Abstract
Poor lifestyle habits, such as unhealthy eating and physical inactivity, are major contributors to increased adult morbidity and mortality from chronic diseases. Over the past decade there has been an increase in sedentary lifestyle and obesity in children and adolescents, both in North America and worldwide. Physicians need to be aware of the scope of this problem, provide anticipatory guidance to families and promote healthy active living in their practices.
Keywords: Healthy active living, Lifestyle
Français en page 351
Asedentary lifestyle and the consumption of foods that are high in total energy and fat content are factors that are associated with obesity, cardiovascular disease, type II diabetes, inadequate bone mineralization and poor mental health. Atherosclerosis, which has been identified as early as the second decade of life, may be the result of five major risk factors: tobacco use, dyslipidemia, hypertension, obesity and inadequate physical activity (1). The objective of this statement is to discuss some of the negative health implications of childhood physical inactivity and inappropriate diet and to outline the benefits of an active, healthy lifestyle.
OBESITY
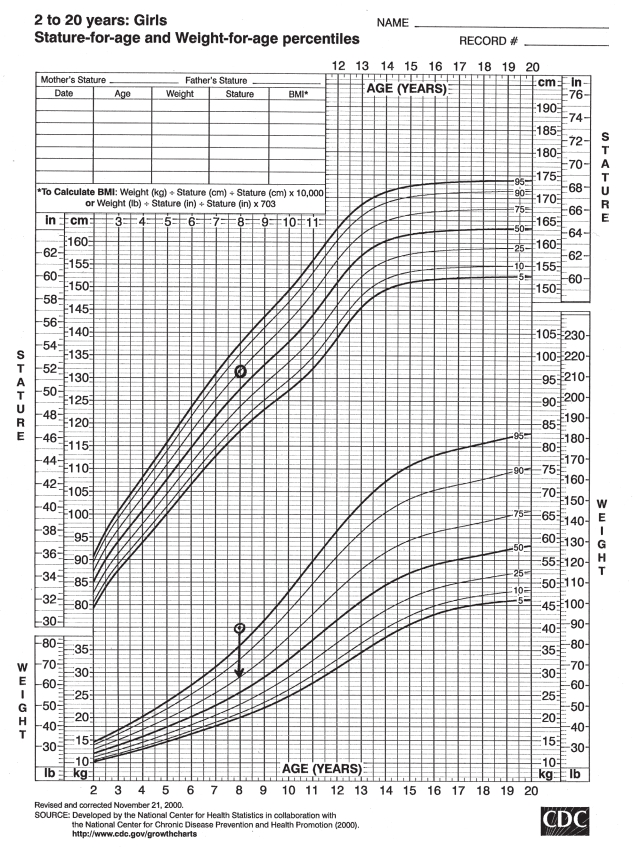
Obesity is defined as having excess body fat (Table 1) (Figure 1) (2–6). The prevalence of childhood obesity in Canada has tripled from 1981 to 1996 (7). Almost 25% of American youth are considered to be obese, which represents a 20% increase in prevalence over the past decade (8). Obesity during childhood increases the risk of adult obesity. Forty per cent of obese seven-year-olds and 70% of obese adolescents become obese adults (9). Genetic heritability accounts for 25% to 40% of juvenile obesity, leaving considerable influence on body weight from environmental factors (10).
TABLE 1.
Definitions of obesity
| Because the measurement of body fat is difficult, surrogate definitions based on weight-for-height relationships have been developed. The most practical definition of obesity is based on actual weight expressed as a percentage of ideal weight for height, age and sex. This involves fitting the child or youth’s height on a standard growth curve. The ideal weight is then derived as the same percentile as that for height. Actual weight is expressed as a percentage of the ideal weight for age, height and sex (2). For example (Figure 1) an eight-year-old girl measures 131.5 cm (75th percentile) and weighs 40 kg (above 95th percentile). Her ideal weight would be derived at 29 kg (75th percentile). Then one can calculate her weight-stature index, which is her actual weight (AW) in kilograms divided by her ideal weight (IW) in kilograms, multiplied by 100 (AW/IW · 100). A normal weight-stature index ranges from 90% to 100%, overweight is from 110% to 120% and obesity is more than 120%. |
| While this same approach can be used in adults, body mass index (BMI) has gained popularity. BMI is defined as the weight in kilograms divided by the height in metres squared (kg/m2). The United States Centers for Disease Control and Prevention have recently developed BMI charts for children and youth (3). The normal ranges for BMI in adults are constant values, with obesity defined as the 85th percentile and superobesity as above the 95th percentile. |
| These same definitions are also used for the range of triceps skin fold percentiles (4). Even though BMI values are lower during childhood and gradually increase to reach adult values around 18 years of age, in practical terms the same percentile ranges of the 85th percentile to define obesity and above the 95th percentile to define superobesity have been applied successfully (5,6). |
Figure 1).
A growth chart showing an example of typical childhood growth. BMI Body mass index; CDC Centers for Disease Control and Prevention. Circles represent actual height and weight; Arrow points to ideal weight for height. <www.cdc.gov/nchs/about/major/nhanes/growthcharts/set1clinical/cj41l022.pdf>
The cause of obesity is a chronically positive energy balance (ie, energy intake exceeds energy expenditure). Recent studies have shown that obese children and adolescents ingest about 20% more energy than normal weight controls (11,12). While studies worldwide agree that obese children and youth have low levels of physical activity, data are less consistent regarding energy expenditure. By using the ‘gold standard’ doubly-labelled water technique, studies have suggested that 24-h energy expenditure is higher, the same or lower in obese children than in nonobese children (7,13,14).
Inappropriate nutrition may play an important role in childhood obesity. In a 1998 Canadian survey (15) of the eating habits of grade 6 students, approximately 73% said that they ate fruit at least once a day, while 45% said that they had at least one serving of vegetables each day. About 15% of these students ate french fries or potato chips daily and 24% ate candy or chocolate bars daily. More than 60% of American youth eat too many fatty foods, and less than 20% eat the recommended five or more servings of fruits and vegetables per day (16).
The consumption of fast foods has been associated with excess weight gain. This may be related to the higher energy and fat content of most of these foods. Fast-food restaurants also offer increasingly larger portions, which encourages the ingestion of greater amounts (16).
While the incidence of juvenile obesity has increased over the past decade, there has been a decrease in overall fat consumption by the general population (17). This suggests that physical inactivity also plays an important role in the development of obesity.
Approximately 28% of Canadians 12 to 14 years old and 66% of Canadian youth aged 15 to 19 years are deemed to be physically inactive (18). In addition, only 46% of Canadian children between the ages of five and 17 years satisfy the energy expenditure guideline for optimal health and development (8 kcal/kg/day), recommended by Sallis in an American consensus statement (19). A higher proportion of girls are inactive at all ages, and a significant decline in physical activity, which is greater in girls, occurs during adolescence. At five to 12 years of age, 30% of girls are physically active compared with 50% of boys, and at 13 to 17 years of age these statistics drop to 25% and 40%, respectively (19).
One of the traditional approaches to addressing physical inactivity has been to focus on individual awareness of the benefits of and opportunities for leisure time physical activity to affect change in behaviour. However, recent research has demonstrated the importance of social, physical and cultural environments in determining the extent to which people are able to be active in all facets of daily life, including work, education, family life and leisure. Modifying the aspects of social, physical and cultural environments that pose barriers to physical activity, and enhancing those which are supportive will make active living an easier choice for Canadians. Creating active school communities is an essential component of a healthy active lifestyle. An active school community is one in which all citizens, including teachers, students, parents, administrators and community leaders, work together to create physical and social environments that support active, healthy lifestyles (20).
In addition to a lack of physical activity, there has been an increase in sedentary behaviour such as watching television and using video games and computers. In the fall of 2000, Canadian children watched an average of 15.5 h of television a week, while youth aged 12 to 17 years watched an average of 14.1 h weekly (21). Ninety-eight per cent of American households in 1998 had a television, and the number of households with two or more televisions has increased dramatically (22). American children aged six to 11 years watch an average of 23 h of television per week (23). Television watching is associated strongly with an increased risk in obesity because it involves both a decrease in energy expenditure and an increase in energy intake by excessively eating high fat-and high energy-containing snack foods (24).
Video and computer games are becoming more popular for children and youth. In 2000, 4.7 million Canadian households were connected to the Internet, and 71% of households reported that at least one person in the home regularly used the Internet at least seven times weekly. This number was up from 65% in 1999 (25). During the first three months of 2000, 11 million personal computers were delivered to American stores for retail sale, which represented a 14.5% increase from the previous year (26). It is difficult to determine whether the time children spend on computers replaces other sedentary activities or further reduces more active pursuits.
Obese children are at an increased risk for hypertriglyceridemia, hypercholesterolemia, hyperinsulinemia, type II diabetes mellitus, hypertension, respiratory disorders, orthopedic problems and psychological problems during their youth. Because juvenile obesity frequently tracks into adulthood, it could lead to higher rates of morbidity and mortality from cardiovascular disease, diabetes, arthritis-related disability and some cancers. Thus, preventing and treating obesity in childhood and adolescence is a critical public health issue and an important determinant of health.
To date, there are limited quality data on the effectiveness of childhood obesity prevention programs. A systematic review of the recent literature found only seven studies that used interventions such as dietary education, physical activity programs and reduction of sedentary activity. These studies were diverse in design, quality, target population and outcome measures, making it difficult to reach generalizable conclusions (27). A good prevention program is one that encourages family lifestyle changes by promoting a healthy, satisfying diet, protecting children against advertisements for nonhealthy, fatty foods and large format servings, and decreasing sedentary behaviours (17). There is an urgent need for well-designed studies that examine a range of interventions so that sound preventive programs can be generated.
HYPERTENSION
Nearly three million American youths have high blood pressure (28). Obese children are especially prone to hypertension. Children aged six to 11 years with triceps skin-fold thickness at or above the 85th percentile were 2.6 and 1.6 times more likely than their leaner peers to have elevated systolic and diastolic blood pressures, respectively (29). Juvenile onset hypertension tracks into adulthood, making it a major public health concern (30).
Preventing and treating childhood-onset hypertension is critical. When continued over eight months or more, aerobic training (ie, running) has been shown to reduce systolic and diastolic blood pressure in adolescents with hypertension (31). Likewise, resistance training following aerobic training can further decrease blood pressure, even though blood pressure increases during acute bouts of resistance exercise (weight lifting for example) (32). Physicians should regularly monitor blood pressure at yearly check-ups and encourage youth to adopt active, healthy lifestyles, and to avoid high fat foods and tobacco use to prevent hypertension in childhood.
TYPE II DIABETES
Type II diabetes affects more than 1.8 million Canadian adults and may result in the accelerated development of cardiovascular disease, end stage renal failure, loss of vision and limb amputations (33). The prevalence of type II diabetes is increasing in youth, with up to 45% of children with newly diagnosed diabetes having nonimmune-mediated disease (34). A family history of type II diabetes is typical and obesity is a hallmark, with up to 85% of affected children overweight or obese at diagnosis. An increased proportion of Canadian Aboriginals, African-Americans, American Indians and Asians have type II diabetes (34,35). The usual age of onset is 12 to 14 years, which coincides with relative insulin resistance known to occur in puberty. The rise in obesity and decrease in physical activity levels in this age group also contribute to insulin resistance and may be significant risk factors for the development of diabetes (36). The treatment of type II diabetes in children requires a comprehensive understanding of the cultural, linguistic, geographic, economic and religious background of the family, as well as an understanding of the family’s life experience with complications of the disease. Modification of lifestyle, with attention to proper nutrition and physical activity, must be the foundation of all treatment programs. Scientific evaluation of various pharmacological treatments is limited (37).
OSTEOPOROSIS
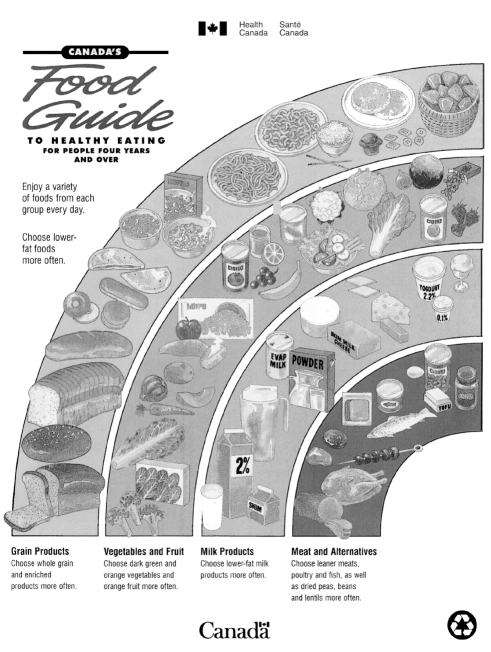
Osteoporosis is a major health problem in Canada that causes fractures, disability, pain and deformity in the elderly population. It affects one in four women and one in eight men over 50 years of age (38). Peak bone mineral mass is usually achieved by the third decade of life, and the maximum bone acquired during the first 20 years of life is an important determinant of final bone mass and bone health in later years (39). Before puberty, bone mineral density in boys and girls is similar; however, adolescent females achieve peak bone mass at 11 to 14 years of age and it rapidly declines thereafter, and adolescent males continue to increase bone mass until 15 to 16 years of age and then follow a slower subsequent decline (40). Central hormonal factors such as estrogen, appropriate nutrition and local mechanical forces positively affect bone mass during growth and development. Weight bearing exercises during puberty may improve bone mineral content and result in a greater peak bone mass, which may delay the age at which the osteoporotic fracture limit is reached (41). Prolonged periods of inactivity during youth result in higher osteoclastic activity and bone atrophy, which may have a serious negative impact on peak bone mass. Sedentary lifestyles in childhood may, therefore, contribute to increasing rates of osteoporosis and its complications later in life. To improve good bone health, physicians should recommend appropriate nutrition, including an age-appropriate vitamin D and calcium intake in accordance with Canada’s Food Guide (Figure 2), regular weight-bearing physical activity and avoidance of tobacco use.
Figure 2).
Canada’s Food Guide to Healthy Eating <www.hc-sc.gc.ca/hppb/nutrition/pube/foodguid/index.html>
MENTAL HEALTH
In 1996–97, 113,000 Canadians 12 to 17 years of age were given the diagnosis of depression lasting an average of 4.5 weeks (42). Body image and ‘fitting in’ with perceived norms of weight, height and sexual development are key concerns for adolescents. Juvenile obesity is associated with poor self-esteem, depression and social discrimination (43).
Regular physical activity is beneficial psychologically for all youths, regardless of weight. It is associated positively with self-esteem and self-concept, and associated negatively with anxiety and depression (44). Some studies have shown a reduction in the proportion of youth smoking cigarettes, drinking alcohol and taking illicit drugs when they are involved in regular physical activities (45–47).
SCHOOL PERFORMANCE
In 1999, Canada’s high school dropout rate was 12%, down 33% from an estimated 18% in 1991 (48). Students leaving before graduation were more likely to report a lack of enjoyment with school, dissatisfaction with their courses and teachers, and nonparticipation in extracurricular activities.
School physical education programs and extracurricular physical activities could play a significant role in improving students’ attitudes, discipline and behaviours (49). Although information on the number of children in Canada taking regular physical education classes is incomplete, it is estimated that most schools offer half of the recommended provincial requirement, and less than 4% offer quality daily physical education programs. Unfortunately, in 2001, only 33% of all schools in Canada had formal physical education classes, and programming varied from school to school (Guy Tanguay, personal communication). Formal physical education is optional after grade nine in Canada. In recent years, parents and the business community have pressured educators to adjust the curriculum to prepare students for the workforce. Some claim that reducing the number of hours spent on physical activity will increase academic achievement. Yet, there is no evidence that regular physical activity hinders educational performance and there is modest evidence that shows that it actually enhances academic achievement (50). The 1996 United States Surgeon General’s report recommend 1 h or more of aerobic physical activity and exercise on most days (51).
Physicians have a vital role to play in the reinstatement of regular quality daily physical education in all schools and in all age groups. Children and youth should be provided with safe school recreation facilities that are stocked with appropriate equipment, ensuring exposure to a wide range of physical activities, especially those encouraging lifestyle changes. School-based facilities are not only important for increasing physical activity during school hours, they are an essential means to allow all children access to cost effective community recreation programs after school.
RECOMMENDATIONS
Physicians and health care professionals are encouraged to promote healthy active living for all family members by:
inquiring about nutritional intake and physical activity levels of all children and youth at regular health care visits.
promoting an increased consumption of cereal fibre, fruit, vegetables and water, rather than high fat-and sugar-containing snacks, and juice or soft drinks, in accordance with Canada’s Food Guide (Figure 2).
encouraging children and adolescents to increase the time that they spend on physical activities and sports by at least 30 min/day, with at least 10 min involving vigorous activities. Vigorous activities are those that increase the heart rate and respiratory rate and increase body temperature (Table 2) (51). To get added benefit, they should review their activity patterns every month and progressively increase their efforts. Once the first goal of increasing their current activities by at least 30 min is achieved, the goals should be reset to involve more time and to be more challenging. For example, if children or youth are inactive, they should begin with at least 20 min of moderate physical activity plus 10 min of vigorous physical activity per day for the first month. They should then increase the moderate component by 10 min/day and the vigorous component by 5 min/day each month to achieve an exercise protocol of at least 90 min/day of total physical activity. Events should include a wide variety of weight-bearing activities as part of sports, recreation, transportation, chores, work, planned exercise and school-based physical education classes. Activities should be fun and unstructured for best compliance.
counselling families to reduce sedentary activities by limiting exposure to television and video and/or computer games. An achievable first step is to reduce these activities by 30 min/day, and subsequently decreasing sedentary activities by 5 min/month, allowing up to 90 min/day for these activities.
encouraging parents to be positive role models for their children and incorporate physical activities that family members of all ages can do together. Families should take part in activities safely by wearing appropriate protective equipment (bicycle helmets, life jackets, etc).
advising parents to enrol their children in age-and developmentally appropriate sports and recreational activities.
encouraging youth to be involved in the promotion of physical activities for their peers.
promoting and using Canada’s Physical Activity Guide (www.paguide.com) for healthy active living for children and youth as a tool to encourage children and youth to be more active.
TABLE 2.
Energy costs of activities of daily living (expressed in relationship to basal metabolic rate [BMR])
| Activity factor | ||
|---|---|---|
| Sleeping | 1.0 | |
| Lying awake | 1.2 | |
| Sitting quietly | 1.2 | |
| Standing quietly | 1.4 | |
| Walking slowly | 2.8 | |
| Walking at normal pace | 3.2 | |
| Walking uphill fast | 7.5 | |
| Recreation | ||
| light (billiards, baseball, golf, sailing) | 2.2–4.4 | |
| moderate (dancing, swimming, tennis) | 4.4–6.6 | |
| heavy (soccer, jogging, rowing) | 6.6+ | |
| BMR values for children and youth (kcal/min) | ||
| Age group (years) | Girls | Boys |
| 5–10 | 0.7 | 0.7 |
| 10–14 | 0.89 | 0.95 |
| 14–18 | 0.98 | 1.2 |
| Example | ||
| A nine-year-old girl walking at a normal pace for 30 min | ||
| 0.7 ·3.2 ·30 = 67.2 kcal (or 2.24 kcal/min) (BMR) ·(activity factor) ·(time) | ||
FAO/WHO/UNU Expert Consultation. Energy and protein requirements. Data from reference 52
Physicians and health care professionals should advocate for:
initiatives to serve healthy foods and eliminate the sale of high carbohydrate soft drinks and high fat or sugar snacks in schools. Alternate funding for healthier food choices should be sought.
policies that reduce the sale of over-sized fast foods.
initiatives that provide children and youth with quality daily physical education classes (kindergarten to grade 12) by qualified, trained educators and the use of school-based sports facilities during after-school hours.
comprehensive community sport and recreation programs in which the use of community and school facilities after hours may make more recreation programs available to all children at reasonable costs. Access to these facilities should be equally available to both sexes.
the construction of safe recreational facilities, playgrounds, parks, bike paths, sidewalks and roads.
the reinstatement of compulsory physical education throughout all age groups in all schools.
the appropriate allocation of funding for quality research in the prevention of childhood obesity.
Acknowledgments
Financial assistance for the development of this position statement was provided by Health Canada.
Footnotes
ADVISORY COMMITTEE ON HEALTHY ACTIVE LIVING FOR CHILDREN AND YOUTH
Members: Drs Oded Bar-Or, Children’s Exercise and Nutrition Centre, McMaster University, Hamilton, Ontario; Danielle Grenier, Gatineau, Quebec (CPS Medical Affairs Officer); Robert M Issenman, Department of Paediatrics, Children’s Hospital-Hamilton Health Sciences Centre, Hamilton, Ontario; Claire LeBlanc, Children’s Hospital of Eastern Ontario, Ottawa, Ontario (chair); Peter Nieman, Calgary, Alberta; Alain Pavilanis, St Mary’s Hospital Centre, Montreal, Quebec (College of Family Physicians of Canada); Paul Pencharz, Division of Gastroenterology and Nutrition, Hospital for Sick Children, Toronto, Ontario; Ron Siemens, Pediatric Clinic, Queen Elizabeth Hospital, Charlottetown, Prince Edward Island; Trent Smith, British Columbia Children’s Hospital, Vancouver, British Columbia; Michael Westwood, Beaconsfield, Quebec
Principal Author: Dr Claire LeBlanc
The recommendations in this statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate.
Internet addresses are current at the time of publication.
REFERENCES
- 1.Gidding SS. Preventive pediatric cardiology. Pediatr Clin North Am. 1999;46:253–62. doi: 10.1016/s0031-3955(05)70116-4. [DOI] [PubMed] [Google Scholar]
- 2.Moore DJ, Durie PR, Forstner GG, Pencharz PB. The assessment of nutritional status in children. Nutr Res. 1985;5:797–9. [Google Scholar]
- 3.Kuczmarshi RJ, Ogden CL, Grummer-Strawn LM, et al. CDC Growth charts: United States advance data from vital health statistics no 314. Hyattville: National Center for Health Statistics; 2000. [Google Scholar]
- 4.Must A, Dallal GE, Dietz WH. Reference data for obesity: 85th and 95th percentiles of body mass index (wt/ht2) and triceps skinfold thickness. Am J Clin Nutr. 1991;53:839–46. doi: 10.1093/ajcn/53.4.839. [DOI] [PubMed] [Google Scholar]
- 5.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flegal KM, Ogden CL, Wei R, Kuczmarski RL, Johnson CL. Prevalence of overweight in US children: Comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass index. Am J Clin Nutr. 2001;73:1086–93. doi: 10.1093/ajcn/73.6.1086. [DOI] [PubMed] [Google Scholar]
- 7.Tremblay MS, Willms JD. Secular trends in the body mass index of Canadian children. CMAJ. 2000;163:1429–33. 2001;164:970. [PMC free article] [PubMed] [Google Scholar]
- 8.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson JC. Overweight prevalence and trends for children and adolescents. Arch Pediatr Adolesc Med. 1995;149:1085–91. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 9.Mossberg HO. 40-year follow-up of overweight children. Lancet. 1989;ii:491–3. doi: 10.1016/s0140-6736(89)92098-9. [DOI] [PubMed] [Google Scholar]
- 10.Bouchard C. Genetics of obesity: Overview and research directions. In: Bouchard C, editor. The Genetics of Obesity. Boca Raton: CRC Press; 1994. pp. 223–33. [Google Scholar]
- 11.Maffies C, Schutz Y, Zaffanello M, Piccoli R, Pinelli L. Elevalted energy expenditure and reduced energy intake in obese prepubertal children: Paradox of poor dietary reliability in obesity? J Pediatr. 1994;124:348–54. doi: 10.1016/s0022-3476(94)70355-8. [DOI] [PubMed] [Google Scholar]
- 12.Bandini LG, Schoeller DA, Cyr HN, Dietz WH. Validity of reported energy intake in obese and nonobese adolescents. Am J Clin Nutr. 1991;52:421–5. doi: 10.1093/ajcn/52.3.421. [DOI] [PubMed] [Google Scholar]
- 13.Delany JP, Harsha DW, Kime JC, Kumler J, Melancon L, Bray GA. Energy expenditure in lean and obese prepubertal children. Obes Res. 1995;1:67–72. doi: 10.1002/j.1550-8528.1995.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 14.Davies PSW, Gregory J, White A. Physical activity and body fatness in pre-school children. Int J Obes. 1995;19:6–10. [PubMed] [Google Scholar]
- 15.Trends in the Health of Canadian Youth. Ottawa: Health Canada; 1999. [Google Scholar]
- 16.The Importance of Physical Activity and Good Nutrition. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention 2001.
- 17.Bar-Or O, Foreyt J, Bouchard C, et al. Physical activity, genetic, and nutritional considerations in childhood weight management. Med Sci Sports Exerc. 1998;30:2–10. doi: 10.1097/00005768-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Canadian statistics – exercise frequency. Statistics Canada. 1998.
- 19.1999 Physical Activity Monitor. Ottawa: Canadian Fitness and Lifestyle Research Institute; [Google Scholar]
- 20.Health Canada 2001 . The Population Health Template: Key Elements and Actions that Define a Population Health Approach. Ottawa: Health Canada; 2001. [Google Scholar]
- 21.Average hours per week of television viewing (Catalogue no. 87F0006XPB) Ottawa: Statistics Canada; <www.statcan.ca/english/Pgdb/People/Culture/arts23.htm> (Version current at April 22, 2002). [Google Scholar]
- 22.Norris J, Harnack L, Carmichael S, Pouane T, Wakimoto P, Block G. US trends in nutrient intake: The 1987 and 1992 National Health Interview Surveys. Am J Public Health. 1997;87:740–6. doi: 10.2105/ajph.87.5.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AC Nielsen Company . Nielsen Report on Television. New York: Nielsen Media Research; 1990. 1990. [Google Scholar]
- 24.Dietz WH, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75:807–12. [PubMed] [Google Scholar]
- 25.Household Internet Use Survey The Daily July262001Ottawa: Statistics Canada; <http://www.statcan.ca/Daily/English/010726/d010726a.htm> (Version current at April 22, 2002). [Google Scholar]
- 26.New York Times PC sales in the first quarter show double-digit growthNew York Times, April 24, 2000.
- 27.Campbell K, Waters E, O’Meara S, Summerbell C.Interventions for preventing obesity in children The Cochrane library, issue 1, 2002<www.cochranelibrary.com> (Version current at April 22, 2002).
- 28.National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents 1996 Update on the 1987 task force report on high blood pressure in children and adolescents: A working group report from the National Blood Pressure Education Program. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 29.Gortmaker SL, Dietz WH, Sobol AM, Wehler CA. Increasing pediatric obesity in the United States. Am J Dis Child. 1987;141:535–40. doi: 10.1001/archpedi.1987.04460050077035. [DOI] [PubMed] [Google Scholar]
- 30.Anderson LB, Haraldsdottir J. Tracking cardiovascular disease risk factors including maximal oxygen uptake and physical activity from late teenage to adulthood. An 8-year follow-up study. J Int Med. 1993;234:309–15. doi: 10.1111/j.1365-2796.1993.tb00748.x. [DOI] [PubMed] [Google Scholar]
- 31.Hansen HA, Froberg K, Hyldebrandt N, Nielsen JR. A controlled study of eight months of physical training and reduction of blood pressure in children: The Odense schoolchild study. BMJ. 1991;303:682–5. doi: 10.1136/bmj.303.6804.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hagberg JM, Ehsani AA, Goldring D, Hernandez A, Sinacore DR, Holloszy JO. Effect of weight training on blood pressure and hemodynamics in hypertensive adolescents. J Pediatr. 1984;104:147–51. doi: 10.1016/s0022-3476(84)80615-0. [DOI] [PubMed] [Google Scholar]
- 33.About Diabetes Toronto: Canadian Diabetes Association; <www.diabetes.ca/about_diabetes/index.html> (Version current at April 22, 2002). [Google Scholar]
- 34.American Diabetes Association Consensus Conference Type 2 Diabetes in Children and Adolescents. Pediatrics. 2000;105:671–80. doi: 10.1542/peds.105.3.671. [DOI] [PubMed] [Google Scholar]
- 35.Young TK, Reading J, Elias B, O’Neil JD. Type 2 Diabetes mellitus in Canada’s First Nations: Status of an epidemic in progress. CMAJ. 2000;163:561–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Callahan ST, Mansfield MJ. Type 2 diabetes mellitus in adolescents. Curr Opin Pediatr. 2000;12:310–15. doi: 10.1097/00008480-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Dean H. Treatment of type 2 diabetes in youth: An argument for randomized controlled studies. Paediatr Child Health. 1999;10:265–9. doi: 10.1093/pch/4.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hanley DA, Josse RG. Prevention and management of osteoporosis: Consensus statements from the Scientific Advisory Board of the Osteoporosis Society of Canada. 1. Introduction. CMAJ. 1996;155:921–3. [PMC free article] [PubMed] [Google Scholar]
- 39.Haapasalo H, Kannus P, Sievanen H, et al. Development of mass, density, and estimated mechanical characteristics of bones in Caucasian females. J Bone Miner Res. 1996;11:1751–60. doi: 10.1002/jbmr.5650111119. [DOI] [PubMed] [Google Scholar]
- 40.Kemper HCG. Skeletal development during childhood and adolescence and the effects of physical activity. Pediatr Exerc Sci. 2000;12:198–216. [Google Scholar]
- 41.Heinonen A, Sievanen H, Kannus P, Oja P, Pasanen M, Vuori I. High-impact exercise and bones of growing girls: A 9-month controlled trial. Osteoporos Int. 2000;11:1010–7. doi: 10.1007/s001980070021. [DOI] [PubMed] [Google Scholar]
- 42.Satistics Canada National Population Health Survey 1996–1997 Ottawa: Satistics Canada; 1998. <www.statcan.ca/english/Pgdb/People/Health/health35.htm> (Version current at April 30, 2002). [Google Scholar]
- 43.Friedman MA, Brownell KD. Psychological correlates of obesity: Moving to the next research generation. Psychol Bull. 1995;117:3–20. doi: 10.1037/0033-2909.117.1.3. [DOI] [PubMed] [Google Scholar]
- 44.Calfas KJ, Taylor WC. Effects of physical activity on psychological variables in adolescents. Pediatr Exerc Sci. 1994;6:406–23. [Google Scholar]
- 45.Shields EW., Jr Sociodemographic analysis of drug use among adolescent athletes: Observations-perceptions of athletic directors-coaches. Adolescence. 1995;30:839–61. [PubMed] [Google Scholar]
- 46.Forman ES, Dekker AH, Javors JR, Davison DT. High-risk behaviors in teenage male athletes. Clin J Sport Med. 1995;5:36–42. doi: 10.1097/00042752-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 47.Oler MJ, Mainous AG, 3rd, Martin CA, et al. Depression, suicidal ideation, and substance use among adolescents – Are athletes at less risk? Arch Fam Med. 1994;3:781–7. doi: 10.1001/archfami.3.9.781. [DOI] [PubMed] [Google Scholar]
- 48.Statistics Canada Youth in Transition SurveyThe Daily, January 23, 2002. <www.statcan.ca/Daily/English/020123/d020123a.htm> (Version current at April 22, 2002).
- 49.Keays JJ, Allison KR. The effects of regular moderate to vigorous physical activity on student outcomes: A review. Can J Public Health. 1995;86:62–5. [PubMed] [Google Scholar]
- 50.Shephard RJ. Curricular physical activity and academic performance. Pediatr Exerc Sci. 1997;9:113–26. [Google Scholar]
- 51.US Department of Health and Human Services . 1996 Physical Activity and Health: Report of the Surgeon General. Atlanta: United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Diseases; 1996. [Google Scholar]
- 52.FAO/WHO/UNU Expert Consultation Energy and protein requirements World Health Organization 1985 Technical Report Series 724. Geneva: World Health Organization; 1985 [PubMed] [Google Scholar]