAneny had high hopes for the new employee. She thought he might free up enough time from the nursing staff to preclude the need to hire another nurse. “I have to admit I was wrong,” she says—and very happily so. “He's far more valuable than just that,” she adds. In fact, McAneny now considers the practice's clinical pharmacist invaluable.
Inventory no longer piles up, and it is so well managed that the possibility of drugs doing a disappearing act now seems almost nonexistent. And the improvements in oversight don't end there. From adding updates on evidence-based protocols in the electronic medical record (EMR) to keeping precise track of medications, the clinical pharmacist has lightened the load by providing in-service education on guideline revisions and new drugs, and by implementing operational technology that makes that information available at the touch of a few keystrokes.
“He's so good at figuring out what we need,” she says. Under the pharmacist's purview, two pharmacy technicians provide patient refills and help in patient-assistance programs for securing free or low-cost medications for those who need them.
At a time in which treatment regimens seem subject to near-constant revision and in an era in which error prevention in medicine has been made a national priority, the collaboration between oncologists and clinical pharmacists seems destined to grow, says James G. Stevenson, PharmD, director of pharmacy services at the University of Michigan Health System and associate dean for clinical sciences at the College of Pharmacy. It benefits both oncologists and pharmacists, he suggests. The teamwork allows oncologists to focus on disease eradication, while pharmacists help keep patients informed about the multiple-drug usage that often becomes a routine part of life during treatment.
Figure u1.
The role of clinical pharmacist as health educator has grown. Now, many spend more time than ever in direct patient contact, explaining treatment goals, possible adverse effects, and safe and successful use of medications. In fact, patients with cancer often receive information about their chemotherapy regimen and supportive-therapy options from a clinical pharmacist, he observes. “With this higher patient contact, the field is drawing people into it who are more patient-oriented,” Stevenson notes. Because the impact on quality of life can be sudden and significant, the latter can be particularly important to patients, who want to live as normally as possible after diagnosis.
Pharmacists also have played a big part in helping ensure safer medication prescribing and dispensing practices at many hospitals, by assisting in the implementation of electronic order-entry systems that prevent the kind of medical errors highlighted nearly a decade ago, in the Institute of Medicine (IOM) report, “To Err is Human: Building a Safer Health System.” Practice guidelines have flourished since the publication of the IOM report, necessitating changes in information technology (IT) to keep up with the frequent growth and changes in such guides. In terms of the IT that helps prompt compliance with them, “a lot of pharmacists have been very active helping their hospitals to do this,” Stevenson says.
Beyond the benefits of IT improvement, inventory flow, and protocol expertise, there are other reasons an oncologist might want to bring a pharmacist on board. Clinical pharmacy is a field that has made pharmacogenics an increasingly important area of study, as research continues to show how individual genes may relate to drug metabolism and treatment response.2 And, in community practices, the inclusion of clinical pharmacists has been shown to improve outcomes in chronic disease, particularly when they are directly involved in patient care. In one study, for example, pharmacist involvement resulted in substantial reductions of glycemia measures in patients with type 2 diabetes.3
To be most cost saving and effective, a clinical pharmacist needs to have a strong relationship with all departments in an oncology practice, advises Steven D'Amato, RPh, BCOP, clinical pharmacy specialist at the Maine Center for Cancer Medicine in Scarborough, Maine. In many cases, a clinical pharmacist makes sense for the practice—dollars and cents, that is. “In private practices, there isn't room to lose a dollar,” he explains.
Keeping clinical regimens consistent with current guidelines, staying abreast of the operational technology required for the EMR, clinical education, oversight of research protocols, and providing financial oversight of most coding procedures and certain practice contracts are among the tasks now associated with clinical pharmacists in oncology practices. One report estimates that currently a majority of oncology practices that have eight or more oncologists on staff also have pharmacists and pharmacy technicians.4 From efficient management of drug inventory to effective use of the EMR, a clinical pharmacist can mean significant “charge capture” that keeps cost-saving high and unnecessary expenditure low, D'Amato explains. And data routinely can be caught and analyzed, too, when clinical pharmacists are well versed in medical informatics.
In the coming years, as the baby-boom population presumably increases the demand for cancer care, there will be even more need for screening and prevention of potential drug interactivity from both prescription and over-the-counter medications, a knowledge niche that may be filled by clinical pharmacists.5
However, for practices with fewer than five oncologists, a clinical pharmacist might not make as much financial sense, McAneny speculates. Clinical pharmacists typically do not bill directly for their services—although Medicare Part D medication therapy management opens the door to some direct billing.6
One other aspect of the job that may become more important in the next few years is supervision of pharmacy technicians, according to D'Amato. In the practice in which he works—four sites, 17 physicians—there are seven pharmacy technicians. Because of growing reliance on such staffers, states are now taking a hard look at the training and certification of them. “Nationally, this is starting to be addressed,” he observes. One result will likely be more participation by clinical pharmacists in educating and managing these technicians.
How do clinical pharmacists like working side by side with oncologists? Early anecdotal accounts in pharmacy journals peg it almost as a match made in health care heaven. Being a clinical pharmacist in a busy practice is demanding, but also very gratifying, affirms D'Amato. His profession often isn't just a critical member of the team, but also an integral part of the leadership, he notes. As such, clinical pharmacists help build practices, not just support them. “It's been challenging and fun,” he adds.
“This isn't replacing what the physician does,” reiterates David Chen, RPh, MBA, director of the section of home, ambulatory, and chronic care practitioners for the American Society of Health-System Pharmacists (ASHP) in Bethesda, Maryland. But with the aging demographic, the pharmacist is the right person to manage patients on complex drug regimens, he stresses. However, for the most part, pharmacists don't bill directly for services. That is predicted to change.
A primary goal of the ASHP is to work with the Centers for Medicare and Medicaid Services to achieve provider status under Part B, so that these clinical services—which now have been formally labeled as medication therapy management (MTM)—can be made more broadly available to patients, Chen says.
Pharmacists already can receive direct compensation for a small percent of Medicare Part D beneficiaries who need multiple drugs and have multiple disease states. And, in certain parts of the country, there are provisions for direct reimbursement by state-sanctioned programs for MTM in which the pharmacist may be a primary provider. These include states such Florida, Minnesota, and North Carolina. The latter is a state that has set aside appropriations for just such a purpose—a form of funding that may increase in the coming years, Chen suggests. But, because pharmacists are not currently listed as providers on the CMS Medicare Part B, it's currently left to the marketplace to determine the value range for MTM service codes.
However, three new entries—99605, 99606, 99607—in the 2008 coding manual of Current Procedural Terminology (CPT) now describe the patient-care services provided by pharmacists, and they create a viable mechanism to bill insurers, notes Dan Buffington, PharmD, MBA, president and chief executive officer of Clinical Pharmacology Services in Tampa, Florida. These codes were converted from temporary “Category III” codes to permanent “Category I” codes within 2 years of approval for placement in the CPT manual. “This is a reflection of the rapid uptake in the health care market based on both volume of use and value to insurers,” he says. However, receiving a nationally recognized “valuation” or range-of-service rates will likely take longer to establish, he cautions.
Clinching those recommended values is just a question of time, though, and not a difficult professional challenge, Buffington asserts. At CPT editorial panel hearings on coding changes, for example, oncologists have repeatedly expressed support for the emerging role of the pharmacist in patient care, he observes. In oncology, the addition of a pharmacist “is clearly associated with a strong return on investment from financial, liability, time efficiency and clinical perspectives,” he adds.
Though the codes have yet to be given an official monetary assignment, they are being utilized for billing—and paid for—by insurers in many practices across the country, he says. Typically, billing success begins with opening a dialogue between the practice and the payor to discern if MTM codes are covered and to discuss the anticipated fee schedule, he says. In most cases, the MTM codes are yielding payment rates similar to those paid for mid- to high level evaluation and management cognitive service codes utilized by their physician counterparts, according to Buffington.
Pharmacists are positioned to be more of a “consultative support role” to improve medication outcomes and support the prescriber in the management of patient, not a “primary care” role, he emphasizes. In fact, most states have enhanced their pharmacy and medical practice acts to reinforce the “collaborative” nature of pharmacist and physician relationships, Buffington says. “It is all about helping physicians to select, refine, and implement the most effective medication regimens.”
After all, pharmacists “take a 10,000 foot view of a patient's medications,” adds Buffington—a perspective that helps ensure safe medication usage and lighten the burden that can overwhelm practitioners in a busy practice
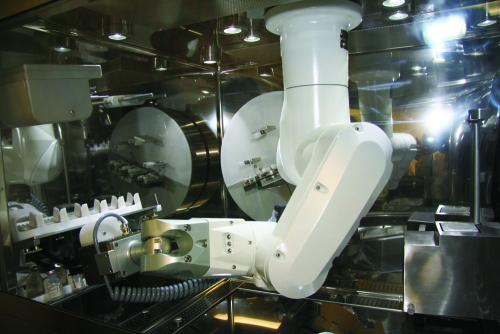
A totally automated mixing system for chemotherapy medications is making its debut at two American medical centers, with little fanfare but a lot of optimism that this new way of compounding will benefit cancer care.
Michael Sanborn, RPH, MS, corporate vice president at Baylor Health System in Dallas, Texas, said oncology has been the driving force behind a pilot program on the system that is scheduled to begin there in May. He thinks the approach will be “better for patients, better for pharmacy operations.”
Testing already is underway by the pharmacy staff at the University of Colorado Hospital, just outside Denver, Colorado, says Nancy Stolpman, PharmD, PhD, the pharmacy director. A robotic workbench prepares chemotherapy regimens in a new kind of error-preventing way. “The robot has numerous redundancies built in,” she says. A “picture library” contained in the technology, for example, validates that the active ingredient is correct; bar code technology ensures that the mixture is the right drug, for the right patient. The engineering involved also protects the sterility of the compound, and uses specific gravity calculations to determine that the dose is precisely accurate.
The technology also will help protect pharmacy staff who now may be exposed to cytotoxic agents during the course of manual mixing. “This robot is ideal because it pushes the exposure to zero for pharmacy personnel,” she says.
The system is designed to cut down on waste, to promote patient safety, to increase the volume of admixture that can be mechanically produced, and to improve dosing accuracy.
References
- 1.Ukens C: Pharmacist salaries: Drug Topics. http://drugtopics.modernmedicine.com/drugtopics/Independent+Pharmacy/Pay-dirt-Pharmacist-salaries-are-still-climbing-bu/ArticleStandard/Article/detail/408159?contextCategoryId=6880&searchString=Pay%20dirt
- 2.Grabinski JL: Pharmacogenomics of anticancer agents: Implications for clinical pharmacy practice. J Pharm Pract 20:246-251, 2007 [Google Scholar]
- 3.Clifford RM, Davis WA, Batty KT, Davis TME: Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes. Diabetes Care 28:771-776, 2005 [DOI] [PubMed] [Google Scholar]
- 4.News Report: Oncology practices recruit pharmacists for efficiency, savings. Am J Health Syst Pharm 63:1774-1775, 2006 [DOI] [PubMed] [Google Scholar]
- 5.De Lemos ML: Pharmacist's role in meeting the psychosocial needs of cancer patients using complementary therapy. Psychooncology 14:204-210, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Dole EJ, Murawski MM: Reimbursement for clinical services provided by pharmacists: What are we doing wrong? Am J Health Syst Pharm 64:104-106, 2007 [DOI] [PubMed] [Google Scholar]