Abstract
Cardiovascular magnetic resonance is a noninvasive imaging modality that provides superior anatomical and functional information in the absence of ionizing radiation. The cardiovascular magnetic resonance imaging program has been active at the Quebec Heart Institute at Laval Hospital for two years, now providing advanced imaging studies to over 42 referral centres from eastern and central Quebec as well as providing training for national and international fellows. The program benefits from the collborative work of cardiologists and radiologists, who both bring to the table their unique expertise. The following text reviews current clinical applications useful in the daily practice of the cardiovascular specialist.
Keywords: Magnetic resonance imaging, Myocardial ischemia, Myocardial viability, Noninvasive imaging
Abstract
La résonance magnétique cardiovasculaire est une modalité d’imagerie non effractive qui procure des informations anatomiques et fonctionnelles supérieures en l’absence d’irradiation ionisante. Un programme d’imagerie par résonance magnétique cardiovasculaire est en place à l’Institut de cardiologie de Québec à l’hôpital Laval depuis deux ans, fournissant maintenant des épreuves d’imagerie de pointe à plus de 42 centres de référence de l’Est du Québec et assurant la formation de fellows d’ici et d’ailleurs. Le programme bénéficie de la collaboration des cardiologues et des radiologues qui s’enrichissent mutuellement de leur savoir-faire respectif. Le texte qui suit passe en revue les applications cliniques actuelles utilisées dans la pratique quotidienne du cardiologue.
Cardiovascular magnetic resonance (CMR) has found widespread use as an important tool in the cardiologists’ armamentarium over the past decade, mainly because of its superior diagnostic accuracy and ability to perform complete anatomical and functional assessment in a single study without ionizing radiation. The present paper reviews specific applications of CMR that may be useful for the clinical cardiologist who is less familiar with this imaging modality (Table 1).
TABLE 1.
Summary table of common indications for cardiovascular magnetic resonance studies
|
Coronary artery disease |
|
|
Valvular heart disease (native or prosthesis) |
|
|
Cardiomyopathy |
|
|
Arrhythmia |
|
|
Congenital heart disease |
|
|
Research applications |
|
THEORETICAL AND PRACTICAL CONCEPTS (1,2)
Magnetic resonance imaging (MRI) is based on the detection of protons (1H) in water and fat in the body. 1H in water contain molecular magnets that align with the magnetic field of the MRI scanner. The intrinsic angular momentum of 1H results in precession (or rotation) around the axis of the scanner’s magnetic field, referred to as ‘spin’. When a weaker perpendicular field is applied transiently, 1H spins rotate together, emitting a coherent oscillating signal that decays in amplitude and coherence with time. The decays in amplitude (T1 relaxation) and coherence (T2 relaxation) are unique to each specific tissue and generate radiofrequency energy. Receiver coils positioned near the region of interest collect radiofrequency signals to gather information on tissue, which are translated into an image.
In practical terms, patient preparation begins by confirming the absence of major contraindications (cerebrovascular clips, cochlear implants, ocular metallic fragments, and most pacemakers and defibrillators). Many coronary and peripheral stents are safe for CMR immediately after implantation, as are several nitinol-based devices, such as septal occluders (3). In view of the fact that gadolinium (Gd)-based contrast agents used for CMR are comparable with iodine-based agents with regard to nephrotoxicity, serum creatinine must be determined before considering CMR, although a much smaller volume of agent (20 mL to 40 mL) is used in contrast MRI. Patients undergoing CMR stress should withhold heart rate-reducing medications or caffeine-containing substances. A 20-gauge intravenous catheter is positioned in the patient’s arm vein, and patients are fitted with vectorcardiographic chest leads for electrocardiogram gating, as well as a flexible phased array cardiac receiver coil on the precordium. Brachial cuff pressure and digital pulse oximetry are measured throughout. Visual and auditory communication are maintained. During the 20 min to 45 min examination (depending on the indication), most imaging sequences are performed during repeated 6 s to 12 s breath-holds on expiration.
CARDIOVASCULAR ANATOMY AND FUNCTION
CMR combines excellent tissue contrast with superior spatial and temporal resolution, providing images of exceptional quality throughout the cardiac cycle, enabling accurate volumetric quantification for global and regional functional analysis. Myocardial tagging offers insights into wall strain patterns, revealing intrinsic mechanisms of ventricular function. Velocity-encoding techniques accurately assess blood flow to measure valvular function and shunts, and calculate pressure gradients.
Standardized measurements of global and regional left and right ventricular function are commonly performed in sequential short-axis slices of 6 mm to 10 mm thickness with 0 mm to 10 mm gaps between slices. In end-systole and end-diastole, endocardial and epicardial borders are traced semiautomatically in each of the eight to 12 short-axis slices, and the left ventricle is segmented according to the 17-segment model of the American Heart Association. Applying the modified Simpson’s rule, left and right ventricular end-systolic and end-diastolic volumes, ejection fraction and cardiac output are obtained. Left ventricular mass is derived from volume. Left ventricular regional wall thickening is determined per segment. Volumetric ventricular quantification is more reliable and reproducible than the geometric assumptions used in planar imaging techniques (contrast ventriculography, radionuclide scintigraphy and echocardiography) (4). CMR has become the gold standard for the assessment of right ventricular structure and function, a key component in the evaluation of many congenital heart conditions, as well as an important prognostic risk factor after myocardial infarction (Figure 1) (5). Diastolic function is assessed by velocity-encoding CMR and derived from rates of inflow of blood into the left and right ventricles. Velocity-encoding CMR also provides the basis for pressure gradient and flow measurements pivotal in the evaluation of valvular stenosis and insufficiency, as well as shunt estimation in congenital cardiovascular disease (Figure 2). The ability to precisely determine cardiovascular anatomy and physiology and to provide three-dimensional models that can be rotated into all planes is becoming central to invasive cardiologists and surgeons in the planning of therapeutic procedures.
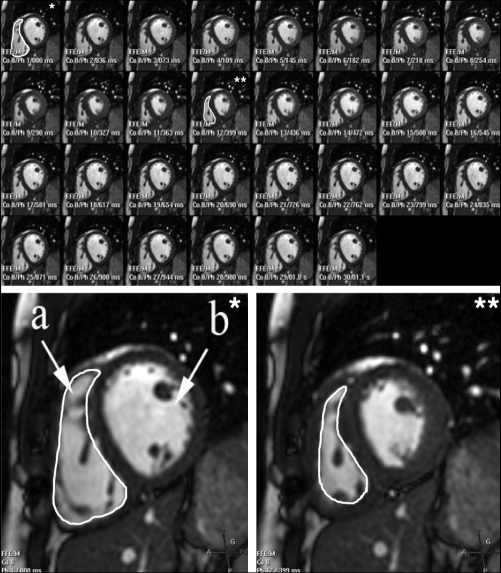
Figure 1).
Volumetric method for the measurement of right ventricular function. Contiguous 8 mm thick slices of the ventricles (right ventricle [a] and left ventricle [b]) in dynamic short-axis allow precise measurement of end-diastolic (bottom left) and matching end-systolic (bottom right) endocardial areas. Modified Simpson’s rule allows the measurement of end-diastolic and end-systolic volumes, and the precise calculation of ejection fraction
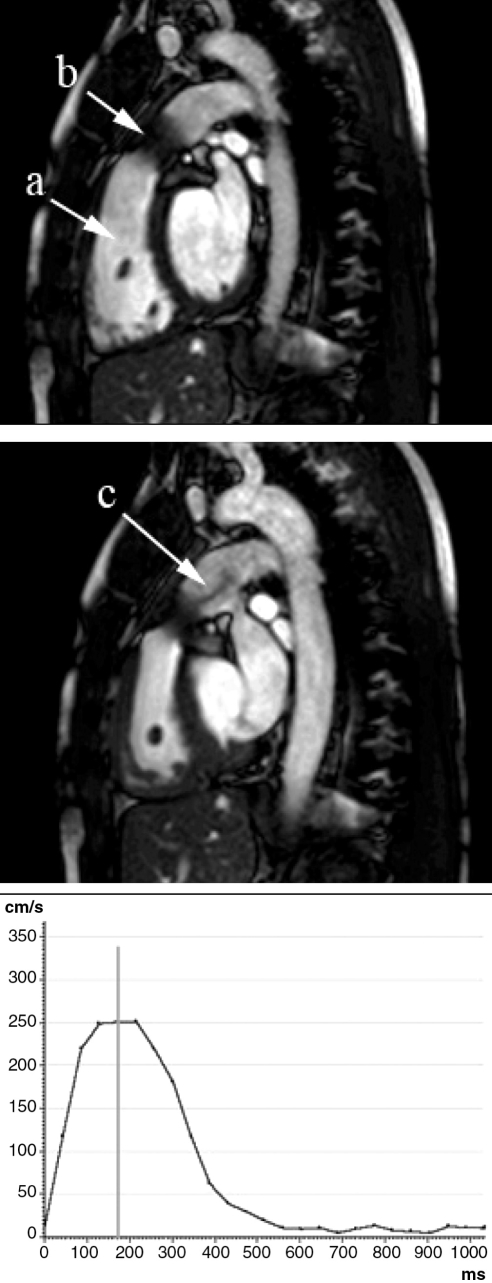
Figure 2).
Assessment of valvular stenosis. Modified sagittal end-diastolic (top) and end-systolic (middle) dynamic images illustrating right ventricle (a) and percutaneously implanted pulmonary bioprosthesis (b). Acceleration jet in the pulmonary artery (c) indicates persisting gradient measured by a velocity-encoded magnetic resonance velocity graph (bottom)
MYOCARDIAL ISCHEMIA
Flow-limiting coronary artery stenosis is identified as a perfusion deficit or a wall motion abnormality inducible by stress. One unique feature of CMR is that it accurately identifies both perfusion and wall motion defects, potentially improving diagnostic accuracy. Pharmacological stress is induced by increasing heart rate and contractility (dobutamine), or by vasodilation (adenosine or dipyridamole), applying protocols previously validated for other stress imaging techniques.
Gd contrast first-pass CMR perfusion imaging provides superior spatial (in the order of 2 mm2) and temporal resolution for the diagnosis of ischemic heart disease. The contrast media is injected as an intravenous bolus and circulates to the coronary arteries, increasing the T1 signal in perfused myocardium. T1-weighted pulse sequences identify perfusion deficits at first pass during stress (hyperemia) and rest, reflecting either hypoperfused viable myocardium or scar tissue (Figure 3). Late-enhancement imaging is performed 10 min later to differentiate hypoperfused viable myocardium from scar (discussed later). Analysis is performed according to the American Heart Association’s 17-segment model by visual assessment, or quantitative measurement of peak signal intensity or single change over time (6). CMR first-pass perfusion imaging has been repeatedly validated in animal models (7). CMR is significantly superior to single-photon emission computed tomography at identifying greater than 70% diameter stenoses on quantitative coronary angiography (areas under the receiver operating characteristic curves of 0.90 for CMR versus 0.73 for single-photon emission computed tomography) (8). CMR yielded a sensitivity of 90% and a specificity of 85% for the detection of angiographically significant coronary stenoses. When compared with positron emission tomography imaging, stress perfusion CMR yielded a sensitivity of 91% and a specificity of 94%, with an area under the receiver operating characteristic curve of 0.93 (9). The clinical usefulness of stress perfusion CMR has been validated in multicentre studies (10).
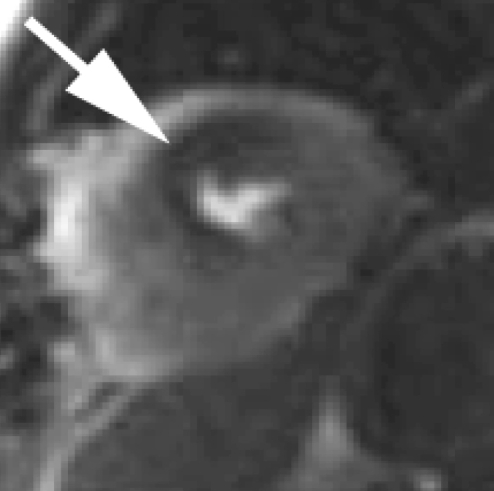
Figure 3).
First-pass gadolinium perfusion study. Hypoperfusion is evidenced by the dark area indicated by the white arrow in contrast to the lighter areas of the myocardium, where gadolinium contrast indicates perfused myocardium
Diagnosis of ischemic heart disease is also performed with CMR by the identification of inducible wall motion abnormalities. Segmental wall motion and systolic wall thickening are compared at rest and at each successive stage of stress. Dobutamine stress echocardiography has been validated as a useful screening tool for patients with suspected coronary artery disease, but it is limited by nondiagnostic studies in up to 10% to 15% of patients (11). Dobutamine stress CMR has been shown to be superior to stress echocardiography for sensitivity (86% versus 74%), specificity (86% versus 70%) and accuracy (86% versus 73%) for the detection of myocardial ischemia (12). Furthermore, CMR yields diagnostic studies in 94% of patients with nondiagnostic stress echocardiography (13). Ultimately, CMR identifies, in a single study, both reversible perfusion and reversible functional defects.
In addition to stress studies for the identification of clinically significant coronary artery stenosis, rest first-pass perfusion CMR is useful for the identification of microvascular dysfunction and obstruction, and has demonstrated prognostic value (14).
MYOCARDIAL NECROSIS AND VIABILITY
In daily practice, delayed-enhancement CMR (DE-CMR) is used to differentiate stunned from infarcted myocardium in acute patients, and to predict response to coronary revascularization in chronic left ventricular systolic dysfunction. While several techniques extrapolate myocardial necrosis from wall thickness or thickening, perfusion or tracer uptake, or improvements in contraction with dobutamine, CMR is unique in precisely identifying the presence or absence of living cardiomyocytes with superior spatial resolution. DE-CMR has been extensively validated in animal and human studies. When compared with the fine details and area of necrosis seen with triphenyl tetrazolium chloride staining on ex vivo specimens, DE-CMR precisely mirrored histological findings in animal models (15). While both acute myocardial infarction (AMI) and severe ischemia manifest loss of systolic function, necrosis identified by DE-CMR consistently differentiates myocardial stunning from infarct (15). Discrimination of reversible from irreversible injury is achieved by DE-CMR in both acute and chronic settings (16). Infarct size determined by DE-CMR is highly reproducible and correlates closely with cardiac enzyme rise in the setting of AMI (17,18). The transmural extent of necrosis identified by DE-CMR is strongly correlated with improvement in global and regional systolic function, including recovery from stunning in AMI and success of revascularization in chronic ischemic cardiomyopathy (19,20). Superior spatial resolution of CMR allows identification of as little as 2 g of necrosis, compared with the minimum requirement of 10 g for reproducible identification of necrosis by nuclear techniques (21). Previously unrecognized microinfarction and subendocardial necrosis are identified, portending important implications (22).
DE-CMR is routinely performed at Laval Hospital (Sainte-Foy, Quebec) in patients with AMI or chronic ischemic cardiomyopathy to predict the success of revascularization and determine the best therapeutic strategy. After a 10 min delay, intravenous Gd-diethylenetriamine pentaacetic acid (DTPA) distributes to where myocardial cells are absent (scar in chronic infarct) or where their sarcolemmal membranes are altered (necrosis in acute infarct). In T1-weighted imaging, inversion time is set to null normal myocardium, and Gd-DTPA-rich scar or necrosis is viewed as a bright signal at least 2 SDs brighter than remote normal myocardium (and typically at least five times brighter) (Figure 4). Adjustment of the inversion time is straightforward and critical in insuring reproducibility of infarct size measurements (17). Each segment is attributed a transmural score for necrosis (0%; 1% to 25%; 26% to 50%; 51% to 75%; 76% to 100%). Potential for functional recovery is determined based on transmurality of necrosis, with greater than 50% transmural necrosis carrying less than 20% potential for improvement, based on the work of Kim et al (20).
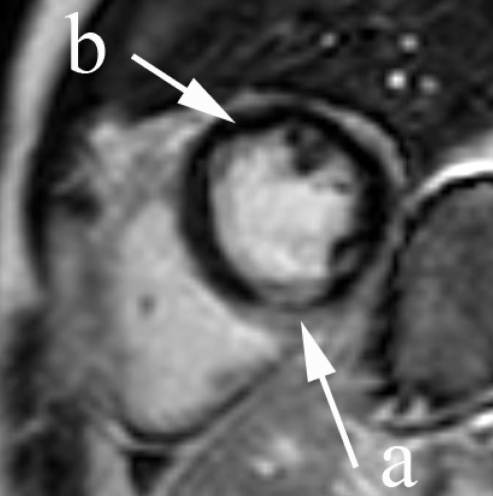
Figure 4).
Delayed-enhancement cardiovascular magnetic resonance for identification of myocardial necrosis and determination of viability. Normal myocardium is nulled, or black (b), while gadolinium contrast appears bright in infarcted myocardium (a). Transmural necrosis is identified at the inferior and inferoseptal segments of the midventricle, denoting the absence of viability. The black stripe crossing the midportion of the bright, infarcted myocardium corresponds to microvascular obstruction
ATHEROSCLEROTIC PLAQUE BURDEN AND CHARACTERIZATION
Compared with histology, CMR provides accurate assessment of the vessel lumen, vessel wall, and atherosclerotic plaque areas and volumes, with errors within 5% and high interobserver reproducibility (23,24). Arguably more important than atherosclerotic burden is the biology within plaque. Features of plaque-causing acute thrombosis include a large, lipid-rich core, thin fibrous cap and active inflammation (25). CMR has the ability to characterize tissue within plaque (ie, lipid, fibrous, calcified tissues and hemorrhage) (26), as well as to identify the presence of inflammatory cells (27,28). Paramagnetic markers of molecular processes within plaque detectable by CMR are a burgeoning area of intense research (29). At present, characterization of atherosclerosis by CMR is mostly restricted to larger vessels close to the surface of the body. Work is in progress to develop novel receiver antennas able to image atherosclerosis from the body surface or from within using intravascular MRI to achieve an optimal signal to noise ratio and to identify vulnerable characteristics of smaller arteries deep within the body (30).
CONCLUSIONS
CMR has become a key component in the daily care of patients with proven or suspected cardiovascular disease. Clinical cardiologists now have a powerful ally to aid in diagnosis, risk stratification and the optimization of treatment strategies.
Footnotes
SUPPORT: The authors are partly supported by La fondation de l’institut de cardiologie de Québec.
REFERENCES
- 1.Lauterbur PC. Image formation by induced local interactions: Examples employing nuclear magnetic resonance. Nature. 1973;242:190–1. [PubMed] [Google Scholar]
- 2.Mansfield P, Morris P. NMR Imaging in Biomedicine. New York: Academic Press; 1982. [Google Scholar]
- 3.MRIsafety.com. <www.MRIsafety.com> (Version current at August 2, 2007).
- 4.Chuang ML, Hibberd MG, Salton CJ, et al. Importance of imaging method over imaging modality in noninvasive determination of left ventricular volumes and ejection fraction: Assessment by two- and three-dimensional echocardiography and magnetic resonance imaging. J Am Coll Cardiol. 2000;35:477–84. doi: 10.1016/s0735-1097(99)00551-3. [DOI] [PubMed] [Google Scholar]
- 5.Larose E, Ganz P, Reynolds HG, et al. Right ventricular dysfunction assessed by cardiovascular magnetic resonance imaging predicts poor prognosis late after myocardial infarction. J Am Coll Cardiol. 2007;49:855–62. doi: 10.1016/j.jacc.2006.10.056. [DOI] [PubMed] [Google Scholar]
- 6.Keijer JT, van Rossum AC, van Eenige MJ, et al. Magnetic resonance imaging of regional myocardial perfusion in patients with single-vessel coronary artery disease: Quantitative comparison with (201)Thallium-SPECT and coronary angiography. J Magn Reson Imaging. 2000;11:607–15. doi: 10.1002/1522-2586(200006)11:6<607::aid-jmri6>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 7.Schwitter J, Saeed M, Wendland MF, et al. Assessment of myocardial function and perfusion in a canine model of non-occlusive coronary artery stenosis using fast magnetic resonance imaging. J Magn Reson Imaging. 1999;9:101–10. doi: 10.1002/(sici)1522-2586(199901)9:1<101::aid-jmri14>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 8.Ishida N, Sakuma H, Motoyasu M, et al. Noninfarcted myocardium: Correlation between dynamic first-pass contrast-enhanced myocardial MR imaging and quantitative coronary angiography. Radiology. 2003;229:209–16. doi: 10.1148/radiol.2291021118. [DOI] [PubMed] [Google Scholar]
- 9.Schwitter J, Nanz D, Kneifel S, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: A comparison with positron emission tomography and coronary angiography. Circulation. 2001;103:2230–5. doi: 10.1161/01.cir.103.18.2230. [DOI] [PubMed] [Google Scholar]
- 10.Giang TH, Nanz D, Coulden R, et al. Detection of coronary artery disease by magnetic resonance myocardial perfusion imaging with various contrast medium doses: First European multi-centre experience. Eur Heart J. 2004;25:1657–65. doi: 10.1016/j.ehj.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 11.Geleijnse ML, Fioretti PM, Roelandt JR. Methodology, feasibility, safety and diagnostic accuracy of dobutamine stress echocardiography. J Am Coll Cardiol. 1997;30:595–606. doi: 10.1016/s0735-1097(97)00206-4. [DOI] [PubMed] [Google Scholar]
- 12.Nagel E, Lehmkuhl HB, Bocksch W, et al. Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: Comparison with dobutamine stress echocardiography. Circulation. 1999;99:763–70. doi: 10.1161/01.cir.99.6.763. [DOI] [PubMed] [Google Scholar]
- 13.Hundley WG, Hamilton CA, Thomas MS, et al. Utility of fast cine magnetic resonance imaging and display for the detection of myocardial ischemia in patients not well suited for second harmonic stress echocardiography. Circulation. 1999;100:1697–702. doi: 10.1161/01.cir.100.16.1697. [DOI] [PubMed] [Google Scholar]
- 14.Yan AT, Gibson CM, Larose E, et al. Characterization of microvascular dysfunction after acute myocardial infarction by cardiovascular magnetic resonance first-pass perfusion and late gadolinium enhancement imaging. J Cardiovasc Magn Reson. 2006;8:831–7. doi: 10.1080/10976640600778049. [DOI] [PubMed] [Google Scholar]
- 15.Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 16.Rehwald WG, Fieno DS, Chen EL, Kim RJ, Judd RM. Myocardial magnetic resonance imaging contrast agent concentrations after reversible and irreversible ischemic injury. Circulation. 2002;105:224–9. doi: 10.1161/hc0202.102016. [DOI] [PubMed] [Google Scholar]
- 17.Mahrholdt H, Wagner A, Holly TA, et al. Reproducibility of chronic infarct size measurement by contrast-enhanced magnetic resonance imaging. Circulation. 2002;106:2322–7. doi: 10.1161/01.cir.0000036368.63317.1c. [DOI] [PubMed] [Google Scholar]
- 18.Ingkanisorn WP, Rhoads KL, Aletras AH, Kellman P, Arai AE. Gadolinium delayed enhancement cardiovascular magnetic resonance correlates with clinical measures of myocardial infarction. J Am Coll Cardiol. 2004;43:2253–9. doi: 10.1016/j.jacc.2004.02.046. [DOI] [PubMed] [Google Scholar]
- 19.Choi KM, Kim RJ, Gubernikoff G, Vargas JD, Parker M, Judd RM. Transmural extent of acute myocardial infarction predicts long-term improvement in contractile function. Circulation. 2001;104:1101–7. doi: 10.1161/hc3501.096798. [DOI] [PubMed] [Google Scholar]
- 20.Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–53. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 21.Larose E. Below radar: Contributions of cardiac magnetic resonance to the understanding of myonecrosis after percutaneous coronary intervention. Circulation. 2006;114:620–2. doi: 10.1161/CIRCULATIONAHA.106.644732. [DOI] [PubMed] [Google Scholar]
- 22.Kwong RY, Chan AK, Brown KA, et al. Impact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms of coronary artery disease Circulation 20061132733–43. (Erratum in 2006;114:e365). [DOI] [PubMed] [Google Scholar]
- 23.Kang X, Polissar NL, Han C, Lin E, Yuan C. Analysis of the measurement precision of arterial lumen and wall areas using high-resolution MRI. Magn Reson Med. 2000;44:968–72. doi: 10.1002/1522-2594(200012)44:6<968::aid-mrm20>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 24.Fayad ZA, Fuster V, Fallon JT, et al. Noninvasive in vivo human coronary artery lumen and wall imaging using black-blood magnetic resonance imaging. Circulation. 2000;102:506–10. doi: 10.1161/01.cir.102.5.506. [DOI] [PubMed] [Google Scholar]
- 25.Libby P. What have we learned about the biology of atherosclerosis? The role of inflammation. Am J Cardiol. 2001;88(7B):3J–6J. doi: 10.1016/s0002-9149(01)01879-3. [DOI] [PubMed] [Google Scholar]
- 26.Larose E, Kinlay S, Selwyn AP, et al. Improved characterization of atherosclerotic plaques by gadolinium contrast during intravascular magnetic resonance imaging of human arteries Atherosclerosis 2007. (In press) [DOI] [PubMed]
- 27.Yuan C, Mitsumori LM, Beach KW, Maravilla KR. Carotid atherosclerotic plaque: Noninvasive MR characterization and identification of vulnerable lesions. Radiology. 2001;221:285–99. doi: 10.1148/radiol.2212001612. [DOI] [PubMed] [Google Scholar]
- 28.Fayad ZA, Fuster V. Clinical imaging of the high-risk or vulnerable atherosclerotic plaque. Circ Res. 2001;89:305–16. doi: 10.1161/hh1601.095596. [DOI] [PubMed] [Google Scholar]
- 29.Jaffer FA, Libby P, Weissleder R. Molecular and cellular imaging of atherosclerosis: Emerging applications. J Am Coll Cardiol. 2006;47:1328–38. doi: 10.1016/j.jacc.2006.01.029. [DOI] [PubMed] [Google Scholar]
- 30.Larose E, Yeghiazarians Y, Libby P, et al. Characterization of human atherosclerotic plaques by intravascular magnetic resonance imaging. Circulation. 2005;112:2324–31. doi: 10.1161/CIRCULATIONAHA.105.538942. [DOI] [PubMed] [Google Scholar]