Abstract
Purpose: Several studies have documented a deficiency in the delivery of preventive services to adolescents during physician visits in the United States. This study sought to assess and compare pediatric, family medicine (FM), and obstetrics and gynecology (OB/GYN) resident perceptions of their responsibility, training, and experience with providing comprehensive health care services to adolescents.
Methods: A 57-item, close-ended survey was designed and administered to assess resident perceptions of the scope of their practice, training, and experience with providing adolescent health care across a series of health care categories.
Results: Of the 87 respondents (31 OB/GYN, 29 FM, and 27 pediatric), most residents from all three fields felt that the full range of adolescent preventive and clinical services represented in the survey fell under their scope of practice. Residents from all three fields need more training and experience with mental health issues, referring teenagers to substance abuse treatment programs, and addressing physical and sexual abuse. In addition, OB-GYN residents reported deficiencies in training and experience regarding several preventive counseling and general health services, while pediatric residents reported deficiencies in training and experience regarding sexual health services.
Conclusions: Our results indicate that at this time, residents from these three specialties are not optimally prepared to provide the full range of recommended preventive and clinical services to adolescents.
Keywords: adolescent medicine, internship and residency, obstetrics, gynecology, pediatrics, family practice
Introduction
The major causes of morbidity and mortality experienced by adolescents in the United States can be attributed to preventable causes, including sexually transmitted infections (STI), suicide, unintended pregnancy, accidents, and obesity. However, only 39 percent of adolescents received any type of preventive counseling during ambulatory visits as documented by the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) in 1997-2000 [1]. Similarly, in the 1997 Commonwealth Fund Survey of the Health of Adolescent Girls, 71 percent of teens reported at least one potential health risk, yet only 37 percent of these teens reported discussing any of these risks with their provider [2].
The relationship between physician training in adolescent health care and the delivery of comprehensive health services to teenagers has been well documented [3-8], and professional societies, including the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the American College of Obstetricians and Gynecologists (ACOG), have recommended increased adolescent medicine training in primary care residencies.
There is insufficient data to evaluate whether an increased emphasis on adolescent health care has altered resident attitudes, knowledge, comfort, and effectiveness administering health care to adolescents. Additionally, assessments of resident experience and training in administering care to adolescents in the United States have been sparse. The primary aim of this study was to assess and compare pediatric, family medicine (FM), and obstetrics and gynecology (OB/GYN) resident perceptions of their responsibility, training, and experience with providing preventive services and health care to adolescents.
Methods
Sample
We conducted a cross-sectional study with convenience sampling of all residents present during resident educational sessions on a given day at participating residency programs between February 19 and March 16, 2007. The Yale University School of Medicine Human Investigation Committee determined that this protocol was exempt from review. OB/GYN, FM, and pediatric residency programs in Connecticut were contacted to request participation of their residents in the study. An additional FM program in New York was contacted in order to increase the sample size for family medicine. FM, pediatrics, and OB/GYN were chosen since these specialties see the greatest number of adolescent patients in the United States [1,9-12]. Participating residencies included the FM programs of the University of Connecticut and Montefiore/Albert Einstein College of Medicine; the pediatrics programs of the University of Connecticut and Yale-New Haven Hospital; and the OB/GYN programs of Danbury Hospital, Bridgeport Hospital, Stamford Hospital/Columbia University College of Physicians and Surgeons, and Yale-New Haven Hospital.
Survey instrument
The questionnaire consisted of 57 close-ended questions about which adolescent health services the residents considered part of their scope of practice in their respective field; the perceived adequacy of training they had received with regard to select adolescent health services; and the experience they had performing select clinical activities with adolescents. The questions were not based on any prior survey instrument, because a validated instrument addressing the range and specific focus of these questions does not exist.
Study variables
Survey questions regarding scope, training, and experience covered five main topics in adolescent medicine, including general adolescent health, mental health, substance abuse, physical and sexual abuse, and sexual health. A greater number of sexual health questions were included in each category in deference to the recent national survey of adolescents performed by the Kaiser Family Foundation that demonstrated adolescents are more concerned about sexual health than any other health topic [13]. In addition, several studies of practicing physicians have demonstrated specialty-specific differences, particularly in the provision of care related to sexual health [7,8,14,15].
Statistical analysis
Data analysis was performed using SAS 9.1 (SAS Institute Inc., Cary, N.C.) statistical analysis software package. Resident responses to each survey question were the primary outcome variables. The primary exposure variable was specialty. Chi-squared tests or Fisher’s exact test were used to examine the relationship between resident specialty and survey responses for each item on the questionnaire. Potential confounders (sex, hospital religious affiliation, plans to specialize, and level of training) were investigated by stratified analyses.
Results
Of the 88 subjects approached during the resident education session, 87 (99 percent) agreed to complete the survey. Thirty-six percent of the residents were from an OB/GYN program, 33 percent from a FM program, and 31 percent from a pediatrics program. Table 1 displays demographic data by field using chi-square analysis. Across all three fields, 31 percent were interns, 31 percent were second-year residents and 38 percent were third- or fourth-year residents. The number of residents in each level was approximately equal between the three different fields. A greater number of females (63 percent) were represented compared to males (37 percent). A significantly (p = 0.037) greater percentage of OB/GYN residents (80 percent) were female compared to the number of female residents surveyed in FM (48 percent) and pediatrics (58 percent). More than half (58 percent) planned to practice as general physicians, and 42 percent planned to specialize. Intention to specialize differed across fields, with the majority of OB/GYN and pediatric residents planning to specialize, compared to the majority of family medicine residents who planned to practice as generalists (p = 0.002). Approximately 37 percent of residents were from programs with religious hospital affiliations; no OB/GYN residents were from programs with religious hospital affiliations.
Scope
Overall, residents from different fields were largely in agreement about what adolescent services they considered to be part of their scope of practice (Table 2). Prescribing emergency contraception to teens and referring adolescents to clinics where they could receive an abortion, along with counseling about pregnancy termination options, were the only practices that varied significantly between different fields. OB/GYN residents (97 percent) were the most likely to consider prescribing emergency contraception as part of their scope of practice and pediatric residents (78 percent) least likely, with FM residents (89 percent) falling in the middle. OB/GYN (100 percent) and FM (97 percent) residents most often considered counseling about pregnancy termination options their responsibility, while pediatric residents (85 percent) were less likely to consider such counseling their responsibility. In regard to providing teens information about where they could obtain abortions, OB/GYN residents unanimously felt it fell under their scope, while FM (79 percent) and pediatric (77 percent) residents were less likely to feel it was part of their responsibility.
Training
Overall, counseling about STI risk and prevention was the only service for which greater than 90 percent of residents felt they had received adequate training (Table 3). Several significant differences exist between fields in regard to their reported level of training (Table 3). OB/GYN residents reported significantly less training than FM or pediatric residents in several preventive services, including counseling about diet/exercise, eating disorders/body image and substance abuse, screening for depression/suicide, and discussing sexual partners. Pediatric residents, on the other hand, reported significantly less training than OB/GYN or FM residents in several services pertaining to sexual health, including conducting pelvic exams; counseling and prescribing contraception; counseling and prescribing emergency contraception; and counseling about pregnancy termination. When interns are excluded from the analysis (Table 5), the difference in the training reported by pediatric residents in regard to pelvic exams and counseling and prescribing contraception is diminished, but the trend remains the same.
Experience
Significant differences by field were found for the majority of survey items (Table 4). Similar to the deficiencies noted in responses to training questions, OB/GYN residents were significantly less likely than FM and pediatric residents to have had at least one experience with an adolescent patient in defining confidentiality in the patient-doctor relationship; evaluating positive aspects of life; counseling about weight loss, depression, suicide, and alcohol or drug use; and discussing sexual partners. The significance of the difference noted for defining confidentiality, counseling a depressed adolescent, counseling about drug use, and discussing sexual partners is diminished when interns are excluded from the analysis but the trend remains the same (Table 5). While OB/GYN residents were significantly less likely to have counseled a teen about alcohol or drug use, they were significantly more likely to have referred an adolescent to a substance abuse program as compared to FM and pediatric residents.
Pediatric residents were significantly less likely than FM and OB/GYN to have had at least one encounter in which they counseled an adolescent who experienced physical abuse. Likewise, they were less likely to have counseled about pregnancy termination. Moreover, pediatric residents report significantly less experience than FM and OB/GYN residents in prescribing emergency contraception when interns are excluded from the analysis (Table 5). Pediatric residents also reported significantly lower rates of conducting pelvic exams and prescribing contraception compared to OB/GYN and FM residents. Around 15 percent of pediatric residents reported they had never conducted a pelvic exam on an adolescent, and 56 percent conducted fewer than 11. Approximately 26 percent of pediatric residents reported they had never prescribed contraception, and 70 percent had prescribed contraception fewer than 11 times. FM residents were more likely to have counseled adolescents about contraceptive options than OB/GYN or pediatric residents. However, this difference is diminished when interns are excluded from the analysis (Table 5). FM residents were less likely than pediatric residents but more likely than OB/GYN residents to have counseled a suicidal adolescent. In addition, FM residents were less likely than OB/GYN residents but more likely than pediatric residents to have counseled about pregnancy termination options.
Potential confounding variables
Survey items for which differences by field are altered by excluding intern level residents from the analysis are described in each section as appropriate and illustrated in Table 5. Interns in all three fields are less likely to have encountered the full breadth of training and experience in their training programs. Subsequent experience in later years may serve to even out these initial differences. However, for many survey items, trends and differences between specialties remain when interns are excluded from analysis.
Three other demographic variables (namely, gender, hospital religious affiliation, and intention to specialize) were noted to be significantly different between fields and thus had the potential to confound survey results by field. For the majority of survey items for which religious affiliation was identified as having a potential significant influence, the pattern among residents within non-religiously affiliated hospitals mirrored the patterns observed in the full data set. Nonetheless, careful consideration of the results of stratified analysis suggests a religious affiliation effect occurred with regard to FM residents and items concerning abortion. FM resident positive responses to abortion questions concerning scope and experience increased substantially, matching the level of positive response observed in OB/GYN residents, when FM residents in programs with religious affiliation were excluded.
Female providers have been documented to provide more preventive services in several studies [6,8,14,16-18]. We did not observe this trend in our study. However, given the low number of male OB/GYN residents, we would need a larger sample size to fully evaluate the effect of gender. Stratified analyses by “intention to specialize” revealed no significant differences from the non-stratified analysis.
Discussion
The primary aim of this study was to assess and compare pediatric, FM, and OB-GYN resident perceptions of their responsibility, training, and experience in providing comprehensive preventive health services to adolescents. Our results identify strengths and weaknesses in each field and lend insight into how each specialty training program could improve resident training and experience in adolescent services.
Understanding adolescent health care patterns helps in both understanding the needs of the group and explaining some differences between the perceptions of FM, pediatric, and OB/GYN residents noted in this study. While the proportion of teens visiting either FM, pediatric, or OB/GYN providers changes significantly across early (11-14 years), middle (15-17 years), and late (18-21 years) adolescence, very few make use of multiple specialties at a single time [19,20]. Since the average adolescent is likely to have a limited number of visits to a single health provider, it is important for all adolescent health professionals to provide comprehensive care.
Family Medicine
Based upon these survey results, FM residents consider the broadest range of preventive adolescent health care subjects within the scope of their practice and also report the most experience and training across the greatest number of subjects. These findings were expected, given that FM as a field seeks to provide comprehensive primary care for all age groups, genders, and health needs, whereas pediatrics and OB/GYN are limited in scope by age, content, and patient gender. Teen visit patterns also support the ability of FM physicians to gain experience with all adolescent health issues. According to the National Ambulatory Medical Care Survey data from 1994 to 2003, FM physicians care for a relatively constant percentage of adolescents across the age groups, providing 22 percent of early adolescent visits and 29 percent of late adolescent visits [21]. This consistency in visits across the age groups is unique to FM physicians, as pediatricians are less likely to care for older adolescents, and OB/GYNs care for very few teens younger than 14. Because the needs of adolescents change as they age, FM residents are likely to encounter a broad range of health needs and potentially benefit the most from having comprehensive and adequate training across the various adolescent health topics.
Overall, FM residents in this survey reported high levels of training across all of the surveyed subjects, with only screening for sexual abuse and teaching of correct condom use falling below 75 percent. Perceived adequacy in training was higher for FM residents across more subjects than for the other two residency programs. However, fewer than 55 percent of the FM residents reported any experience counseling about eating disorders, physical and sexual abuse, pregnancy termination, making referrals to substance abuse programs, and counseling a suicidal teen. Possible reasons for deficiencies in experience in residency training programs could be related to patient demographics, clinical care settings, time and preparation for adequate screening, and availability of adequate resources to deal with the above subjects. Residency programs within religiously affiliated hospitals also may affect both the training and experience of residents in subject areas related to contraception and pregnancy termination. Identifying ways to improve resident experiences with these subjects should be a goal of all residency training programs.
Pediatrics
For many adolescent patients, pediatricians are their only medical care provider when they enter their teen years. Pediatricians are in a unique position to build upon the continuity, trust, and familiarity that this relationship fosters and initiate patient education and counseling regarding the primary health concerns faced by teens. In our study, pediatric residents reported general health concerns, counseling about substance abuse, and STI prevention as strengths in their training and experience and often fell between FM and OB/GYN in terms of reported adequacy across most health topics.
However, sexual health-related topics were less universally considered as part of the scope of pediatric practice. Particularly, fewer pediatric residents considered the performance of pelvic exams (85 percent), prescribing emergency contraception (77 percent), counseling about pregnancy termination options (84.6 percent), and instructing patients where they could obtain an abortion (76 percent) within the scope of their practice, compared to FM or OB/GYN residents. This trend in sexual health carried over for both training and experience for pediatric residents.
Deficiencies in sexual health care is consistent with patterns observed among practicing pediatricians [4,6,9,15,22,23]. The deficiencies seen in training and experiences in adolescent reproductive and sexual health may be a reflection of health care visit patterns of adolescents. In the NAMCS, pediatricians steadily decrease as the primary providers for teens as they age. Pediatricians care for the greatest percentage of early adolescents, providing 41.2 percent of the visits, 21 percent of visits to middle adolescents between 15 and 17 years of age, and only 4.1 percent of late adolescents ages 18-21 years [19]. Late adolescent females, who primarily seek care for pregnancy and gynecologic complaints, are more likely to visit OB/GYN and FM providers [19,24]. This is likely to impact the experiences of pediatric residents as well as perceptions of the scope of pediatric care with respect to sexual and reproductive health. The responses obtained in our survey suggest the increased emphasis on adolescent medicine during the past decade, and the creation of a required rotation in adolescent medicine may not be providing adequate training and experience in sexual health issues and pelvic exams for all pediatric residents.
New guidelines recommending that PAP smear screening for cervical dysplasia need not begin until three years after the initiation of sexual intercourse [25], the ability to screen for gonorrhea and chlamydia in the urine [26,27], and recommendations that contraception can be prescribed without a PAP smear or a pelvic exam [28] should be taught to all residents and should encourage all pediatricians to continue to provide care and counseling in these venues for their adolescent patients. However, any provider caring for teens should be prepared to conduct a gynecologic exam when indicated by patient concern or symptoms.
Obstetrics and Gynecology
The OB/GYN specialty is unique in its care of female patients only and its traditional focus on medical and surgical concerns related to pregnancy, gynecology, and reproductive endocrinology. However, in 2006, ACOG recommended that all adolescent females undergo an initial reproductive health visit, during which the physician is expected to provide comprehensive preventive care on the items included in this survey [29].
While OB/GYN residents report good training and experience in all sexual health-related issues, they identified a number of areas in general and mental health that would need to receive greater attention in training programs in order for OB/GYN practitioners to serve as comprehensive providers for adolescents. OB/GYN residents are less likely than FM or pediatric residents to consider areas of general health, psychiatric health, and substance abuse, included in this survey, as part of the scope of their practice. Their reported levels of training and experience in defining confidentiality, counseling about weight and exercise, eating disorders, depression/suicide, and screening and counseling for substance abuse were all significantly lower than FM and pediatric residents. Deficits in these areas have been reported both among other OB/GYN residents and practicing physicians [30]. These observations may be related to the relatively recent nature of the ACOG-initiated emphasis on providing comprehensive adolescent health care in the field of OB/GYN, whereas adolescent care is well established within the fields of FM and pediatrics. Additionally, as the data have well supported, adolescents primarily seek OB/GYN care for issues related to pregnancy and gynecologic health and are typically older than teens visiting FM and pediatric practices. These patterns likely limit the opportunities for experiences in general health care available to OB/GYN residents. This study suggests that residency programs may need to broaden their training and expectations of resident experiences in general and psychiatric care in order to meet the goals set out by ACOG. Identifying barriers to expanding this care is a subject for further research.
Limitations
Our study had several limitations, including sample size; sample characteristics, including small geographic location; inaccuracies possible with self-report; and inconsistencies in the manner in which different fields interpreted survey questions. Our ability to analyze the effect of religious affiliation and gender was limited by our sample as discussed previously. Trends reported in the study should be substantiated by sampling residents from a greater diversity of programs. Inconsistent patterns of accuracy have been observed with physician self-report; it is possible that the survey responses provided an inflated view of the level of resident training and experience [31]. However, a recent study focused on resident self-assessment found good internal consistency between resident self-report and external chart review [32], suggesting self-report can provide valuable information about general trends. The manner in which resident experience was queried may have further contributed to an inflated view of resident experience, since a single experience of a given activity was enough to qualify as experience. This does not necessarily correlate to the experience required for competency and the incorporation of the given activity into future practice. Finally, there appears to have been some inconsistencies in the manner in which residents in different fields interpreted survey questions, in particular with regard to sexual health items. OB/GYN resident training is focused on sexual health topics; thus, it was surprising to note the occasional report of inadequate training for conducting pelvic exams and counseling about and prescribing contraception by upper level OB/GYN residents. While this may reflect real inadequacies, it also could reflect a more specific interpretation by OB/GYN residents in terms of training.
Conclusions
Ideally, residents in the primary specialties who provide health care to teenagers should receive training and experience that prepares them to deliver comprehensive health services to adolescents as indicated by GAPS, AAP, AAFP, and ACOG. While there were some areas in which residents reported consistent positive responses regarding scope, training, and experience, there were multiple services for which resident training and experience was limited. Several studies have noted a connection between inadequate physician provision of preventive and clinical services to adolescents and physician training and experience with such [3-8,33]. Therefore, it is important to provide residents with training and experiences that reflect the stated goals of comprehensive health care for adolescents in order to improve delivery of health services to adolescents in the future. This study has helped identify areas within each of these three training programs in which greater emphasis, training, and experience will benefit trainees in regard to adolescent health care, so that future practicing physicians from these three specialties will be more prepared to provide the full range of recommended preventive and clinical services to adolescents.
Table 1. Characteristics of Residents Surveyed*.
| All | OBG | FM | Peds | |||
| (n = 87) | (n=31) | (n=29) | (n=27) | p value | ||
| Resident Characteristics | n (%) | n (%) | n (%) | n (%) | ||
| Level of training | 0.580 | |||||
| Intern | 27 (31.0) | 9 (29.0) | 10 (34.5) | 8 (29.6) | ||
| 2nd year resident | 27 (31.0) | 10 (32.3) | 11 (37.9) | 6 (22.2) | ||
| 3rd or 4th year resident | 33 (37.9) | 12 (38.7) | 8 (27.6) | 13 (48.2) | ||
| Sex | 0.037 | |||||
| Female | 52 (62.7) | 24 (80.0) | 14 (48.3) | 14 (58.3) | ||
| Male | 31 (37.2) | 6 (20.0) | 15 (51.7) | 10 (41.7) | ||
| Intention to specialize | 0.002 | |||||
| Generalist | 46 (58.2) | 13 (48.2) | 23 (85.2) | 10 (40.0) | ||
| Specialist | 33 (41.8) | 14 (51.9) | 4 (14.8) | 15 (60.0) | ||
| Program affiliation | < 0.001 | |||||
| Non-religous hospital | 55 (63.2) | 31 (100) | 14 (48.3) | 10 (37.0) | ||
| Religious hospital | 32 (36.8) | 0 (0) | 15 (51.7) | 17 (63.0) |
OBG, Obstetrics/Gynecology; FM,Family Medicine; Peds, Pediatrics.
*Numbers do not add to total if missing responses.
Table 2. Resident perceptions of the scope of their practice.
| Scope of Practice* | All | OBG | FM | Peds | ||
| Topic | (n = 87) | (n=31) | (n=29) | (n=27) | p value | |
| Activity with Adolescent Patients | n (%) | n (%) | n (%) | n (%) | ||
| General | ||||||
| Define confidentiality | Yes | 87 (100) | 31 (100) | 29 (100) | 27 (100) | ‡ |
| Counsel about eating habits and physical activity | Yes | 86 (98.9) | 30 (96.8) | 29 (100) | 27 (100) | 0.356 |
| Psychiatric | ||||||
| Identify depression and suicidal ideation | Yes | 84 (96.6) | 28 (90.3) | 29 (100) | 27 (100) | 0.105 |
| Substance abuse | ||||||
| Counsel about tobacco, alcohol, and drug abuse | Yes | 87 (100) | 31 (100) | 29 (100) | 27 (100) | ‡ |
| Refer to substance abuse treatment programs | Yes | 85 (97.7) | 30 (96.8) | 29 (100) | 26 (96.3) | 0.224 |
| Sexual health | ||||||
| Discuss number and gender of sexual partners | Yes | 87 (100) | 31 (100) | 29 (100) | 27 (100) | ‡ |
| Conduct pelvic exams with sample collection | Yes | 84 (93.1) | 30 (96.8) | 28 (96.6) | 23 (85.2) | 0.239 |
| Counsel about STD prevention | Yes | 87 (100) | 31 (100) | 29 (100) | 27 (100) | ‡ |
| Teach correct condom use | Yes | 82 (94.3) | 28 (90.3) | 28 (96.6) | 26 (96.3) | 0.614 |
| Counsel about pregnancy prevention | Yes | 87 (100) | 31 (100) | 29 (100) | 27 (100) | ‡ |
| Prescribe contraception | Yes | 85 (98.8) | 31 (100) | 29 (100) | 25 (96.2) | 0.302 |
| Prescribe emergency contraception | Yes | 76 (88.4) | 30 (96.8) | 25 (89.3) | 21 (77.8) | 0.081 |
| Counsel about pregnancy termination options | Yes | 81 (94.2) | 31 (100) | 28 (96.6) | 22 (84.6) | 0.023 |
| Inform where to go to obtain an abortion | Yes | 74 (86.1) | 31(100) | 23 (79.3) | 20 (76.9) | 0.006 |
OBG, Obstetrics/Gynecology; FM,Family Medicine; Peds, Pediatrics.
*"Yes” indicates residents believe activity is part of the scope of their practice.
‡P value not calculated.
Table 3. Resident perceptions of their training in adolescent medicine. Percent of residents within a given field that answered adequate or excellent training (Adequate) with the remainder (not shown) answering either no or minimal training.
| All | OBG | FM | Peds | |||
| Topic | Training | (n = 87) | (n=31) | (n=29) | (n=27) | p value |
| Activity with Adolescent Patients | n (%) | n (%) | n (%) | n (%) | ||
| General | ||||||
| Define confidentiality | Adequate | 71 (81.6) | 20 (64.5) | 26 (89.7) | 25 (92.6) | 0.009 |
| Counsel about eating habits and physical activity | Adequate | 65 (74.7) | 13 (41.9) | 26 (89.6) | 26 (96.3) | < 0.001 |
| Psychiatric | ||||||
| Counsel about eating disorders and body image | Adequate | 53 (60.9) | 12 (38.7) | 23 (79.3) | 18 (66.7) | 0.004 |
| Screen for depression and suicidal ideation | Adequate | 65 (74.7) | 16 (51.6) | 27 (93.1) | 5 (81.5) | 0.001 |
| Substance abuse | ||||||
| Screen and counsel about tobacco, alcohol, and drug use | Adequate | 73 (83.9) | 22 (71.0) | 28 (96.6) | 23 (85.2) | 0.022 |
| Abuse | ||||||
| Screen for physical abuse | Adequate | 61 (70.1) | 18 (58.1) | 23 (79.3) | 20 (74.1) | 0.172 |
| Screen for sexual abuse | Adequate | 58 (66.7) | 18 (58.1) | 21 (72.4) | 19 (70.4) | 0.443 |
| Sexual health | ||||||
| Discuss number and gender of sexual partners | Adequate | 70 (80.5) | 21 (67.7) | 27 (93.1) | 22 (81.5) | 0.046 |
| Conduct pelvic exams with sample collection | Adequate | 73 (83.9) | 26 (83.9) | 29 (100) | 18 (66.7) | 0.001 |
| Counsel about STD prevention | Adequate | 80 (92.0) | 27 (87.1) | 28 (96.6) | 25 (92.6) | 0.437 |
| Teach correct condom use | Adequate | 46 (52.9) | 17 (54.8) | 17 (58.6) | 12 (44.4) | 0.548 |
| Counsel about contraception | Adequate | 71 (81.6) | 25 (80.7) | 27 (93.1) | 19 (70.4) | 0.089 |
| Prescribe contraception | Adequate | 71 (81.6) | 26 (83.9) | 28 (96.6) | 17 (63.0) | 0.005 |
| Counsel about emergency contraception | Adequate | 62 (71.3) | 24 (77.4) | 26 (89.7) | 12 (44.4) | 0.001 |
| Prescribe emergency contraception | Adequate | 60 (69.0) | 24 (77.4) | 25 (86.2) | 11 (40.7) | 0.001 |
| Counsel about pregnancy termination options | Adequate | 58 (66.7) | 25 (80.7) | 23 (79.3) | 10 (37.0) | < 0.001 |
OBG, Obstetrics/Gynecology; FM,Family Medicine; Peds, Pediatrics.
Table 4. Resident experience with adolescent patients. Percent of residents within a field that answered “yes” to having had at least one encounter of a given activity.
| EXP* | All | OBG | FM | Peds | ||
| Topic | (n = 87) | (n=31) | (n=29) | (n=27) | p value | |
| Activity with Adolescent Patients | n (%) | n (%) | n (%) | n (%) | ||
| General | ||||||
| Define confidentiality | Yes | 82 (94.3) | 26 (83.9) | 29 (100) | 27 (100) | 0.010 |
| Evaluated positive aspects of life | Yes | 62 (84.9) | 9 (52.9) | 27 (93.1) | 26 (96.3) | < 0.001 |
| Counseled obese adolescent about weight loss | Yes | 71 (81.6) | 18 (58.1) | 26 (89.7) | 27 (100) | < 0.001 |
| Psychiatric | ||||||
| Counseled adolescent with eating disorder | Yes | 38 (43.7) | 10 (32.3) | 15 (51.7) | 13 (48.2) | 0.269 |
| Counseled adolescent with depression | Yes | 61 (70.1) | 17 (54.8) | 25 (86.2) | 19 (70.4) | 0.030 |
| Counseled suicidal adolescent | Yes | 37 (42.5) | 9 (29.0) | 11 (37.9) | 17 (63.0) | 0.028 |
| Substance abuse | ||||||
| Counseled about tobacco cessation | Yes | 79 (90.8) | 26 (83.9) | 27 (93.1) | 26 (96.3) | 0.267 |
| Counseled about alcohol use | Yes | 76 (87.4) | 22 (71.0) | 28 (96.6) | 26 (96.3) | 0.003 |
| Counseled about drug use | Yes | 78 (89.7) | 23 (74.2) | 28 (96.6) | 27 (100) | 0.002 |
| Referred to substance abuse treatment program | Yes | 23 (26.4) | 14 (45.2) | 5 (17.2) | 4 (14.8) | 0.013 |
| Abuse | ||||||
| Counseled adolescent who experienced physical abuse | Yes | 27 (31.0) | 12 (38.7) | 11 (37.9) | 4 (14.8) | 0.090 |
| Counseled adolescent who experienced sexual abuse | Yes | 36 (41.9) | 13 (41.9) | 11 (37.9) | 12 (46.2) | 0.827 |
| Sexual health | ||||||
| Discuss number and gender of sexual partners | Yes | 76 (87.4) | 23 (74.2) | 27 (93.1) | 26 (96.3) | 0.035 |
| Counseled about STD risk and prevention | Yes | 84 (96.6) | 28 (90.3) | 29 (100) | 27 (100) | 0.105 |
| Taught correct condom use | Yes | 42 (48.8) | 14 (46.7) | 16 (55.2) | 12 (44.4) | 0.694 |
| Counseled about contraception options | Yes | 78 (89.7) | 26 (83.9) | 29 (100) | 23 (85.2) | 0.057 |
| Prescribed emergency contraception | Yes | 45 (51.7) | 17 (54.8) | 18 (62.1) | 10 (37.0) | 0.158 |
| Counseled about pregnancy termination options | Yes | 46 (52.9) | 22 (71.0) | 17 (58.6) | 7 (25.9) | 0.002 |
| Number of times performed pelvic exam | 0 | 7 (8.1) | 2 (6.7) | 1 (3.5) | 4 (14.8) | 0.060 |
| 1-10 | 28 (32.6) | 7 (23.3) | 10 (34.5) | 11 (40.7) | ||
| 11-20 | 18 (20.9) | 7 (23.3) | 3 (10.3) | 8 (29.6) | ||
| 21-50 | 22 (25.6) | 8 (26.7) | 10 (34.5) | 4 (14.8) | ||
| > 50 | 11 (12.8) | 6 (20.0) | 5 (17.2) | 0 (0) | ||
| Number of times prescribed contraception | 0 | 10 (11.6) | 2 (6.7) | 1 (3.5) | 7 (25.9) | 0.003 |
| 1-10 | 32 (37.2) | 6 (20.0) | 14 (48.2) | 12 (44.4) | ||
| 11-20 | 17 (19.8) | 9 (30.0) | 3 (10.3) | 5 (18.5) | ||
| 21-50 | 14 (16.3) | 4 (13.3) | 8 (27.6) | 2 (7.4) | ||
| > 50 | 13 (15.1) | 9 (30.0) | 3 (10.3 | 1 (3.7) |
*EXP, experience. ‘Yes’ refers to having had at least one clinical encounter of a given activity, except for the last two items in which percentages reflect resident reports of having had the # of clinical encounters as categorized in the table.
Table 5. Survey items for which differences by field are altered when intern level residents are excluded from the analysis.
| All | OBG | FM | Peds | p value | ||
| Answer | (n = 60) | (n=22) | (n=19) | (n=19) | ||
| Question Topic | n (%) | n (%) | n (%) | n (%) | ||
| Training | ||||||
| Conduct pelvic exams with sample collection | Good | 53 (88.3) | 18 (81.8) | 19 (100) | 16 (84.2) | 0.174 |
| Counsel about contraception | Good | 55 (91.7) | 19 (86.4) | 19 (100) | 17 (89.5) | 0.357 |
| Prescribe contraception | Good | 53 (88.3) | 19 (86.4) | 19 (100) | 15 (78.9) | 0.137 |
| Experience | ||||||
| Define confidentiality | Yes | 57 (95.0) | 19 (86.4) | 19 (100) | 19 (100) | 0.102 |
| Counseled adolescent with depression | Yes | 46 (76.7) | 14 (63.6) | 17 (89.5) | 15 (78.9) | 0.148 |
| Counseled about drug use | Yes | 57 (95.0) | 19 (86.4) | 19 (100) | 19 (100) | 0.102 |
| Discussed number and gender of sexual partners | Yes | 55 (91.7) | 18 (81.8) | 18 (94.7) | 19 (100) | 0.118 |
| Counseled about contraceptive options | Yes | 59 (98.3) | 21 (95.5) | 19 (100) | 19 (100) | 1.000 |
| Prescribed emergency contraception | Yes | 42 (70.0) | 16 (72.7) | 17 (89.5) | 9 (47.4) | 0.019* |
OBG, Obstetrics/Gynecology; FM,Family Medicine; Peds, Pediatrics.
*In this item, the difference between fields becomes significant when interns are excluded. For other items in table, significance is lost when interns are excluded from analysis.
Survey.
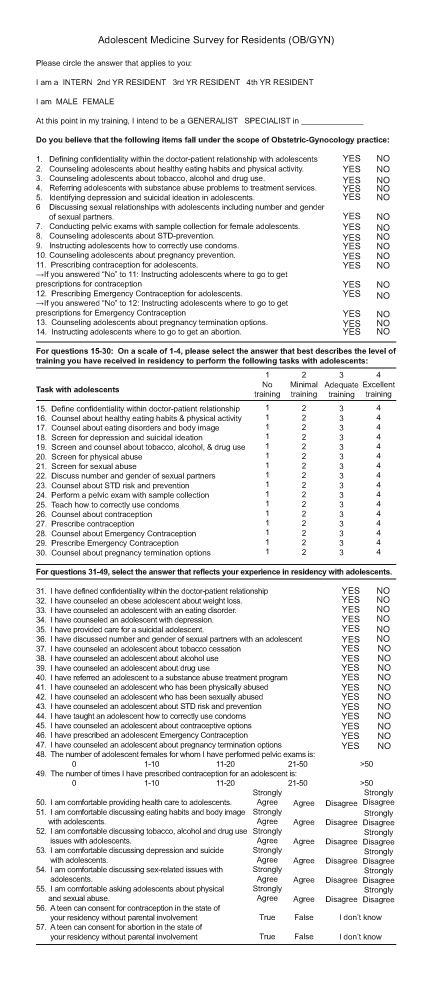
Adolescent Medicine Survey for Residents (OB/GYN)
Abbreviations
- FM
family medicine
- OB/GYN
obstetrics and gynecology
- STI
sexually transmitted infections
- NAMCS
National Ambulatory Medical Care Survey
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- AAP
American Academy of Pediatrics
- AAFP
American Academy of Family Physicians
- ACOG
American College of Obstetricians and Gynecologists
References
- Ma J, Wang Y, Stafford RS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36(5):441. doi: 10.1016/j.jadohealth.2004.08.024. [DOI] [PubMed] [Google Scholar]
- Chung PJ. et al. Preventive care for children in the United States: quality and barriers. Annu Rev Public Health. 2006;27:491–515. doi: 10.1146/annurev.publhealth.27.021405.102155. [DOI] [PubMed] [Google Scholar]
- Ozer EM. et al. Provider self-efficacy and the screening of adolescents for risky health behaviors. J Adolesc Health. 2004;35(2):101–107. doi: 10.1016/j.jadohealth.2003.09.016. [DOI] [PubMed] [Google Scholar]
- Fisher M. et al. Update on adolescent health care in pediatric practice. J Adolesc Health. 1996;19(6):394–400. doi: 10.1016/s1054-139x(96)00161-9. [DOI] [PubMed] [Google Scholar]
- Golden NH. et al. Emergency contraception: pediatricians' knowledge, attitudes, and opinions. Pediatrics. 2001;107(2):287–292. doi: 10.1542/peds.107.2.287. [DOI] [PubMed] [Google Scholar]
- Kelts EA, Allan MJ, Klein JD. Where are we on teen sex?: Delivery of reproductive health services to adolescents by family physicians. Fam Med. 2001;33(5):376–381. [PubMed] [Google Scholar]
- Wiesenfeld HC. et al. Knowledge about sexually transmitted diseases in women among primary care physicians. Sex Transm Dis. 2005;32(11):649–653. doi: 10.1097/01.olq.0000175393.71642.c8. [DOI] [PubMed] [Google Scholar]
- Ashton MR. et al. Primary care physician attitudes regarding sexually transmitted diseases. Sex Transm Dis. 2002;29(4):246–251. doi: 10.1097/00007435-200204000-00011. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Gandhi H, Cheng TL. Availability of adolescent health services and confidentiality in primary care practices. Pediatrics. 2003;111(2):394–401. doi: 10.1542/peds.111.2.394. [DOI] [PubMed] [Google Scholar]
- Rand CM. et al. Preventive counseling at adolescent ambulatory visits. J Adolesc Health. 2005;37(2):87–93. doi: 10.1016/j.jadohealth.2005.02.008. [DOI] [PubMed] [Google Scholar]
- Graves CE, Bridge MD, Nyhuis AW. Residents’ perception of their skill levels in the clinical management of adolescent health problems. J Adolesc Health. 1987;8(5):413–418. doi: 10.1016/0197-0070(87)90229-4. [DOI] [PubMed] [Google Scholar]
- Orr DP. et al. Adolescent health care: perceptions and needs of the practicing physician. J Adolesc Health. 1987;8(3):239–245. doi: 10.1016/0197-0070(87)90427-x. [DOI] [PubMed] [Google Scholar]
- [cited 2006];National Survey of Adolescents and Young Adults: Sexual Health Knowledge, Attitudes and Experiences [Internet] 2003 Available from: http://www.kff.org/youthhivstds/3218-index.cfm.
- Ewing GB. et al. Self-report of delivery of clinical preventive services by U.S. physicians. Comparing specialty, gender, age, setting of practice, and area of practice. Am J Prev Med. 1999;7(1):62–72. doi: 10.1016/s0749-3797(99)00032-x. [DOI] [PubMed] [Google Scholar]
- Orr MT. Private physicians and the provision of contraceptives to adolescents. Family Planning Perspectives. 1984;16(2):83–86. [PubMed] [Google Scholar]
- Klein JD, Wilson KM. Delivering quality care: adolescents’ discussion of health risks with their providers. J Adolesc Health. 2002;30(3):190–195. doi: 10.1016/s1054-139x(01)00342-1. [DOI] [PubMed] [Google Scholar]
- Haley N. et al. Sexual health risk assessment and counseling in primary care: how involved are general practitioners and obstetrician-gynecologists? Am J Public Health. 1999;89(6):899–902. doi: 10.2105/ajph.89.6.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller NH, Miller DJ, Pinkston Koenigs LM. Attitudes of the physician membership of the society for adolescent medicine toward medical abortions for adolescents. Pediatrics. 1998;101(5):E4. doi: 10.1542/peds.101.5.e4. [DOI] [PubMed] [Google Scholar]
- Ziv A, Boulet JR, Slap GB. Utilization of physician offices by adolescents in the United States. Pediatrics. 1999;104(1 Pt 1):35–42. doi: 10.1542/peds.104.1.35. [DOI] [PubMed] [Google Scholar]
- Klein JD, McNulty M, Flatau CN. Adolescents’ access to care: teenagers’ self-reported use of services and perceived access to confidential care. Arch Pediatr Adolesc Med. 1998;152(7):676–682. doi: 10.1001/archpedi.152.7.676. [DOI] [PubMed] [Google Scholar]
- Rand CM. et al. National health care visit patterns of adolescents: implications for delivery of new adolescent vaccines. Arch Pediatr Adolesc Med. 2007;161(3):252–259. doi: 10.1001/archpedi.161.3.252. [DOI] [PubMed] [Google Scholar]
- Beatty ME, Lewis J. Adolescent contraceptive counseling and gynecology: a deficiency in pediatric office-based care. Conn Med. 1994;58(2):71–78. [PubMed] [Google Scholar]
- Wallace JL. et al. Emergency contraception: knowledge and attitudes of family medicine providers. Fam Med. 2004;36(6):417–422. [PubMed] [Google Scholar]
- Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001-02. Vital Health Stat 13. 2006;159:1–66. [PubMed] [Google Scholar]
- Saslow D. et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52(6):342–362. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- Shafer MA, Pantell RH, Schachter J. Is the routine pelvic examination needed with the advent of urine-based screening for sexually transmitted diseases? Arch Pediatr Adolesc Med. 1999;153(2):119–125. doi: 10.1001/archpedi.153.2.119. [DOI] [PubMed] [Google Scholar]
- Peralta L, Durako SJ, Ma Y. Correlation between urine and cervical specimens for the detection of cervical Chlamydia trachomatis and Neisseria gonorrhoeae using ligase chain reaction in a cohort of HIV infected and uninfected adolescents. J Adolesc Health. 2001;29(3 Suppl):87–92. doi: 10.1016/s1054-139x(01)00283-x. [DOI] [PubMed] [Google Scholar]
- Revised oral contraceptive labeling: FDA approves recommendation allowing delay of pelvic exam. Contracept Rep. 1993;4(5):4–7. [PubMed] [Google Scholar]
- ACOG Committee Opinion. Number 335, May 2006: The initial reproductive health visit. Obstet Gynecol. 2006;107(5):1215–1219. doi: 10.1097/00006250-200605000-00053. [DOI] [PubMed] [Google Scholar]
- Laube DW, Ling FW. Primary care in obstetrics and gynecology resident education: a baseline survey of residents’ perceptions and experiences. Obstet Gynecol. 1999;94(4):632–636. doi: 10.1016/s0029-7844(99)00350-6. [DOI] [PubMed] [Google Scholar]
- Davis DA. et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- Yeazel MW, Lindstrom Bremer KM, Center BA. A validated tool for gaining insight into clinicians' preventive medicine behaviors and beliefs: the preventive medicine attitudes and activities questionnaire (PMAAQ) Prev Med. 2006;43(2):86–91. doi: 10.1016/j.ypmed.2006.03.021. [DOI] [PubMed] [Google Scholar]
- Huang J. et al. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156–161. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]


