Abstract
Objective
To evaluate the efficacy of different types of behavioral treatments for geriatric anxiety [cognitive-behavioral therapy (CBT) alone, CBT with relaxation training (RT), and RT alone].
Method
We compared effect sizes from 19 trials. Analyses were based on uncontrolled outcomes (comparing post-treatment and pre-treatment scores) and effects relative to control conditions on both anxiety and depressive symptoms.
Results
Treatments for older adults with anxiety symptoms were, on average, more effective than active control conditions. Effect sizes were comparable to those reported elsewhere for CBT for anxiety in the general population or for pharmacotherapy in anxious older adults. CBT (alone or augmented with RT) does not appear to add anything beyond RT alone, although a direct comparison is challenging given differences in control conditions. Effects on depressive symptoms were smaller, with no differences among treatment types.
Conclusion
Results suggest that behavioral treatments are effective for older adults with anxiety disorders and symptoms. Results must be interpreted with caution given the limitations of the literature, including differing sample characteristics and control conditions across studies.
Keywords: Psychotherapy, Geriatric, Anxiety, Relaxation Training, Cognitive Behavioral Therapy
The prevalence of anxiety among older adults is high (1), surpassing the rates of depression and severe cognitive dysfunction (2). Almost twice as many mental health Medicare claims are filed for anxiety disorders (38%) as for affective disorders (21%; 3). Anxiety disorders are associated with decreased quality of life (4) and increased disability (5) in older adults. Persistent anxiety symptoms that do not meet criteria for an anxiety disorder are also associated with serious negative consequences such as sleep disturbance, interference with daily activities, and distress (6,7). Prospective as well as cross-sectional research in the elderly has demonstrated that anxiety symptoms are associated with medical illness such as coronary heart disease (8), self-reported mobility limitations (9), and higher levels of health care utilization, including more primary care visits and more time spent during each visit (10).
There is growing evidence that, in the absence of treatment, anxiety symptoms and disorders are unlikely to fully remit (11,12). A recent meta-analysis (13) found that suicide risk among patients with anxiety disorders was higher than previously believed, at levels 10 times the general population, despite the fact that participants in the analyzed studies were believed to be at minimal suicide risk. The authors found no significant differences in suicide risk among the anxiety disorders. It is important to emphasize that suicide rates increase with age (14), and thus it is likely that older adults with anxiety disorders may be at particular risk of suicide.
Despite the high prevalence and established adverse effects of anxiety in later life, there is a paucity of treatment studies focused on this population. In fact, many anxiety treatment studies explicitly exclude adults over a certain age (often as young as 55 years old). As older adults often present to primary care physicians for psychiatric problems, pharmacotherapy is common. Benzodiazepines are the most commonly used anxiety management medication among older adults, followed by serotonergic antidepressants, buspirone, and venlafaxine (15). Benzodiazepines have been linked to toxicity, dependence, abuse, cognitive impairment/decline, psychomotor retardation and falls among older individuals who use them (11,16,17,18,19,20). Selective serotonin reuptake inhibitors (SSRIs) appear to be efficacious for older adults with anxiety disorders, and may be more effective than behavioral interventions (21,22,23). However, older adults may be reluctant to take medications, due in part to concerns about side effects and cost. Primary care providers may be wary of prescribing psychotropic medications to older adults because of complications due to medical problems or interactions due to polypharmacy.
Psychotherapeutic interventions provide an alternative to pharmacological treatments. There is ample evidence for the efficacy of psychotherapy in treating anxiety in mixed-age samples (24). However, as Gatz et al. (25) argued, we cannot assume that psychological treatments that are effective with younger adults will be effective with older adults. There has been a surge of interest in investigating psychosocial treatments for anxiety symptoms and disorders in older samples, as evidenced by many recent publications on this topic. Recent meta-analyses have concluded that behavioral interventions for geriatric anxiety have, on average, large effects when compared to baseline scores or wait list control conditions (22,26). No studies to date, however, have compared specific types of behavioral interventions beyond the broad distinction of CBT vs. other treatment or have presented data separately from studies that included active control conditions. In order to move the field forward by developing and testing new interventions, it is of interest to know the relative strength of different treatment components after controlling for attention and other nonspecific elements.
Types of psychotherapy or behavioral interventions that have been investigated for anxiety in older adults include relaxation training alone (RT), cognitive-behavioral therapy (CBT) without RT, and CBT with RT. RT is easier to conduct than CBT and requires less training on the part of the therapist. Moreover, a recent meta-analysis found no differences between RT and cognitive therapy for GAD in younger adults (27).
The objective of the current study is to review the psychotherapy outcome studies targeting anxiety among older adults and to compare effect sizes among different types of psychotherapeutic interventions. Individuals with anxiety disorders often have comorbid depressive symptoms, so we additionally examined treatment effects on depression measures when they were included.
Method
Selection of Studies
We identified potential studies for inclusion by searching Internet databases (i.e., Medline, PsycINFO) using relevant key words or phrases [“anxiety” (and specific anxiety disorders, such as “Generalized Anxiety Disorder”), “psychotherapy,” “psychosocial,” “behavioral,” “older adult,” “geriatric,” and “late-life”]; examining reference lists for promising titles; and consulting experts in the field of geriatric anxiety. We considered all potential articles that were published in English before September 2007. To be eligible for inclusion in our meta-analysis, studies were required to: (1) provide a prospective test of a psychotherapeutic intervention for anxiety disorders or symptoms; (2) report a mean subject age of 65 years or older or a lower limit on age no less than 55 years; (3) include at least 5 subjects (due to methodological and power concerns about studies with smaller sample sizes; thus excluding such studies as 28,29,30); (4) include only subjects who reported at least subjective anxiety symptoms (excluding 31,32,33); (5) investigate a treatment that was at least two sessions in length (excluding 34); (6) provide sufficient data for the calculation of effect sizes (excluding 35); and (7) report results from published and cited anxiety or depression measures (excluding 36,37). Regarding this last criterion, we did not include study-specific indices in analyses (e.g., “trips out of the house,” “number of panic attacks”) unless they were items from validated measures (e.g., generalized anxiety disorder severity from structured diagnostic interviews). We also did not analyze measures of constructs other than anxiety or depression (e.g., quality of life, headaches, heart rate).
Effect Size Calculation
We calculated effect sizes using the standardized mean difference statistic (Hedges’ g): (mean1 - mean2)/sp (where sp is the pooled standard deviation weighted by the size of the samples). Hedges’ g is an unbiased estimator with adjustment for small sample bias, related to Cohen’s d as follows: g = d √ (N/DF) (38). We calculated the Q statistic to test for heterogeneity among effect sizes of individual studies separately for anxiety and depression measures. Analysis of variance (ANOVA) with fixed effects was then performed separately for anxiety and depression, with type of treatment as the independent variable. We conducted analyses for uncontrolled studies as well as controlled studies so that we could include more studies in this review of a relatively small research area.1 In our analyses, a positive effect size indicates a relative reduction in anxiety or depressive symptoms.
For two studies, standard deviations were not reported. Shadish and colleagues (39) note that while it is possible to estimate effect sizes based on results described as “significant,” “nonsignificant,” or “significant based on a certain probability level (e.g., p <.05),” it is preferable to estimate based on related research or normative data. Thus, for the DeBerry studies (40,41) we substituted standard deviations for state and trait anxiety from a similar sample [42, for pre- and post-change (treatment or waitlist) for each condition], and for the DeBerry (41) depression measure we substituted the standard deviation from Dunn and Sacco (43, the same “young-old subjects” sd at pre- and post-change for both conditions). In another study (23), neither means nor standard deviations were reported in the original article, but we were able to obtain these statistics from the first author.
We included anxiety and depression measures only, and so measures which mixed constructs (e.g., the Symptom Check List-90-Revised Global Severity Index) were excluded. In the event that both full-scale and subscale scores on an anxiety or depression instrument were reported, we included only the full-scale score in analyses. If subscale scores only were reported, we included each subscale score in analyses. For summary statistics, we calculated the effect size for each reported anxiety or depression measure within each sample, averaged the effect sizes across measures of each construct (anxiety or depression) within each sample, and weighted the final result by sample size when averaging across studies. Many studies were lacking follow-up data collection, and the studies that did have a follow-up varied widely in the assessment intervals. Thus, we did not include follow-up assessments in our analyses.
We screened approximately 300 abstracts and obtained and reviewed 83 promising articles. Based on our stated criteria, 19 studies described in 18 publications (44 reported two studies) were eligible for inclusion in our meta-analysis (see Table 1). These studies represent a diversity of methodological approaches and samples from several distinct research laboratories. Half of the eligible articles were published within the past 5 years, demonstrating the burgeoning of interest in this area of research.
Table 1.
Studies Included in Meta-analytic Review
| Author, Year | Sample Description | Age: Mean (sd) or Range) | Type of Condition(s) (n) | Mode of Treatment | Anxiety Measures | Depression Measures |
|---|---|---|---|---|---|---|
| * Barrowclough et al., 2001 (57) | Primary care patients: 51% PD; 19% GAD; 28% ADNOS; 2% social phobia | 72 | CBT-RT (19); Active Control (24) | Individual, home delivered | Trait Anxiety; BAI; HAMA | BDI; GDS |
| * DeBerry, 1981 (40) | Recent widows with complaints of anxiety | 68.9 | RT (5); Active Control (5) | Group | Trait Anxiety; State Anxiety | None |
| * DeBerry, 1982 (41) | Recent widows with complaints of anxiety | 69 to 84 | RT (13); CBT-RT (10); Active Control (9) | Group | Trait Anxiety; State Anxiety | SDS |
| * DeBerry et al., 1989 (42) | Recent widows and widowers with complaints of anxiety | 63 to 79 | RT (24); Active Control (12) | Group | Trait Anxiety; State Anxiety | BDI |
| * Gorenstein et al., 2005 (49) | GAD or PD or trait anxiety | 68.5 | CBT+RT (14); Active Control (14) | Individual | Trait Anxiety; PSWQ; SCL-Anxiety subscale; SCL-Phobic Anxiety subscale; SCL- Obsessive Compulsive subscale | BDI-II |
| King & Barrowclough, 1991 (62) | GAD or PD with or without Agoraphobia | 73 | CBT-RT (10) | Individual | BAI | BDI |
| Ladouceur et al., 2004 (63) | GAD | 64 | CBT-RT (8) | Individual | BAI; PSWQ; Worry and Anxiety Questionnaire; Worry Domains Questionnaire Form for the Elderly | BDI |
| Mohlman et al., 2005 (44) | GAD | 65 to 67 | CBT+RT − Intact EF (10) CBT+RT − Improved EF (5) CBT+RT − Impaired EF (7) WL (10) | Individual | Trait Anxiety; BAI; PSWQ | BDI |
| Mohlman et al., 2003 Study 1 (64) | GAD | 66.4 | CBT+RT (11); WL (10) | Individual | Trait Anxiety; BAI; PSWQ; GAD Severity (SCID for DSM-IV); SCL-Anxiety subscale | BDI |
| Mohlman et al., 2003 Study 2 (64) | GAD | 67.5 | CBT+RT (8); WL (7) | Individual | Trait Anxiety; BAI, PSWQ; GAD Severity (SCID for DSM-IV); SCL-Anxiety subscale | BDI |
| Radley et al., 1997 (61) | Women with GAD (some with phobias) | 65 to 76 | RT (6) | Group | Trait Anxiety; State Anxiety; HAMA; Fear Inventory; Hospital Anxiety and Depression Scale – Anxiety; Generalized Anxiety Questionnaire; Cognitive Anxiety Questionnaire | None |
| * Sallis et al., 1983 (59) | At least moderate depression and trait anxiety | 71.3 | RT (8); CBT-RT (8) Active Control (8) | Group | Trait Anxiety | BDI |
| Schurmanns et al., 2006 (23) | GAD, PD, Agoraphobia, and/or Social Anxiety | 69.8 | CBT+RT (30); WL (9) (Sertraline trial not analyzed in present review) | Individual | BAI; HAMA; Worry Domains Questionnaire | CES-D |
| Scogin et al., 1992 (47) | “uncomfortable” anxiety | 68 | RT (19); RT (19); WL (16) | Individual | Trait Anxiety; State Anxiety | None |
| * Stanley et al., 1996 (48) | GAD | 68.3 | CBT+RT (18); Active Control (13) | Group | Trait Anxiety; HAMA; PSWQ; GAD Severity (ADIS-R); WS; % of day worried (ADIS-R); FQ | BDI; HAMD |
| Stanley, Beck et al., 2003a (65) | GAD | 66.2 | CBT+RT (29); WL (35) | Group | Trait Anxiety; HAMA; PSWQ; GAD Severity (ADIS-IV); WS | BDI; HAMD; GDS-15 |
| Stanley, Hopko et al., 2003b (66) | GAD | 70.6 | CBT+RT (5); WL (4) | Individual | BAI; PSWQ; GAD Severity (SCID for DSM-IV) | BDI |
| Swales et al., 1996 (45) | PD | 63.2 | CBT+RT (15) | Individual | BAI; Average ACQ; Average BSQ; TPRPS – Situations, Alone; MIA – Situations, Alone; FQ – Total | BDI; GDS |
| * Wetherell et al., 2003 (67) | GAD | 67.1 | CBT+RT (18); Active Control (18); WL (21) | Group | BAI; PSWQ; HAMA; GAD Severity (ADIS- IV); % of day worried (ADIS-IV) | BDI; HAMD |
Note. PD = panic disorder; GAD = generalized anxiety disorder; ADNOS = anxiety disorder not otherwise specified; NR = Not reported; CBT = Cognitive-Behavioral Therapy; RT = Relaxation Training;. WL = Wait List; EF = Executive Functioning; BAI = Beck Anxiety Inventory; PSWQ = Penn State Worry Questionnaire; HAMA = Hamilton Rating Scale for Anxiety; ADIS = Anxiety Disorders Interview Schedule; SCL = Symptom Checklist −90 – Revised; SCID = Structured Clinical Interview for the DSM; WS = Worry Scale; FQ = Fear Questionnaire; ACQ = Agoraphobia Cognitions Questionnaire; BSQ = Body Sensations Questionnaire; TPRPS = Texas Panic-Related Phobia Scale; MIA = Mobility Inventory for Agoraphobia; BDI = Beck Depression Inventory; HAMD = Hamilton Rating Scale for Depression; GDS = Geriatric Depression Scale; CES-D = Center for Epidemiological Studies Depression Scale; SDS = (Zung) Self-Rating Depression Scale.
Sample Characteristics
Of the 19 studies included in the present meta-analysis, eight included subjects with generalized anxiety disorder (GAD), five included subjects with mixed anxiety disorders (predominantly GAD and panic disorder (PD), with some social anxiety disorder and specific phobias), five included subjects who complained of anxiety symptoms, and one (45) included subjects with a primary diagnosis of PD (with or without agoraphobia). Thus, GAD and PD are heavily represented in psychosocial treatment outcome studies of late-life anxiety, whereas obsessive-compulsive disorder (OCD) and posttraumatic stress disorder (PTSD) are not represented.
Four of the eligible studies had no control condition for comparison, but the remaining 15 of the 19 studies included a control condition or two. There were 24 treatment samples (excluding one of the samples in 23, which was treatment with a medication only) with eight active control samples and eight wait-list control samples. Thus, across the 19 studies we report on the 40 samples with anxiety measures (total n = 522) and 34 of these samples that included depression measures as well (total n = 452). Ten active treatment samples with anxiety measures (total n = 257) and a subset with depression measures (total n = 247) were compared to an active control condition.
We report outcomes for five different types of samples, as presented in Table 2 with mean uncontrolled effect sizes by sample type. Two blind raters classified each intervention into categories; agreement was perfect. Categories were as follows: 1) Wait list or no-treatment control conditions (8 samples) describe periods without active intervention (but which may include weekly, monthly, or pre/post assessments), which are described by researchers as “delayed training,” “minimal contact,” or “usual care.” 2) CBT with relaxation training (CBT + RT; 12 samples), which comprises treatments that include relaxation training as well as other techniques for cognitive and behavioral change. These techniques include traditional CBT strategies such as thought monitoring, cognitive restructuring, exposure methods and response prevention, behavioral activation, and problem solving coupled with traditional relaxation strategies such as progressive muscle relaxation (PMR), breathing exercises, meditation, and imagery.2 3) CBT without relaxation training (CBT – RT; 5 samples) comprises the CBT components without explicit mention of the relaxation components in treatment descriptions. 4) Relaxation Training alone (RT; 7 samples) comprises the relaxation components without other CBT elements. 5) Active control conditions (8 samples) include “supportive counseling or psychotherapy,” “non-formal” training in CBT or relaxation training, group discussion, psychoeducation, time for quiet reflection, and weekly medication management.
Table 2.
Uncontrolled Effect Sizes
| Anxiety Measures |
Depression Measures |
|||||
|---|---|---|---|---|---|---|
| Condition | N Studies | N Patients | Mean g (95% CI) | N Studies | N Patients | Mean g (95% CI) |
| CBT−RT | 5 | 55 | 1.18 (0.78, 1.59) | 5 | 55 | 0.78 (0.38, 1.17) |
| CBT+RT | 12 | 170 | 0.86 (0.63, 1.08) | 12 | 170 | 0.77 (0.55, 1.00) |
| RT | 7 | 82 | 0.91 (0.68, 1.24) | 3 | 33 | 0.77 (0.26, 1.27) |
| Active Control | 8 | 103 | 0.50 (0.22, 0.78) | 7 | 98 | 0.53 (0.24, 0.82) |
| Wait List/No Treatment | 8 | 112 | 0.05 (−0.21, 0.31) | 7 | 96 | 0.20 (−0.08, 0.49) |
Note. N = Number of patients; CI = Confidence interval; CBT = Cognitive-Behavioral Therapy; RT = Relaxation Training.
Measures
Thirteen of the 19 studies utilized the trait anxiety measure from Spielberger and colleagues (46). With a few exceptions, mean baseline Spielberger trait anxiety scores fell within a narrow range (50.0 – 57.0). Outliers included Scogin et al. (47), who reported a mean of 42.9; DeBerry et al. (42): 43.2; Stanley et al. (48): 48.0; and at the other end of the spectrum, Gorenstein et al. (49): 73.1. Reflecting the relative emphasis of GAD, 10 of the studies included worry measures such as the Penn State Worry Questionnaire (50). Studies included from one to seven anxiety measures (mean: 3.74), and 9 of the studies included clinician-rated measures (from one to three measures; mean: 1.56) in addition to self report instruments. Sixteen studies included at least one depressive symptom measure, and these studies included from one to three depressive symptom measures (mean: 1.38). By far the most common measure of depressive symptoms (found in 14 studies) was one of the versions of the Beck Depression Inventory (51). Only three studies included a clinician-rated measure of depression, and each used the Hamilton Rating Scale for Depression (HAMD; 52).
Results
Table 1 summarizes information about the subjects, design, conditions, and measures in each study. Table 2 presents uncontrolled effect sizes (within-group; pre vs. post).
Anxiety Symptoms
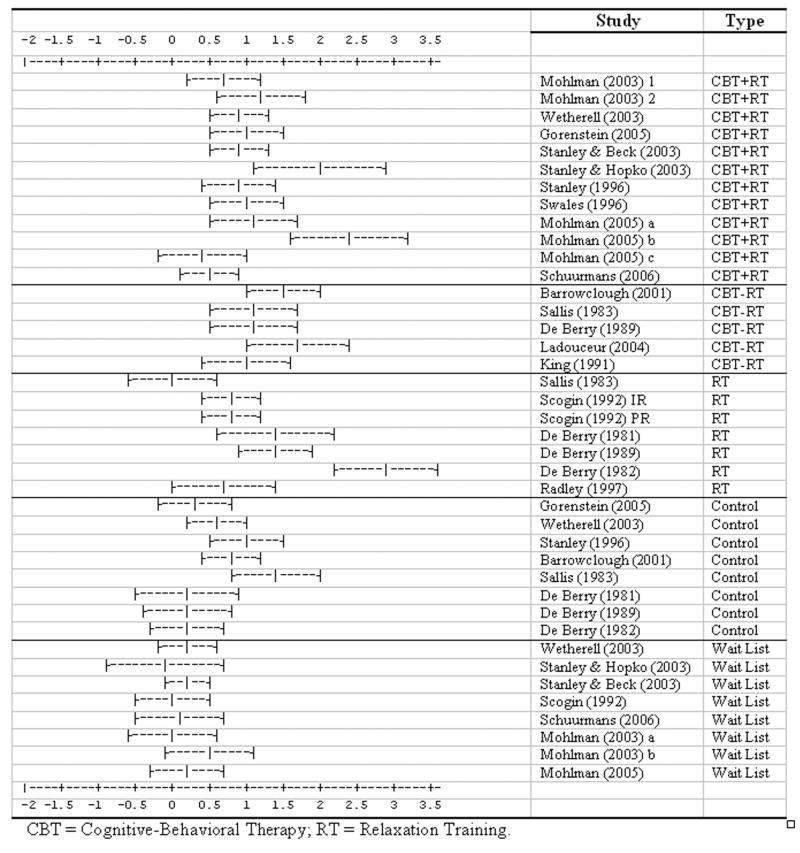
For the anxiety measures, the omnibus heterogeneity test revealed significant differences among all studies (Cochran’s Q = 71.21; χ2 (31), p = .001), but no differences among studies within each treatment condition. However, significant differences were found among the samples, Q = 33.62, χ2 (4), p <.0001, indicating that all treatments (but not the active control conditions) were more effective than the wait list. The omnibus test showed that effect sizes differed among the conditions even when excluding the wait list, Q = 8.63, χ2 (3), p = .03, with all three types of treatment showing large effects, compared with medium effects for the active controls. Note that this contrast between the treatments and the active controls is statistically significant even though there is slight overlap in confidence intervals (see van Belle, 2002,53). Pairwise comparisons showed a significant difference between CBT-RT and the active control conditions, but the other pairwise comparisons were not significant. Effect sizes and standard errors for each study are depicted in Figure 1.
Figure 1.
Uncontrolled Anxiety Effect Sizes With Standard Errors
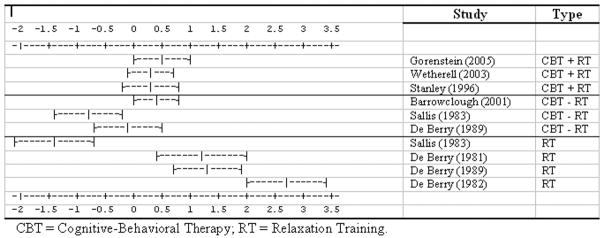
When analyses of anxiety measures were limited to studies in which treatments were compared to active control conditions (Table 3), the heterogeneity test indicated differences among studies (Q = 39.44, χ2 (9), p <.0001). In separate heterogeneity tests for each treatment condition, there were significant differences within RT (Q = 28.46, χ2 (3), p <.0001). In the omnibus ANOVA, controlled effects differed significantly across treatments, Q = 6.86, χ2 (2), p = .03. RT showed large effects, whereas CBT with or without RT showed effects that did not differ significantly from zero. Again, however, pairwise comparisons were not significant. Effect sizes and standard errors relative to active control conditions for each study are depicted in Figure 2.
Table 3.
Controlled Effect Sizes
| Anxiety Measures |
Depression Measures |
|||||
|---|---|---|---|---|---|---|
| Condition vs. Active Control | N Studies | N Patients | Mean g (95% CI) | N Studies | N Patients | Mean g (95% CI) |
| CBT-RT | 3 | 37 | 0.00 (−0.46, 0.46) | 3 | 37 | 0.23 (−0.22, 0.69) |
| CBT+RT | 3 | 50 | 0.33 (−0.07, 0.74) | 3 | 50 | 0.12 (−0.29, 0.52) |
| RT | 4 | 38 | 0.90 (0.44, 1.44) | 3 | 33 | 0.23 (−0.29, 0.76) |
Note. CI = Confidence interval; CBT = Cognitive-Behavioral Therapy; RT = Relaxation Training.
Figure 2.
Controlled Anxiety Effect Sizes With Standard Errors
Depressive Symptoms
With respect to measures of depressive symptoms, uncontrolled effect sizes differed among studies (Q = 52.63, χ2 (33), p = .02). There was no evidence for heterogeneity within any treatment condition. ANOVA indicated that effect sizes differed across conditions, Q = 11.26, χ2 (4), p = .02. All three treatments had large effects, active control conditions had medium effects, and effects of wait lists did not differ from zero (Table 2). In pairwise comparisons, only the CBT+RT condition had a significantly larger effect than the wait list/no treatment comparison condition. Excluding the wait list, there were no significant differences among conditions in controlled effect sizes, Q = 2.08, χ2 (2), p = .35 (Table 3).
When analyses for depression were limited to studies in which treatments were compared to active control conditions (Table 3), the heterogeneity test indicated differences among studies (Q = 19.77, χ2 (8), p = .01). In heterogeneity tests by condition, there were significant differences among studies within RT (Q = 13.28, χ2 (2), p = .001). There were no significant differences in effect sizes among conditions (Q = 0.18, χ2 (2), p = .91).
Discussion
Mean uncontrolled effect sizes suggest that: (1) spontaneous remission of symptoms during a wait-list period is unlikely; (2) active control conditions had moderate effects for both anxiety and depressive symptoms; (3) compared to active control conditions, psychosocial treatments have relatively large effects on depressive symptoms and a larger effect on anxiety symptoms; and (4) there are no apparent outcome differences among conditions on depressive symptoms.
When treatment samples are compared to active control conditions on anxiety measures, the mean controlled effect sizes for RT (.90), CBT with RT (0.33), and CBT without RT (0.00) compare with results previously reported by others: a mean controlled effect size of 0.71 for CBT for GAD in the general population and 0.83 for pharmacotherapy for anxiety in older adults (22,53). There are no apparent outcome differences among the three treatment types on depressive symptoms, with all effect sizes in the small range.
We chose to present both uncontrolled and controlled results (e.g., within and between groups), as meta-analyses of psychotherapy studies for GAD frequently calculate effects both ways (e.g., 53). Response rates in treatment studies appear to vary depending upon the type of control condition (54). For this reason, it seems appropriate to report both sets of results, as has been done in recent meta-analyses of pharmacotherapy for late-life anxiety and depression also published in this journal (22,55).
Most psychotherapy treatment studies in late-life anxiety do not include active control conditions, so that more than twice as many comparisons are included in Table 2 (uncontrolled effect sizes) as in Table 3 (controlled effect sizes). Of note, if Table 2 were limited to those studies included in Table 3, the uncontrolled effect sizes reported for CBT+RT, CBT-RT, and RT would be .93, 1.20, and 1.50, respectively. These results are broadly consistent with Table 3 in suggesting that RT may be somewhat more effective for geriatric anxiety than the alternatives tested to date. However, this also suggests that all three treatments were compared to somewhat powerful control conditions, and more equitable (ideally, identical) control conditions would help to reveal any true differences between treatments.
Results for CBT-RT vary widely between uncontrolled and controlled studies. Although the 5 studies included in Table 2 show that patients do make gains after CBT-RT, two of the three studies, conducted by different investigative teams, comparing CBT-RT to an active alternative condition (Table 3) found that the alternative condition led to greater gains than did CBT-RT. This may suggest that CBT-RT could be a relatively weak intervention for late-life anxiety, but certainly more research is needed.
All but two of the studies examined psychotherapies administered in groups. Individual therapy is often expected to yield superior outcomes when compared to group therapy. However, both of the studies which offered individual treatment (49,56) were in the CBT categories (with or without RT), and thus this distinction does not appear to explain the results.
The results of this study suggest that relaxation training and cognitive therapy are effective psychosocial treatments for older adults with anxiety disorders or symptoms. CBT (alone or augmented with RT) does not appear to add anything beyond RT alone, although a direct comparison is challenging given differences in control conditions. Relaxation training is a brief intervention that brings rapid relief, and training providers to do relaxation training appropriately is simpler than training them in more complex CBT methods. Moreover, older adults report high levels of satisfaction with relaxation training (57). A psychosocial treatment that combines components (e.g., CBT techniques plus relaxation training) may be attractive because it offers a variety of skills, but the results of our analysis suggest that more does not always mean better for anxious samples of older adults.
Limitations
Our analysis of the relatively small treatment outcome literature for older adults with anxiety disorders or symptoms has several limitations. We developed our own taxonomy to describe the treatments used in these studies. Other researchers may have defined the treatment categories differently. However, the interrater reliability on our categories was perfect. One of our goals was to compare psychosocial treatments based on whether they included relaxation training. Treatment components were not often directly compared within studies, however, and more dismantling studies are needed to demonstrate the true value of relaxation training.
We found significant heterogeneity among the results of the RT studies, with apparent outliers falling in both the positive and negative direction. RT protocols vary and can include diaphragmatic breathing, imagery, progressive muscle relaxation, and meditation techniques. The studies conducted by De Berry and colleagues (40,41,42), which had larger effects than other investigations, included meditation to a greater extent than the other RT protocols. It is possible that meditation may offer benefits beyond what are achieved with other RT strategies. Overall, our conclusions with respect to the effectiveness of RT should be tempered with the knowledge that different RT protocols may lead to different results.
Three of the studies we examined did a direct comparison of active psychotherapies, as opposed to an active control condition. Sallis et al. (58) compared a relaxation-based “anxiety management training” (without other CBT components, but including imagery, relaxation, and meditation) with a CBT-based “depression treatment” (without relaxation training, but including pleasant event monitoring, problem solving, and cognitive restructuring). Both treatments separately fared poorly against a robust “placebo” control (including self-disclosure and reflection of feelings), but an effect size analysis favored the CBT-based depression treatment on anxiety measures (mean d = 0.77) though ironically not on depression measures (mean d = .03) when CBT and relaxation were compared directly. DeBerry et al. (42) compared progressive muscle relaxation with imagery and meditation (without explicit cognitive therapy) to cognitive restructuring and assertiveness training (without relaxation training). An effect size analysis revealed that relaxation was superior to CBT on anxiety measures (mean d = 1.39) and depression measures (mean d = 0.82). Stanley and colleagues (48) compared CBT with relaxation training to supportive psychotherapy. Results indicated that both treatments significantly and equivalently reduced anxiety, worry, and depression.
Results were confounded by different sample characteristics and different comparison groups. The majority of the studies recruited samples with primary GAD, PD with or without agoraphobia, or subjective reports of anxiety. Our review included those with anxiety disorders and those with sub-threshold symptoms, for whom the magnitude of change is typically smaller. Indeed, the different results obtained from the Sallis et al. (58) and DeBerry et al. (42) studies may be attributable to sample differences, as the Sallis sample was recruited for having moderate anxiety (and depression) while the DeBerry sample had only “complaints of anxiety” (and slightly lower trait anxiety scores compared to the Sallis sample at baseline). None of the studies solely focused on social phobia or specific phobias, and none included subjects with known OCD or PTSD.
As noted above, however, baseline severity of anxiety symptoms as measured by the Spielberger trait anxiety scale was quite consistent across studies. Fewer than half of the studies included clinician-rated measures. This is especially important because the Hamilton Anxiety Scale is the standard in most drug studies. Researchers are therefore encouraged to include this scale in studies of late-life anxiety. Furthermore, in the four studies that included both clinician- rated and self-report measures, clinician-rated measures tended to yield larger effects (d = 1.37) than self-report measures (d = .81); this difference, however, was not statistically significant.
Recommendations and Future Directions
This study adds to the literature on late-life anxiety disorders by comparing different types of behavioral interventions. As such, it represents the closest approximation available to a dismantling study. Such studies are important to guide both clinicians in the selection of appropriate treatments, as well as interventions researchers in developing new forms and combinations of treatments.
The results must be interpreted with caution because of methodological limitations of analyses based on a small number of studies, differences in sample selection, and diverse control conditions (when controls were used). We suggest that in order to strengthen this nascent literature, psychotherapy studies of late-life anxiety should include active comparison conditions whenever possible. It is also important for researchers to identify the specific components involved in CBT (and other multi-component treatments), and true dismantling studies could add greatly to the theoretical and practical foundations of psychotherapy for older adults. Researchers should similarly take great care in selecting and describing control conditions. It is a great challenge to discover relatively inert but credible active control conditions, as evidenced by this review. Studies that compare two or more distinct and well-defined treatments to a well-defined control condition will greatly advance research on treatments for late-life anxiety, as would dismantling studies that compare separate components of treatments.
Acknowledgments
This research is supported by NIMH Grant No. K23 MH067643.
Footnotes
The formula for g for pre/post analyses would ideally take into account the correlation between pretest and posttest scores (39). However, because these correlations were rarely reported we used the standard formula to estimate g, which may have resulted in an underestimate of g for the pre/post analyses, assuming that correlations between pre- and post-test scores are higher than .50, which is usually the case (59).
Note that Mohlman et al. (44) contributes three samples of “CBT with RT” because treatment data from three separate samples (defined by subjects’ relative status of executive functioning) were reported.
Note that Scogin et al. (47) contribute two RT samples (“progressive relaxation” and “imaginal progressive relaxation”) and both Radley et al. (60) and Sallis et al. (58) describe “anxiety management training” which teaches methods of “dealing with” avoidance, “coping with” anxiety, “thinking processes,” and “self-monitoring” that we did not deem as explicit CBT methods for the purposes of this review.
Contributor Information
Steven R. Thorp, UCSD Department of Psychiatry and VA San Diego Healthcare System
Catherine R. Ayers, Sharp Grossmont Hospital and VA San Diego Healthcare System
Roberto Nuevo, Universidad Autonoma de Madrid
Jill A. Stoddard, UCSD Department of Psychiatry and VA San Diego Healthcare System
John T. Sorrell, Clinical Trials & Research, San Mateo Medical Center
Julie Loebach Wetherell, UCSD Department of Psychiatry and VA San Diego Healthcare System
References
- 1.Beekman AT, Bremmer MA, Deeg DH, et al. Anxiety disorders in later life: A report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13:717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.Regier DA, Rae DS, Narrow WE, et al. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. British Journal of Psychiatry. 1998;173 (Suppl 34):24–28. [PubMed] [Google Scholar]
- 3.Ettner SL, Hermann RC. Provider specialty choice among Medicare beneficiaries treated for psychiatric disorders. Health Care Financing Rev. 1997;18:43–59. [PMC free article] [PubMed] [Google Scholar]
- 4.Wetherell JL, Thorp SR, Patterson TL, et al. Quality of life in geriatric generalized anxiety disorder: a preliminary investigation. J Psychiatr Res. 2004;38:305–312. doi: 10.1016/j.jpsychires.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 5.De Beurs E, Beekman AT, Van Balkom AM, et al. Consequences of anxiety in older persons: Its effect on disability, well-being and use health services. Psychol Med. 1999;29:583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- 6.Diefenbach GJ, Hopko DR, Feigon S, et al. ‘Minor GAD’: characteristics of subsyndromal GAD in older adults. Behav Res Ther. 2003;41:481–487. doi: 10.1016/s0005-7967(02)00130-4. [DOI] [PubMed] [Google Scholar]
- 7.Wetherell JL, Le Roux H, Gatz M. DSM-IV criteria for generalized anxiety disorder in older adults: distinguishing the worried from the well. Psychol Aging. 2003;18:622–627. doi: 10.1037/0882-7974.18.3.622. [DOI] [PubMed] [Google Scholar]
- 8.Kubzansky LD, Kawachi I, Weiss ST, et al. Anxiety and coronary heart disease: a synthesis of epidemiological, psychological, and experimental evidence. Ann Behav Med. 1998;20:47–58. doi: 10.1007/BF02884448. [DOI] [PubMed] [Google Scholar]
- 9.Mehta KM, Yaffe K, Brenes GA, et al. Anxiety symptoms and decline in physical function over 5 years in the health, aging and body composition study. J Am Geriatr Soc. 2007;55:265–270. doi: 10.1111/j.1532-5415.2007.01041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stanley MA, Roberts RE, Bourland SL, et al. Anxiety disorders among older primary care patients. J Clin Geropsychology. 2001;7:105–116. [Google Scholar]
- 11.Schuurmans J, Comijs HC, Beekman AT, et al. The outcome of anxiety disorders in older people at 6-year follow-up: Results from the Longitudinal Aging Study Amsterdam. Acta Psychiatr Scand. 2005;111:420–428. doi: 10.1111/j.1600-0447.2005.00531.x. [DOI] [PubMed] [Google Scholar]
- 12.Yonkers KA, Bruce SE, Dyck IR, et al. Chronicity, relapse, and illness – course of panic disorder, social phobia, and generalized anxiety disorder: Findings in men and women from 8 years of follow-up. Depress Anxiety. 2003;17:173–179. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]
- 13.Khan A, Leventhal R, Khan S, et al. Severity of depression and response to antidepressants and placebo: An analysis of the Food and Drug Administration database. J Clin Psychopharmacol. 2002;22:40–45. doi: 10.1097/00004714-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Pearson JL, Brown GK. Suicide prevention in late life: directions for science and practice. Clin Psychol Rev. 2000;20:685–705. doi: 10.1016/s0272-7358(99)00066-5. [DOI] [PubMed] [Google Scholar]
- 15.Mamdani M, Rapoport M, Shulman KI, et al. Mental health-related drug utilization among older adults: Prevalence, trends, and costs. Am J Geriatr Psychiatry. 2005;13:892–900. doi: 10.1176/appi.ajgp.13.10.892. [DOI] [PubMed] [Google Scholar]
- 16.Allain H, Bentue-Ferrer D, Polard E, et al. Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging. 2005;22:749–765. doi: 10.2165/00002512-200522090-00004. [DOI] [PubMed] [Google Scholar]
- 17.Bogunovic OJ, Greenfield SF. Use of benzodiazepines among elderly patients. Psychiatric Serv. 2004;55:233–235. doi: 10.1176/appi.ps.55.3.233. [DOI] [PubMed] [Google Scholar]
- 18.Gray SL, LaCroix AZ, Hanlon JT, et al. Benzodiazepine use and physical disability in community-dwelling older adults. J Am Geriatr Soc. 2006;54:224–230. doi: 10.1111/j.1532-5415.2005.00571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Longo LP, Johnson B. Addiction: Part I. Benzodiazepines--side effects, abuse risk and alternatives. Am Fam Physician. 2000;7:2121–2128. [PubMed] [Google Scholar]
- 20.Paterniti S, Dufouil C, Alperovitch A. Long-term benzodiazepine use and cognitive decline in the elderly: the Epidemiology of Vascular Aging Study. J Clin Psychopharmacol. 2002;22:285–293. doi: 10.1097/00004714-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Lenze EJ, Mulsant BH, Shear MK, et al. Efficacy and tolerability of citalopram in the treatment of late-life anxiety disorders: results from an 8-week randomized, placebo-controlled trial. Am J Psychiatry. 2005;162:146–150. doi: 10.1176/appi.ajp.162.1.146. [DOI] [PubMed] [Google Scholar]
- 22.Pinquart M, Duberstein PR. Treatment of anxiety disorders in older adults: A meta-analytic comparison of behavioral and pharmacological interventions. Am J Geriatr Psychiatry. 2007;15:639–651. doi: 10.1097/JGP.0b013e31806841c8. [DOI] [PubMed] [Google Scholar]
- 23.Schuurmans J, Comijs H, Emmelkamp PM, et al. A randomized, controlled trial of the effectiveness of cognitive-behavioral therapy and sertraline versus a waitlist control group for anxiety disorders in older adults. Am J Geriatr Psychiatry. 2006;14:255–263. doi: 10.1097/01.JGP.0000196629.19634.00. [DOI] [PubMed] [Google Scholar]
- 24.Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- 25.Gatz M, Fiske A, Fox LS, et al. Empirically validated psychological treatments for older adults. J Mental Health Ageing. 1998;4:9–46. [Google Scholar]
- 26.Nordhus IH, Pallesen S. Psychological treatment of late-life anxiety: an empirical review. J Consult Clin Psychol. 2003;71:643–51. doi: 10.1037/0022-006x.71.4.643. [DOI] [PubMed] [Google Scholar]
- 27.Sieve J, Chambless D. Specificity of treatment effects: Cognitive therapy and relaxation for generalized anxiety and panic disorders. Journal of Consulting and Clinical Psychology. 2007;75:513–522. doi: 10.1037/0022-006X.75.4.513. [DOI] [PubMed] [Google Scholar]
- 28.Lohr JM, Tolin DF, Kleinknecht RA. An intensive design investigation of eye movement desensitization and reprocessing of claustrophobia. J Anx Disord. 1996;10:73–88. [Google Scholar]
- 29.Junginger J, Ditto B. Multitreatment of obsessive-compulsive checking in a geriatric patient. Behav Mod. 1984;8:379–390. doi: 10.1177/01454455840083005. [DOI] [PubMed] [Google Scholar]
- 30.Maercker A. Life-review technique in the treatment of PTSD in elderly patients: Rationale and three single case studies. J Clin Geropsychol. 2002;8:239–249. [Google Scholar]
- 31.Keller JF, Croake JW, Brooking JY. Effects of a program in rational thinking on anxieties in older persons. J Couns Psychol. 1975;22:54–57. [Google Scholar]
- 32.Scates SK, Randolph DL, Gutsch KU, et al. Effects of cognitive-behavioral, reminiscence, and activity treatments on life satisfaction and anxiety in the elderly. Int J Aging Hum Devel. 1985;22:141–146. doi: 10.2190/2v33-6hdj-xmpd-568f. [DOI] [PubMed] [Google Scholar]
- 33.Viney LL, Benjamin YN, Preston CA. An evaluation of personal construct therapy for the elderly. Br J Med Psychol. 1989;62:35–41. doi: 10.1111/j.2044-8341.1989.tb02808.x. [DOI] [PubMed] [Google Scholar]
- 34.Powers CB, Wisocki PA. An examination of the therapeutic benefits of focus groups on elderly worriers. Int J Aging Hum Devel. 1997;45:159–167. doi: 10.2190/5GHQ-QFWR-JVYJ-TNHP. [DOI] [PubMed] [Google Scholar]
- 35.Ingersoll B, Silverman A. Comparative group psychotherapy for the aged. The Gerontologist. 1978;18:201–206. doi: 10.1093/geront/18.2.201. [DOI] [PubMed] [Google Scholar]
- 36.Hyer L, Swanson G, Lefkowitz R, et al. The application of the cognitive behavioral model to two older stressor groups. Clin Gerontol. 1990;9:145–190. [Google Scholar]
- 37.Welden S, Yesavage JA. Behavioral improvement with relaxation training in senile dementia. Clin Gerontol. 1982;1:45–49. [Google Scholar]
- 38.Rosnow RL, Rosenthal R, Rubin DB. Contrasts and correlations in effect-size estimation. Psychol Sci. 2000;11:446–453. doi: 10.1111/1467-9280.00287. [DOI] [PubMed] [Google Scholar]
- 39.Shadish WR, Robinson L, Lu C. ES: A computer program and manual for effect size calculation. Minneapolis, MN: Assessment Systems; 1999. [Google Scholar]
- 40.De Berry S. An evaluation of progressive muscle relaxation on stress related symptoms in a geriatric population. Int J Aging Hum Devel. 1981;14:255–269. doi: 10.2190/5c1r-9d61-yg2n-a7lv. [DOI] [PubMed] [Google Scholar]
- 41.De Berry S. The effects of meditation-relaxation on anxiety and depression in a geriatric population. Psychother: Theory, Res Prac. 1982;19:512–521. [Google Scholar]
- 42.De Berry S, Davis S, Reinhard KE. A comparison of meditation-relaxation and cognitive/behavioral techniques for reducing anxiety and depression in a geriatric population. J Geriatr Psychiatry. 1989;22:231–247. [PubMed] [Google Scholar]
- 43.Dunn VK, Sacco WP. Psychometric evaluation of the Geriatric Depression Scale and the Zung Self-Rating Depression Scale using an elderly community sample. Psychol Aging. 1989;4:125–126. doi: 10.1037//0882-7974.4.1.125. [DOI] [PubMed] [Google Scholar]
- 44.Mohlman J, Gorman JM. The role of executive functioning in CBT: a pilot study with anxious older adults. Behav Res Ther. 2005;43:447–465. doi: 10.1016/j.brat.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 45.Swales PJ, Solfvin JF, Sheikh JI. Cognitive-behavioral therapy in older panic disorder patients. Am J Geriatr Psychiatry. 1996;4:46–60. doi: 10.1097/00019442-199624410-00006. [DOI] [PubMed] [Google Scholar]
- 46.Spielberger CD, Gorsuch RL, Lushene RE. STAI manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1970. [Google Scholar]
- 47.Scogin F, Rickard HC, Keith S, et al. Progressive and imaginal relaxation training for elderly persons with subjective anxiety. Psychol Aging. 1992;7:419–424. doi: 10.1037//0882-7974.7.3.419. [DOI] [PubMed] [Google Scholar]
- 48.Stanley MA, Beck JG, Glassco JD. Treatment of generalized anxiety in older adults: A preliminary comparison of cognitive-behavioral and supportive approaches. Behav Ther. 1996;27:565–581. [Google Scholar]
- 49.Gorenstein EE, Kleber MS, Mohlman J, et al. Cognitive-behavioral therapy for management of anxiety and medication taper in older adults. Am J Geriatr Psychiatry. 2005;13:901–909. doi: 10.1176/appi.ajgp.13.10.901. [DOI] [PubMed] [Google Scholar]
- 50.Meyer TJ, Miller ML, Metzger RL, et al. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 51.Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 52.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 53.van Belle G. Statistical rules of thumb. New York, NY: Wiley Interscience; 2002. [Google Scholar]; (53) Borkovec TD, Ruscio AM. Psychotherapy for generalized anxiety disorder. J Clin Psychiatry. 2001;62(Suppl 11):37–42. [PubMed] [Google Scholar]
- 54.Sneed JR, Rutherford BR, Rindskopf D, et al. Design makes a difference: A meta-analysis of antidepressant response rates in placebo-controlled versus comparator trials in late-life depression. Am J Geriatr Psychiatry. 2007;15:1–1. doi: 10.1097/JGP.0b013e3181256b1d. [DOI] [PubMed] [Google Scholar]
- 55.Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493–501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- 56.Barrowclough C, King P, Colville J, et al. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol. 2001;69:756–762. doi: 10.1037//0022-006x.69.5.756. [DOI] [PubMed] [Google Scholar]
- 57.Landreville P, Landry J, Baillargeon L, et al. Older adults’ acceptance of psychological and pharmacological treatments for depression. J Gerontol B: Psychol Sci. 2001;56:P285–291. doi: 10.1093/geronb/56.5.p285. [DOI] [PubMed] [Google Scholar]
- 58.Sallis JF, Lichstein KL, Clarkson AD, et al. Anxiety and depression management for the elderly. Int J Behav Geriatrics. 1983;1:3–12. [Google Scholar]
- 59.Dunlop WP, Cortina JM, Vaslow JB, et al. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Meth. 1996;1:170–177. [Google Scholar]
- 60.Radley M, Redston C, Bates F, et al. Effectiveness of group anxiety management with elderly clients of a community psychogeriatric team. Int J Geriatr Psychiatry. 1997;12:79–84. doi: 10.1002/(sici)1099-1166(199701)12:1<79::aid-gps467>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 61.King P, Barrowclough C. A clinical pilot study of cognitive-behavioural therapy for anxiety disorders in the elderly. Behav Psychotherapy. 1991;19:337–345. [Google Scholar]
- 62.Ladouceur R, Leger E, Dugas M, et al. Cognitive-behavioral treatment of generalized anxiety disorder (GAD) for older adults. Int Psychogeriatrics. 2004;16:195–207. doi: 10.1017/s1041610204000274. [DOI] [PubMed] [Google Scholar]
- 63.Mohlman J, Gorenstein EE, Kleber M, et al. Standard and enhanced cognitive-behavioral therapy for late-life generalized anxiety disorder. Am J Geriatr Psychiatry. 2003;11:24–32. [PubMed] [Google Scholar]
- 64.Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71:309–319. doi: 10.1037/0022-006x.71.2.309. [DOI] [PubMed] [Google Scholar]
- 65.Stanley MA, Hopko DR, Diefenbach GJ, et al. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care. Am J Geriatr Psychiatry. 2003;11:92–96. [PubMed] [Google Scholar]
- 66.Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71:31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]