Abstract
This study examines the variations in the use of inpatient care that can be explained by travel distance among patients with schizophrenia living in Taiwan. Data were drawn from the Psychiatric Inpatient Medical Claims Database. We used mediation analysis and multilevel analysis to identify associations. Travel distance did not significantly account for lower readmission rates after an index admission, but significantly explained the longer length of stay of an index admission by 9.3 days (P < 0.001, 85% of variation) between remote and non-remote regions. Policies are discussed aimed at reducing the impact of travel distance on rural mental health care through inter-disciplinary collaboration and telepsychiatry.
Keywords: Schizophrenia, Travel distance, Remote, Length of stay, Readmission
Introduction
In Taiwan, patients with schizophrenia are disadvantaged in their use of psychiatric services, because most psychiatrists practice in hospitals, and do not work as specialists in local communities. Thus, most outpatient care for schizophrenia is provided by hospitals with psychiatric outpatient departments, mostly in urban or suburban areas. Because of this centralization of services, and without a well-established community-based mental health care system, the distance to hospitals that can treat mental illnesses becomes crucial for patients with schizophrenia, especially for those who live in remote areas.
Although Taiwan’s Mental Health Act (1990) somewhat mitigates the negative effects of distance on access to psychiatric care, by stating that the health authority should establish medical networks to deliver psychiatric care based on demographics and the distribution of medical resources, the distribution of psychiatric health services remains uneven, partly for geographical reasons. The high mountains in the center of the island cover almost two-thirds of the country, separating the east coast from the more urbanized west.
The literature has documented differences in rural and urban patients’ use of medical care. For example, Lambert and Agger (1995) found that beneficiaries of the Aid to Families with Dependent Children (AFDC) Medicaid program in rural Maine were less likely to use psychiatric care, including both outpatient visits and hospitalizations, than were their urban counterparts. Nemet and Bailey (2000) confirmed that distance to a provider was associated with less frequent use of medical services among the rural elderly. They concluded that variations in health service utilization could be explained by whether or not a provider was within the activity zone of an elderly patient. Haynes et al. (1999) found that, at the village level, the distance to the nearest hospital available for a census area accounted for the use of psychiatric care, geriatric care and acute care, independent of the demand and supply of medical services.
One of the implications of rural–urban differences in the use of health care is the distance effect exerted on health service utilization. Mental health researchers have long considered the importance of distance on psychiatric service use (Shannon et al. 1986). Systemic analyses regarding the relationship between distance and the use of mental health care can be traced back to the mid nineteenth century, when Edward Jarvis (1866) identified inverse associations between home-to-hospital distance and the rates of admission to Oneida County Hospital of New York and the Kentucky Lunatic Asylum in Fayette County. He claimed that people living near psychiatric hospitals send more patients there for admission than do those living far away (Jarvis’s law). In the early twentieth century, researchers focused more on the epidemiology of mental disorders—i.e. investigating their distribution and etiology, rather than paying much attention to distance effects on psychiatric care use. Faris and Dunham (1939), examining the geographic locations of patients prior to admission to public and private hospitals in Chicago, found that a high proportion of people with severe mental disorders, especially those with psychosis, aggregated around the city center. The study also revealed urban–rural differences in the prevalence of insanity, and high admission rates to psychiatric hospitals among people residing near the city center. Jarvis’s law has been identified in numerous studies since the mid-twentieth century. For example, in Denmark, they discovered higher first admission rates among people living in areas close to psychiatric facilities than among those living more distant from them (Bille 1963). In Zambia, Haworth (1980) found a significant negative correlation between living distance from psychiatric hospitals and admission rates. Other investigators, however, have argued that the severity of mental disorders, the referral patterns of practice physicians, and the availability of other mental health services might account for the observed association between distance and hospitalizations at psychiatric facilities (Norris 1959). In a study of first admissions to Connecticut state psychiatric hospitals, the negative association between distance and first psychiatric hospitalizations remained evident even when population size, disease type (Sohler and Thompson 1970) and other parameters of availability (Sohler 1970) were controlled. Blumberg (1965) examined admissions to California state hospitals and found that distance to the nearest psychiatric facility was the most important predictor of hospitalization among all county-specific variables. On the other hand, in their study of Western Australia, Stampfer et al. (1984) found that the impact of distance on hospitalizations only was significant for people with less severe mental illnesses, and emphasized the concept of threshold distance, in that distance itself no longer determines admissions to psychiatric facilities beyond a certain extent of distance.
The relationship between home-to-hospital distance and admission rates of psychiatric facilities has prompted investigators to assess the relationship between distance and length of stay in psychiatric hospitals. Sohler and Clapis (1972) evaluated Jarvis’s law by incorporating length of stay into their analyses. They found that longer distances from psychiatric facilities were associated with longer lengths of stay. Miclutia et al. (2007) posited that patients living in rural regions find it difficult to access psychiatric care. When they finally are admitted to hospital, they may stay longer because prompt readmission may not be possible if a patient relapses. Smith et al. (2007) evaluated over 4000 hospitalizations to the Ontario Provincial Asylum in the city of Hamilton, between 1876 and 1902, and identified both a negative relationship between distance from the asylum and the likelihood of being readmitted to the same facility; and a positive association between length of stay and distance from a psychiatric institution. That study also confirmed Jarvis’s law.
Studies addressing the association between distance and length of hospital stay have been conducted in fields other than psychiatry. For example, Waddell and Dibley (1986) found that aboriginal children and children in the Northern Territory of Australia stayed longer in hospitals than did non-aboriginal children and those in Western Australia, implying that the remoteness of homes influences length of hospitalization. Moreover, in a retrospective study in a Turkish military hospital (Teke et al. 2004), patients living outside Ankara tended to have more hospital days and more inappropriate admissions than did patients from Ankara.
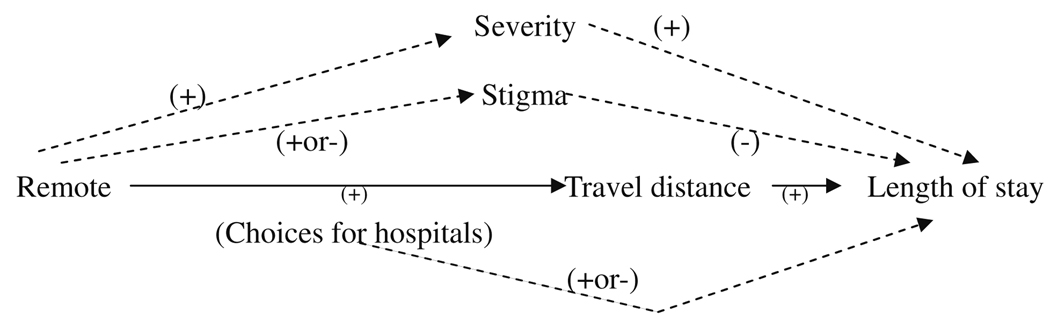
We propose a conceptual model to account for the influential causal role of residential remoteness in the use of psychiatric care (Fig. 1). Many factors account for the discrepancy that exists in the use of psychiatric services between those living in remote versus non-remote regions, such as travel distance, perceived stigma, health status, and income, all of which can be mediators in this causal pathway.
Fig. 1.
Conceptual model of mediation analysis, (use length of stay as an example) Note: Solid lines represent the main hypothesis we tested and dotted lines represent the relationships mentioned in prior research
As an example, consider perceived stigma as a mediator. Rost et al. (1993) found that rural residents with depression were more likely to express more negative views (i.e. stigma) with respect to seeking professional care than urban residents. In contrast, Phillips et al. (2002) found that people with schizophrenia living in more urbanized areas of China report a greater influence of stigma in their lives; they feel socially inferior because of their difficulty meeting the minimal adult standards expected of city dwellers. Because stigma can discourage the use of psychiatric care (e.g. Rost et al. 1993), rural residency influences the use of health care through its contextual effect on perceived stigma.
Disease severity is another potential mediator. Due to difficulties finding providers, many patients in rural areas may resist seeing a doctor until they are severely sick (Goldsmith et al. 1997), even though a lower prevalence and incidence of psychiatric disorders are noted in rural versus urban areas (Peen et al. 2007). Rural residency, therefore, influences the use of psychiatric care through its contextual effects on the occurrence and severity of psychiatric illness.
Prior investigators rarely have claimed that travel distance is a clear intermediate factor between rural residency and the use of psychiatric care. Thus, in this study, we emphasized distance as a mediator of rural–urban differences in the use of psychiatric services. Moreover, we focused on the use of psychiatric inpatient care among patients with schizophrenia, because the majority of psychiatric inpatient care is used by patients with schizophrenia; consequently, patterns in care seeking behavior among these patients represent access to psychiatric care in Taiwan. We specifically asked “with respect to differences between remote and non-remote areas in Taiwan, to what extent does travel distance account for (1) length of stay during an index hospitalization, and (2) readmissions after an index admission among patients with schizophrenia?” We formulated two hypotheses: (1) home-to-hospital travel distance explains the longer hospitalization stays observed during index admissions among Taiwanese patients with schizophrenia; and (2) home-to-hospital travel distance explains the lower readmission rates observed after an index admission among Taiwanese patients with schizophrenia.
The overall aim of our study was to supplement the literature pertaining to how home-to-hospital travel distance explains differences in the use of psychiatric inpatient care among patients with schizophrenia across remote and non-remote regions. The secondary aim was to describe the policy implications of the renovation of psychiatric care in Taiwan and countries with centralized psychiatric care. We achieved these goals using a nationwide National Health Insurance claims database and analyzing the data by means of mediation analysis (Baron and Kenny 1986).
Methods
Data and Study Population
We merged data from several sources. The Psychiatric Inpatient Medical Claims Database of Taiwan consisted of all inpatient claims for insured patients who had been admitted at least once to a psychiatric ward, with a psychiatric diagnosis. The Registry of Contracted Medical Facilities and Beds provided information on hospitals, and allowed us to calculate a town’s medical supply. The Insurance Enrollment File contained individual information on residence and payroll information. Finally, town-level variables were derived from the census.
The study cohort consisted of patients who were admitted to psychiatric wards with schizophrenia—defined by the International Classification of Diseases, 9th Revision Clinical Modification Codes (ICD-9-CM, 295)—as their principal diagnosis, between January 1, 1996 and December 31, 2000. The study unit was an index admission, defined as the first hospitalization during this five-year period. We included patients from 15 to 85 years of age. Seriously-ill patients tended to live near the hospitals that could treat mental illness because they tended to use more psychiatric services, and stayed longer in hospitals (McClellan et al. 1994). We therefore excluded the residents of Yuli town (697 observations were deleted), where many patients with severe mental disorders resided, because Taiwan’s largest psychiatric hospital was located there. We also deleted observations with incomplete information. A total of 28,839 patients were included in the analysis (9% attrition of the sample).
Dependent Variables
The study investigated two dependent variables: readmission after an index admission and length of stay of the index admission. We identified readmissions within 30 days, 90 days, and 1 year after the discharge of an index admission. Length of stay was calculated as a number of bed days spent in hospitals during the index admission.
Remote Area, Distance and Factors Related to Remoteness
Remoteness is an aggregate factor, consisting of diminished availability of medical care, longer distance to a provider, smaller population, and poverty (Murray et al. 2004; Wakerman 2004). Since no single standardized method can define remoteness, we adopted the governmental definition of remoteness, which classifies 44% of towns (164 of 369) as being in remote regions based on location, geography, and medical availability, including isolated islands, mountainous regions, rural areas, and the east coast (Research, Development and Evaluation Commission, Executive Yuan 2002). The governmental definition for remote towns also has policy implications. Therefore, the remoteness in our analysis was a binary variable—whether or not a patient lived in a remote area. Thus, it was crucial to test the governmental definition of remoteness for meaningfulness. We, therefore, performed a factor analysis to validate this operational definition.
Other variables representing the components of remoteness were used in the factor analysis. First, we measured two types of distance. At the town level, we computed minimum distance to a town with inpatient capacity for mental care (i.e. towns with at least one bed for psychiatric patients). At the patient level, we measured travel distance from the town where a patient lived, and the town where the hospital admission occurred. It was calculated as the miles of a straight line between the centers of the two towns, using longitudinal and latitudinal information. The measure of travel distance should have revealed an actual route for a patient to get to a hospital from home. Because a measurement tool for actual route was unavailable, a straight-line distance is the currently available (albeit imperfect) measurement of travel distance.
Moreover, several variables represented availability of medical facilities in towns, including the number of hospitals, beds, psychiatric hospitals, and beds for psychiatric patients. These variables were computed as numbers per thousand people.
Covariates
The covariates were gender, age, individual income level, co-morbidity, and time. Information on payroll status was used to represent an individual’s income level, since the premiums were collected based on the insured’s salary. We used the Charlson Index (Charlson et al. 1994) to represent a patient’s co-morbidity. The co-morbidity could reflect the severity of the patient’s physical condition. The Charlson Index was derived from 12 co-morbid diseases: previous myocardial infarction, peripheral vascular disease, dementia, pulmonary disease, rheumatologic disease, mild liver disease, mild to moderate diabetes, diabetes with chronic complications, renal disease, any malignancy, moderate to severe liver disease, and metastatic solid tumor. We totaled the number of diseases and dichotomized them to indicate whether a patient had a co-morbid physical illness due to a right-skewed distribution. To adjust for time trends, we also created year dummies based on dates of index admissions.
Statistical Analysis
Since remoteness has multidimensional aspects, differences in medical care use between remote and non-remote areas arise from multiple factors, such as variations in disease severity, medical availability, and travel distance. To identify the differences between remote and non-remote regions that were only related to travel distance, we adopted a statistical technique—mediation analysis (Baron and Kenny 1986)—which employs the following logic. Residents of remote towns chose providers according to their own preferences and the types of medical care available in their towns. Then, they traveled to hospitals for care. Travel distance was in a causal pathway between remoteness and the dependent variables (Fig. 1). Mediation analysis could determine the effect of the mediating factor of interest (i.e. travel distance) by examining changes in point estimates after we controlled for travel distance. We expected an upward change for the point estimate of remoteness on readmissions but a downward change for length of stay estimates, once we controlled for travel distance. We quantified the changes, which suggested the variations between remote and non-remote regions that can be explained by travel distance. The key concept of mediation analysis is to separate the variations that are related to travel distance in the causal pathway between the remoteness and the health care use. We did not necessarily add other mediators, such as perceived stigma and severity of the disease, to the model if they did not influence travel distance. Due to data limitation, we did not have those variables.
The modeling strategy was as follows. First, we set up a basic model—examining the coefficient of remoteness adjusted for age, gender, payroll status, co-morbidity, and the time trend. Since a catastrophic earthquake happened during the study period, we created earthquake-region dummies to adjust for the disaster impact. Then, we put travel distance variables in the model. We tested the non-linearity of travel distance with the dependent variables by adopting a quadratic form of distance. To interpret the results, we predicted readmission probability and length of stay after regression analyses by the method proposed in the literature (Newhouse 1993).
We also adopted multilevel analysis to consider clustering (Subramanian 2004) among patients living in the same town. For the utilization hypothesis, the dependent variable was “readmission”: a binary variable. Logistic regressions were adopted for readmissions within 30 days, 90 days, and one year. For the length of stay hypothesis, the dependent variable was “bed days”—a positive integer skewed to the right. Both over-dispersed Poisson and negative binomial regressions were better options than a linear or Poisson regression for modeling our data (Gardner et al. 1995). The over-dispersed Poisson (i.e., extra-Poisson) regression fit our data better than the negative binomial regression. Therefore, we presented results of an over-dispersed Poisson regression. We used the software of STATA 8.2 for descriptive analyses and MLwin 2.02 for multilevel analyses.
Empirical Model Specification
The following shows multilevel random intercept models (i: level-1 unit, individual; j: level-2 unit, town).
- Readmission Hypothesis (logistic regression)
- Length of stay (LOS) hypothesis (extra-Poisson regression):
πij represents an expected value of a dependent variable conditional on a patient’s characteristics and a random effect of the town where a patient lived. U0j represents a town-level random error, which was assumed to be normally distributed with a variance of Ωu. Age and payroll variables are ordinal and modeled as categorical.
Earthquake is the binary variable that indicates whether a town was closer to the epicenter. Besides, “pre” and “post” represent whether the date of an index admission was before and after the earthquake respectively. These are random-intercept models. α indicates the patient-level (level-1) dispersion parameter for the variance of an extra-Poisson distribution.
Results
Sample Characteristics (Table 1)
Table 1.
Descriptive statistics of patients with schizophrenia
| Variable | Remote | Non-remote | Test statisticsd |
P | Overall % |
||
|---|---|---|---|---|---|---|---|
| % | N | % | N | ||||
| Sex (male)a | 61 | 2,241 | 56 | 14,223 | 35.84 | <0.001 | 57 |
| Having co-morbidity | 2 | 70 | 2 | 493 | 0.02 | 0.88 | 2 |
| Medical centera | 14 | 521 | 22 | 5,673 | 125.13 | <0.001 | 21 |
| Public hospitala | 60 | 2,179 | 61 | 15,437 | 2.04 | 0.15 | 61 |
| Teaching hospitala | 74 | 2,704 | 83 | 21,029 | 187.39 | <0.001 | 82 |
| Psychiatric hospitala | 37 | 1,347 | 43 | 10,829 | 47.23 | <0.001 | 42 |
| Hospital with large psychiatric capacitya,b |
39 | 1,436 | 40 | 10,022 | 0.18 | 0.67 | 40 |
| Mean | SD | Mean | SD | Overall Mean (SD) |
|||
| Age | 35.1 | 12.0 | 35.3 | 11.9 | 1.01 | 0.31 | 35.3 (11.9) |
| Travel distance (mile) | 26 | 31 | 15 | 28 | −22.12 | <0.001 | 16 (29) |
| Nc | 3,644 (13%) | 25,195 (87%) | 28,839 | ||||
Sex and hospital characteristics were dummies, equal to one if an option was chosen
Hospitals with large psychiatric capacity: psychiatric beds >150
N represented the number of patients with non-missing values
Test statistics, comparing remote and non-remote regions, were Chi-square statistics with df = 1 for all variables, except age and travel distance, for which t statistics were used
Of the patients, 57% were male. The mean age was 35 years old. Only 2% of them had physical co-morbidity. A total of 21% used medical centers, while the remaining chose regional or local hospitals. The majority used public hospitals (61%) or teaching hospitals (82%). A total of 13% of patients with schizophrenia lived in remote towns—the same proportion as the general population. Compared to patients living in non-remote towns, patients with schizophrenia living in remote regions were more likely to be male (61% vs. 56%), less likely to use medical centers (14% vs. 22%), teaching hospitals (74% vs. 83%), or psychiatric hospitals (37% vs. 43%). On average, they traveled further (26 miles vs. 15 miles). No significant differences in age, having a co-morbidity, using public hospitals, and hospitals with a large capacity for psychiatric care were observed.
Validation of Remoteness (Town-level Characteristics, Table Not Shown)
Compared to non-remote towns, remote towns had smaller populations (18,112 vs. 93,581), lower average income (US $13,891 vs. US $15,998), fewer beds (1.75 vs. 6.35 per 1,000 people), and fewer hospitals (0.76 vs. 1.28 per 1,000 people). On average, they were farther away from the town with inpatient capacity for mental care (14.7 vs. 3.1 miles). The factor analysis revealed that smaller population, lower income, and less medical availability (number of beds and hospitals) was in the same category as remoteness, validating the definition of remote towns.
The Extent to Which Travel Distance Accounted for the Use of Inpatient Care for Schizophrenia (Table 2)
Table 2.
Distance in relation to readmission and length of stay for patients with schizophrenia
| Dependent variable: Conditioning on distance or not |
Remote | Non-remote | Gapa | Change in gapb |
|---|---|---|---|---|
| Predicted probability (%) | ||||
| 30-day readmission | ||||
| Without conditioning on distance | 12.68 | 12.15 | 0.53 | −0.04 |
| Conditioning on distance | 12.72 | 12.15 | 0.57 | |
| 90-day readmission | ||||
| Without conditioning on distance | 19.86 | 19.95 | −0.10 | −0.29 |
| Conditioning on distance | 20.12 | 19.93 | 0.19 | |
| One-year readmission | ||||
| Without conditioning on distance | 36.97 | 38.23 | −1.25 | −0.32 |
| Conditioning on distance | 37.27 | 38.2 | −0.93 | |
| Predicted bed days | ||||
| Length of stay | ||||
| Without conditioning on distance | 95.1 | 84.1 | 11.0** | 9.3*** |
| Conditioning on distance | 86 | 84.3 | 1.7 |
Gap: remote vs. non-remote
Change in gap: without conditioning on distance vs. conditioning on distance
P < 0.01;
P < 0.001. P values were computed by Wald tests
Compared to patients living in non-remote towns, patients from remote regions tended to be readmitted within 30 days (12.68% vs. 12.15%, gap: 0.53%) but were less likely to be readmitted within 90 days and one year after index admissions (gap: −0.10% and −1.25% respectively). Nonetheless, the estimates were not significant. Further, if we compared the gap (remote vs. non-remote) without conditioning on distance to that conditioning on distance, the difference revealed the extent to which travel distance accounted for variations in readmissions between remote and remote regions. On average, travel distance explained 0.04% lower readmission within 30 days after the discharge of index admissions for patients with schizophrenia across remote and non-remote regions. The changes in gaps were larger for 90-day (−0.29%) and one-year readmissions (−0.32%). These estimates, however, were not significant.
For the association of distance with length of stay of an index admission, patients living in remote regions stayed 11 days longer than patients living in non-remote areas (95.1 days vs. 84.1 days). If we controlled for travel distance, the difference fell to 1.7 days. The change difference was 9.3 days (9.3/11 = 85%)—the estimate that indicated the variations in length of stay explained by travel distance, across remote and non-remote towns. The estimate was significant at the 0.001 level.
Other Factors Associated with Readmission and Length of Stay (Table 3)
Table 3.
Multilevel regressions for readmission and length of stay among patients with schizophrenia
| Model information | Outcome |
|||
|---|---|---|---|---|
| 30-day readmission |
90-day readmission |
1-year readmission |
Length of stay | |
| Level-1: patient (N) | 28,839 | 28,839 | 28,839 | 28,839 |
| Level-2: town (N) | 360 | 360 | 360 | 360 |
| Cluster size (Range) | 1–691 | 1–691 | 1–691 | 1–691 |
| Regression | Logit | Logit | Logit | Extra-Poisson |
| Fixed part estimate | OR (95% C·I.) | OR (95% C·I.) | OR (95% C·I.) | Ratio (95% C·I.) |
| Remote | 1.05(0.93–1.18) | 0.99(0.90–1.09) | 0.95(0.88–1.02) | 1.13**(1.05–1.22) |
| Gender (male vs. female) | 1.20***(1.12–1.29) | 1.17***(1.10–1.24) | 1.12***(1.07–1.18) | 1.20***(1.15–1.25) |
| Age 15–30 | (ref.) | (ref.) | (ref.) | (ref.) |
| Age 30–45 | 0.94(0.86–1.01) | 0.89***(0.83–0.94) | 0.87***(0.83–0.92) | 1.49***(1.42–1.56) |
| Age 45–60 | 0.94(0.84–1.06) | 0.85***(0.77–0.93) | 0.76***(0.70–0.82) | 1.74***(1.64–1.85) |
| Age 60–75 | 0.68***(0.54–0.84) | 0.62***(0.52–0.74) | 0.54***(0.47–0.63) | 1.46***(1.31–1.63) |
| Age 75–85 | 0.51*(0.27–0.94) | 0.57*(0.36–0.91) | 0.41***(0.27–0.60) | 1.21(0.90–1.61) |
| Payroll group 1 | (ref.) | (ref.) | (ref.) | (ref.) |
| Payroll group 2 | 0.76***(0.66–0.87) | 0.79***(0.71–0.89) | 0.80***(0.73–0.87) | 0.70***(0.64–0.76) |
| Payroll group 3 | 0.74***(0.67–0.80) | 0.78***(0.73–0.84) | 0.80***(0.76–0.85) | 0.69***(0.66–0.72) |
| Payroll group 4 | 0.48***(0.35–0.67) | 0.54***(0.42–0.69) | 0.48***(0.39–0.58) | 0.33***(0.27–0.42) |
| Having co-morbidity | 0.95(0.73–1.25) | 0.87(0.69–1.09) | 0.87(0.72–1.04) | 0.57***(0.47–0.69) |
| Region closer to the earthquake · Pre |
0.84**(0.75–0.94) | 0.85***(0.78–0.92) | 0.92*(0.86–0.99) | 0.69***(0.63–0.74) |
| Region closer to the earthquake · Post |
1.27**(1.09–1.48) | 1.11(0.98–1.26) | 1.04(0.93–1.15) | 1.81***(1.64–2.00) |
| Year 1996 | (ref.) | (ref.) | (ref.) | (ref.) |
| Year 1997 | 0.94(0.84–1.04) | 0.89**(0.82–0.97) | 0.82***(0.77–0.88) | 0.89***(0.85–0.94) |
| Year 1998 | 0.99(0.89–1.11) | 0.91*(0.83–1.00) | 0.82***(0.76–0.88) | 0.73***(0.69–0.77) |
| Year 1999 | 0.95(0.85–1.06) | 0.92(0.84–1.01) | 0.79***(0.74–0.86) | 0.59***(0.56–0.63) |
| Year 2000 | 0.84**(0.74–0.95) | 0.83***(0.75–0.91) | 0.76***(0.70–0.82) | 0.38***(0.35–0.41) |
| Random part estimate | Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) |
| Level-2 variance | 0.047***(0.012) | 0.016***(0.006) | 0.012***(0.004) | 0.045***(0.007) |
| Level-1 variance: Var(Readmissonij|πij) |
πij · (1−πij) | πij · (1−πij) | πij · (1−πij) | α · πij |
| α = 245.60***(2.06) | ||||
P < 0.05;
P < 0.01;
P < 0.001;
πij: expected values conditional on individual characteristics and random effects of towns
C·I.: Confidence interval; SE: Standard error; OR: Odds ratio; ref.: Reference group
Table 3 shows estimates of the multilevel models we specified in the hypotheses without conditioning on the distance. Men were more likely than women to be readmitted, especially within 30 days after discharge of index admissions (odds ratio [OR]: 1.20, 95% confidence interval [95% CI]: 1.12–1.29). They stayed longer in hospitals (ratio: 1.20, 95% CI: 1.15–1.25). Older patients were less likely to be readmitted. Middle-aged patients (45–60) stayed in hospitals longer than did people in other age groups. Patients with larger salaries were less likely to be readmitted and to have shorter stays. The presence of physical co-morbidity was not associated with readmission but it was associated with a shorter length of stay (ratio: 0.57, 95% CI: 0.47–0.69). By comparing the estimates of the earthquake regions (closer to vs. further from the epicenter) before and after the earthquake (difference-in-difference), the catastrophe increased the likelihood of readmissions, and length of stay. Finally, hospitalization days of index admissions declined on average. Town-level variances were all significant, indicating strong clustering effects among patients living in the same town. We compared the results of multilevel analyses to those of single-level regressions, and found that the point estimates were similar but that the standard errors increased.
Discussion
In this study, we found that, among patients with schizophrenia, home-to-hospital travel distance does not significantly account for differences in readmission rates after an index admission. However, travel distance does explain most of the discrepancy in the length of hospital stay during an index admission between individuals residing in remote versus non-remote regions.
Our study was similar to prior research in some respects. Like the study conducted by Sohler and Clapis (1972), we examined the relationship between home-to-hospital distance and length of stay. Moreover, we measured linear distance at the town level, consistent with most previous studies (Shannon et al. 1986). On the other hand, our study differed from prior research in several aspects. For example, Jarvis (1866) simply compared admission rates according to successive distance. However, he ignored other contextual variables that might explain the association, like the availability of county-level psychiatric resources and socioeconomic variables. Bille’s Danish study (1963) adopted similar comparisons, but it used first admission rates as the main outcome indicator. Sohler’s Connecticut study used first admission rate (Sohler 1970; Sohler and Thompson 1970) and length of stay (Sohler and Clapis 1972) as the main outcome variables and controlled for others, including age, race, disease type, population size, poverty level (Sohler and Thompson 1970) and town-level availability factors (Sohler 1970) by means of stratification and standardization. Our study not only compared remote and non-remote differences in the use of psychiatric services, it also adopted mediation analyses to tease out the total impact of distance on these differences. Second, we chose readmission after an index admission (defined as a first admission to a psychiatric ward during the study period) as one of the main outcome variables, rather than admission or first admission, because we defined our study population differently. Third, we adopted multilevel analyses, in that we were able to identify both town-level and individual-level variations as accounting for the associations in which we were interested. Thus, contextual effects at the town level can be taken into consideration by modeling the random part of the regression models. A multilevel approach to assessing distance relative to use of mental health care can also be seen in Smith et al.’s study (2007) in Canada. Fourth, we used regression analysis, which allowed us to efficiently adjust for covariates. In this way, we adjusted for age, gender, income status, time trend, and a major earthquake.
In our study, Jarvis’s law did not hold true for the relationship between home-to-hospital distance and the rate of readmission. We propose possible explanations for the non-significant mediating effects of travel distance on readmission among patients with schizophrenia. The association with a binary outcome variable (i.e. readmission) was vulnerable to measurement errors related to place of residency. Approximately 15% to 20% of the citizens were absent from the residency register for various reasons (National Policy Foundation 2002). One scenario is that if patients with schizophrenia who had registered their residency in rural communities moved to urban areas for better access to mental care, without notifying the administrative agency that they had changed their address, this would cause differential misclassification of residency information, leading to upward bias. However, we do not know what percentage of misclassification of residency was due to looking for better access to mental care within our study population. Non-differential misclassification also was possible, resulting in bias toward the null. Both types of bias would tend to underestimate the association between distance and inpatient utilization. Moreover, contextual differences between Taiwan and Western nations, including culture and geographic area, might account for the different findings we identified versus other investigators.
Our results suggest that home-to-hospital travel distance exerts a strongly positive mediation effect upon the relationship between remoteness and hospitalization days. Misclassification errors pertaining to residency also might influence the length of stay analysis. Any differential misclassification that caused an upward bias would offset the effects of any non-differential classification that moved the association toward the null, if the two types of measurement error were equal. However, we did not have this information. In our study, Jarvis’s law holds for the association between distance and hospitalization days for patients with schizophrenia. From an economic perspective, the individual utility of a day spent in hospital among patients who travel farther increases to compensate for large upfront time costs related to home-to-hospital travel.
Our study has several strengths. First, we used mediation analysis to tease out any differences in the use of psychiatric inpatient care between remote and non-remote regions that are associated with travel distance. Second, we adopted a multilevel approach that allowed us to consider contextual effects. Third, we used a large nationwide database, which gave us enough statistical power to detect differences, and enhanced the generalizability of our results, at least within Taiwan if not beyond.
There were, however, some limitations. Aside from the measurement errors mentioned before, straight-line distance, which should reflect time and transportation costs, is an imperfect measure of traveling costs. For instance, some people living in the mountains may have had a short straight-line distance to a provider, but they incurred huge time costs due to the topography and limited transportation options. Jordan et al. (2004) compared remoteness in terms of travel time and straight-line distance. They found that travel time is a more accurate indicator of remoteness than straight-line distance. We, therefore, suggest that future studies adopt travel time, if available, instead of travel distance as an estimator of access to health care. Finally, our data lacked certain important variables like disease severity, which might confound the mediation effects of travel distance. Thus, we call for future inpatient claims databases to contain severity measures for schizophrenia.
The mediation relationship between travel distance to hospital and length of stay among patients with schizophrenia taps into crucial issues about the relative lack of deinstitutionalization and the absence of adequate community-based psychiatric services in Taiwan. For example, between 1995 and 2006, the number of acute psychiatric beds kept increasing, from 2,600 to 6,000 beds, and the number of chronic psychiatric beds increased from 11,000 to 13,000 (Department of Health 2006). The number of psychiatric hospitals increased, as well. Following the main era of mental health care institutionalization—prior to the mid 1980’s when several larger psychiatric hospitals were built and many public or private hospitals expanded their medical services to include psychiatric inpatient care—the Taiwanese government began to promote community mental health care. To achieve this, they classified several catchment areas, their primary objective being to deliver psychiatric services in a more efficient way. Nonetheless, there still are few psychiatric clinics and centers that provide prevention, treatment or rehabilitation outside major urban centers (Wang 1997).
Moreover, during the 1990s, the Taiwanese government became committed to reducing disparities in access to medical care across the island. The National Health Insurance Program, which was implemented in 1995, has narrowed the financial gap that used to influence the use of medical services (Cheng and Chiang 1997). Nonetheless, without eliminating disparities in medical resource access, any gains in financial equity are likely to be offset by the inefficient use of medical care, such as longer stays in hospital resulting from greater travel costs. This is even more conspicuous for patients with schizophrenia, who are the most in need of psychiatric inpatient care in Taiwan. In 2001, the number of hospitalization days for schizophrenia totaled four million, exceeding any other physical or mental disease in Taiwan (Bureau of National Health Insurance 2003). The majority of Taiwan’s psychiatric beds were occupied by patients with schizophrenia. Between 1995 and 2000, the average length of hospital stay among patients admitted to acute psychiatric wards was about 36 days. For patients admitted to chronic psychiatric wards, the mean number of hospitalization days for the whole nation ranged from a high of 709 days to a low of 118 days over the same period (Department of Health 2006). If we could reduce the length of stay by removing barriers to physical access to mental health care in Taiwan, we likely would substantially reduce the number of days spent in the hospital for mental health conditions, and save a significant proportion of the financial and other health service resources that currently are spent on such hospitalizations.
To compensate for the scarcity of mental health care that exists in rural areas, some authors have recommended extending the supply of mental health care to non-healthcare professionals, like religious staff, schoolteachers, police, and/or government officials (Heyman and VandenBos 1989). Non-physician health care providers—like nurses, clinical psychologists, and Bachelor-level case managers—could assume some of the responsibilities of psychiatrists (National Association for Rural Mental Health 2006). With this system, psychiatrists then would collaborate with paramedical staff (Reed 1992), acting primarily as consultants and managing prescriptions. Moreover, the use of communication technologies (i.e. telepsychiatry) like the telephone and internet (Brown 1998; Farrell and McKinnon 2003) would be another innovative way to overcome current difficulties gaining access to rural psychiatric care. Although, at present, telepsychiatry focuses more on mood disorders than anything else (Greenwood et al. 2004), schizophrenia deserves more attention, because it is such a costly illness, both to the individual and society.
In summary, reforming current community-based care through the integration of psychiatric care resources, and improving the delivery of psychiatric care through innovative technologies will be important components in the revamping of Taiwan’s mental health system. Now that we have described the problems that exist, we suggest future exploration of the cost-effectiveness of those interventions in Taiwan.
Acknowledgements
We wish to thank the National Health Research Institute and the Bureau of National Health Insurance of Taiwan for generously providing the data for the analysis. Dr. S. V. Subramanian is supported by the National Institutes of Health Career Development Award (NHLBI K25 HL081275).
Contributor Information
Kuan-Chiao Tseng, Department of Psychiatry, National Taiwan University Hospital, No. 7 Chung-san S. Rd, Taipei 100, Taiwan, ROC, ktseng@ntu.edu.tw.
David Hemenway, Department of Health Policy and Management, Harvard School of Public Health, 677 Huntington Avenue, Kresge Building, Room 309, Boston, MA 02115, USA, hemenway@hsph.harvard.edu.
Ichiro Kawachi, Department of Society, Human Development, and Health, Harvard School of Public Health, 677 Huntington Avenue, Kresge Building 7th Floor, Boston, MA 02115, USA, society@hsph.harvard.edu.
S. V. Subramanian, Department of Society, Human Development, and Health, Harvard School of Public Health, 677 Huntington Avenue, Kresge Building 7th Floor, Boston, MA 02115, USA, svsubram@hsph.harvard.edu
Wei J. Chen, Institute of Epidemiology, College of Public Health, National Taiwan University, Room 123, No.17, XuZhou Road, Taipei City 100, Taiwan, ROC, wjchen@ntu.edu.tw
References
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bille M. The influence of distance on admissions to mental hospitals; first admissions. Acta Psychiatrica Scandinavica. 1963;39 Suppl. 169:226–233. doi: 10.1111/j.1600-0447.1963.tb07869.x. doi:10.1111/j.1600-0447.1963.tb07869.x. [DOI] [PubMed] [Google Scholar]
- Blumberg MS. Psychiatric bed need: Factors relating to demand for psychiatric services in California. Sacramento: Office of Planning, California Department of Mental Hygiene; 1965. [Google Scholar]
- Brown FW. Rural telepsychiatry. Psychiatric Services. 1998;49:963–964. doi: 10.1176/ps.49.7.963. [DOI] [PubMed] [Google Scholar]
- Bureau of National Health Insurance. The expenditure report of national health insurance, January 2000 to December 2002 (Committee No. 98) Taipei, Taiwan: Author; 2003. [Google Scholar]
- Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. Journal of Clinical Epidemiology. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. doi:10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- Cheng SH, Chiang TL. The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment. Journal of the American Medical Association. 1997;278:89–93. doi: 10.1001/jama.278.2.89. doi:10.1001/jama.278.2.89. [DOI] [PubMed] [Google Scholar]
- Department of Health. Health statistics in Taiwan. Taipei, Taiwan: Author; 2006. [Google Scholar]
- Faris REL, Dunham HW. Mental disorders in urban areas: An ecological study of schizophrenia and other psychoses. Chicago: University of Chicago Press; 1939. [Google Scholar]
- Farrell SP, McKinnon CR. Technology and rural mental health. Archives of Psychiatric Nursing. 2003;17:20–26. doi: 10.1053/apnu.2003.4. doi:10.1053/apnu.2003.4. [DOI] [PubMed] [Google Scholar]
- Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological Bulletin. 1995;118:392–404. doi: 10.1037/0033-2909.118.3.392. doi:10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Goldsmith HF, Wagenfeld MO, Manderscheid RW, Stiles D. Specialty mental health services in metropolitan and nonmetropolitan areas: 1983 and 1990. Administration and Policy in Mental Health. 1997;24:475–488. doi: 10.1007/BF02042826. doi:10.1007/BF02042826. [DOI] [PubMed] [Google Scholar]
- Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12:268–272. doi: 10.1080/j.1039-8562.2004.02097.x. doi:10.1111/j.1039-8562.2004.02097.x. [DOI] [PubMed] [Google Scholar]
- Haworth A. The distance factor in the use of psychiatric facilities. Medical Journal of Zambia. 1980–1981;15:6–9. [PubMed] [Google Scholar]
- Haynes R, Bentham G, Lovett A, Gale S. Effects of distances to hospital and GP surgery on hospital inpatient episodes, controlling for needs and provision. Social Science and Medicine. 1999;49:425–433. doi: 10.1016/s0277-9536(99)00149-5. doi:10.1016/S0277-9536(99)00149-5. [DOI] [PubMed] [Google Scholar]
- Heyman SR, VandenBos GR. Developing local resources to enrich the practice of rural community psychology. Hospital and Community Psychiatry. 1989;40:21–23. doi: 10.1176/ps.40.1.21. [DOI] [PubMed] [Google Scholar]
- Jarvis E. Influence of distance from and nearness to an insane hospital on its use by the people. American Journal of Insanity. 1866;22:361–418. [Google Scholar]
- Jordan H, Roderick P, Martin D, Barnett S. Distance, rurality and the need for care: access to health services in South West England. International Journal of Health Geographics. 2004;3:21. doi: 10.1186/1476-072X-3-21. doi:10.1186/1476-072X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert D, Agger MS. Access of rural AFDC Medicaid beneficiaries to mental health services. Health Care Financing Review. 1995;17:133–145. [PMC free article] [PubMed] [Google Scholar]
- McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. Journal of the American Medical Association. 1994;272:859–866. doi:10.1001/jama.272.11.859. [PubMed] [Google Scholar]
- Mental Health Act. Legislative Yuan of Taiwan. 1990 [Google Scholar]
- Miclutia I, Junjan V, Popescu CA, Tigan S. Migration, mental health and costs consequences in Romania. Journal of Mental Health Policy and Economics. 2007;10:43–50. [PubMed] [Google Scholar]
- Murray G, Judd F, Jackson H, Fraser C, Komiti A, Hodgins G, et al. Rurality and mental health: The role of accessibility. Australian and New Zealand Journal of Psychiatry. 2004;38:629–634. doi: 10.1080/j.1440-1614.2004.01426.x. doi:10.1111/j.1440-1614.2004.01426.x. [DOI] [PubMed] [Google Scholar]
- National Association for Rural Mental Health. Rural and frontier mental and behavioral health care: Barriers, effective policy strategies, best practices (Contract No. 02-0279P) Waite Park, MN: Author; 2006. [Google Scholar]
- National Policy Foundation. Issues of absentee voting (Publication No. 091-004) Taipei, Taiwan: Author; 2002. [Google Scholar]
- Nemet GF, Bailey AJ. Distance and health care utilization among the rural elderly. Social Science and Medicine. 2000;50:1197–1208. doi: 10.1016/s0277-9536(99)00365-2. doi:10.1016/S0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. Free for all? Lessons from the RAND health insurance experiment. Cambridge, MA: Harvard University Press; 1993. pp. 39–436. [Google Scholar]
- Norris V. Mental illness in London. London: Chapman and Hall; 1959. [Google Scholar]
- Peen J, Dekker J, Schoevers RA, Have MT, de Graaf R, Beekman AT. Is the prevalence of psychiatric disorders associated with urbanization? Social Psychiatry and Psychiatric Epidemiology. 2007;42:984–989. doi: 10.1007/s00127-007-0256-2. doi:10.1007/s00127-007-0256-2. [DOI] [PubMed] [Google Scholar]
- Phillips MR, Pearson V, Li F, Xu M, Yang L. Stigma and expressed emotion: A study of people with schizophrenia and their family members in China. British Journal of Psychiatry. 2002;181:488–493. doi: 10.1192/bjp.181.6.488. doi:10.1192/bjp. 181.6.488. [DOI] [PubMed] [Google Scholar]
- Reed DA. Adaptation: the key to community psychiatric practice in the rural setting. Community Mental Health Journal. 1992;28:141–150. doi: 10.1007/BF00754281. discussion 151–154. doi:10.1007/BF00754281. [DOI] [PubMed] [Google Scholar]
- Research Development Evaluation Commission, Executive Yuan. The strategic program of establishing public information service stations on remote areas (Retrieval No. 573.9029/6054) Taipei: Taiwan Government Printing Office; 2002. [Google Scholar]
- Rost K, Smith GR, Taylor JL. Rural-urban differences in stigma and the use of care for depressive disorders. Journal of Rural Health. 1993;9:57–62. doi: 10.1111/j.1748-0361.1993.tb00495.x. doi:10.1111/j.1748-0361.1993.tb00495.x. [DOI] [PubMed] [Google Scholar]
- Shannon GW, Bashshur RL, Lovett JE. Distance and the use of mental health services. Milbank Quarterly. 1986;64:302–330. doi:10.2307/3349974. [PubMed] [Google Scholar]
- Smith CA, Wright D, Day S. Distancing the mad: Jarvis’s Law and the spatial distribution of admissions to the Hamilton Lunatic Asylum in Canada, 1876–1902. Social Science and Medicine. 2007;64:2362–2377. doi: 10.1016/j.socscimed.2007.01.003. doi:10.1016/j.socscimed.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Sohler KB. Jarvis’ law and the planning of mental health services. Role of alternative psychiatric service in Connecticut. Public Health Reports. 1970;85:510–515. [PMC free article] [PubMed] [Google Scholar]
- Sohler KB, Clapis JA. Jarvis’ law and the planning of mental health services. HSMHA Health Reports. 1972;87:75–80. [PMC free article] [PubMed] [Google Scholar]
- Sohler KB, Thompson JD. Jarvis’ law and the planning of mental health services. Influence of accessibility, poverty, and urbanization on first admissions to Connecticut State hospitals. Public Health Reports. 1970;85:503–510. [PMC free article] [PubMed] [Google Scholar]
- Stampfer H, Reymond J, Burvill PW, Carlson J. The relationship between distance from inpatient facilities and the rate of psychiatric admissions in Western Australia. Social Science of Medicine. 1984;19:879–884. doi: 10.1016/0277-9536(84)90406-4. doi:10.1016/0277-9536(84)90406-4. [DOI] [PubMed] [Google Scholar]
- Subramanian SV. Statistical approach to inequalities in health. In: Rajan SI, James KS, editors. Demographic change, health inequality and human development. Hyderabad: Centre for Economic and Social Studies; 2004. pp. 185–209. [Google Scholar]
- Teke K, Kisa A, Demir C, Ersoy K. Appropriateness of admission and length of stay in a Turkish Military Hospital. Journal of Medical Systems. 2004;28:653–663. doi: 10.1023/b:joms.0000044967.14313.5f. doi:10.1023/B:JOMS.0000044967.14313.5f. [DOI] [PubMed] [Google Scholar]
- Waddell C, Dibley M. The medicalization of aboriginal children: A comparison of the lengths of hospital-stay of aboriginal and non-aboriginal children in Western Australia and the Northern Territory. Australian Paediatric Journal. 1986;22:27–30. doi: 10.1111/j.1440-1754.1986.tb00178.x. [DOI] [PubMed] [Google Scholar]
- Wakerman J. Defining remote health. Australian Journal of Rural Health. 2004;12:210–214. doi: 10.1111/j.1440-1854.2004.00607.x. doi:10.1111/j.1440-1854.2004.00607.x. [DOI] [PubMed] [Google Scholar]
- Wang KY. A review of mental health policy in Taiwan: Types of elite and the decision-making process. Chinese Journal of Mental Health. 1997;10(1):29–47. [Google Scholar]