Abstract
Purpose
To investigate the level of burnout in the oncology community in the United States.
Patients and Methods
Seven thousand seven hundred fifteen oncology physicians were queried by e-mail or during attendance at oncologic meetings and asked to complete a 22-question survey concerning their feelings of personal burnout and their perceptions of physician burnout in the oncology community. The data were analyzed using standard statistical methods including a multivariate analyses using logistic regression with stepwise selection.
Results
One thousand seven hundred forty oncologists (22.6%) completed and returned the survey, with 92.6 % representing medical oncologists or hematologist-oncologists. Two thirds of the respondents were from community practice and one third from academia. Overall, 61.7% of the respondents reported feelings of burnout, with the top three signs being frustration (78%), emotional exhaustion (69%), and lack of satisfaction with their work (50%). The highest-ranked causes for their feelings of burnout included overwork, lack of time away from the office, and reimbursement concerns. The top remedies for burnout were felt to be fewer patients, more time away from the office, and increased attendance at medical meetings. The multivariate analyses demonstrated highly significant associations between burnout and hours spent on patient care, personal time off, and number of educational meetings attended.
Conclusion
The rate of burnout in the oncology community of the United States exceeds 60%. This report suggests causes and potential solutions for the high rate of burnout. Such information may lead to an improved understanding of the needed steps to improve the quality of life for the oncology community with the ultimate goal of further improving patient care. Patients deserve optimal medical and emotional support that is best provided by caring and well-informed practitioners.
Introduction
Medical professionals in general and practitioners of oncology specifically face a host of highly stressful issues on a daily basis during the routine practice of their profession. Such stresses include dealing with extremely, and often terminally, ill patients who require and deserve a great deal of emotional support as well as high quality and optimal medical care; an ever more complex and rapidly evolving diagnostic and therapeutic landscape; increasing financial stresses that derive from a combination of more complex and more expensive therapeutic options coupled with simultaneous changes in federal reimbursement strategies; and ever-increasing patient numbers and complexities. The end result of these stresses is reflected in high rates of burnout among medical practitioners. Mount describes burnout as the end result of stress in one's professional life that ultimately results in apathy, suspicion, self-protection, disillusion, and depression.1,2 Whippen and Canellos1 performed an investigation in 1,000 randomly selected physician subscribers to the Journal of Clinical Oncology in the spring of 1990. This study was designed to quantitate the level of burnout in the oncology community and to better understand the causes and potential remedies for physician burnout. This investigation found the rate of burnout to be 56% among all 598 respondents, and specifically 58% for adult medical oncologists. Of interest, university-based oncologists reported a lower incidence of burnout (47%). Lack of personal time away from the office was cited as the most common (57%) reason for burnout as well as what the majority (69%) of oncologists felt would alleviate their feelings of burnout. A subsequent survey by Whippen et al3 was conducted in 16,635 ASCO members in 2002. Among the 1,299 respondents (12.8%), 34% reported burnout. Lack of time away from the office continued to be the reason most commonly (40%) cited for burnout, and more personal time was most often (46%) felt to be a potential remedy for burnout.
Given the ever-changing stresses associated with the practice of medicine, we felt it was important to reassess the level of burnout among U.S. oncologists to understand any changes that may have occurred in the oncology community in recent times. The Network for Medical Communication and Research developed a 22-question survey based on the earlier published burnout survey with the goal of reassessing the level of burnout specifically in the oncology physician community of the United States. The survey defined “burnout” as “the end result of stress resulting in emotional exhaustion, apathy, suspicion, disillusion, diminished empathy, lack of a sense of achievement or work satisfaction and depression.” The survey was distributed to oncologists throughout the United States via e-mail and at live educational meetings.
Materials and Methods
Survey Population
The survey was sent via e-mail on three separate occasions to a database of 7,715 U.S. oncologists maintained by the Network for Medical Communication and Research of all U.S. oncologists who participate in their educational programs. The surveys were sent over a 2-month period during April and May 2003. On each occasion that the survey was sent to the oncology community, oncologists were instructed to complete the survey only if they had not already done so. In addition, the survey was circulated to oncologists who attended the Network for Medical Communication and Research live educational meetings during this same time period (also included in the database of 7,715 U.S. oncologists). The physicians attending the live meetings were instructed to not complete the survey if they had previously completed an electronic version. No compensation of any kind was provided for completing the survey.
Questionnaire
The questionnaire comprised a total of 22 questions. The demographics of the responding population was explored in 15 questions and the physicians were asked to prioritize their presumptive causes for, adverse effects from, and potential solutions to their signs of burnout.
Statistical Analysis
Demographic variables were tested for ordinal association with burnout by the Jonckheere-Terpstra trend test.4 When ordinal association was either not possible or not apparent, association with burnout was tested with Fisher's exact test5 for variables with two response levels and the χ2 test6 for variables with more than two response levels. Multivariate analyses used logistic regression with stepwise selection7 to identify a subset of demographic variables that were independently important in explaining the likelihood of burnout. All analyses were carried out using the SAS system for Windows, version 8.02 (SAS Institute, Inc., Cary, NC).
Results
Demographics
Of the 7,715 physicians solicited via the Internet and at live meetings, 1,464 (19%) responded by completing the survey using the Internet and 276 (3.6%) via the live meetings. Although there were minor differences in demographics and responses from the two sets of physicians, the data were combined for a total of 1,740 respondents (22.6%) to best reflect the population of physicians we were trying to describe. The demographics for the 1,740 respondents are shown in Table 1.3 Of interest, 93% were either medical oncologists (23.3%) or medical hematologist-oncologists (69.3%). Two thirds were from community practice, with the balance being from an academic or salaried position. The sample was equitably distributed across the United States. Fourteen percent of the respondents were solo practitioners, whereas 44% had at least six partners in their practices. Eighty percent spent at least 71% of their time on patient care, with 69% caring for more than 51 patients per week and, remarkably, 64% spending at least 51 hours per week on patient care. Despite these extremely heavy patient care responsibilities, two thirds spent at least 4 to 7 hours each week in educational activities related to their profession and almost half attended four or more live meetings each year in pursuit of education.
Table 1.
Demographic questions
| Question | No. | % |
|---|---|---|
| How would you define your specialty? | ||
| Medical oncologist | 406 | 23.33 |
| Medical oncologist/hematologist | 1,206 | 69.31 |
| Hematologist | 24 | 1.38 |
| Radiation oncologist | 40 | 2.3 |
| Pediatric oncologist | 10 | 0.57 |
| Surgical oncologist | 11 | 0.63 |
| Gynecologic oncologist | 33 | 1.9 |
| Gastroenterologist | 1 | 0.06 |
| Urologist | 3 | 0.17 |
| No response | 6 | 0.34 |
| Which best describes your practice? | ||
| Community practice | 1,159 | 66.61 |
| Academic or salaried practice | 560 | 32.18 |
| No response | 21 | 1.21 |
| Where is your practice based? | ||
| Northeast | 543 | 31.21 |
| South | 417 | 23.97 |
| Midwest | 362 | 20.8 |
| West | 181 | 10.4 |
| Southwest | 174 | 10 |
| Northwest | 42 | 2.41 |
| No response | 21 | 1.21 |
| When did you complete your oncology training? | ||
| Before 1970 | 59 | 3.39 |
| 1970-1975 | 158 | 9.08 |
| 1976-1980 | 231 | 13.28 |
| 1981-1985 | 270 | 15.52 |
| 1986-1990 | 219 | 12.59 |
| 1991-1995 | 248 | 14.25 |
| 1996-2000 | 247 | 14.2 |
| After 2000 | 295 | 16.95 |
| No response | 13 | 0.75 |
| How many physicians are in your practice? | ||
| Solo | 251 | 14.43 |
| 5 | 719 | 41.32 |
| 6-10 | 314 | 18.05 |
| > 10 | 436 | 25.06 |
| No response | 20 | 1.15 |
| What percentage of your time is devoted to patient care activities? | ||
| 0-10% | 15 | 0.86 |
| 11-25% | 24 | 1.38 |
| 26-40% | 48 | 2.76 |
| 41-55% | 74 | 4.25 |
| 56-70% | 158 | 9.08 |
| 71-85% | 303 | 17.41 |
| > 85% | 1,084 | 62.3 |
| No response | 34 | 1.95 |
| What percentage of your time is devoted to either clinical (excluding patient care) or laboratory research? | ||
| 0-10% | 1,195 | 68.68 |
| 11-25% | 327 | 18.79 |
| 26-40% | 74 | 4.25 |
| 41-55% | 43 | 2.47 |
| 56-70% | 22 | 1.26 |
| 71-85% | 23 | 1.32 |
| > 85% | 37 | 2.13 |
| No response | 19 | 1.09 |
| What percentage of your time is dedicated to teaching activities? | ||
| 0-10% | 1,265 | 72.7 |
| 11-25% | 377 | 21.67 |
| 26-40% | 46 | 2.64 |
| 41-55% | 13 | 0.75 |
| 56-70% | 7 | 0.4 |
| 71-85% | 3 | 0.17 |
| > 85% | 3 | 0.17 |
| No response | 26 | 1.49 |
| What percentage of your time is dedicated to administrative activities? | ||
| 0-10% | 1,175 | 67.53 |
| 11-25% | 467 | 26.84 |
| 26-40% | 48 | 2.76 |
| 41-55% | 15 | 0.86 |
| 56-70% | 4 | 0.23 |
| > 85% | 5 | 0.29 |
| No response | 26 | 1.49 |
| Approximately how many patients do you see in a typical week? | ||
| 0-10 | 35 | 2.01 |
| 11-30 | 174 | 10 |
| 31-50 | 305 | 17.53 |
| 51-75 | 436 | 25.06 |
| 76-100 | 460 | 26.44 |
| > 100 | 301 | 17.3 |
| No response | 29 | 1.67 |
| How many hours do you spend in patient related activities in a typical week? | ||
| 0-10 | 32 | 1.84 |
| 11-30 | 142 | 8.16 |
| 31-50 | 436 | 25.06 |
| 51-75 | 754 | 43.33 |
| 76-100 | 295 | 16.95 |
| > 100 | 69 | 3.97 |
| No response | 12 | 0.69 |
| Do you feel that you are experiencing any signs of “burnout”? | ||
| Yes | 1,073 | 61.67 |
| No | 648 | 37.24 |
| No response | 19 | 1.09 |
| Do you believe any of your colleagues have suffered or are suffering from “burnout”? | ||
| Yes | 1,447 | 83.16 |
| No | 235 | 13.51 |
| No response | 58 | 3.33 |
| How many days of personal time (excluding weekends) have you taken in the last year? | ||
| 0-5 | 201 | 11.55 |
| 6-10 | 318 | 18.28 |
| 11-15 | 378 | 21.72 |
| 16-21 | 406 | 23.33 |
| > 21 | 406 | 23.33 |
| No response | 31 | 1.78 |
| Approximately how many hours each week do you spend keeping up with your educational needs? | ||
| 1-3 | 587 | 33.74 |
| 4-7 | 768 | 44.14 |
| 8-12 | 260 | 14.94 |
| 13-20 | 60 | 3.45 |
| > 20 | 28 | 1.61 |
| No response | 37 | 2.13 |
| How many educational meetings have you attended in the last year? | ||
| None | 72 | 4.14 |
| 1-3 | 887 | 50.98 |
| 4-6 | 470 | 27.01 |
| 7-10 | 152 | 8.74 |
| > 10 | 126 | 7.24 |
| No response | 33 | 1.9 |
Rate of Burnout
As a group, 61.7% (95% CI, 59.39% to 63.95%) of the physicians stated that they had signs of burnout, and 83.2% felt that they detected signs of burnout in their colleagues. Seventy-seven percent of physicians reporting burnout felt that their signs of burnout were becoming more apparent. As shown in Table 2, the top three signs reported for feelings of burnout included frustration (78%), emotional exhaustion (69%), and lack of satisfaction with their work (50%). When asked to rank the causes of their burnout, the highest cause was felt to be overwork, followed by a lack of time away from the office and reimbursement-related stress. Their marriages were felt to suffer the most as a result of their burnout, followed by their careers. The top three mechanisms for alleviating burnout were felt to be more time away from the office, fewer patients to care for, and increased attendance at professional meetings—which were also ranked as their most favored means for obtaining medical education, followed by print sources and the Internet. Interestingly, audiotapes and video discs were felt to be the least favorable means for obtaining medical education.
Table 2.
Feelings, persistence, causes, adverse effects of, and ways to alleviate burnout
| Question | No. | % | Rank |
|---|---|---|---|
| If you answered yes to question #12, which of the following characterizes your sense of “burnout”? List all that apply. | |||
| Feelings of frustration | 841 | 78.4 | |
| Lack of empathy | 248 | 23.1 | |
| Apathy | 209 | 19.5 | |
| Emotional exhaustion | 738 | 68.8 | |
| Lack of a sense of achievement or work satisfaction | 535 | 49.9 | |
| Sense of failure | 233 | 21.7 | |
| Boredom | 180 | 16.8 | |
| Depression | 288 | 26.8 | |
| Disinterest | 242 | 22.6 | |
| Disillusionment | 430 | 40.1 | |
| If you answered yes to question #12, which of the following do you feel are the cause(s) for your sense of “burnout”? Rank order from most important = 1 to least important. | |||
| Insufficient personal/vacation time | 2 | ||
| Academic or salaried practice | 4 | ||
| Frustration with limited therapeutic success | 5 | ||
| Reimbursement uncertainties | 3 | ||
| Lack of intellectual stimulation | 6 | ||
| Overwork | 1 | ||
| Other | 7 | ||
| If you answered yes to question #12, rank order (most affected = 1 to least affected) each of the following that you feel has been adversely affected by “burnout”? | |||
| Marriage | 1 | ||
| Relationship with children | 4 | ||
| Relationships other than spouse or children | 3 | ||
| Career | 2 | ||
| Other | 5 | ||
| If you answered yes to #12, do you feel that, over the last 3 to 5 years, your level of “burnout” has: | |||
| Remained generally constant | 182 | 16.96 | |
| Become generally more intense | 824 | 76.79 | |
| Become generally less intense | 49 | 4.57 | |
| No response | 18 | 1.68 | |
| Which of the following do you feel would be ways to alleviate “burnout”? Rank order from most important = 1 to least important. | |||
| More vacation/personal time | 1 | ||
| Sabbaticals | 4 | ||
| Greater intellectual stimulation through more professional travel to interact with peers at meetings | 3 | ||
| Fewer patients | 2 | ||
| Greater intellectual stimulation through research involvement | 5 | ||
| Greater intellectual stimulation through teaching | 6 | ||
| Greater administrative involvement | 7 | ||
| Other | 8 | ||
| Which do you consider to be a desirable means for exchanging information? Rank order from most desirable = 1 to least desirable. | |||
| Print media | 2 | ||
| Audio CDs | 4 | ||
| Peer-to-peer meetings | 1 | ||
| Internet programs | 3 | ||
| Video conferencing | 5 | ||
| Other | 6 | ||
Univariate Analyses
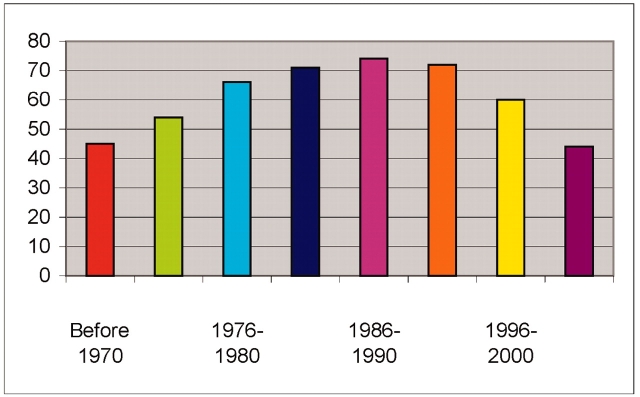
We next performed univariate analyses to assess the associations between signs of burnout and each of the demographic factors (Table 3). In this analysis, we identified 12 primary factors that were significantly associated with burnout. Specifically, community oncologists experienced significantly more burnout than academic oncologists. Burnout was more prevalent in oncologists who spent more of their time on patient care, with increasing hours per week on patient care, and with greater numbers of patients seen per week. Similarly, those involved with more administrative activities also demonstrated significantly more burnout. In terms of length of oncology service, those between 10 and 25 years after completing their oncology training demonstrated the highest level of burnout (Fig 1). In contrast, those who spend more time in research or teaching have less burnout. Other factors that were associated with less burnout included attendance at more educational meetings, increasing number of hours devoted to educational pursuits, and increased amounts of time away from work. Of note, neither the geographic location of the individual's practice nor the area of subspecialty were significantly associated with burnout.
Table 3.
Univariate and multivariate association of demographic variables with burnout, listed in order of decreasing multivariate significance
| Question | Type of Association | Univariate P | Multivariate P |
|---|---|---|---|
| Do you believe any of your colleagues have suffered or are suffering from “burnout”? | General | < .0001 | < .0001 |
| How many hours do you spend in patient related activities in a typical week? | Ordinal | < .0001 | < .0001 |
| When did you complete your oncology training? | General | < .0001 | < .0001 |
| How many educational meetings have you attended in the past year? | Ordinal | < .0001 | < .0001 |
| How many days of personal time (excluding weekends) have you taken in the past year? | Ordinal | .0005 | < .0001 |
| What percentage of your time is dedicated to administrative activities? | Ordinal | < .0001 | < .0001 |
| Which best describes your practice? | General | .0055 | .0008 |
| Approximately how many patients do you see in a typical week? | Ordinal | < .0001 | .0027 |
| What percentage of your time is dedicated to teaching activities? | Ordinal | .0032 | .0081 |
| What percentage of your time is devoted to patient care activities? | Ordinal | < .0001 | .0188 |
| Approximately how many hours each week do you spend keeping up with your educational needs? | Ordinal | < .0001 | .0338 |
| The questions below were excluded from the multivariate model. The multivariate P value shown is the P value obtained by individually adding these questions to the model above. | |||
| Where is your practice based? | General | .1688 | .0672 |
| What percentage of your time is devoted to either clinical (excluding patient care) or laboratory research? | Ordinal | .0003 | .111 |
| How many physicians are in your practice? | Ordinal | .4028 | .5251 |
| How would you define your specialty? | General | .638 | .5291 |
Figure 1.
Percentage of burnout by year oncology training was completed. Illustrates the percentage of physicians who acknowledge feelings of burnout as a function of the year in which they completed their oncology training.
Multivariate Analysis
Because many of the variables queried could be confounded, we performed a multivariate analysis to see which variables would remain significantly associated with burnout. Surprisingly, 11 of the 12 variables identified as significant in univariate testing remained independently significant in the multivariate logistic regression model. Only percentage of time spent on research was not significant in multivariate testing after being identified as significant in a univariate test. Table 3 lists the variables that remained significant in order of decreasing significance. Of particular note, hours spent on patient care and having colleagues with burnout were amongst the most critical positive associations with burnout, whereas attendance at educational meetings and number of days away from the office were highly significantly associated with less burnout. Physicians with fewer than 10 or more than 25 years since completing their training had significantly less burnout than their counterparts who completed their training 10 to 25 years ago.
Discussion
This survey included the opinions of 1,740 oncologists working throughout the United States and represents the largest published sampling of U.S. oncologists. This response represented almost 22% of the physicians surveyed in the Network for Medical Communication and Research database of 7,715, which is not as high a response rate as the original study published by Whippen and Canellos in 1991 but is almost twice as high as the more recent study presented at the 2004 ASCO annual meeting (June 5-8, New Orleans, Louisiana). Unlike prior surveys, which used the mail service, our survey relied primarily on electronic media. This difference may account for some of the differences in response rates.
In general, the surveyed population consisted of medical oncologists or hematologist-oncologists who represented equally the major geographic areas in the United States. As expected, most of the respondents spent the majority of their effort on patient care activities. Overall, we identified a rate of perceived burnout of almost 62% among the surveyed population. This rate is very similar to the 56% rate reported by Whippen and Cannellos in 598 physician subscribers to the Journal of Clinical Oncology in 1991, and substantially higher than the 34% reported in 2004 among 1,299 members of the American Society of Clinical Oncology surveyed in 2002.1,3 Why the most recent rate of burnout reported is relatively low is not clear; however, differences in the demographics of the respondents may provide an explanation. A similar survey of burnout in almost 400 cancer clinicians and palliative care specialists in the United Kingdom published in 1995 found a rate of 28% in this population.8 Presumably, many differences in the stresses impacting care providers in Europe may account for the noted rate differences between the populations, and the relatively lower rate of burnout reported in the United Kingdom may in part explain the recently reported lower rates, because the surveyed population may have included oncologists outside the United States.3 It is interesting to note that the rate of self-assessed burnout appears to be relatively stable since the initial survey performed 14 years prior to the present survey, despite the apparent increased reimbursement concerns and complexity of oncology patient management coupled with the perception in 77% who reported that their signs of burnout were becoming more apparent. As is the case with any survey, there is an inherent selection bias in those electing to complete the survey. This self-selection may bias the results and therefore needs to be considered in drawing definitive conclusions.
The primary reasons that were reported as the perceived cause for burnout were overwork and a lack of time away from the office. These causes were mirrored by the need for more time away from the office, including attendance at professional meetings and fewer patients as the most often stated remedies for the reported physician burnout. Recent reports have identified additional factors that contribute to lower rates of burnout including a “hardy personality,” a greater perception of oneself as being religious, and highly developed communication skills that promote a successful doctor-patient relationship.9,10 Because many of the factors that appeared to be directly related to the reported incidence of burnout could be confounded, we performed a multivariate analysis to identify those factors that retained an independent and significant association with burnout. As shown in Table 3, all but a single variable identified by univariate analysis remained significant in the multivariate model. Although the causes of burnout appear to be multifactorial, the most significant associations included the amount of time spent on patient care, lack of time away from the office, and attendance at fewer educational meetings. The peak in burnout appears to occur between 10 and 25 years after completing oncology training. These data suggest that it generally takes about 10 years to develop burnout. The decrease in burnout in physicians with more than 25 years after oncology training presumably reflects individuals who have either successfully developed mechanisms to alleviate burnout or who have changed careers and are therefore no longer represented in the population with more than 25 years of experience. Interestingly, neither the area of the country in which the clinician worked nor the number of partners in an oncology practice was associated with the rate of burnout.
These data support a relatively stable but high rate of perceived burnout in the U.S. oncology community that is attributable primarily to overwork and inadequate time away from the office. This information suggests a need to train more oncologists and to make provisions for increasing both personal time and time spent in educational pursuits through attendance at professional meetings.
Footnotes
Authors' Disclosure of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
References
- 1.Whippen DA, Canellos GP: Burnout syndrome in the practice of oncology: Results of a random survey of 1,000 oncologists. J Clin Oncol 9:1916-1920, 1991 [DOI] [PubMed] [Google Scholar]
- 2.Mount BM: Dealing with our losses. J Clin Oncol 4:1127-1134, 1986 [DOI] [PubMed] [Google Scholar]
- 3.Whippen DA, Zukerman EL, Andersen JW, et al: Burnout in the practice of oncology: Results of a follow-up survey. J Clin Oncol 22:532s, 1994. (suppl) [Google Scholar]
- 4.Pirie W: Encyclopedia of Statistical Sciences, vol 4, Jonckheere tests for ordered alternatives in Kotz S Johnson NL (eds.).New York, NY, John Wiley & Sons, Inc. 1983, 315-318 [Google Scholar]
- 5.Agresti A: An Introduction to Categorical Data Analysis. New York, NY, John Wiley & Sons, Inc. 1996
- 6.Fienberg SE: The Analysis of Cross-Classified Data: ed 2, Cambridge, MA, MIT Press, 1980
- 7.SAS Institute, Inc.: SAS/STAT User's Guide, Version 8. Cary, NC, SAS Institute, Inc. 1999
- 8.Ramirez AJ, Graham J, Richards MA, et al: Burnout and psychiatric disorder among cancer clinicians. Br J Cancer 71:1263-9, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kash KM, Holland JC, Breitbart W, et al: Stress and burnout in oncology. Oncology 14:1621-1633, 2000 [PubMed] [Google Scholar]
- 10.Armstrong J, Holland J: Surviving the stresses of clinical oncology by improving communication. Oncology 18:363-368, 2004 [PubMed] [Google Scholar]