Abstract
Background
Lower-extremity injuries constitute the leading cause of trauma hospitalizations among people under the age of 65 years. Rehabilitation has the potential to favorably influence the outcomes associated with traumatic lower-extremity injuries.
Objectives
The objectives of this study were to explore variability in surgeon and physical therapist assessments of the need for physical therapy in patients with traumatic lower-extremity injuries and to determine the factors associated with assessments of need.
Design
This study was a retrospective cohort investigation.
Methods
Participants were 395 patients treated by reconstruction in the Lower-Extremity Assessment Project. They were evaluated at 8 level I trauma centers at 3, 6, and 12 months after hospitalization by an orthopedic surgeon and a physical therapist to determine the need for physical therapy. Analyses included multilevel logistic regression.
Results
Chi-square analyses showed that surgeon and therapist assessments of need differed statistically across trauma centers. Surgeons were more likely to assess a need for therapy at 3 months when participants had low work self-efficacy, impaired knee flexion range of motion (ROM), and weight-bearing limitations and at 6 and 12 months when participants had impaired knee flexion ROM and weight-bearing and balance limitations. Therapists were more likely to assess a need for therapy at 3 months when participants had moderate to severe pain and at 6 and 12 months when participants had low work self-efficacy, pain, impaired knee flexion ROM, and balance limitations.
Conclusions
The results revealed variability in assessments of the need for physical therapy at the provider and trauma center levels. Differences in provider assessments highlight the need for communication and further investigation into the outcomes and timing of physical therapy for the treatment of traumatic lower-extremity injuries.
Lower-extremity injuries constitute the leading cause of trauma hospitalizations among adolescents and adults under the age of 65 years.1–3 Long-term impairments often are significant, with research showing moderate to severe levels of disability, low rates of return to employment, and chronic pain for up to 7 years after injury.4–7 Rehabilitation has the potential to favorably affect these long-term outcomes, but limited research has suggested low levels of use of physical therapy in patients with traumatic lower-extremity injuries.2,3,8–13 Physician referral practices may contribute to the low levels of use of rehabilitation services. The literature on referral to physical therapists has indicated wide variability in referral rates.14–17 Research also has demonstrated variations in physician attitudes toward physical therapy and knowledge of available services.18–20 Overall, these studies on referral patterns have suggested that variations may result in underreferral or inappropriate referral practices.14–20
Concerns about the implications of referral variability for access to services and patient outcomes have prompted researchers to examine the physical therapy referral process. In several studies, the content of physician referral with regard to the provision of specific diagnoses and therapeutic procedures has been examined to provide a better understanding of the professional role of physical therapists.19,21–23 Findings consistently have shown that limited referral information is provided to physical therapists and that physicians perceive therapists as technicians rather than as professional colleagues.21 Research also has explored patient-related factors associated with referral to physical therapists, with evidence supporting associations with the age and sex of patients, injury severity, and insurance status.14–21 However, patient-related factors explain only a small proportion of the observed variations in physical therapy referral rates.14,15,24 To our knowledge, in only one study have the clinical factors associated with referral to physical therapists been examined. Freburger et al15 found that scores on the Oswestry Disability Index and on the bodily pain, physical function, and role–physical subscales of the Medical Outcomes Study 36-Item Health Survey Questionnaire were associated with referral for the treatment of spine disorders. These authors also reported significant variations in physical therapy referral rates from center to center.
On the basis of the poor long-term outcomes of patients with traumatic lower-extremity injuries and the potential for significant provider and site variations in referral practices, the goals of our study were to use the Lower-Extremity Assessment Project (LEAP) database to explore variability in assessments of the need for physical therapy and to compare the factors associated with orthopedic surgeon and physical therapist assessments of need in patients with traumatic lower-extremity injuries. The LEAP database is unique because it allows for comparisons across various centers and of surgeon and therapist clinical decision making. Specifically, we aimed to examine variability in assessments of the need for physical therapy in patients across 8 level I trauma centers and to examine the patient-related, medical, and clinical factors associated with surgeon and physical therapist assessments of the need for physical therapy.
After a review of the literature on both physical therapy referral and outcomes after traumatic lower-extremity injuries, we tested the hypotheses that variability in assessments of the need for physical therapy would exist at the trauma center level and that patients who had traumatic lower-extremity injuries, patients who were not working, and patients who experienced more pain would be more likely to be assessed as needing physical therapy.
Method
For the present study, we used a retrospective cohort design. Data on 395 patients (16–69 years of age) treated by lower-extremity reconstruction were obtained from the LEAP database.
The LEAP was a multicenter, prospective cohort study designed to examine differences in functional outcomes after reconstruction or amputation because of traumatic lower-extremity injuries. A total of 601 patients were enrolled between March 1994 and June 1997 at 8 level I trauma centers (Carolinas Medical Center, Cleveland MetroHealth Medical Center, Harborview Medical Center, North Carolina Baptist Hospital, R. Adams Cowley Shock Trauma Center, Tampa General Hospital, University of Texas Southwestern Medical Center, and Vanderbilt University Medical Center).25 Lower-extremity trauma was defined, as described by Gustilo et al,26 as type IIIB and IIIC fractures, selected type IIIA fractures, dysvascular limbs, major soft tissue injuries, and severe foot or ankle injuries. The most notable exclusion criteria were scores of less than 15 on the Glasgow Coma Scale at admission, spinal cord deficits, prior amputation, third-degree burns, inability to speak English or Spanish, documented psychiatric disorders, and active military duty.4
Participants were evaluated at hospital discharge and at 3, 6, and 12 months after hospitalization. Follow-up assessments included a nurse interview and separate orthopedic surgeon and physical therapist evaluations.
Measurement of Variables
Outcomes.
Outcomes included surgeon and physical therapist assessments of a patient's need for physical therapy and disagreements about assessments of need. At follow-up visits at 3, 6, and 12 months, surgeons and physical therapists conducted separate evaluations of participants. Each provider independently documented either “yes” or “no” as to whether a participant would need physical therapy between that assessment and the next follow-up assessment. A positive, or “yes,” response was considered to be an assessment of the need for physical therapy, and a negative, or “no,” response was considered to be an assessment of no need for physical therapy.
Characteristics of participants.
Data on the age, sex, race, education, health insurance coverage, poverty level, health before injury, and smoking status of the participants during the initial hospitalization were collected. Poverty was calculated by relating total household income to household size and was categorized as follows: not poor—incomes higher than 200% of the federal poverty level defined by the US Census Bureau, nearly poor—incomes within 125% of the federal poverty level, or poor—incomes lower than 125% of the federal poverty level.25,27 Participants rated their health before injury as excellent, good, fair, or poor and were classified as active if they reported involvement in regular exercise at least once per week. Participants were asked if they had any of the following health conditions before injury: asthma, chronic bronchitis, emphysema, arthritis, hypertension, stroke, diabetes, cancer, tuberculosis, or kidney disease. A positive response for at least one of the conditions led to the classification of an individual as having a prior health condition. Participants also were asked if they had ever required medical attention for joint disease, fracture, dislocation, sprain or strain, burn, or ligament injury that involved either leg. A positive response for any of the injury categories indicated a prior leg condition.
At each follow-up assessment, participants reported their use of physical therapy services. Participants were asked at 3 months if they had received physical therapy since hospital discharge and were asked at 6 and 12 months if they had received physical therapy since last speaking with the interviewers.
Characteristics of injuries.
Lower-extremity injuries were classified at the time of admission as tibia shaft or articular fractures, severe ankle or foot injuries, and major soft tissue or dysvascular injuries. The Hannover Fracture Scale28 was used to indicate the extent of bone loss (<2 or >2 cm) and contamination (none, single, multiple, or massive). The Predictive Salvage Index29 was used to categorize bone and muscle injuries as mild, moderate, or severe.
Complications at each follow-up visit were noted, and surgeons recorded whether these complications resulted in a subsequent hospitalization. Fracture healing, as determined from radiographs, was rated as completed healing, progressive healing, or no healing. Edema was described as no edema, mild edema (1+), or moderate to severe edema (2+ to 4+).
Occupational factors.
Preinjury work status was recorded during the initial hospitalization as either working or not working, and current work status was assessed at each follow-up visit. Participants who reported returning to work either full time or part time were categorized as working.
Work self-efficacy was measured in the hospital by asking participants to rate from 1 to 10 how confident they were in their ability to return to work within 1, 3, 6, and 12 months.5 A score of 1 indicated that they were not at all confident, and a score of 10 indicated that they were completely confident. A work self-efficacy score was calculated by multiplying the mean for the 4 levels of confidence by 10. These 4 levels and the scoring method were adapted from self-efficacy scales that were used by Bandura et al30 and Ewart et al31 and that were found to have moderate test-retest reliability and validity, with Pearson correlation coefficients of greater than .80.30,31
Pain.
Participants rated their average daily leg pain from “no pain” to “unbearable pain” by using a visual analog scale (VAS), a horizontal line from 0 to 100 mm. The VAS scores were recorded by measuring the distance from 0 (no pain) to the participant's mark on the line. The scores were categorized as no pain (0–4 mm), mild pain (5–44 mm), moderate pain (45–74 mm), or severe pain (75–100 mm).32
Disability.
The Sickness Impact Profile (SIP) was administered to measure self-reported health status, with a score of greater than 20 indicating severe disability.33 The SIP consists of 136 items grouped into 12 categories and 2 dimensions of health (physical and psychosocial). The physical dimension comprises the ambulation, mobility, and body care and movement categories, and the psychosocial dimension includes the communication, alertness, and emotional behavior categories. Scores can range from 0 to 100 for the overall instrument, each category, and the 2 dimensions of health. The SIP has been shown to have high test-retest reliability (r=.92) and internal consistency (r=.94), a multidimensional perspective on function, and sensitivity to small differences in function.34,35
Weight bearing and balance.
The weight-bearing status of the injured leg was documented at each follow-up visit as full weight bearing, partial weight bearing, toe touch weight bearing, or non–weight bearing. Two categories were used: full weight bearing and not full weight bearing (including partial weight bearing and toe touch weight bearing).
Balancing on the involved limb was assessed with an unsupported single-leg stance task. Participants were asked to stand on 1 leg with their eyes open and their arms across their chest for 30 seconds. The number of seconds a participant was able to stand before dropping the other leg was recorded. A score of 0 seconds was attributed to participants who were unable to perform the task. Participants were classified as either being able to perform the balance task (standing for ≥30 seconds) or being unable to perform the task (standing for <30 seconds). A score of less than 30 seconds in an unsupported single-leg stance task has been defined as functionally poor.36,37
Range of motion (ROM).
Participants were placed in the supine position and asked to actively move the hip and knee joints through flexion and the ankle joint through dorsiflexion (DF) and plantar flexion (PF). In the prone position, participants were asked to lift the hip into extension. The ROM of the hip and knee joints was measured with a universal goniometer, and the ROM of the ankle was measured with a small, full-circle goniometer.38 High intrarater reliability of the goniometers for knee ROM and ankle ROM has been reported, with intraclass correlation coefficients ranging from .97 to .99 for the knee and from .82 to .86 for the ankle.39,40 The starting and ending positions of each joint, as recommended by the American Academy of Orthopaedic Surgeons, were used to appropriately record measurements; norms were determined on the basis of the averages published by the American Academy of Orthopaedic Surgeons.41
Strength (force-generating capacity).
Hip flexion and extension, knee flexion and extension, and ankle DF and PF strength were measured with a Force Evaluation and Testing System (model FET5000) force gauge* anchored to a table; this instrument previously was found to have acceptable levels of interrater and intrarater reliability.42,43 Participants were placed into antigravity positions and asked to apply maximum force against the forceplates. A force transducer produced an output that represented each participant's force, and the output was displayed on a digital panel meter. Three measurements of each motion of the involved and uninvolved limbs were recorded. An average strength score for the involved and uninvolved limbs and the ratio of the maximum effort of the injured limb to that of the uninjured limb were calculated.
Data Analysis
Descriptive statistics explored the percentages of participants needing physical therapy, as assessed by surgeons and physical therapists at each follow-up visit. Chi-square tests were used to compare surgeon and physical therapist assessments of the need for physical therapy in participants across the 8 level I trauma centers.
Two outcomes were of interest: surgeon assessment of a participant's need for physical therapy and physical therapist assessment of a participant's need for therapy. Separate multilevel logistic regression analyses (1 for surgeon assessment of need and 1 for physical therapist assessment of need) were performed for the 3-, 6-, and 12-month follow-up visits. Random effects were included in all analyses to account for the clustering of visits at the provider and center levels. Subsequently, 2-level random-intercept models were analyzed with the generalized linear latent and mixed model (GLLAMM) macro in the Stata statistical package, version 9.0.†,44,45 The GLLAMM macro produced estimates of the variance of the random effects for providers (τ2) and centers (ω2) but not for participants (σ2). The fractions of the variance attributable to differences between providers and differences between centers were calculated by dividing the variance of the specific random effect by the total variance (σ2 + τ2 + ω2) in the model. The variance for σ2 was considered to be π2/3 for calculation purposes.44,45
Separate multilevel bivariate regression analyses at each of the 3 follow-up visits included the following variables for the participants: age, sex, race, education, insurance status, poverty status, smoking status, prior health status, activity level, and prior health conditions and leg injuries; injury type, bone loss, contamination, complications, subsequent hospitalizations, and bone and muscle damage; work self-efficacy and prior and current work status; and fracture healing, edema level, VAS pain score, SIP score, weight-bearing status, single-leg balancing on the involved leg, hip and knee flexion and extension ROM, ankle DF and PF ROM, dynamometric strength measurements of hip and knee flexion and extension and ankle DF and PF, and use of physical therapy services. Independent variables that had P values of less than or equal to .25 (Wald test) or that were considered to be relevant to the assessment decision were identified and entered into multiple-variable mixed-model forward and backward logistic regression models.44 The .25 level was used as a screening criterion to allow for the possibility that several variables, each of which may be weakly associated with the outcome, may become important predictors when placed in a model together.46 Patient-related factors (sex, race, insurance status, and prior physical therapy), occupational factors (work status and self-efficacy), injury-related factors (injury severity, fracture healing, and edema level), and clinical factors (VAS pain score, weight-bearing status, balance, knee flexion and extension ROM and strength, and ankle DF and PF strength) were entered as separate groups.
Likelihood ratio tests were conducted to remove the least significant covariates, and models also were compared with goodness-of-fit tests. Multicollinearity was explored after regression with the variance inflation factor. Variables that had P values of less than .05 or that were relevant from a theoretical (participant's sex, race, insurance status, and prior physical therapy) or clinical (injury severity and work status) perspective were retained. The stability of the final model was tested by adding back in each excluded variable one at a time.
Overall, missing data represented less than 5% of the following variables: self-efficacy, edema level, VAS pain score, balance, hip flexion and extension ROM and strength, knee flexion and extension ROM and strength, and ankle DF and PF ROM and strength. Missing data were processed by multiple imputation with regression models that imputed the missing values as a function of the other covariates. More specifically, each regression model was analyzed 5 times, and the results were combined to produce a final estimate for the missing values.47,48
Role of the Funding Source
This research was supported with funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (ROI-AR42659); the Johns Hopkins Education and Research Center for Occupational Safety and Health at the Johns Hopkins Bloomberg School of Public Health, which is sponsored by the National Institute for Occupational Safety and Health (T42OH00842428); and the Johns Hopkins Center for Injury Research and Policy at the Johns Hopkins Bloomberg School of Public Health, which is funded by the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (CE000198-03).
Results
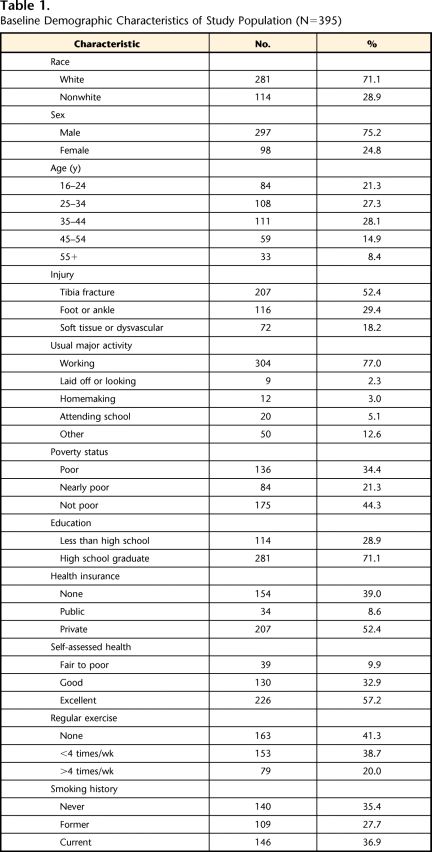
Selected demographic characteristics of the study population are shown in Table 1. A complete description of this population can be found elsewhere.4,25 Most participants were white (71%), were men (75%), and were between 25 and 54 years of age (70%). Approximately 50% of injuries occurred through motor vehicle and motorcycle collisions. The distribution of injuries included tibia fractures (52.4%), severe foot or ankle injuries (29.4%), and major soft tissue or dysvascular injuries (18.2%).
Table 1.
Baseline Demographic Characteristics of Study Population (N=395)
Seventy-nine percent of the participants and 75% of the participants were assessed as needing physical therapy by surgeons and by physical therapists, respectively, at the 3-month follow-up visit. The need for physical therapy, as assessed by surgeons, steadily declined, with 52% of the participants needing therapy at 6 months and 28% of the participants needing therapy at 12 months. In comparison, physical therapists found that 70% and 47% of the participants needed therapy at 6 months and at 12 months, respectively.
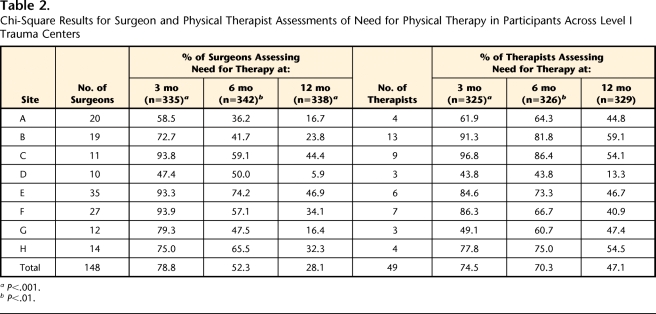
Chi-square analyses were used to test variability in assessments of the need for physical therapy in participants across the 8 level I trauma centers; these analyses revealed that surgeon assessments of need differed statistically across sites at the 3-, 6-, and 12-month follow-up visits (P<.01) (Tab. 2). Surgeon assessments of the need for physical therapy ranged from 94% to 47%, 74% to 36%, and 47% to 6% at the 3-, 6-, and 12-month follow-up visits, respectively. Physical therapist assessments of need differed statistically across sites at the 3- and 6-month follow-up visits (P<.01). The ranges of physical therapist assessments were 97% to 44%, 86% to 44%, and 59% to 13% at the 3-, 6-, and 12-month follow-up visits, respectively. The centers had different numbers of surgeons and physical therapists participating in the study; some centers had fewer than 15 surgeons and 3 or 4 therapists, whereas others had more than 20 surgeons and 5 therapists.
Table 2.
Chi-Square Results for Surgeon and Physical Therapist Assessments of Need for Physical Therapy in Participants Across Level I Trauma Centers
aP<.001.
bP<.01.
Factors Associated With Assessments of Need for Physical Therapy at 3 Months
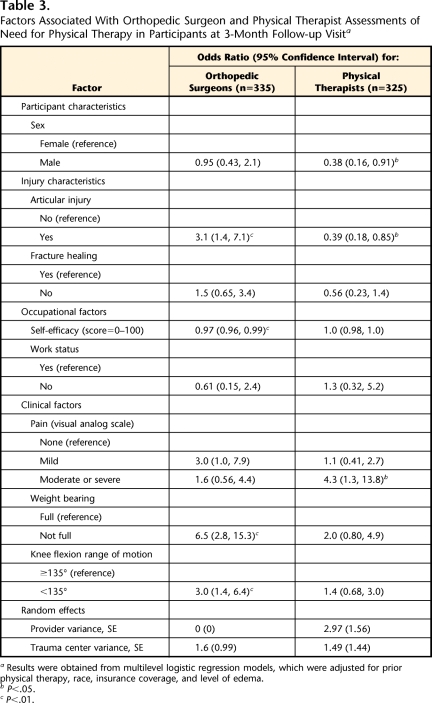
Table 3 shows multiple-variable multilevel logistic regression results for both surgeon and physical therapist assessments of the need for physical therapy at the 3-month follow-up visit.
Table 3.
Factors Associated With Orthopedic Surgeon and Physical Therapist Assessments of Need for Physical Therapy in Participants at 3-Month Follow-up Visita
Results were obtained from multilevel logistic regression models, which were adjusted for prior physical therapy, race, insurance coverage, and level of edema.
bP<.05.
cP<.01.
Characteristics of participants.
The sex of the participants was statistically associated with therapist assessments of the need for therapy, with men being assessed as needing therapy less often than women (odds ratio [OR]=0.38, P<.05).
Characteristics of injuries.
Surgeons assessed participants with articular injuries (OR=3.1, P<.01) as needing therapy more often than participants with nonarticular injuries, whereas therapists assessed participants with articular injuries (OR=0.39, P<.05) as needing therapy less often than participants with nonarticular injuries.
Occupational factors.
Higher work self-efficacy beliefs were negatively associated with surgeon assessments of the need for physical therapy (OR=0.97, P<.01).
Clinical factors.
No association was found between surgeon assessments of need and participants’ VAS pain scores, but physical therapists were more likely to assess participants as needing therapy when they had moderate to severe pain (OR=4.3, P<.05) rather than no pain. However, participants with weight-bearing limitations were more likely to be assessed as needing therapy by surgeons (OR=6.5, P<.01), whereas no association was found with therapist assessments. Impaired knee flexion ROM was statistically associated with surgeon assessments of the need for physical therapy (OR=3.0, P<.01).
Random effects.
The fractions of the variance attributable to nonmeasured provider characteristics were 0% in the surgeon assessment model and 38% in the therapist assessment model. Trauma center characteristics explained 33% and 19% of the variance in the surgeon and therapist models, respectively.
Factors Associated With Assessments of Need for Physical Therapy at 6 Months
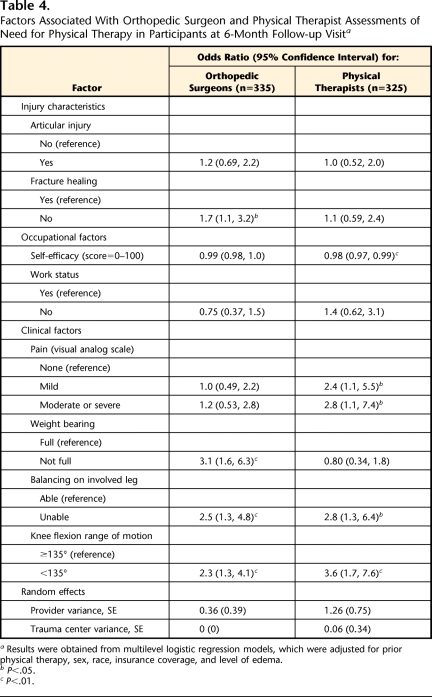
Table 4 shows multiple-variable multilevel logistic regression results for both surgeon and physical therapist assessments of the need for physical therapy at the 6-month follow-up visit.
Table 4.
Factors Associated With Orthopedic Surgeon and Physical Therapist Assessments of Need for Physical Therapy in Participants at 6-Month Follow-up Visita
Results were obtained from multilevel logistic regression models, which were adjusted for prior physical therapy, sex, race, insurance coverage, and level of edema.
bP<.05.
cP<.01.
Characteristics of injuries.
Progressive healing or no fracture healing (OR=1.7) was statistically associated with surgeon assessments of the need for physical therapy (P<.05).
Occupational factors.
Higher work self-efficacy beliefs were negatively associated with therapist assessments of the need for physical therapy (OR=0.98, P<.01).
Clinical factors.
No association was found between surgeon assessments of need and participants’ VAS pain scores, but physical therapists were more likely to assess participants as needing therapy when they had mild pain (OR=2.4, P<.05) or moderate to severe pain (OR=2.8, P<.05) rather than no pain. However, participants with weight-bearing limitations were more likely to be assessed as needing therapy by surgeons (OR=3.1, P<.01), whereas no association was found with therapist assessments. Limitations of the involved leg in the single-leg balance task and impaired knee flexion ROM were statistically associated with both surgeon and therapist assessments of the need for physical therapy (P<.05).
Random effects.
The fractions of the variance attributable to nonmeasured provider characteristics were 10% in the surgeon assessment model and 27% in the therapist assessment model. Trauma center characteristics explained 0% and 1% of the variance in the surgeon and therapist models, respectively.
Factors Associated With Assessment of Need for Physical Therapy at 12 Months
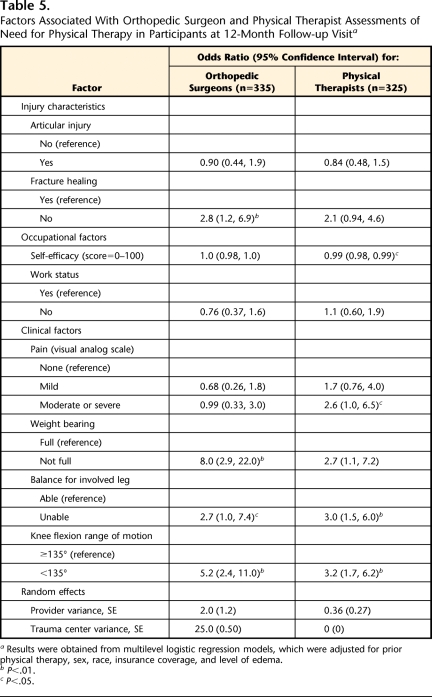
Table 5 shows multiple-variable multilevel logistic regression results for both surgeon and physical therapist assessments of the need for physical therapy at the 12-month follow-up visit.
Table 5.
Factors Associated With Orthopedic Surgeon and Physical Therapist Assessments of Need for Physical Therapy in Participants at 12-Month Follow-up Visita
Results were obtained from multilevel logistic regression models, which were adjusted for prior physical therapy, sex, race, insurance coverage, and level of edema.
bP<.01.
cP<.05.
Characteristics of injuries.
Progressive or no fracture healing (OR=2.8) was statistically associated with surgeon assessments of the need for physical therapy (P<.01).
Occupational factors.
Higher work self-efficacy beliefs were negatively associated with therapist assessments of the need for physical therapy (OR=0.98, P<.05).
Clinical factors.
No association was found between surgeon assessments of need and participants’ VAS pain scores, but physical therapists were more likely to assess participants as needing therapy when they had moderate to severe pain (OR=2.6, P<.05) rather than no pain. However, participants with weight-bearing limitations were more likely to be assessed as needing therapy by surgeons (OR=8.0, P<.01), whereas no association was found with therapist assessments. Limitations of the involved leg in the single-leg balance task and impaired knee flexion ROM were statistically associated with both surgeon and therapist assessments of the need for physical therapy (P<.05).
Random effects.
The fractions of the variance attributable to nonmeasured provider characteristics were 36% in the surgeon assessment model and 10% in the therapist assessment model. Trauma center characteristics explained 5% and 0% of the variance in the surgeon and therapist models, respectively.
Discussion
A weight-bearing limitation and impaired knee flexion ROM were consistently associated with surgeon assessments of the need for physical therapy across a 12-month recovery period in participants with traumatic lower-extremity injuries; for physical therapists, the associated factor was moderate to severe pain. Injury severity was important to both surgeons and physical therapists at the 3-month follow-up assessment, and balance limitations and impaired knee flexion ROM were important at the 6- and 12-month assessments. Characteristics of injuries associated only with surgeon assessments of need at 6 and 12 months included delayed fracture healing.
Although these findings provide insight into similarities and differences in surgeon and therapist assessments of the need for physical therapy, they explain only a small proportion of the observed assessment variability. The variability in assessments across the 8 participating level I trauma centers and between providers and the variance of the random effects indicate that some of the variability can be attributed to trauma center and provider characteristics. As indicated in the literature, provider characteristics may include practice style, clinical uncertainty, outcome expectations, and knowledge of and experience with physical therapy, and trauma center characteristics such as medical culture, colleagues’ expectations, and training protocols may influence the assessment process.49–56
Characteristics of the participants were not found to significantly influence surgeon assessments of the need for physical therapy. This finding was surprising because studies of physician referral to both physical therapists and medical specialists have reported an association between referral and the age, sex, education, and insurance coverage of the participants.15,50–57 However, these studies did not control for the extensive clinical and injury factors included in our analyses. In addition, this difference might be attributable to the severity of the injuries in our study population.
As expected, participants with more severe injuries, such as articular fractures and delayed fracture healing, were more likely to be assessed by surgeons as needing physical therapy. However, fracture healing did not significantly influence therapist assessments of need, and an articular injury was negatively associated with a therapist assessment at 3 months. This difference might have been a result of minimal communication between the surgeon and the therapist about the nature of the injury, the surgical procedure, and postoperative radiographic findings. Further support for a lack of communication between providers was demonstrated by the findings for weight-bearing limitations. Surgeons considered weight bearing to be one of the most important factors during assessments of the need for physical therapy at all follow-up time points, but weight bearing was not statistically associated with therapist assessments. This difference might have reflected a desire by therapists to postpone gait rehabilitation until later in the recovery period and to focus instead on pain and on ROM and balance impairments. An important finding was that, although ROM was explored for the hip, knee, and ankle, only the knee appeared to be particularly relevant to assessments of the need for physical therapy. The insignificant hip joint findings might have been related to the distribution of injuries in the present study because relatively few participants had hip impairments (as opposed to knee and ankle impairments).
Our hypothesis that pain would be associated with surgeon assessments of the need for physical therapy was not supported by the study results. This finding was unexpected because pain has been found to contribute to long-term disability and poor vocational outcomes10,58,59 and because clinical trials have found physical therapy to favorably affect pain in patients with various musculoskeletal conditions.60–63 On the basis of the poor long-term outcomes of this patient population, it is important to determine the specific effects of physical therapy on patients’ pain complaints and disseminate this information to both surgeons and physical therapists treating traumatic lower-extremity injuries. In addition, it would be beneficial to examine orthopedic surgeons’ attitudes and beliefs about the management of postoperative pain.
The nonsignificant finding for work status was also unexpected because rehabilitation has been shown to improve occupational outcomes3,64,65 and often has been considered an appropriate treatment for patients experiencing workplace limitations.66,67 Instead, patients’ work self-efficacy was significantly related to surgeon assessments of the need for physical therapy at 3 months and therapist assessments at 6 and 12 months, suggesting that patients’ belief in their ability to return to work and not their actual work status influenced assessments. This finding might be explained by the severity of injuries in this patient population. Lower-extremity injuries treated by reconstruction have high rates of complications and often require additional surgery during the first year of recovery, leading to a delayed return to work.68,69 Thus, physical deficits and patients’ work self-efficacy, important predictors of a return to work,10 may be more important during the first 12 months of recovery than employment status per se.
Of interest was the finding of differences in assessments between surgeons and physical therapists across the 12-month recovery period. The results suggested that surgeons and therapists tended to assess participants as needing physical therapy at 3 months but that, although there was a steady decline in surgeon assessments of participants as needing therapy at 6 and 12 months, the rates of therapist assessments of the need for therapy remained relatively high. Seventy percent of the participants at 6 months and almost half of the participants at 12 months were assessed by therapists as needing therapy. The results suggested that participants with traumatic lower-extremity injuries might not be referred by surgeons for physical therapy further into their recovery. The findings support the need for more communication between surgeons and physical therapists about the plan of care for participants at 6- and 12-month follow-up evaluations.
The limitations of the present study must be taken into account in interpretations of the results. First, the LEAP study was conducted more than 10 years ago. Studies have documented little change in the physical therapy referral process,19,21,22 with variability in referral rates, the content of referral prescriptions, the limited professional role of physical therapists, and the influence of patient-related factors on referral to physical therapists remaining consistent.14–24,70 However, both formal and informal roles of physical therapists in the health care system have expanded during the last decade; thus, study results need to be interpreted with caution because of the age of the data set. We attempted to mitigate this limitation of the present study by conducting a prospective, cross-sectional survey of 274 surgeon members of the Orthopaedic Trauma Association (OTA) to verify the findings in the surgeon assessment model.71 Surgeons were asked to make physical therapy referral decisions on the basis of traumatic lower-extremity cases abstracted from the LEAP database. The results supported the association between surgeon referral to physical therapists and weight-bearing status, knee flexion ROM, and injury severity. Furthermore, pain relief and return to work did not appear to be expected outcomes of referral to physical therapists for the treatment of traumatic lower-extremity injury.
A second limitation is that the outcome measures of assessments of need for physical therapy were not confirmed with documented referral prescriptions, a fact that limited the generalizability of our findings to the broader referral process. Also, the results might not be generalizable beyond providers at level I trauma centers because of their training and expertise. Third, the occupational factors of preinjury work status and current work status were based on patient self-report, a fact that might have resulted in an underestimation of the association between work status and the assessment of need. Fourth, orthopedic surgeons and physical therapists followed different evaluation protocols, a fact that might have contributed to the differences in the assessment models. However, surgeon and physical therapist evaluation procedures are inherently different because of training and experience, and the LEAP study procedures represented current clinical practice at level I trauma centers.
Despite these study limitations, we found evidence that variability in assessments of the need for physical therapy existed not only at the provider and trauma center levels but also throughout the 12-month recovery period. The findings emphasized the need for communication about the nature of the patient's injury, the surgical procedure, postoperative healing status, the patient's pain level, and weight-bearing status. Focusing on these factors has the potential to improve access to and appropriate use of physical therapy for patients with traumatic lower-extremity injuries.
On the basis of the findings of the present study, specific recommendations for future research on traumatic lower-extremity injuries include identifying the surgeon and level I trauma center characteristics that contribute to variations in referral practices to facilitate the development of an effective strategy for decreasing variability; determining surgeon perceptions and management of postoperative pain and work status in patients to facilitate an understanding of current clinical practice; and exploring the optimal time for referral to physical therapists of patients with traumatic lower-extremity injuries. Furthermore, examining the effects of physical therapy on pain and work outcomes in this patient population and disseminating this information to orthopedic surgeons have the potential to improve the long-term outcomes associated with traumatic lower-extremity injuries.
Supplementary Material
Footnotes
All authors provided concept/idea/research design and data analysis. Dr Archer, Dr MacKenzie, and Dr Castillo provided writing. Dr Castillo and Dr Bosse provided data collection and fund procurement. Dr Castillo provided project management. Dr Bosse provided participants. Dr MacKenzie provided institutional liaisons. Dr Archer and Dr Castillo provided consultation (including review of manuscript before submission).
This study was approved by the institutional review boards at the coordinating center (Johns Hopkins School of Public Health, Baltimore, Maryland) and at each study site.
This research was supported with funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (ROI-AR42659); the Johns Hopkins Education and Research Center for Occupational Safety and Health at the Johns Hopkins Bloomberg School of Public Health, which is sponsored by the National Institute for Occupational Safety and Health (T42OH00842428); and the Johns Hopkins Center for Injury Research and Policy at the Johns Hopkins Bloomberg School of Public Health, which is funded by the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (CE000198-03).
A platform presentation of this research was given at the Annual Conference and Exposition of the American Physical Therapy Association; June 11–14, 2008; San Antonio, Texas.
Hoggan Health Industries, PO Box 488, West Jordan, Utah 84084.
Stata Corp, 4905 Lakeway Dr, College Station, TX 77845.
References
- 1.Rice DP, MacKenzie EJ, Jones AS, et al. Cost of Injury in the United States: A Report to Congress San Francisco, CA: Institute for Health and Aging at the University of California and Injury Prevention Center at The Johns Hopkins University; ; 1989. [Google Scholar]
- 2.Dillingham TR, Pezzin LE, MacKenzie EJ. Incidence, acute care length of stay, and discharge to rehabilitation of traumatic amputee patients: an epidemiologic study. Arch Phys Med Rehabil 1998;79:279–287 [DOI] [PubMed] [Google Scholar]
- 3.Pezzin LE, Dillingham TR, MacKenzie EJ. Rehabilitation and long-term outcomes of persons with trauma-related amputations. Arch Phys Med Rehabil 2000;81:292–300 [DOI] [PubMed] [Google Scholar]
- 4.Bosse MJ, MacKenzie EJ, Kellam JF, et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med 2002;347:1924–1931 [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie EJ, Bosse MJ, Pollak AN, et al. Long-term persistence of disability following severe lower-limb trauma. J Bone Joint Surg Am 2005;87:1801–1809 [DOI] [PubMed] [Google Scholar]
- 6.McCarthy ML, MacKenzie EJ, Edwin D, et al. Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am 2003;85:1689–1697 [DOI] [PubMed] [Google Scholar]
- 7.Castillo RC, MacKenzie EJ, Wegener ST, Bosse MJ. Prevalence of chronic pain seven years following limb threatening lower extremity trauma. Pain 2006;124:321–329 [DOI] [PubMed] [Google Scholar]
- 8.MacKenzie EJ, Morris JA, Jurkovich GJ, et al. Return to work following injury: the role of economic, social, and job-related factors. Am J Public Health 1998;88:1630–1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoppen T, Boonstra A, Groothoff JW, et al. Employment status, job characteristics, and work-related health experience of people with a lower limb amputation in the Netherlands. Arch Phys Med Rehabil 2001;82:239–245 [DOI] [PubMed] [Google Scholar]
- 10.MacKenzie EJ, Bosse MJ, Kellam JF, et al. Early predictors of long-term work disability following major limb trauma. J Trauma 2006;61:688–694 [DOI] [PubMed] [Google Scholar]
- 11.Jelic M, Eldar R. Rehabilitation following major traumatic amputation of lower limbs: a review. Clin Rev Phys Rehabil Med 2003;15:235–252 [Google Scholar]
- 12.Archer KR, Castillo RC, MacKenzie EJ, Bosse MJ. Gait symmetry and walking speed analysis following lower-extremity trauma. Phys Ther 2006;86:1630–1640 [DOI] [PubMed] [Google Scholar]
- 13.Castillo RC, MacKenzie EJ, Webb LX, et al. Use and perceived need of physical therapy following severe lower-extremity trauma. Arch Phys Med Rehabil 2005;86:1722–1728 [DOI] [PubMed] [Google Scholar]
- 14.Freburger JK, Holmes GM, Carey TS. Physician referrals to physical therapy for the treatment of musculoskeletal conditions. Arch Phys Med Rehabil 2003;84:1839–1849 [DOI] [PubMed] [Google Scholar]
- 15.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J 2005;5:530–541 [DOI] [PubMed] [Google Scholar]
- 16.Ward AW, Williams BT, Dixon RA. Physiotherapy: its prescription and implementation for orthopaedic out-patients. Rheumatol Rehabil 1978;17:14–22 [DOI] [PubMed] [Google Scholar]
- 17.Pless BI, Satterwhite B, Van Vechten D. Chronic illness in childhood: a regional survey of care. Pediatrics 1976;52:37–46 [PubMed] [Google Scholar]
- 18.Ritchey FJ, Pinkston D, Goldbaum JE, Heerten ME. Perceptual correlates of physician referral to physical therapists: implications for role expansion. Soc Sci Med 1989;28:69–80 [DOI] [PubMed] [Google Scholar]
- 19.Uili RM, Shepard KF, Savinar E. Physician knowledge and utilization of physical therapy procedures. Phys Ther 1984;64:1523–1529 [DOI] [PubMed] [Google Scholar]
- 20.Kerssens JJ, Groenewegen PP. Referrals to physiotherapy: the relation between the number of referrals, the indication for referral, and the inclination to refer. Soc Sci Med 1990;30:797–804 [DOI] [PubMed] [Google Scholar]
- 21.Davenport TE, Watts HG, Kulig K, Resnik C. Current status and correlates of physicians’ referral diagnoses for physical therapy. J Orthop Sports Phys Ther 2005;35:572–579 [DOI] [PubMed] [Google Scholar]
- 22.Clawson Al, Domholdt E. Content of physician referrals to physical therapists at clinical education sites in Indiana. Phys Ther 1994;74:356–360 [DOI] [PubMed] [Google Scholar]
- 23.Wong WP, Galley P, Sheehan M. Changes in medical referrals to an outpatient physiotherapy department. Aust J Physiother 1994;40:9–14 [DOI] [PubMed] [Google Scholar]
- 24.Ehrmann-Feldman D, Rossignol M, Abenhaim L, Gobeille D. Physician referral to physical therapy in a cohort of workers compensated for low back pain. Phys Ther 1996;76:150–157 [DOI] [PubMed] [Google Scholar]
- 25.MacKenzie EJ, Bosse MJ, Kellam JF, et al. Characterization of patients with high-energy lower extremity trauma. J Orthop Trauma 2000;14:455–466 [DOI] [PubMed] [Google Scholar]
- 26.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742–746 [DOI] [PubMed] [Google Scholar]
- 27.Fisher GM. The development and history of the poverty thresholds. Soc Sci Bull 1992;55:3–14 [PubMed] [Google Scholar]
- 28.Suedkamp NP, Barbey N, Veuskens A, et al. The incidence of osteitis in open fractures: an analysis of 948 open fractures (a review of the Hannover experience). J Orthop Trauma 1993;7:473–482 [DOI] [PubMed] [Google Scholar]
- 29.Howe HR, Poole GV, Hansen KJ, et al. Salvage of lower extremities following combined orthopedic and vascular trauma: a predictive salvage index. Am Surg 1987;53:205–208 [PubMed] [Google Scholar]
- 30.Bandura A, O'Leary A, Taylor CB, et al. Perceived self-efficacy and pain control: opioid and nonopioid mechanisms. J Pers Soc Psychol 1987;53:563–571 [DOI] [PubMed] [Google Scholar]
- 31.Ewart CK, Stewart KJ, Gillian RE, Keleman MH. Self-efficacy mediates strength gains during circuit weight training in men and women with coronary artery disease. Med Sci Sports Exerc 1986;18:531–540 [PubMed] [Google Scholar]
- 32.Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 2003;4:407–414 [DOI] [PubMed] [Google Scholar]
- 33.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981;19:787–805 [DOI] [PubMed] [Google Scholar]
- 34.De Bruin AF, de Witte LP, Stevens F, Diedriks JP. Sickness Impact Profile: the state of the art of a generic functional status measure. Soc Sci Med 1992;35:1003–1014 [DOI] [PubMed] [Google Scholar]
- 35.Jurkovich G, Mock C, MacKenzie E, et al. The Sickness Impact Profile as a tool to evaluate functional outcome in trauma patients. J Trauma 1995;39:625–631 [DOI] [PubMed] [Google Scholar]
- 36.Schoppen T, Boonstra A, Groothoff JW, et al. Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Arch Phys Med Rehabil 2003;84:803–811 [DOI] [PubMed] [Google Scholar]
- 37.Magee DJ. Orthopedic Physical Assessment Philadelphia, PA: WB Saunders Co; ;1997 [Google Scholar]
- 38.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry 3rd ed.Philadelphia, PA: FA Davis Co; ;2003 [Google Scholar]
- 39.Brosseau L, Balmer S, Tousignant M, et al. Intra- and intertester reliability and criterion validity of the parallelogram and universal goniometers for measuring maximum active knee flexion and extension of patients with knee restrictions. Arch Phys Med Rehabil 2001;82:396–402 [DOI] [PubMed] [Google Scholar]
- 40.Youdas JW, Bogard CL, Suman VJ. Reliability of goniometric measurements and visual estimates of ankle joint active range of motion obtained in a clinical setting. Arch Phys Med Rehabil 1993;74:111–118 [DOI] [PubMed] [Google Scholar]
- 41.American Academy of Orthopaedic Surgeons Joint Motion: Method of Measuring and Recording Chicago, IL: American Academy of Orthopaedic Surgeons; ;1965 [Google Scholar]
- 42.Peindl RD, McCarthy ML, MacKenzie EJ, inventors; The Johns Hopkins University and The Charlotte-Mecklenburg Hospital Authority, assignees Apparatus for exercising and measuring strength of a patient's limb and an adjustable pivot clamp. US patent 5,662,591 September2, 1997.
- 43.McCarthy ML, McAndrew MP, MacKenzie EJ, et al. Correlation between the measures of impairment, according to the modified system of the American Medical Association, and function. J Bone Joint Surg Am 1998;80:1034–1042 [DOI] [PubMed] [Google Scholar]
- 44.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata College Station, TX: Stata Press; ;2005 [Google Scholar]
- 45.Rabe-Hesketh S, Skrondal A, Pickles A. GLLAMM Manual (October 2004). UC Berkeley Division of Biostatistics Working Paper Series Working Paper 160. Available at: http://www.bepress.com/ucbbiostat/paper160 Accessed September 4, 2009 [Google Scholar]
- 46.Hosmer DW, Lemeshow S. Applied Logistic Regression New York, NY: John Wiley & Sons, Inc; ;2000 [Google Scholar]
- 47.van Buuren S, Oudshoorn CGM. Multivariate Imputation by Chained Equations: MICE V1.0 User's Manual Leiden, the Netherlands: TNO Preventie en Gezondheid; ;2000Report PG/VGZ/00.038 [Google Scholar]
- 48.Royston P. Multiple imputation of missing values. Stata Journal 2004;4:227–241 [Google Scholar]
- 49.Jorgensen CK, Olesen F. Predictors for referral to physiotherapy from general practice. Scand J Prim Health Care 2001;19:48–53 [DOI] [PubMed] [Google Scholar]
- 50.Bertakis KD, Callahan EJ, Azari R, Robbins JA. Predictors of patient referrals by primary care residents to specialty care clinics. Fam Med 2001;33:203–209 [PubMed] [Google Scholar]
- 51.Shea D, Stuart B, Vasey J, Nag S. Medicare physician referral patterns. Health Serv Res 1999;34:331–348 [PMC free article] [PubMed] [Google Scholar]
- 52.Cowen ME, Zodet MW. Methods for analyzing referral patterns. J Gen Intern Med 1999;14:474–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Franks P, Williams GC, Zwanziger J, et al. Why do physicians vary so widely in their referral rates? J Gen Intern Med 2000;15:163–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chan BT, Austin PC. Patient, physician, and community factors affecting referrals to specialists in Ontario, Canada: a population-based, multi-level modeling approach. Med Care 2003;41:500–511 [DOI] [PubMed] [Google Scholar]
- 55.Bachman KH, Freeborn DK. HMO physicians’ use of referrals. Soc Sci Med 1999;8:547–557 [DOI] [PubMed] [Google Scholar]
- 56.Forrest CB, Nutting P, Werner JJ, et al. Managed health plan effects on the specialty referral process: results from the Ambulatory Sentinel Practice Network referral study. Med Care 2003;41:242–253 [DOI] [PubMed] [Google Scholar]
- 57.Franks P, Clancy CM. Referrals of adult patients from primary care: demographic disparities and their relationship to HMO insurance. J Fam Pract 1997;45:47–53 [PubMed] [Google Scholar]
- 58.MacKenzie EJ, Cushing BM, Jurkovich GJ, et al. Physical impairment and functional outcomes six months after severe lower extremity fracture. J Trauma 1993;34:528–539 [DOI] [PubMed] [Google Scholar]
- 59.Mock C, MacKenzie E, Jurkovich G, et al. Determinants of disability after lower extremity fracture. J Trauma 2000;49:1002–1011 [DOI] [PubMed] [Google Scholar]
- 60.Hurwitz EL, Aker PD, Adams AH, et al. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine 1996;21:1746–1759 [DOI] [PubMed] [Google Scholar]
- 61.Bergman GJ, Winters JC, Groenler KH, et al. Manipulative therapy in addition to usual care for patients with shoulder dysfunction and pain. Ann Intern Med 2004; 141:432–439 [DOI] [PubMed] [Google Scholar]
- 62.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med 2005;142:776–785 [DOI] [PubMed] [Google Scholar]
- 63.Harris GR, Susman JL. Managing musculoskeletal complaints with rehabilitation therapy: summary of the Philadelphia Panel evidence-based clinical practice guidelines on musculoskeletal rehabilitation interventions. J Fam Pract 2002;51:1042–1046 [PubMed] [Google Scholar]
- 64.Sheikh K. Return to work following limb injuries. J Soc Occup Med 1985;35:114–117 [DOI] [PubMed] [Google Scholar]
- 65.Schmidt SH, Oort-Marburger D, Meijman TF. Employment after rehabilitation for musculoskeletal impairments: the impact of vocational rehabilitation and working on a trial basis. Arch Phys Med Rehabil 1995;76:950–954 [DOI] [PubMed] [Google Scholar]
- 66.Livingston DH, Keenan D, Kim D, et al. Extent of disability following traumatic extremity amputation. J Trauma 1994;37:495–499 [DOI] [PubMed] [Google Scholar]
- 67.Morris JA, Jr, Sanchez AA, Bass SM, MacKenzie EJ. Trauma patients return to productivity. J Trauma 1991;31:827–834 [DOI] [PubMed] [Google Scholar]
- 68.Fairhurst MJ. The function of below-knee amputees versus the patient with salvaged grade III tibial fracture. Clin Orthop 1994;301:227–232 [PubMed] [Google Scholar]
- 69.Busse JW, Jacobs CL, Swiotkowski MF, et al. Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J Orthop Trauma 2007;21:70–76 [DOI] [PubMed] [Google Scholar]
- 70.Joyce J, Kuperstein J. Improving physical therapy referrals. Am Fam Phys 2005;71:1183–1184 [PubMed] [Google Scholar]
- 71.Archer KR, MacKenzie EJ, Bosse MJ, et al. Factors associated with surgeon referral for physical therapy in patients with traumatic lower-extremity injury: results of a national survey of orthopedic trauma surgeons. Phys Ther 2009;89:893–905 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.