Abstract
Previous research has shown that depression and social anxiety—two “facets” of internalizing psychopathology— both are characterized by low levels of extraversion/positive emotionality (E/PE). However, little is known about the relations of the facets of E/PE with symptoms of depression and social anxiety. This study utilized multiple measures of each facet of E/PE, as well as depression and social anxiety symptoms. Self-report data were collected from large samples of college students and psychiatric outpatients. Separate factor analyses in each sample revealed a four-factor structure of E/PE, consisting of Sociability, Positive Emotionality, Ascendance, and Fun-Seeking. Structural equation modeling revealed that, after controlling for the higher-order internalizing factor and the overlap among the E/PE facets, social anxiety was broadly related to all four facets of E/PE, whereas depression was strongly related only to low positive emotionality. Implications for hierarchical models of personality and psychopathology, assessment and treatment, and etiological models are discussed.
Keywords: depression, extraversion, internalizing, positive emotionality, social anxiety
Social anxiety disorder and depression are impairing, highly comorbid disorders (e.g., Kessler, Chiu, Demler, Merikangas, & Walters, 2005). According to the National Comorbidity Survey Replication, both are very common, with twelve-month prevalence rates of nearly 7%. Among the anxiety disorders, social anxiety is second only to generalized anxiety disorder for comorbidity with major depression (Kessler et al., 2005). Given the prevalence and high rate of comorbidity of depression and social anxiety, it is important for both theoretical and diagnostic purposes to delineate their phenotypes accurately.
Structural Models of Depression and Anxiety
Basic structural models of affect provide a framework for describing depression and anxiety symptoms. These hierarchical models state that each individual depressive and anxiety syndrome has a shared component (accounting for comorbidity among disorders), and its own unique component that distinguishes it from the others (e.g., Brown, Chorpita, & Barlow, 1998; Mineka, Watson, & Clark, 1998). Such models extend beyond descriptive symptomatology to include more long-standing associated personality traits. Because personality traits are heritable, relatively stable, and can predict and explain behaviors, the relations between personality and psychopathology has been a fruitful and expanding area of study (Krueger, McGue, & Iacono, 2001).
The source of common variance among these disorders— referred to as “internalizing”— is closely linked with the personality trait neuroticism/negative emotionality (N/NE; tendency to experience negative emotions, such as fear, anger, and sadness; Krueger et al., 2001). This shared component has been delineated well in structural models; in contrast, however, our understanding of sources of specific variance for depression and anxiety disorders is not well developed. Researchers have noted the importance of explicating these structural models to clarify the lower-order personality correlates of each disorder and its underlying symptoms (e.g., Clark, Watson, & Mineka, 1994; Markon, Krueger, & Watson, 2005; Tackett, Quilty, Sellbom, Rector, & Bagby, 2008).
Low positive emotionality (the tendency to experience positive emotions, such as joy and enthusiasm) was originally theorized to be specific to depression, distinguishing it from the anxiety disorders (Watson, Clark, & Carey, 1988). However, subsequent studies indicated that social anxiety is similarly characterized by low positive emotionality, and that positive emotionality is more strongly related to both depression (r = −.37 to −.63) and social anxiety (r = −.23 to −.47) than to any other anxiety symptoms (e.g., Brown et al., 1998; Sellbom, Ben-Porath, & Bagby, 2008; Watson et al., 1988; Watson, Gamez, & Simms, 2005). Thus, low positive emotionality is specific to both depression and social anxiety, but does not distinguish between them.
Because positive emotionality and the associated trait of extraversion subsume numerous distinguishable facets (Watson & Clark, 1997), exploring symptom relations at the lower-order trait level may be important in expanding structural models of depression and social anxiety to determine their shared and unique features. Furthermore, depression and social anxiety can be conceptualized as lower-order factors of internalizing; thus, an expanded structural model has broader implications for our understanding of the hierarchical structure of internalizing and N/NE. Finally, an improved understanding of the concomitants and distinguishing features of depression and social anxiety may have implications for assessment and treatment.
Positive Emotionality and Extraversion
Positive emotionality and extraversion are closely related constructs, with correlations ranging from .50 to .65 (Watson & Clark, 1992). Broadly speaking, extraversion may be defined as a multidimensional higher-order trait that includes both interpersonal/social and positive emotional facets (Watson & Clark, 1997). In this article, the higher-order construct will be referred to as “extraversion/positive emotionality” (E/PE) to explicitly include both components of the trait.
Facets of E/PE
There are numerous models of the hierarchical structure of E/PE (e.g., Costa & McCrae, 1992; Depue & Collins, 1999). All include facets assessing sociability and ascendance, but they differ regarding the inclusion of additional traits. Based on an extensive review of data relevant to E/PE models, Watson and Clark (1997) created an integrative structure that synthesizes the major components of the construct. Their model has four central facets: affiliation (warmth and gregariousness), positive affectivity (joy and enthusiasm), energy (liveliness and activity), and ascendance (exhibitionism and dominance).
Two additional facets are considered to be part of E/PE, but have a more peripheral role: venturesomeness (excitement-seeking and desire for change) and ambition (achievement and endurance). Venturesomeness (a trait related to impulsivity) is generally seen as overlapping with—but distinguishable from—E/PE, representing an interaction between extraversion and the trait of disinhibition (e.g., Depue & Collins, 1999). Ambition scales are most often located in the conscientiousness domain, rather than extraversion (e.g., Costa & McCrae, 1992; Markon et al., 2005; Simms, Wu, & Watson, 2001); therefore, the current study excludes ambition and instead focuses on the other five facets.
Relating Depression and Social Anxiety to the Facets of E/PE
Although many studies have examined the relation of E/PE to the internalizing disorders, little research has investigated how the facets of E/PE relate to these symptoms. Clark and colleagues (1994) describe the importance of examining both higher-order and lower-order personality variables in relation to psychopathology. Examining these relations at both levels is necessary to locate the appropriate level of abstraction that is responsible for a given association. Determining the “potent” level of the hierarchy allows for a more precise understanding of the relations among personality and psychopathology, while providing an expanded context in which to interpret the results. In this particular case, is the higher-order E/PE construct most relevant to understanding depression and social anxiety, or do the lower-order traits add additional information? Comprehensive facet-level studies are required to address this key issue.
To date, only one study has examined E/PE facets in relation to both social anxiety and depression. Using a population-based sample, Bienvenu et al. (2004) found that those diagnosed with social anxiety disorder scored significantly lower than controls on all six Extraversion facets of the Revised NEO Personality Inventory (NEO PI-R; Costa & McCrae, 1992), whereas only the Assertiveness scale was low for participants with depression. Two studies used multiple regression to examine the relation of NEO PI-R Extraversion facets to depression: low Warmth was a significant E/PE predictor in one (Costa, Bagby, Herbst, & McCrae, 2005), whereas low Positive Emotions was significant in another (Chioqueta & Stiles, 2005).
Thus, the few existing studies have not produced converging evidence as to which specific facets are most strongly related to each of these symptoms. Furthermore, the NEO PI-R was the sole measure of extraversion in all of the above studies, limiting the generalizability of these findings beyond this particular instrument. To address this concern, the current study includes multiple measures that collectively tap the entire E/PE construct. In addition, the above studies all utilized categorical diagnoses; the current study takes a dimensional symptom-based approach, as continuous assessments typically retain more information and are more stable than dichotomous assessments (Watson, 2005).
Methods
Participants
Participants consisted of two samples: 1) 350 introductory psychology students at the University of Iowa, recruited online through the introductory psychology research participation pool site, and 2) 204 psychiatric outpatients recruited from the waiting room of two local psychiatric care centers.1 Most of the psychiatric patients (90.6%) reported that they were currently taking one or more psychotropic medications, with 77.5% taking antidepressants and 31.5% taking antianxiety drugs.
The students had a mean age of 19.2 years (SD = 1.7) and 76.6% were female. In terms of ethnic background, 90.0% identified themselves as Caucasian, 5.4% as Asian/Pacific Islander, 2.3% as Black or African American, 1.7% as Hispanic, and 0.6% as other. Thirty-one students (8.9%) reported mental health treatment at the time of participation. The psychiatric patients had a mean age of 44.0 years (SD = 13.2; range = 18 to 74) and 68.5% were female. Ninety-two percent identified themselves as Caucasian, 2.0% as Asian, 2.0% as Black or African American, 0.5% as Hispanic, 1.0% as American Indian/Alaska native, and 2.5% as multiracial.
A subset of the psychiatric patients (N = 104; 51%) was diagnosed using the SCID-I/P (First, Spitzer, Gibbon, & Williams, 1997). Within this subset, 38% were diagnosed with current major depression and 13% were diagnosed with social phobia. These patients were interviewed as part of a related study; the interviewers were trained staff members who had masters' level training in clinical/counseling psychology or public heath. For that study, audiotape interrater reliability was excellent for both major depression (κ = .95) and social phobia (κ = .87) (Watson et al., 2008, Table 1).
Table 1.
Descriptive Statistics for Trait and Symptom Scales with Between-Sample Mean Comparisons, Organized By Hypothesized Factor Markers
| Student Sample |
Psychiatric Patient Sample |
||||||
|---|---|---|---|---|---|---|---|
| Scale (# of items) | Mean | SD | α | Mean | SD | α | Cohen's d |
| Affiliation | |||||||
| FI-FFM Sociability (9) | 33.19 | 6.5 | .83 | 25.50 | 7.8 | .83 | 1.07** |
| MPQ-BF Social Closeness (12) | 9.58 | 2.9 | .85 | 5.92 | 3.8 | .88 | 1.08** |
| NEO PI-R Gregariousness (8) | 29.08 | 5.3 | .77 | 21.69 | 6.0 | .78 | 1.31** |
| NEO PI-R Warmth (8) | 31.82 | 4.8 | .83 | 28.09 | 5.8 | .81 | .70** |
| SNAP Detachment (18) | 4.22 | 3.8 | .85 | 8.71 | 4.9 | .88 | 1.02** |
| Positive Affectivity | |||||||
| BAS Reward Responsive (5) | 17.56 | 2.2 | .72 | 16.20 | 2.9 | .80 | .53** |
| FI-FFM Positive Temp. (8) | 29.05 | 6.2 | .90 | 21.91 | 7.4 | .87 | 1.05** |
| MPQ-BF Wellbeing (14) | 10.39 | 3.7 | .87 | 6.67 | 4.7 | .91 | .88** |
| NEO PI-R Positive Emot. (8) | 30.09 | 5.0 | .75 | 24.92 | 6.4 | .78 | .90** |
| PANAS-X Joviality (8) | 27.04 | 6.6 | .94 | 20.57 | 7.3 | .94 | .93** |
| SNAP Positive Affectivity (11) | 7.39 | 2.5 | .81 | 5.26 | 3.5 | .86 | .70** |
| Energy | |||||||
| IPIP Activity (10) | 6.82 | 2.7 | .81 | 4.58 | 3.2 | .85 | .76** |
| NEO PI-R Activity (8) | 25.43 | 4.0 | .61 | 21.19 | 5.1 | .68 | .93** |
| PANAS-X Attentiveness (4) | 12.66 | 2.8 | .75 | 12.26 | 2.3 | .80 | .16 |
| SNAP Energy (12) | 7.45 | 2.9 | .76 | 5.57 | 3.5 | .85 | .58** |
| Ascendance | |||||||
| BAS Drive (4) | 11.56 | 2.5 | .76 | 9.97 | 3.0 | .81 | .58** |
| FI-FFM Ascendance (8) | 26.12 | 6.5 | .85 | 20.75 | 7.4 | .85 | .77** |
| FI-FFM Frankness (8) | 26.13 | 6.2 | .83 | 26.24 | 7.3 | .84 | .02 |
| MPQ-BF Social Potency (14) | 7.79 | 3.5 | .80 | 4.93 | 3.7 | .84 | .79** |
| NEO PI-R Assertiveness (8) | 24.57 | 5.2 | .79 | 21.63 | 6.1 | .82 | .52** |
| PANAS-X Self-Assurance (6) | 17.64 | 4.3 | .80 | 15.61 | 5.2 | .85 | .43** |
| SNAP Exhibitionism (16) | 9.32 | 4.0 | .83 | 5.14 | 4.1 | .87 | 1.03** |
| Venturesomeness | |||||||
| BAS Fun Seeking (4) | 12.99 | 2.3 | .75 | 10.78 | 2.6 | .68 | .90** |
| FI-FFM Venturesomeness (8) | 30.33 | 6.1 | .86 | 22.04 | 7.0 | .82 | 1.26** |
| NEO PI-R Excitement (8) | 30.40 | 4.7 | .63 | 22.45 | 5.8 | .65 | 1.51** |
| Neuroticism/ Negative Emotionality | |||||||
| BFI Neuroticism (8) | 22.44 | 6.0 | .80 | 28.42 | 6.4 | .81 | .96** |
| PANAS-X NA (10) | 20.16 | 6.6 | .87 | 25.74 | 8.7 | .89 | .72** |
| Depression | |||||||
| Beck Depression Inventory (21) | 9.83 | 9.27 | .93 | 19.33 | 12.36 | .93 | .87** |
| IDAS General Depression (20) | 43.69 | 11.75 | .88 | 52.54 | 15.19 | .91 | .65** |
| Social Anxiety | |||||||
| IDAS Social Anxiety (5) | 9.57 | 3.81 | .79 | 11.27 | 5.08 | .85 | .38** |
| PSRS Social Fear (11) | 27.25 | 6.54 | .85 | 29.37 | 7.45 | .86 | .30** |
| SIAS (19) | 22.41 | 13.18 | .90 | 32.03 | 15.72 | .93 | .66** |
| Social Phobia Scale (20) | 17.78 | 13.43 | .93 | 22.38 | 16.72 | .94 | .30** |
Note. N = 350 students, 204 psychiatric patients. The number of items in each scale is shown in parentheses. For each measure, sample means that are significantly higher are shown in boldface. BFI = Big Five Inventory; BAS = Behavioral Activation System Scales; IDAS = Inventory of Depression and Anxiety Symptoms; IPIP = International Personality Item Pool; MPQ-BF = Multidimensional Personality Questionnaire- Brief Form; NA = Negative Affect; NEO PI-R = Revised NEO Personality Inventory; PANAS-X = Expanded Form of the Positive and Negative Affect Schedule; PSRS= Phobic Stimuli and Response Scales; SIAS = Social Interaction and Anxiety Scale; SNAP = Schedule for Nonadaptive and Adaptive Personality.
difference between sample means significant at p < .01, two-tailed.
Overview of Measures
Based on correlational evidence and an analysis of item content, the assessment battery was “pre-structured” such that the five hypothesized components of E/PE each had at least three potential markers, giving each facet the opportunity to form a distinct factor in subsequent structural analyses (see Table 1 for the hypothesized markers for each facet). The hypothesized depression factor had only two markers; three or more markers per factor are generally preferred. Therefore, the Beck Depression Inventory-II items (BDI-II; Beck, Steer, & Brown, 1996) were parceled into two unit-weighted subscales (α's =. 86 to .89) in order to improve model identification. Numerous studies have reported a two-factor structure for the BDI-II; these factors are centered around the cognitive items and somatic items, with the affective items joining either factor (Vanheule, Desmet, Groenvynck, Rosseel, & Fontaine, 2008). In a comparative analysis of BDI-II factor solutions, Vanheule and colleagues (2008) concluded that Beck et al.'s (1996) two-factor structure (consisting of somatic/affective and cognitive factors) is most suitable for assessing the dimensions of the BDI-II. Therefore, the subscales in the current study were based on this solution. Because N/NE and internalizing are closely related, two measures of N/NE were included in the battery (see Table 1) to help identify the higher-order internalizing factor in structural analyses.
Symptom Measures
Beck Depression Inventory – Second Edition (BDI-II; Beck et al., 1996)
The BDI-II assesses depressive symptoms within the past two weeks. Each item has four statements that range from an absence to a severe manifestation of the symptom. This widely used measure has been shown to have good internal consistency and adequate retest reliability in a variety of populations (Beck et al., 1996).
Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007)
The IDAS is a factor analytically derived, multidimensional inventory that uses a 5-point Likert scale to assess symptoms over the past two weeks. The IDAS has strong internal consistency reliability, with median coefficient alphas greater than .80 (Watson et al., 2007). The IDAS has shown good convergent and discriminant validity with diagnoses and self-report measures, as well as good short-term retest reliability in a psychiatric patient sample (Watson et al., 2007; Watson et al., 2008).
Phobic Stimuli Response Scales (PSRS; Cutshall & Watson, 2004)
The PSRS Social Fear Scale assesses fear of social situations on a 4-point Likert scale. The scale has strong internal consistency (α = .88; Cutshall & Watson, 2004). It also shows good convergent validity with other measures of social anxiety and substantial criterion validity in relation to diagnoses of social phobia (Watson, 2008).
Social Interaction Anxiety Scale (SIAS) and Social Phobia Scale (SPS) (Mattick & Clarke, 1998)
This set of companion scales measures the fear of interaction with others and the fear of being observed while doing routine activities, respectively. Statements are rated on a 5-point Likert scale. The measures show good convergent validity with other measures of social anxiety, and discriminant validity with other anxiety disorders. They also demonstrate good internal consistency in various populations and strong retest reliability across a four-week interval (Mattick & Clarke, 1998).
Trait Measures
Behavioral Inhibition System/Behavioral Activation System Scales (BIS/BAS Scales; Carver & White, 1994)
The BIS/BAS Scales were designed to measure the behavioral inhibition system and behavioral activation system. The BAS scales are used in the current study as measures of E/PE, and they demonstrate good convergent validity with measures of trait affectivity. The respondent rates each item on a 4-point Likert scale. The BIS/BAS scales show acceptable internal consistency and retest reliability (r = .65 eight weeks after the initial test; Carver & White, 1994).
Big Five Inventory (BFI; John & Srivastava, 1999)
The BFI consists of 44 short phrases that are rated on a 5-point Likert scale and that correspond to one of the “Big Five” traits; only the Neuroticism scale was used in this study. The Neuroticism scale has good internal consistency and strong convergent validity with other measures of the Big Five. In addition, the BFI has demonstrated good retest reliability, with r = .85 after a three-month interval (John & Srivastava, 1999).
Faceted Inventory of the Five Factor Model (FI-FFM; Simms et al., 2001)
The FI-FFM is a factor analytically derived measure designed to assess lower-order personality traits within the framework of the Five Factor Model. This study included the five Extraversion facets. The items are rated using a 5-point Likert format. The FI-FFM Extraversion facets show good internal consistency (mean α = .79, ranging from .77 to .82) and expected patterns of discriminant and convergent validity with the BFI and other Five Factor measures of personality. The Extraversion facets have a mean two week test-retest correlation of .74 (Simms et al., 2001).
International Personality Item Pool (IPIP) Activity Level (Goldberg, 2005)
The IPIP Activity Level scale uses a true/false format and is modeled after the Energy Level scale from the Jackson Personality Inventory- Revised (Jackson, 1994). The IPIP scale demonstrates good internal consistency (α = .81; Goldberg, 2005).
Multidimensional Personality Questionnaire-Brief Form (MPQ-BF; Patrick, Curtin, & Tellegen, 2002)
The MPQ-BF is a factor analytically developed personality inventory that uses a true/false format. Three of the scales that define the higher-order Positive Emotionality factor were selected for this study. The MPQ-BF scales used in this study demonstrate good internal consistency and also show strong convergent-discriminant validity patterns with other personality measures (Patrick et al., 2002).
Positive and Negative Affect Schedule- Expanded Form (PANAS-X; Watson & Clark, 1999)
The PANAS-X is a self-report measure of specific types of affect, where each mood term is rated on a 5-point intensity scale. The trait version of three positive affect scales and the general negative affect scale were used in this study. The PA subscales and NA scale have shown strong internal consistency in diverse samples. The PANAS-X also has demonstrated good convergent and discriminant validity with other measures of affectivity, and adequate retest reliability after two months (r = .59; Watson & Clark, 1999).
Schedule for Nonadaptive and Adaptive Personality (SNAP; Clark, 1993)
The SNAP was designed to assess personality pathology; this assessment battery included the four scales related to positive temperament. Each item is answered using a true-false format. The SNAP scales for this study have shown good convergent validity with other inventories of personality pathology and strong internal consistency in student and patient samples (Clark, 1993).
Revised NEO Personality Inventory (NEO PI-R; Costa & McCrae, 1992)
The NEO PI-R measures personality domains and facets in the Five Factor model; respondents rate themselves using a 5-point Likert scale. This study included the six Extraversion facets. Overall, the NEO PI-R scales have good long-term retest reliability (r = .68-.83 after six years) and internal consistency, as well as good convergent and discriminant validity with other personality measures (Costa & McCrae, 1992).
Procedure
The students completed the measures in groups of 10 to 20 people, and they received research credit hours for their participation. The majority of the psychiatric patients completed the measures in one session (N = 121, 59.3%), whereas the rest of the patients completed the measures over the course of two sessions. This latter group of participants had already completed the PANAS-X and BFI in a related study within the previous two weeks. They filled out the remainder of the measures in a second session (M length between sessions = 8.1 days, SD = 3.4). The psychiatric patients completed the measures in small groups and were compensated for their participation.
Results
Preliminary Analyses
Table 1 presents descriptive statistics, coefficients alpha, and comparisons of mean scores across the two samples for each scale. As expected, independent t-tests revealed that the psychiatric patients reported more severe symptoms than students on all depression and social anxiety measures (p < .01, two-tailed), with Cohen's d ranging from .30 to .87. Please refer to Tables A and B in the online supplemental materials for zero-order correlations among the variables.
The Structure of E/PE
Factor analyses of the trait scales
To examine the structure of E/PE, the 25 trait scales were subjected to a separate principal factor analysis in each sample. Parallel analysis and the minimum average partial test (MAP) were used to determine the optimal number of factors to extract. These methods are more objective than the examination of scree plots, and they tend to yield convergent solutions (O'Connor, 2000). In parallel analysis, the observed eigenvalues are compared with the eigenvalues of random sets of data that contain the same numbers of variables and observations, while the MAP test is based on the examination of residual correlation matrices.
Both parallel analysis and the MAP test indicated that four factors should be extracted from the student and psychiatric patient data (see Table 2). Because we expected the facets of E/PE to be moderately related, the factors were rotated using an oblique promax rotation that produced four clearly interpretable factors. The factor loadings are reported in Tables 3 and 4 for students and psychiatric patients, respectively. In both samples, the first and second factors may be labeled “Sociability” and “Positive Emotionality.” Sociability consists of warmth, gregariousness, and enjoying social interactions, while Positive Emotionality consists of the positive affectivity and energy markers. The third factor appears to be Ascendance (marked by assertiveness and dominance), and we have labeled the fourth factor Fun-Seeking. Fun-Seeking consists largely of the BAS scales, but also has primary loadings from the FI-FFM Venturesomeness and NEO PI-R Excitement Seeking scales. The E/PE facets were moderately correlated with one another in both samples (mean r = .53 for students and .48 for psychiatric patients). Thus, the resulting factors largely conformed to our expectations, except that the markers of positive affectivity and energy combined to form a single Positive Emotionality factor.
Table 2.
Results of Parallel Analysis and MAP for the Principal Factor Analyses of E/PE Scales in Each Sample (first eight factors shown)
| Students |
Psychiatric Patients |
|||||
|---|---|---|---|---|---|---|
| Factor | Actual EV | Sim. EV | Ave. partial r2 | Actual EV | Sim. EV | Ave. partial r2 |
| 1 | 10.80 | 1.52 | .041 | 11.00 | 1.70 | .052 |
| 2 | 2.46 | 1.44 | .035 | 2.59 | 1.59 | .038 |
| 3 | 1.99 | 1.38 | .026 | 2.02 | 1.50 | .034 |
| 4 | 1.44 | 1.33 | .024 | 1.64 | 1.43 | .025 |
| 5 | .98 | 1.28 | .025 | 1.04 | 1.36 | .026 |
| 6 | .84 | 1.23 | .026 | .95 | 1.30 | .026 |
| 7 | .73 | 1.19 | .027 | .70 | 1.25 | .027 |
| 8 | .71 | 1.15 | .031 | .59 | 1.19 | .031 |
Note. N = 350 students, 204 psychiatric patients. E/PE = Extraversion/Positive Emotionality; EV = eigenvalue; Sim. EV = mean of 1000 eigenvalues from simulated datasets. For ave. (average) partial r2, variance shared with preceding factors was removed.
Over-extraction is indicated by a larger simulated than actual eigenvalue (parallel analysis) or an increase in the average partial r2 (MAP). The solution suggested by both analyses is shown in boldface.
Table 3.
Promax-Rotated Factor Loadings of the E/PE Scales in Student Sample
| Factor Loading |
||||
|---|---|---|---|---|
| Scale | 1 | 2 | 3 | 4 |
| PANAS-X Attentiveness | .82 | −.11 | −.06 | −.06 |
| PANAS-X Joviality | .77 | .12 | −.18 | .13 |
| SNAP Energy | .70 | −.07 | .19 | −.02 |
| IPIP Activity | .67 | .01 | .02 | −.18 |
| MPQ-BF Wellbeing | .66 | .20 | −.07 | .04 |
| NEO PI-R Activity | .59 | .05 | .14 | −.03 |
| SNAP Positive Affectivity | .54 | .21 | .15 | .09 |
| PANAS-X Self- Assurance | .52 | −.13 | .27 | .17 |
| NEO PI-R Positive Emotions | .50 | .32 | −.16 | .17 |
| FI-FFM Positive Temperament | .50 | .24 | .10 | .18 |
| MPQ-BF Social Closeness | .06 | .92 | −.05 | −.16 |
| SNAP Detachment (−) | .08 | .87 | .08 | −.14 |
| FI-FFM Sociability | .01 | .86 | .06 | −.05 |
| NEO PI-R Gregariousness | −.09 | .78 | .05 | .12 |
| NEO PI-R Warmth | .28 | .59 | −.05 | .10 |
| FI-FFM Ascendance | .02 | −.03 | .86 | .03 |
| MPQ-BF Social Potency | .01 | .01 | .80 | .02 |
| NEO PI-R Assertiveness | .19 | .01 | .78 | −.11 |
| FI-FFM Frankness | −.11 | .07 | .67 | .04 |
| SNAP Exhibitionism | −.07 | .30 | .52 | .11 |
| BAS Fun-Seeking | −.07 | .01 | .01 | .78 |
| BAS Reward Responsiveness | .05 | .03 | −.08 | .73 |
| BAS Drive | .11 | −.25 | .19 | .64 |
| FI-FFM Venturesomeness | −.10 | .46 | .15 | .48 |
| NEO PI-R Excitement Seeking | −.10 | .40 | .02 | .47 |
Note. N = 350 students. Loadings ≥ |.40| are shown in boldface. MPQ-BF = Multidimensional Personality Questionnaire- Brief Form; SNAP = Schedule for Nonadpative and Adaptive Personality; FI-FFM = Faceted Inventory- Five Factor Model; NEO PI-R = Revised NEO Personality Inventory; IPIP = International Pool of Personality Items; BAS = Behavioral Activation System Scales.
Table 4.
Promax-Rotated Factor Loadings of the E/PE Scales in Psychiatric Patient Sample
| Factor Loading |
||||
|---|---|---|---|---|
| Scale | 1 | 2 | 3 | 4 |
| MPQ-BF Social Closeness | .97 | −.04 | −.02 | −.09 |
| SNAP Detachment (−) | .94 | .05 | .04 | −.07 |
| FI-FFM Sociability | .90 | −.13 | .09 | −.02 |
| NEO PI-R Gregariousness | .89 | −.11 | .04 | .00 |
| NEO PI-R Warmth | .75 | .15 | −.01 | −.07 |
| NEO PI-R Positive Emotions | .45 | .32 | −.08 | .26 |
| SNAP Energy | −.15 | .85 | .15 | −.15 |
| IPIP Activity | −.03 | .76 | .15 | −.22 |
| FI-FFM Positive Temperament | .21 | .71 | −.06 | .16 |
| MPQ-BF Wellbeing | .32 | .69 | −.14 | .08 |
| PANAS-X Attentiveness | −.08 | .67 | −.04 | .11 |
| PANAS-X Joviality | .22 | .65 | −.13 | .21 |
| SNAP Positive Affectivity | .31 | .57 | .09 | .04 |
| NEO PI-R Activity | −.10 | .56 | .27 | −.05 |
| PANAS-X Self- Assurance | −.05 | .51 | −.27 | .18 |
| MPQ-BF Social Potency | .00 | .09 | .80 | .06 |
| FI-FFM Ascendance | .14 | .05 | .74 | .05 |
| NEO PI-R Assertiveness | .00 | .24 | .73 | −.13 |
| FI-FFM Frankness | −.05 | −.08 | .58 | .27 |
| SNAP Exhibitionism | .32 | .09 | .50 | .09 |
| BAS Fun-Seeking | −.03 | −.10 | .05 | .85 |
| BAS Reward Responsiveness | −.05 | .15 | −.11 | .67 |
| BAS Drive | −.30 | .21 | .12 | .57 |
| FI-FFM Venturesomeness | .27 | .01 | .20 | .57 |
| NEO PI-R Excitement Seeking | .16 | −.22 | .17 | .53 |
Note. N = 204 psychiatric patients. Loadings ≥ |.40| are shown in boldface. MPQ-BF = Multidimensional Personality Questionnaire- Brief Form; SNAP = Schedule for Nonadpative and Adaptive Personality; FI-FFM = Faceted Inventory- Five Factor Model; NEO PI-R = Revised NEO Personality Inventory; IPIP = International Pool of Personality Items; BAS = Behavioral Activation System Scales.
Analyses of factor similarity
Congruence coefficients, which index the similarity of factor loading matrices, were computed to provide a quantitative comparison of the factor structure of E/PE in the student and psychiatric patient samples. The convergent coefficients ranged from .93 to .97, whereas the discriminant coefficients ranged from only .00 to .17 (mean = .09). Given that congruence coefficients greater than .90 signify equivalent structures, these results establish that the E/PE factor structures were highly similar across samples.
Symptom Structure
A two-factor structure was hypothesized for the symptom measures, consisting of depression and social anxiety; however, an alternative possibility is that a one-factor model (i.e., internalizing) is a better fit to the data. Therefore, the symptom measures (including the two BDI-II subscales described previously) were subjected to separate confirmatory factor analyses (CFA) in each sample, comparing one- and two-factor structures. Because the distributions were highly skewed, a maximum likelihood mean and variance-adjusted (MLMV) chi-square was used in order to provide more accurate standard errors and fit statistics in this and subsequent structural analyses.
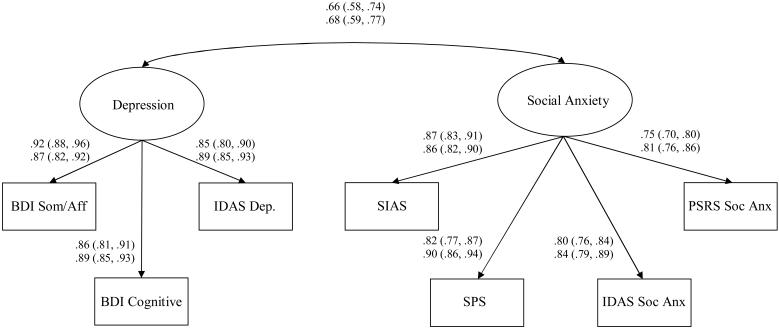
Table 5 shows the fit indices for the one- and two-factor models in each sample. Smaller values for the root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR) indicate better model fit. Similarly, smaller values of Akaike's information criterion (AIC) and Draper's information criterion (DIC)— both of which reward parsimony— indicate better relative fit for a given model. DIC is similar to the Bayesian information criterion, but corrects for sample size more accurately (e.g., Draper, 1995). Nested χ2 difference tests are also reported; a significant value indicates that the simpler model (i.e., internalizing) fits more poorly than the more complex model (i.e., depression and social anxiety). As shown in Table 5, the two-factor model consistently demonstrates better fit than the one-factor model in both samples;2 as expected, the Depression and Social Anxiety factors are strongly correlated (mean r = .67). Standardized arameter estimates and confidence intervals for the two-factor model are shown in Figure 1.
Table 5.
Comparisons of Fit Indices for One Versus Two Factor Models of Symptom Structure
| Sample | Model | RMSEA | SRMR | AIC | DIC | χ2 (1) | p |
|---|---|---|---|---|---|---|---|
| Students | Internalizing | .261 | .093 | 15528 | 15570 | 243.20 | <.001 |
| Depression and Social Anx. | .116 | .046 | 15200 | 15244 | |||
| Psychiatric Patients |
Internalizing | .286 | .102 | 9682 | 9713 | 202.19 | <.001 |
| Depression and Social Anx. | .105 | .036 | 9449 | 9482 | |||
Note. N = 350 students, 204 psychiatric patients. Anx. = anxiety; RMSEA = Root mean square error of approximation; SRMR = Standardized root mean square residual; AIC = Akaike's information criterion; DIC = Draper's information criterion.
Figure 1.
Standardized parameter estimates are shown with 95% confidence intervals in parentheses; estimates for the student sample (N = 350) are shown on top and estimates for the psychiatric patient sample (N = 204) are shown below. BDI = Beck Depression Inventory; Som/Aff = Somatic/Affective scale; IDAS = Inventory of Depression and Anxiety Symptoms; Dep. = General Depression; SIAS = Social Interaction Anxiety Scale; SPS = Social Phobia Scale; Soc Anx = Social Anxiety; PSRS = Phobic Stimuli and Response Scales.
Relations between Traits and Symptoms
Correlational analyses
Table 6 displays correlations between the trait and symptom factors, using regression-based factor scores. The Williams modification of the Hotelling test for two correlations involving a common variable (Kenny, 1987) was used to compare the relative strength of the correlations within and across each symptom type. Correlations with the E/PE facets varied widely (r = −.20 to −.61), showing the importance of examining facet-level relations. Table 6 indicates that Positive Emotionality generally had the strongest relation with Depression among the E/PE facets (r= −.56 and −.51 in the students and psychiatric patients, respectively). Sociability also had relatively strong links to Depression, with correlations of −.42 and −.50 in the students and psychiatric patients, respectively. The data for social anxiety reveal a somewhat different pattern. Similar to depression, Sociability and Positive Emotionality both had relatively strong links to Social Anxiety, with correlations ranging from −.43 to −.61 across the two samples. In contrast to the depression data, however, Ascendance was strongly correlated with Social Anxiety (r = −.50 and −.54 in the students and psychiatric patients, respectively); these correlations were significantly stronger than the Depression-Ascendance correlations. Finally, Fun-Seeking generally was weakly related to both symptoms.
Table 6.
Correlations of Trait Factor Scores with Symptom Factor Scores
| Students |
Psychiatric Patients |
|||
|---|---|---|---|---|
| Depression | Social Anxiety | Depression | Social Anxiety | |
| Sociability | −.42b | −.61a | −.50a | −.56a |
| Positive Emotionality | −.56a | −.55ab | −.51a | −.43b |
| Ascendance | −.20c | −.50b | −.21b | −.54ab |
| Fun-Seeking | −.24c | .41c | −.29b | −.23c |
Note. N = 350 students, 204 psychiatric patients. Correlations ≥ |.40| are shown in boldface. Within each column, correlations not sharing the same superscript differ from one another (p < .05, two-tailed). Within each sample and each row, significantly stronger correlations are underlined (p < .05, two-tailed). All correlations are significant at p < .01.
Structural models in the separate samples
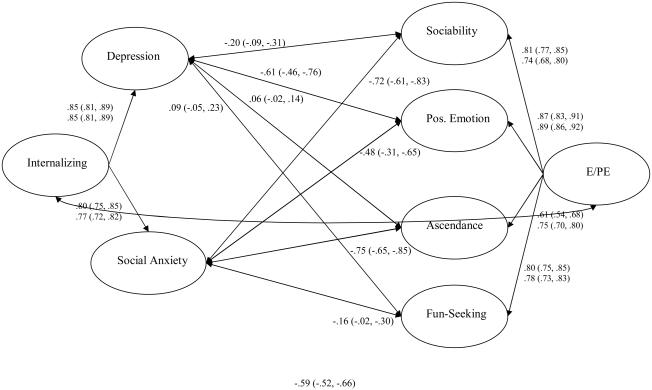
Given the moderate to strong correlations among the E/PE facets and between the symptoms, structural equation modeling (SEM) was used to control for shared variance and examine the unique variance of each construct. Indicators for each construct were assigned based on the primary loadings in the E/PE analyses and the two-factor symptom analyses. First, two competing models were compared to determine whether the facets of E/PE account for variance beyond higher-order E/PE in relation to depression and social anxiety. In the first model, paths were freed from Depression and Social Anxiety to the higher-order E/PE trait. In contrast, the second model allowed paths from each of the four E/PE facets to Depression and Social Anxiety (see Figure 2 for the structural model). Thus, this second model includes the unique relations of the E/PE facets with Depression and with Social Anxiety, even after accounting for Internalizing and higher-order E/PE. In both models, higher-order E/PE and Internalizing (marked by Depression and Social Anxiety, as well as PANAS-X NA and BFI Neuroticism) were allowed to covary.
Figure 2.
Standardized parameter estimates are shown with 95% confidence intervals in parentheses, using multiple group analysis (N = 554). For loadings on Internalizing and E/PE, student estimates are shown on top and psychiatric patient estimates are shown below; correlations among latent variables have been constrained to be equal across the two samples. E/PE = Extraversion/Positive Emotionality; Pos Emotion = Positive Emotionality.
Fit indices indicated that the model that frees paths from the E/PE facets to Depression and Social Anxiety provides superior fit to the data in both samples (Table 7). Thus, examining facet-level E/PE relations with depression and social anxiety adds information beyond that obtained from the higher-order relations. To compare whether individual facets are more strongly correlated with either depression or social anxiety, models were examined in which the estimated correlation with each E/PE facet was constrained to be equal across depression and social anxiety (see Table 7). If the constrained model shows a poorer fit (i.e., significant nested χ2 difference test, higher AIC and DIC values) as compared to the unconstrained facet-level model, we may infer that the path estimates differ. In both samples, Ascendance was more highly related to Social Anxiety than to Depression. Sociability and Fun-Seeking were more highly related to Social Anxiety in the students only, although there was a trend towards differential relations of Sociability in the patients as well. (The standardized path estimates for the lower-order E/PE models may be found in Table C of the online supplement).
Table 7.
Comparisons of Fit Indices for Models of Depression, Social Anxiety, and E/PE
| Sample | Model | RMSEA | SRMR | AIC | DIC | χ2 (1) | p |
|---|---|---|---|---|---|---|---|
| Students | Higher-order E/PE | .092 | .080 | 63451.48 | 63675.71 | -- | |
| Lower-order E/PE | .090 | .074 | 63360.89 | 63597.24 | -- | ||
| Constrained Models | |||||||
| Sociability paths* | .091 | .080 | 63394.55 | 63628.87 | 35.7 | <.01 | |
| PE paths | .090 | .074 | 63359.31 | 63593.64 | 0.33 | .565 | |
| Ascendance paths* | .092 | .082 | 63426.32 | 63660.65 | 61.9 | <.01 | |
| Fun-Seeking paths* | .091 | .077 | 63376.08 | 63610.41 | 16.0 | <.01 | |
| Psychiatric Patients | Higher-order E/PE | .098 | .091 | 39146.52 | 39310.83 | -- | |
| Lower-order E/PE | .094 | .083 | 39062.74 | 39235.92 | -- | ||
| Constrained Models | |||||||
| Sociability paths | .094 | .085 | 39065.69 | 39237.40 | 3.65 | .056 | |
| PE paths | .094 | .085 | 39063.82 | 39235.53 | 3.70 | .055 | |
| Ascendance paths* | .096 | .098 | 39094.26 | 39265.99 | 32.8 | <.01 | |
| Fun-Seeking paths | .094 | .083 | 39061.26 | 39232.99 | 0.46 | .497 | |
| Combined | Higher-order E/PE | .095 | .086 | 102599.20 | 103142.16 | -- | |
| Lower-order E/PE | .092 | .080 | 102423.32 | 102981.16 | -- | ||
| Constrained Models | |||||||
| Sociability paths* | .092 | .083 | 102453.55 | 103008.91 | 25.9 | <.01 | |
| PE paths | .092 | .081 | 102422.42 | 102977.78 | 0.96 | .327 | |
| Ascendance paths* | .093 | .088 | 102525.48 | 103080.84 | 92.2 | <.01 | |
| Fun-Seeking paths* | .092 | .081 | 102427.13 | 102982.49 | 4.75 | .029 | |
Note. N = 350 students, 204 psychiatric patients. Higher-order E/PE = relations between symptoms and higher-order E/PE factor only (without any facets); Lower-order E/PE = relations between symptoms and each E/PE facet; PE = Positive Emotionality; RMSEA = Root mean square error of approximation; SRMR = Standardized root mean square residual; AIC = Akaike's information criterion; DIC = Draper's information criterion.
Models with facets constrained indicate that the correlations of the facet with Depression and with Social Anxiety were constrained to be equal. Combined models are multiple group analyses where all lower-order estimated correlations were constrained to be equal between student and psychiatric patient samples.
signifies a significant nested χ2 difference test, higher AIC, and higher DIC as compared to the (unconstrained) lower-order E/PE model for each sample. This indicates that the correlations of a given facet with Depression and with Social Anxiety are not equal.
Multiple group analyses
To allow for a fuller range of variance and increased power, as well as a test of similarity between samples, multiple group SEM analyses of the relations between E/PE and depression/social anxiety were performed. We first compared the fit of the higher-order E/PE and lower-order E/PE models in the combined sample; the path estimates were free to differ between students and psychiatric patients in these two initial models. Based on the fit indices shown in the bottom portion of Table 7, the lower-order model was a better fit to the multiple group data than was a model only allowing paths from the higher-order E/PE factor.
Next, two competing lower-order E/PE models were tested: 1) all lower-order correlations were free to differ between the samples, versus 2) all lower-order correlations were constrained to be equal across samples (see Figure 2). Other model parameters were freed as much as possible within the limits of model identification. The χ2 difference test indicated that the constrained model did not result in a significant decrement in fit (χ2 (9) = 16.18, ns). Likewise, the AIC and DIC of the constrained model were both better than the unconstrained model (for AIC, unconstrained model = 102,423.624 and constrained model = 102,423.324; for DIC, unconstrained model = 103,003.777 and constrained model = 102,981.164). Thus, given that the constrained model provides an equivalent or superior fit to the data, we may surmise that the structural relations between the symptoms and facets of E/PE are similar across the two samples. Therefore, constrained models (in which the student and psychiatric patient correlations were forced to be equal) were tested in all subsequent analyses.
Constraining Positive Emotionality to have equal path estimates with Depression and with Social Anxiety yielded a slightly better fit than the unconstrained lower-order model, indicating that Positive Emotionality is equally related to these symptoms in the combined sample. However, Sociability, Ascendance, and Fun Seeking all have a stronger negative relation with Social Anxiety than with Depression (see Table 7). Thus, in the combined sample, the facets of E/PE differ in the strength of their relations to depression and social anxiety, even after controlling for symptom comorbidity and the shared variance among the E/PE facets.
The standardized path estimates of the multiple group data may also be examined by focusing on the relative strength of E/PE facets within each symptom type (see Figure 2). Depression shows a specific and strong association with low Positive Emotionality (r = −.61), accounting for most of the association between Depression and E/PE. Sociability is the only other facet that exhibits a significant correlation with Depression, with a more modest coefficient of −.20. In contrast, Social Anxiety is more broadly related to all four facets of E/PE. Social Anxiety exhibits strong negative associations with Sociability (r = −.72) and Ascendance (r = −.75), as well as a moderate negative correlation with Positive Emotionality (r = −.48). Finally, low Fun-Seeking is also significantly (albeit weakly) related to Social Anxiety (r = −.16).
Discussion
This is the first study to model relations between symptoms of depression, social anxiety, and E/PE facets while controlling for the considerable shared variance among these constructs. These results provide support for the hypothesis that facets of E/PE show differential relations (in terms of both magnitude and overall patterns) with depression and with social anxiety, even after accounting for the higher-order constructs. Further, the multiple group analyses suggest that these relations are robust and generalizable across populations with varying levels of symptoms.
Structure of Extraversion and Positive Emotionality
This study identified a replicable structure for E/PE, consisting of sociability, positive emotionality, ascendance, and fun-seeking facets.3 Three of the E/PE facets correspond closely to Watson and Clark's (1997) model: both have ascendance facets, our sociability is equivalent to their affiliation, and our fun-seeking is very similar to their venturesomenss. The only notable difference is that Watson and Clark hypothesized separate facets of positive affectivity and energy; these markers combined to form the single Positive Emotionality factor in the current study. Although positive affect and energy are theoretically separable, they may not be empirically distinct when considered in the context of other closely-related facets of E/PE.
Differential Trait Correlates of Depression and Social Anxiety
Overall patterns
Analyses showed that the unique variance of social anxiety is significantly related to all four facets of E/PE: it has its strongest associations with sociability and ascendance, with more moderate links to positive emotionality and a weak correlation with fun-seeking. In contrast, depressive symptoms have a strong relation only with positive emotionality, as well as a weak correlation with sociability. These results are consistent with the limited previous evidence indicating that social anxiety was more broadly related to facets of E/PE than was depression (see Bienvenu et al., 2004), but this is the first study to find this pattern while controlling for symptom comorbidity.4
Although depression and social anxiety symptoms showed different patterns of relations with E/PE facets, it is noteworthy that no facets were uniquely related to depression. Future research could focus on locating a unique personality correlate of depression that distinguishes it from social anxiety. Based on previous research, potential candidates might include low scores on indicators of Conscientiousness (e.g., Chioqueta & Stiles, 2005; Costa et al., 2005) or on the NEO PI-R “Openness to Actions” facet (defined as a tendency to prefer novel experiences; e.g., Chioqueta & Stiles, 2005). Alternatively, it may be that depression (and GAD) is distinguished from social anxiety and other anxiety disorders by its very strong link to N/NE (see Watson et al., 2005).
Positive emotionality and social anxiety
The current study found that the association between E/PE and social anxiety symptoms is broad and is not simply an artifact of low sociability. In particular, low PE is as strongly related to the unique variance of social anxiety as it is to the unique variance of depression. This finding is consistent with a growing body of literature on positive emotionality deficits in social anxiety (e.g., Brown et al., 1998; Kashdan & Steger, 2006; Sellbom et al., 2008; Watson et al., 2005). The results of the current study suggest that social anxiety is associated with a positive emotionality deficit, independent of depressive symptoms; future research is needed to identify the sources of this deficit.
Assessment and treatment implications
This study has several implications for the assessment and treatment of depression and social anxiety. For patients with depression, these findings demonstrate the specific importance of assessing PE (as opposed to higher-order E/PE— a distinction that is sometimes ignored) and of boosting PE levels in treatment. For instance, behavioral activation is an empirically-supported treatment for depression that specifically targets anhedonia (see Dimidjian, Martell, Addis, & Herman-Dunn, 2008), and it may be particularly helpful for individuals with markedly low PE. Fredrickson's broaden-and-build theory— which states that positive emotions help broaden our thought-action repertoire and build lasting resources for coping with difficulties— provides another framework for increasing PE, with recommended therapeutic techniques such as relaxation, meditation, and “finding positive meaning” (Fredrickson, 2000). Lastly, although low PE is most salient to depression, these results show that sociability should also be assessed to determine whether interpersonal functioning should be a focus of treatment.
The current study suggests that, in contrast to depression, it is important to assess all facets of E/PE in cases of social anxiety to determine particular problem areas for an individual. Commonly-used treatments, such as cognitive-behavioral group therapy (Heimberg & Becker, 2002) include interventions for low ascendance/assertiveness and low sociability. However, low PE (and low fun-seeking) is not typically addressed in the treatment of social anxiety. For those with low PE, the techniques outlined above for raising PE may prove to be useful supplements to treatment; future research could examine the incremental contribution of such techniques beyond current treatments for social anxiety.
Strengths and Limitations
Strengths of the study include comprehensive, diverse measures that thoroughly assess the latent constructs, replication across two samples with different mean psychopathology levels, and multivariate analyses that examined the shared and unique variance for each construct. However, there are several limitations that apply to this study. First, it was cross-sectional in nature; a longitudinal design is necessary to establish causal relations among personality traits and symptoms. Second, all information was collected via self-report, rather than with interviews, informant ratings, or behavioral observation. Because state effects of depression and anxiety could influence self-report ratings of personality, the magnitude of correlations likely were somewhat inflated. This is a significant limitation that future research should address by collecting collateral interview or informant data. However, it is worth noting that we were primarily interested in the overall pattern of correlations, rather than their absolute magnitudes; theoretically, state effects should not alter the overall pattern of the results.
A related concern is that there may have been content overlap between the personality and psychopathology measures used in this study. For instance, measures of sociability and social anxiety may share item content, while measures of positive emotionality and depression also may have highly similar item content. Such criterion contamination would serve to artificially inflate correlations. It is probable that such overlap did contribute somewhat to the observed correlations, although several analyses indicated that the effect likely was not large.5
A final limitation is that this study only assessed symptoms and did not examine relations with formal diagnoses of major depression and social anxiety disorder. Therefore, additional research is needed to determine whether these conclusions would generalize to clinical diagnoses. It should be noted, however, that previous studies in this area generally have obtained similar results across symptom versus diagnostic variables; for example, low levels of PE show a significant, specific link to both symptoms (e.g., Sellbom et al., 2008; Watson et al., 1988, 2005) and diagnoses (e.g., Watson et al., 1988, 2008) of depression. Given that our results replicated across two independent samples with different psychopathology levels, we hypothesize that our findings may apply to populations with diagnoses of depression and social anxiety as well.
Future Directions
The results of this study have potentially important implications for etiological models of psychopathology, in that they help clarify the underlying general and specific components of two facets of internalizing. In this regard, behavioral genetics studies have shown evidence of both shared and specific genetic variance for the facets of E/PE (e.g., Benjamin et al., 1996; Eid, Riemann, Angleitner, & Borkenau, 2003). Genetic studies have not yet examined relations between E/PE facets and facets of internalizing; such work could improve our understanding of the underlying etiology and why these phenotypes are related.
This study also informs the broader literature on the structure of internalizing psychopathology. Researchers have pondered whether it is best to focus on the higher-order internalizing factor in structural models, rather than on specific disorders, given the large portion of shared variance (e.g., Krueger et al., 2001). The current study shows that there is additional systematic (and we would argue, interesting) variance shared between these two facets of internalizing and E/PE, beyond that accounted for by higher-order internalizing. A similar methodology could also be applied to other disorders that have a component of low E/PE, such as agoraphobia and schizophrenia spectrum disorders (Mineka et al., 1998; Watson et al., 2005).
In conclusion, the results of this study illustrate the value of a theory-driven, facet-based approach to the relations between personality and psychopathology, as it was only at the facet level that the differential correlates of depression and social anxiety fully emerged. We believe that this methodology offers exciting possibilities for explicating the nature of the links between personality and psychopathology. These findings delineating depression and social anxiety represent an initial contribution towards this larger goal.
Supplementary Material
Acknowledgments
This research was supported in part by NIMH Grant R01-MH068472 to David Watson. We thank Lee Anna Clark, Michael W. O'Hara and Jenny Gringer Richards for their help in the preparation of this manuscript.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/abn.
These constitute the final sample sizes, following the removal of 16 participants due to random responding (i.e., same response for nearly all items, consistent out-of-range responses) and/or omission of more than 40% of the items. For the participants in the final sample, item-level or scale-level multiple imputation was used to complete any missing data (item-level was used only if a given scale was more than 80% complete).
Although the SRMR values for the two-factor model are very good (<.05), the RMSEA values are somewhat high (e.g., Browne & Cudek, 1993, suggest that RMSEA should be less than .10). Given this borderline fit index, an anonymous reviewer suggested comparing the final model that relates depression and social anxiety to E/PE facets (see Figure 2) with a model relating internalizing to E/PE facets, to provide further evidence that a two-factor symptom model is superior to a one-factor model. All fit indices were better for the two-factor model.
It is noteworthy that these structural findings have relevance to the assessment of Axis II personality disorders, in that this replicable, comprehensive lower-order structure could serve as an organizing model for assessing the E/PE domain in dimensional models of personality pathology.
The current study provides an illustration of the importance of multivariate analyses that control for shared symptom variance: Sociability's moderate zero-order correlation with Depression (r = −.42 to −.50) dropped substantially after controlling for Social Anxiety in the SEM analyses (r = −.20). In this case, interpreting the zero-order correlation would be quite misleading.
To examine the extent to which criterion contamination affected correlations, two additional analyses were conducted. First, two revised BDI-II scales were created: 1) a scale removing the four items related to low PE (i.e., anhedonia and low energy) and 2) a scale consisting of only the PE items. The two scales had very similar correlations with the PE Factor (rs ranged from −.47 to −.56 across the two samples) that did not differ significantly from one another. Similarly, the relation between Sociability and the SPS— one of our strongest markers of social anxiety— was examined. The SPS, a measure of social performance anxiety, has no items directly related to social interactions, and therefore has little content overlap with Sociability. Correlations between the SPS and Sociability were still moderate in magnitude (r = −.50 and −.48). However, they were significantly weaker than correlations with the SIAS (r with Sociability = −.62 and −.59; p < .05), which assesses social interaction anxiety and has more shared content with Sociability.
References
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. 2nd ed. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Benjamin J, Li L, Patterson C, Greenberg BD, Murphy DL, Hamer DH. Population and familial association between the D4 dopamine receptor gene and measures of novelty seeking. Nature Genetics. 1996;12:81–84. doi: 10.1038/ng0196-81. [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Samuels JF, Costa PT, Reti IM, Eaton WW, Nestadt G. Anxiety and depressive disorders and the five-factor model of personality: A higher- and lower-order personality trait investigation in a community sample. Depression and Anxiety. 2004;20:92–97. doi: 10.1002/da.20026. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage Publications; Newbury Park: 1993. pp. 136–161. [Google Scholar]
- Carver CS, White TL. Behavioral Inhibition, Behavioral Activation, and Affective Responses to Impending Reward and Punishment: The BIS/BAS Scales. Journal of Personality and Social Psychology. 1994;67:319–333. [Google Scholar]
- Chioqueta AP, Stiles TC. Personality traits and the development of depression, hopelessness, and suicide ideation. Personality and Individual Differences. 2005;38:1283–1291. [Google Scholar]
- Clark LA. The Schedule for Nonadaptive and Adaptive Personality: Manual for administration and scoring. University of Minnesota Press; Minneapolis: 1993. [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Costa PT, Jr., Bagby RM, Herbst JH, McCrae RR. Personality self-reports are concurrently reliable and valid during acute depressive episodes. Journal of Affective Disorders. 2005;89:45–55. doi: 10.1016/j.jad.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr., McCrae RR. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources, Inc; Odessa, FL: 1992. [Google Scholar]
- Cutshall C, Watson D. The phobic stimuli response scales: A new self-report measure of fear. Behaviour Research and Therapy. 2004;42:1193–1201. doi: 10.1016/j.brat.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. Behavioral and Brain Sciences. 1999;22:491–569. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Martell CR, Addis ME, Herman-Dunn R. Behavioral activation for depression. In: Barlow DH, editor. Clinical Handbook of Psychological Disorders. 4th ed. Guilford Press; New York: 2008. pp. 328–364. [Google Scholar]
- Draper D. Assessment and propagation of model uncertainty. Journal of the Royal Statistical Society: Series B (Methodology) 1995;57:45–97. [Google Scholar]
- Eid M, Riemann R, Angleitner A, Borkenau P. Sociability and positive emotionality: Genetic and environmental contributions to the covariation between different facets of extraversion. Journal of Personality. 2003;71:319–346. doi: 10.1111/1467-6494.7103003. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P) Biometrics Research, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Fredrickson BL. Cultivating positive emotions to optimize to optimize health and well- being. Prevention & Treatment. 2000;3:1–25. [Google Scholar]
- Goldberg LR. International Personality Item Pool: A Scientific Collaboratory for the Development of Advanced Measures of Personality Traits and Other Individual Differences. 2005 Retrieved November 20, 2005, from http://ipip.ori.org/
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press; New York: 2002. [Google Scholar]
- Jackson DN. Jackson Personality Inventory-Revised manual. Sigma Assessment Systems; Port Huron, MI: 1994. [Google Scholar]
- John OP, Srivastava S. The big five trait taxonomy: History, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of personality: Theory and research. 2nd ed. Guilford Press; New York: 1999. pp. 102–138. [Google Scholar]
- Kashdan TB, Steger MF. Expanding the topography of social anxiety: An experience-sampling assessment of positive emotions, positive events, and emotion suppression. Psychological Science. 2006;17:120–128. doi: 10.1111/j.1467-9280.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- Kenny DA. Statistics for the social and behavioral sciences. Little, Brown and Company; Boston: 1987. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personality and Individual Differences. 2001;30:1245–1259. [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- O'Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer's MAP test. Behavior Research Methods, Instruments, & Computers. 2000;32:396–402. doi: 10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14(2):150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Sellbom M, Ben-Porath YS, Bagby RM. On the hierarchical structure of mood and anxiety disorders: Confirmatory evidence and elaboration of a model of temperament markers. Journal of Abnormal Psychology. 2008;117:576–590. doi: 10.1037/a0012536. [DOI] [PubMed] [Google Scholar]
- Simms EN, Wu KD, Watson D. Defining extraversion through facet structure; Poster presented at the 2nd Annual Meeting of the Society for Personality and Social Psychology; San Antonio, TX. Feb, 2001. [Google Scholar]
- Tackett JL, Quilty LC, Sellbom M, Rector N, Bagby RM. Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: The context of personality structure. Journal of Abnormal Psychology. 2008;117:812–825. doi: 10.1037/a0013795. [DOI] [PubMed] [Google Scholar]
- Vanheule S, Desmet M, Groenvynck H, Rosseel Y, Fontaine J. The factor structure of the Beck Depression Inventory II: An Evaluation. Assessment. 2008;15:177–187. doi: 10.1177/1073191107311261. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D. Further validation of the Phobic Stimuli Response Scales (PSRS) in an outpatient sample. 2008 Manuscript in preparation. [Google Scholar]
- Watson D, Clark LA. On traits and temperament: General and specific factors of emotional experience and their relation to the five-factor model. Journal of Personality. 1992;60:441–476. doi: 10.1111/j.1467-6494.1992.tb00980.x. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Extraversion and its positive emotional core. In: Hogan R, Johnson J, Briggs S, editors. Handbook of personality psychology. Academic Press; San Diego, CA: 1997. pp. 767–793. [Google Scholar]
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule- Expanded Form. University of Iowa; Iowa City, IA: 1999. Unpublished manuscript. [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology. 1988;97:346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Watson D, O'Hara MW, Chmielewski M, McDade-Montez EA, Koffel E, Naragon K, Stuart S. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment. 2008;20:248–259. doi: 10.1037/a0012570. [DOI] [PubMed] [Google Scholar]
- Watson D, O'Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Gamez W, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.