Abstract
Studies were conducted to determine whether maternal substrate utilization during pregnancy affects fetal growth and predisposes offspring to metabolic disease. Female wild type (WT) and glucose transporter 4 heterozygous mice (G4+/−, a model of altered peripheral substrate utilization) were fed high fat (HFD, 36% fat) or control chow (C, 10% fat) for 2 weeks prior to mating, throughout pregnancy and lactation (IU/L). WT HFD females exhibited increased serum NEFA and lactate levels and increased hepatic mRNA expression of PGC1-β and SREBP-1c consistent with increased lipogenesis. G4+/− HFD females exhibited enhanced lipid clearance and exposure to HFD did not increase hepatic gene expression. HFD independent of maternal genotype decreased fetal growth, and birth weight. WT offspring were weaned onto a low-fat diet (5% fat). Male offspring of WT mothers exposed to HFD exhibited “catch-up” growth accompanied by increased adiposity, impaired glucose tolerance, and insulin sensitivity. In contrast, male offspring of G4+/− HFD mothers did not exhibit any characteristics of metabolic syndrome. These data suggest that differences in maternal substrate utilization influence offspring metabolic phenotype.
The global epidemic of Metabolic Syndrome (1,2) cannot be explained entirely by genetics and/or lifestyles. Data suggest that predisposition to these adult diseases have an important portion of their origin in the intrauterine (IU) and early postnatal environment (3). Epidemiological and animal studies have demonstrated that incidence of type 2 diabetes mellitus (T2DM) and obesity is increased in offspring whose mothers were themselves diabetic or obese pre-pregnancy (4), perpetuating the prevalence of Metabolic Syndrome and T2DM.
Consumption of Western style high fat (HFD) diets increases the risk for gestational diabetes mellitus (GDM), impaired glucose tolerance (5) and preeclampsia during pregnancy (6). In animal models exposure to HFD IU results in impaired glucose homeostasis, cardiovascular dysfunction, programming of hepatic metabolism and insulin resistance (7). Less is known about the interaction between consumption of a Western style HFD during pregnancy and maternal alterations in substrate utilization in programming metabolic disease in offspring. Fetal development is dependent on maternal supply of nutrients and an altered maternal metabolism would expose the fetus to an unfavorable balance of energy substrate that may predispose offspring to adult disease (8). Mice with homozygous deletion of glucose transporter 4 (GLUT4) alter their substrate utilization to maintain normoglycemia in the absence of GLUT4 (9). Mice with heterozygous deletion of GLUT4 expression (G4+/−) have impaired skeletal muscle insulin-stimulated glucose transport and whole-body glucose utilization (10,11). In this study, we utilize female G4+/− mice as a novel model of altered substrate utilization to determine maternal factors that may contribute to the development of metabolic abnormalities in offspring.
RESEARCH DESIGN AND METHODS
Animals and Experimental Design
Animals were housed in a barrier facility and maintained on a 14-10 hour light-dark cycle with ad libitum access to chow and water. Age- and body weight (BW) matched WT or G4+/− female mice (CD1 background) were maintained on control PicoLab® Mouse Diet #5058 (C: 9% fat as soybean oil and animal fat, 20% protein, 53% carbohydrate, 3.59 kcal/g), or high fat Bio-Serv Product #F3282 (HFD: 35.5% fat as lard, 20% protein, 36.3% carbohydrate, 5.29 kcal/g) 2 weeks prior to mating, throughout pregnancy and lactation (IU/L). Females were bred to non-littermate males of the opposite genotype to control for any potential genotype and phenotype effects (12). Pregnancy was confirmed by detection of a copulatory plug and defined as embryonic day (e) 0.5. Genotyping was performed as previously described (13). Offspring were weaned onto PicoLab® Mouse Diet #5053 (low fat- LF: 4.5% fat as soybean oil, 20% protein, 54.8% carbohydrate wt/wt, 3.4 kcal/g) at postnatal day 21. WT offspring were the focus of this study to eliminate potential confounding effects of genetic factors related to postnatal insulin resistance. Animal protocols were approved by the Animal Institute at the Albert Einstein College of Medicine.
Euglycemic/Hyperinsulinemic Clamps
Euglycemic clamps were performed in conscious, unrestrained, catheterized adult female mice (27–32g) as previously described (11,14).
Serum Analysis
Fed-state blood samples were collected between 11:00 p.m. and 1:00 a.m. Blood glucose concentrations were measured using a glucometer (Precision Q.I.D., a gift from Abbott Laboratories, Chicago, IL). Commercially available kits were used for measuring serum insulin, adiponectin, (Linco Research, St. Charles, MO), non-esterified fatty acids (NEFAs) (Wako Chemicals, Neuss, Germany), triglycerides (TG), glucose (Sigma, St. Louis, MO), and lactate (Trinity Biotech, St. Louis, MO).
Maternal Body Weight Gain During Pregnancy
Maternal BW gain during pregnancy was calculated as [(BW day X — BW e0.5)/BW day mating e18.5] × 100.
Food Intake
Mice were housed individually for 4 days before recording BW and daily food consumption (Kcal/BW/day) for a period of 5-8 days. Pregnant mice were placed in individual cages on e0.5, food intake was assessed daily from e0.5 until e18.5. Food intake in offspring was determined in 5 mice randomly selected from 2-4 litters per group.
Maternal Organ Harvest and Fetal Data Collection
Pregnant mice (WT C n=10, WT HFD n=8, G4+/− C n=5, G4+/−HFD n=8) were sacrificed on e18.5; organs were dissected, weighed, and frozen in liquid nitrogen. Litter number, placental and fetal weights, and crown-rump length (CRL) were recorded, as well as the number of abnormal or dead pups per litter. Fetuses were euthanized by cervical dislocation immediately following dissection from the uterine horn.
Oral Lipid Challenge
Following a 5 hr fast, mice received an oral gavage (16.7ml/kg BW) of olive oil as described previously (9). Serum was collected at the indicated times for TG determination.
Intraperitoneal Insulin and Glucose Tolerance Tests
For insulin tolerance tests (ITT), 6 hr fasted mice received an intraperitoneal (i.p.) injection of insulin (0.75U/kg BW) (Humalog, Lilly, Indianapolis, IN). For glucose tolerance tests (GTT), overnight fasted mice received an i.p. injection of D-(+)-glucose (1.5g/kg BW). Blood glucose levels were determined at the indicated times.
Body Composition
Body composition (% body fat) (n=5/group randomly selected from 2-4 litters per group, males: 7-8 wks, females: 6-7 wks) was determined using MRI as previously described (15) or by magnetic resonance spectroscopy using an ECHO magnetic resonance spectroscopy instrument (Echo Medical Systems, Houston, TX) (16).
Quantitative Real Time-PCR Analysis
mRNA expression was performed in livers from pregnant mothers as previously described (17). Primers were designed using Primer Express software (Applied Biosystems), sequences available on request. Data is expressed relative to the WT C group using the average of the constitutive gene cyclophilin b.
Data Analysis
Data represents the mean ± SEM. Statistical analyses were performed using JMP IN 5.1 software (SAS Institute, Cary, NC) or GraphPad Prism software version 5.00 for Windows (GraphPad Software, San Diego California USA, www.graphpad.com). ANOVA was used to test the difference between the means of two (t-test) or more groups. Growth curves, daily food intake, ITT, GTT, and oral lipid clearance experiments were analyzed by Two-way Repeated Measure ANOVA with Bonferroni posttests.
RESULTS
Non-pregnant G4+/− females exhibit decreased insulin sensitivity on a C diet
Euglycemic hyperinsulinemic clamps were performed on 18-20 wk old (n=5/group), BW matched, WT, and G4+/− mice. Steady-state plasma glucose levels were maintained at similar levels in both genotypes (119 ± 0.01 vs. 127 ± 0.01 mg/dl, WT vs. G4+/− respectively, P=NS). Although insulin-mediated suppression of hepatic glucose production during physiological hyperinsulinemia was similar in both groups, glucose infusion rate (GIR) required to maintain normoglycemia was 50% lower in G4+/− compared to WT mice (5.7 ± 0.4 vs. 2.5 ± 0.4 mg/kg/min, WT vs. G4+/− respectively, p=0.001). Decreased GIR was largely accounted for by decreased whole body insulin mediated glucose uptake in G4+/− mice compared to WT mice (6.6 ± 0.9 vs. 3.6 ± 0.6 mg/kg/min, WT vs. G4+/− respectively, p=0.04), demonstrating that G4+/− females exhibit peripheral but not hepatic insulin resistance.
Non-pregnant G4+/− females exhibit increased lipid clearance on HFD
No significant difference in BW was observed in WT or G4+/− females after 2 weeks on a HFD compared to a C diet (Table 1). WT HFD mice exhibited increased NEFA and free glycerol levels and decreased TG levels compared to WT C (Table 1). HFD did not alter the serum profile in G4+/− mice suggesting that G4+/− is resistant to the acute effect of HFD.
Table 1. Effect of acute HFD on metabolic profile.
Age matched female mice were placed on HFD or maintained on Control diet for 2 weeks prior to the determination of fed metabolic profile.
| WT C | G4+/− C | WT HFD | G4+/− HFD | |
|---|---|---|---|---|
| n=10 | n=8 | n=10 | n=8 | |
| Age (wks) | 13.7±0.7 | 15.2±0.8 | 14.6±0.7 | 15.0±0.9 |
| Body weight (g) | 36.8±1.9 | 39.1±2.3 | 39.0±2.0 | 40.2±2.6 |
| Food intake (kcal/day/g BW) | 0.48 ± 0.07 | 0.46 ± 0.07 | 0.38 ± 0.05 | 0.34 ± 0.3 |
| Glucose (mg/dl) | 125.8±2.5 | 137.0±4.0 | 123.5±6.3 | 137.4±6.2 |
| Insulin (ng/ml) | 2.27±1.0 | 4.64±1.4 | 2.91±1.1 | 4.21±1.32 |
| Lactate (mg/dl) | 47.9±3.9 | 38.8±5.0 | 53.5±4.1 | 40.7±5.0 |
| NEFA (μEq/ml) | 2.36±0.19 | 2.43±0.25 | 3.19±0.19¶ | 2.77±0.29 |
| Triglyceride (mg/dl) | 60.45±6.9 | 37.57±8.5* | 36.58±6.9¶ | 21.93±8.5 |
| Free Glycerol (mg/dl) | 110.2±15.1 | 121.9±16.8 | 144.1±5.3¶ | 123.2±6.2 |
| Adiponectin (ng/ml) | 15.12±2.1 | 16.86±2.5 | 12.41±2.5 | 17.98±2.8 |
Data represents mean ± SE
P<0.05 vs. WT
P<0.05 vs. Control (C) diet
Due to the altered serum lipid profile, the ability to clear orally administrated lipids was assessed (Figure 1). G4+/− HFD mice exhibited the lowest serum TG levels; this may be due to an improved ability to clear TG.
Figure 1.
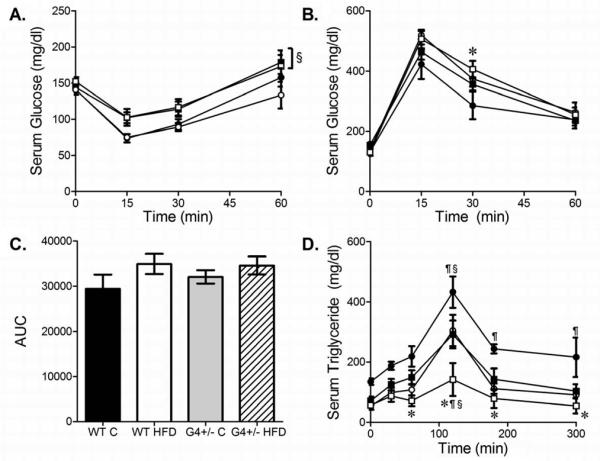
Effect of HFD on (A) ITT, (B) GTT, (C) Area Under the GTT Curve and (D) Lipid Clearance in WT and G4+/− Females. WT C (black circles), WT HFD (white circles), G4+/− C (black squares), and G4+/− HFD (white squares) mice. n=5-7 per group. * P<0.05 vs. WT C, § P<0.05 vs. WT HFD, ¶ P<0.05 vs. G4+/− C.
HFD did not affect insulin and glucose tolerance (Figure 1). Despite not having significant differences in the ITT, G4+/− females were insulin resistant by a clamp study, the gold standard method for measuring insulin action in vivo.
HFD during pregnancy decreases litter weight
Birthweight of offspring exposed to HFD IU was decreased compared with offspring exposed to C diet independent of maternal genotype (Table 2). HFD also decreased the number of pups per litter, although this only reached significance in WT HFD group (Table 2).
Table 2. Characteristics of newborn pups.
Litter size and pup weight was determined within 24 hrs of birth.
| WT C | G4+/− C | WT HFD | G4+/− HFD | |
|---|---|---|---|---|
| Pups per litter (litters) |
12.2 ± 0.9 (10) |
11.6 ± 1.2 (8) |
8.6 ± 0.8¶ (10) |
9.4 ± 0.8 (8) |
| Pup weight (g) (pups) |
1.61 ± 0.01 (164) |
1.59 ± 0.02 (87) |
1.49 ± 0.03¶ (111) |
1.49 ± 0.03¶ (78) |
| Total litter weight (g) |
18.95 ± 1.54 | 17.30 ± 1.57 | 11.47 ± 1.01¶ | 12.6 ± 1.72 |
Data represents mean ± SEM
P<0.05 vs. Control (C) diet
Numbers in parenthesis represents total number of pups per group
HFD alters weight gain during pregnancy
Due to decreased litter weight with HFD, the effects of HFD on maternal BW gain and food intake were assessed. Groups exposed to HFD gained significantly more weight in the first half of pregnancy (e0.5-e9.5) compared to C groups (0.74 ± 0.76, 1.23 ± 0.37 vs. 3.97 ± 0.80, 3.27 ± 0.38 g, WT C, G4+/− C vs. WT HFD, G4+/− HFD respectively, P<0.005) (Figure 2A, B). In the second half of pregnancy (e10.5-e17.5), HFD groups gained less weight compared to C groups (20.02 ± 2.71, 23.82 ± 1.18 vs. 14.17 ± 3.55, 13.05 ± 2.66 g, WT C, G4+/− C vs. WT HFD, G4+/− HFD respectively, P<0.02).
Figure 2.
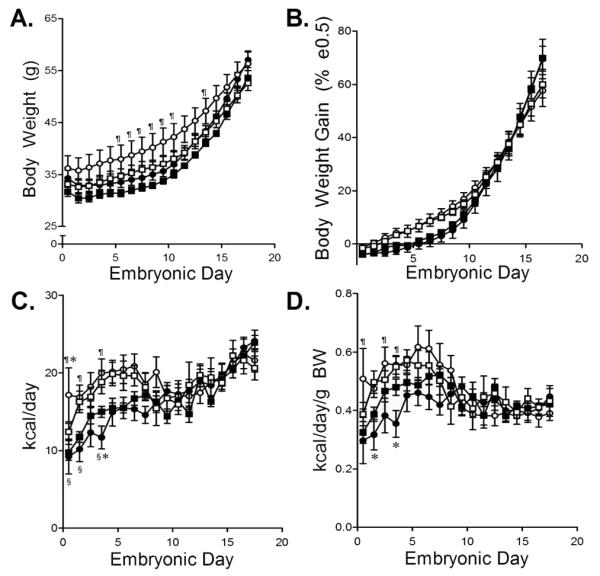
BW Gain and Food Intake During Pregnancy. (A) BW and (B) % BW Gain in WT C (black circles), WT HFD (white circles), G4+/− C (black squares) and G4+/− HFD (white squares) mice. (C) Daily kcal consumed and (D) Daily kcal consumed/BW. 4-10 mice/ group. ¶ P<0.05 vs. G4+/− C, § P<0.05 vs. WT HFD, * P<0.05 vs. G4+/− HFD.
HFD groups consumed more calories from e0.5-e9.5 compared with C groups (110 ± 9, 131 ± 5, 172 ± 12, 151 ± 10 kcal, WT C, G4+/− C, WT HFD, G4+/− HFD respectively, P<0.005) (Figure 2C). No difference in total calories was observed from e10.5-e17.5 (169 ± 7, 167 ± 6, 171 ± 13, 162 ± 9 kcal, WT C, G4+/− C, WT HFD, G4+/− HFD respectively, P=NS) (Figure 2C, D). There was no significant difference in total protein consumption during pregnancy among groups (65 ± 5, 65 ± 3, 55 ± 4, 53 ± 4 kcal, WT C, G4+/− C, WT HFD, G4+/− HFD respectively, n=7-12 mice/group, P=NS).
HFD decreases fetal size but not litter number or maternal organ weights
To determine how fetal and maternal organ weights contributed to differences in weight gain during pregnancy mice were sacrificed at e18.5. No difference in number of fetuses per litter was seen (11.3 ± 0.9, 9.4 ± 0.9, 10.1 ± 0.8, 10.6 ± 0.8, WT C, G4+/− C, WT HFD, G4+/− HFD, n=57-84 fetuses from 5-10 litters per group) and was present at expected Mendelian frequencies (49 vs. 51%, WT vs. G4+/− fetuses, respectively, n=306 fetuses from 31 litters per group, P=NS). Fetal genotype did not affect BW, CRL, or placental weight (data not shown). Exposure to HFD decreased fetal BW (1.46 ± 0.02, 1.51 ± 0.02, 1.28 ± 0.02¶, 1.23 ± 0.02*g, WT C, G4+/− C, WT HFD, G4+/− HFD, ¶P<0.05 vs. WT-C, *P<0.05 vs. G4+/− C), and CRL (data not shown) but not placental weight (data not shown) independent of maternal genotype. Maternal BW, liver, heart, and visceral fat pad weights did not differ between groups (data not shown). HFD was associated with an increased liver/BW ratio in WT compared to G4+/− mice (0.036 ± 0.001, 0.042 ± 0.002, 0.039 ± 0.003, 0.035 ± 0.003 g/g, WT C, G4+/− C, WT HFD, G4+/− HFD respectively, P<0.05).
Exposure to HFD IU decreased fetal growth but not litter size suggesting that decreased pup number in HFD IU litters is due to postnatal mortality (Table 2).
WT HFD mothers exhibit increased expression of genes associated with hepatic lipogenesis
Expression of was increased 94% in WT HFD livers compared with WT C. No differences in expression of the PPARα target genes MCAD and LCAD, key enzymes involved in the oxidation of medium and long chain fatty acids, was observed (data not shown). Expression of peroxisome proliferator activated receptor γ coactivator-1-β (PGC1-β) and sterol regulatory element binding protein 1-c (SREBP-1c), key regulators of hepatic lipogenesis, were increased 112 and 127% respectively in WT HFD compared with WT C livers. Expression of fatty acid binding protein 1 (L-FABP1), involved in fatty acid uptake and utilization, was increased 63% in WT HFD livers compared with WT C. No significant alterations in gene expression were seen in G4+/− livers, suggesting that G4+/− mice were resistant to the effects of HFD to induce lipogenic gene expression (Figure 3). Increased lipogenesis in WT HFD livers may explain why only WT HFD developed altered lipid profile.
Figure 3.
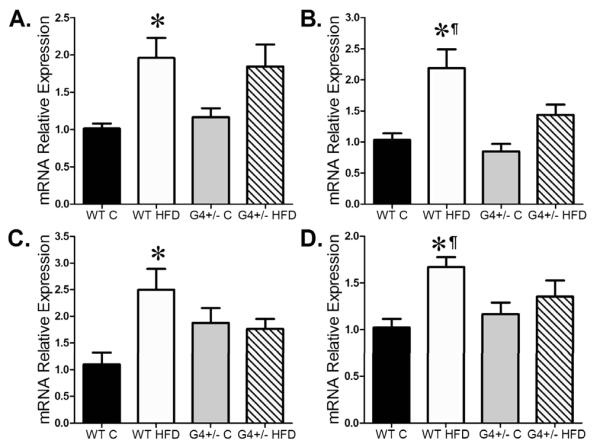
Maternal Hepatic Gene Expression. (A) PPARα, (B) PGC1β, (C) SREBP1-c and (D) L-FABP1. 5-6 mice/ group. * P<0.05 vs. WT-C.
Offspring BW and composition is determined by diet and maternal genotype
Male mice born to WT HFD IU/L mothers caught-up to C IU/L, in contrast, male mice from G4+/− HFD IU/L mothers did not experience catch-up growth (Figure 4A). HFD IU/L was associated with decreased numbers of pups/litter compared to C diet although similar to birth data it reached significance in WT HFD IU/L mothers (11±1, 6±1, 11±1, 8±1 average number of pups/litter in WT C vs. WT HFD vs. G4+/− C, vs. G4+/− HFD IU/L, p<0.01). No difference in BW and growth rate was found in female offspring, suggesting that catch-up growth in male offspring born to a WT HFD IU/L mother is not a result of decreased litter size (Figure 4B).
Figure 4.

Effect of IU/L Diet and Maternal Genotype on BW of (A) Male and (B) Female Offspring. BW was determined weekly until 12 weeks of age. Growth curves of WT offspring of WT C (black circles), WT HFD (white circles), G4+/− C (black squares), and G4+/− HFD (white squares) mothers. n=4-11 mice randomly selected from 3-8 litters per group, where more than one mouse/litter was represented the average pup weight/ litter was used. * P<0.05 vs. WT C, § P<0.05 vs. WT HFD, ¶ P<0.05 vs. G4+/− C.
Adiposity was not different in male offspring of WT and G4+/− C IU/L mothers (0.21±0.02 vs. 0.17 ± 0.01%, WT C IU/L, G4+/− C IU/L). In contrast, male offspring from WT HFD IU/L mothers exhibit increased adiposity compared to mice from G4+/− HFD IU/L mothers (0.28 ± 0.01 vs. 0.17 ± 0.01%, WT HFD IU/L vs. G4+/− HFD IU/L, P<0.0001). Female offspring of G4+/− HFD IU/L mothers exhibited the greatest adiposity (0.13 ± 0.01, 0.14 ± 0.01, 0.15 ± 0.02, 0.20 ± 0.02%, WT C IU/L, G4+/− C IU/L, WT HFD IU/L, G4+/− HFD IU/L, respectively, P=0.054,). Thus, in male offspring exposed to HFD IU/L catch-up growth is accompanied by increased fat accumulation.
Increased fat mass in WT HFD IU/L offspring is not accompanied by increased food intake
Daily food intake in 8-9 week old male mice was not significantly different between the groups (0.44 ± 0.02, 0.49 ± 0.02, 0.48 ± 0.03, 0.46 ± 0.02 kcal/day/g BW, WT C IU/L, G4+/− C IU/L, WT HFD IU/L, G4+/− HFD IU/L, respectively). Similar data was obtained in female mice (data not shown). Thus, food intake after the period of catch-up growth is not different between groups.
Increased adiposity was associated with decreased insulin action and glucose disposal
No difference in GTT or ITT was observed in male offspring exposed to C IU/L. In contrast, male offspring of WT HFD IU/L mothers had decreased glucose disposal (Figure 5A) and insulin sensitivity compared to WT C IU/L (Figure 5B). Baseline glucose levels were not significantly different between male groups for the GTT (161 ± 9, 135 ± 16, 142 ± 6 and 141 ± 12 mg/dl, WT C IU/L, G4+/− C IU/L, WT HFD IU/L and G4+/− HFD IU/L respectively) or ITT (221 ± 10, 189 ± 16, 193 ± 10 and 196 ± 12 mg/dl, WT C IU/L, G4+/− C IU/L, WT HFD IU/L and G4+/− HFD IU/L respectively). No difference in GTT or ITT was observed in female offspring (Figures 5C and 5D respectively). Baseline glucose levels were not significantly different between female groups for the GTT (77 ± 7, 91 ± 3, 95 ± 12 and 93 ± 4 mg/dl, WT C IU/L, G4+/− C IU/L, WT HFD IU/L and G4+/− HFD IU/L respectively) or ITT (144 ± 11, 145 ± 6, 147 ± 7 and 151 ± 8 mg/dl, WT C IU/L, G4+/− C IU/L, WT HFD IU/L and G4+/− HFD IU/L respectively). Increased adiposity in male offspring of WT HFD IU/L mothers was associated with glucose intolerance and insulin resistance.
Figure 5.
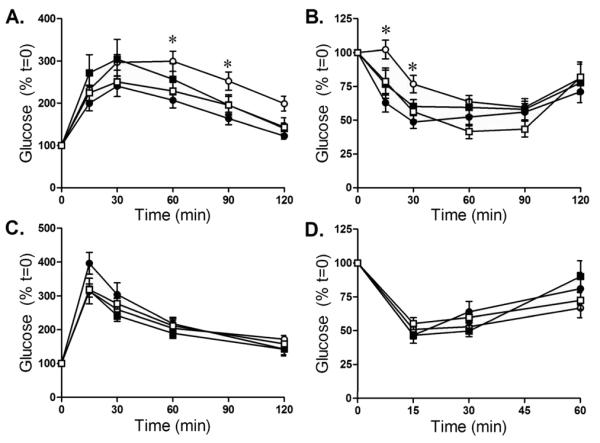
GTT and ITT in (A and B) Male and (C and D) Female Offspring. GTT and ITT were performed on age and sex matched 8-12 week old male and female WT offspring of WT C (black circles), WT HFD (white circles), G4+/− C (black squares) and G4+/− HFD (white squares) mice as described in the Methods section. Data is expressed as a % of time=0, n=5 mice randomly selected from 2-4 litters per group, * P<0.05 vs. WT C.
DISCUSSION
These studies were performed to determine the effect of an altered maternal metabolic milieu during pregnancy on programming of offspring metabolic phenotype. G4+/− female mice are insulin resistant, and exhibit enhanced lipid clearance, suggesting that deletion of GLUT4 results in a metabolic remodeling of liver and muscle substrate utilization similar to the GLUT4 knockout model (9). In WT female mice acute (2 weeks) HFD did not cause a significant change in insulin action but did increase NEFA and glycerol levels without altering TG levels as previously described (18), suggesting that 2 weeks on HFD is adequate to alter serum lipids but not insulin sensitivity. It is possible that the lack of significant effect of HFD on insulin action seen in WT female mice will be secondary to the sample size (n=5-7/group). However, it is unlikely because a similar sample size was able to successfully detect significant differences in clamp studies.
In contrast, G4+/− HFD exhibit enhanced lipid clearance contributing to their normal lipid profile. G4+/− HFD exhibit hepatic gene expression similar to G4+/− C mice, while WT HFD female mice had increased expression of PGC1-β and SREBP-1c (19). Differences in hepatic gene expression may explain, in part, the difference in the phenotype between WT and G4 +/− mice in response to HFD.
Decreased fetal weight and birth weight observed with HF exposure may be related to decreased food intake and BW gain during gestation (20,21). In humans the critical period of maternal weight gain in determining birth weight is the second trimester (22). Decreased fetal weight in mice exposed to diets differing in fatty acid and carbohydrate content have been reported in some studies (20,23) but not others (21). Fetal overgrowth in response to chronic maternal HFD is often accompanied by increased maternal adiposity (24). In our model, acute HFD did not alter maternal BW, allowing us to investigate the effects of altered circulating substrates without the confounding effect of maternal obesity. In agreement with human data, decreased BW gain in the latter part of pregnancy was accompanied by decreased fetal and pup weight.
Fetal growth is regulated by interactions between mother, placenta, and fetus (25,26). Alterations in maternal environment may affect placental structure, decreased uterine blood flow, nutrient transport, epigenetic modification of genes, and increased oxidative stress triggering a fetal maladaptive response (27). In addition, fetal growth can be secondary to alterations in glucose transport. In our model, decreased GLUT4 expression is unlikely to be the cause of altered fetal growth because maximal fetal growth is attained during the second and third trimesters (22), while GLUT4 expression has been found in the syncytiotrophoblast during first trimester (28). Further, HFD decreased fetal BW independent of maternal genotype.
Finally, decreased fetal BW could be secondary to decreased protein intake (29). Protein restriction, as a model of fetal programming, use at least a 50% reduction in protein intake (29). In our model, total protein consumption during pregnancy was not different among groups suggesting that protein restriction is not responsible for decreased fetal weight. Low birth weight followed by rapid weight gain during early postnatal life “catch-up growth” has been associated with increased long-term risks for the metabolic syndrome (30,31). Catch-up growth was observed in male offspring of WT, but not G4+/− HFD mothers. Low birth weight followed by rapid weight gain during early postnatal life “catch-up growth” has been associated with increased long-term risks for the metabolic syndrome (30,31). Catch-up growth was observed in male offspring of WT, but not G4+/− HFD mothers. Catch-up growth in male offspring of WT HFD offspring is unlikely to be the result of decreased litter size. The difference in litter size among the groups was an average of 3 pups per litter; such a difference has not been shown to cause any metabolic alteration later in life. Litter size has to be substantially reduced to 3-4 pups per litter to produce metabolic syndrome later in life (32,33).
Since the aim of the current study was looking at HFD exposure during pregnancy and lactation, not the effect of overfeeding during lactation, we feel that not culling was an appropriate strategy. In addition, male offspring of G4+/− HFD did not exhibit catch-up growth despite having a similar litter size to WT HFD, suggesting that differences in litter size do not explain the difference in growth rate between offspring from WT and G4+/− HFD mothers.
Animals that experienced catch-up growth had increased adiposity and exhibited impaired glucose tolerance and insulin sensitivity. Male offspring from G4+/− HFD IU/L mothers did not exhibit catch-up growth and exhibit normal glucose tolerance and insulin action. Thus, differences in maternal substrate utilization may be the reason why male offspring did or did not develop metabolic abnormalities.
We found a sexually dimorphic response to the same prenatal insult. Sex differences are observed in the pathophysiological response to an adverse fetal environment (34,35). The role of sex hormones and chromosomes, and the regulatory pathways of sexual differentiation may explain the sexual dimorphism seen in fetal programming. Female mice exposed to HFD IU/L have a normal metabolic response when weaned onto a standard chow diet. However, it is not clear how they will respond to an adverse environment.
We chose a diet relevant to Western Societies, where fast food is increasingly popular. In pregnancy, two major dietary patterns are defined: processed meat and high-fat dairy; or vegetables, fruits, poultry and fish. Diets based on processed meat and high-fat are associated with fetal growth restriction (36). One limitation of our study is that it does not discriminate between the specific components of the diet, or address the role of the suckling period. Further studies are warranted to identify specific macro-, or micronutrients as well as the timing of insult that may underlie these associations.
In conclusion, HFD during pregnancy resulted in metabolic syndrome in male WT offspring of WT mothers. In contrast, offspring of G4+/− HFD mothers appeared to be protected, perhaps due to the altered substrate utilization of G4+/− HFD mothers. Our novel mouse model offers the potential for further studies into the effects of maternal substrate utilization in response to different diets, on placental function, fetal growth, and metabolic function in the offspring. Future studies will provide additional information on the maternal factors and the critical period in development that determine susceptibility to metabolic syndrome in adulthood.
Acknowledgments
The authors wish to thank Dr. Ellen Katz for many helpful discussions and for assistance in revising this manuscript. We also thank the Diabetes Research and Training Center, Albert Einstein College of Medicine for help with the ECHO MRI and LINCOPLEX analysis.
Financial Support: This work was supported by grants from the National Institutes of Health R01DK47425, R01HL73163, R01HL58119, R21 DK081194, P50 DK051296, the Diabetes Research and Training program P60-DK020541, and Cancer Centers of Albert Einstein College of Medicine (MJC) and KO8 HD042172 and an Independent Research Award from Pfizer Inc. (PV). KH was supported by a Mentor-Based Postdoctoral Fellowship awarded to MJC from the American Diabetes Association.
Abbreviations
- BW
body weight
- C
control breeding chow
- CRL
crown-rump length
- e
embryonic day
- G4+/−
heterozygous deletion of glucose transporter 4
- GLUT4
glucose transporter 4
- GTT
glucose tolerance test
- HFD
high fat diet
- ITT
insulin tolerance test
- IU
In Utero
- L
lactation
- T2DM
type 2 diabetes mellitus
- TG
triglycerides
REFERENCES
- 1.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 2.Seidell JC. Obesity, insulin resistance and diabetes--a worldwide epidemic. Br J Nutr. 2000;83:S5–S8. doi: 10.1017/s000711450000088x. [DOI] [PubMed] [Google Scholar]
- 3.Hales CN, Barker DJ. The thrifty phenotype hypothesis. Br Med Bull. 2001;60:5–20. doi: 10.1093/bmb/60.1.5. [DOI] [PubMed] [Google Scholar]
- 4.Kral JG. Preventing and treating obesity in girls and young women to curb the epidemic. Obes Res. 2004;12:1539–1546. doi: 10.1038/oby.2004.193. [DOI] [PubMed] [Google Scholar]
- 5.Saldana TM, Siega-Riz AM, Adair LS. Effect of macronutrient intake on the development of glucose intolerance during pregnancy. Am J Clin Nutr. 2004;79:479–486. doi: 10.1093/ajcn/79.3.479. [DOI] [PubMed] [Google Scholar]
- 6.Scholl TO, Leskiw M, Chen X, Sims M, Stein TP. Oxidative stress, diet, and the etiology of preeclampsia. Am J Clin Nutr. 2005;81:1390–1396. doi: 10.1093/ajcn/81.6.1390. [DOI] [PubMed] [Google Scholar]
- 7.Taylor PD, Poston L. Developmental programming of obesity in mammals. Exp Physiol. 2007;92:287–298. doi: 10.1113/expphysiol.2005.032854. [DOI] [PubMed] [Google Scholar]
- 8.Symonds ME, Budge H. Nutritional models of the developmental programming of adult health and disease. Proc Nutr Soc. 2009;68:173–178. doi: 10.1017/S0029665109001049. [DOI] [PubMed] [Google Scholar]
- 9.Ranalletta M, Jiang H, Li J, Tsao TS, Stenbit AE, Yokoyama M, Katz EB, Charron MJ. Altered hepatic and muscle substrate utilization provoked by GLUT4 ablation. Diabetes. 2005;54:935–943. doi: 10.2337/diabetes.54.4.935. [DOI] [PubMed] [Google Scholar]
- 10.Stenbit AE, Tsao TS, Li J, Burcelin R, Geenen DL, Factor SM, Houseknecht K, Katz EB, Charron MJ. GLUT4 heterozygous knockout mice develop muscle insulin resistance and diabetes. Nat Med. 1997;3:1096–1101. doi: 10.1038/nm1097-1096. [DOI] [PubMed] [Google Scholar]
- 11.Rossetti L, Stenbit AE, Chen W, Hu M, Barzilai N, Katz EB, Charron MJ. Peripheral but not hepatic insulin resistance in mice with one disrupted allele of the glucose transporter type 4 (GLUT4) gene. J Clin Invest. 1997;100:1831–1839. doi: 10.1172/JCI119711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petry CJ, Ong KK, Dunger DB. Does the fetal genotype affect maternal physiology during pregnancy? Trends Mol Med. 2007;13:414–421. doi: 10.1016/j.molmed.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Katz EB, Stenbit AE, Hatton K, DePinho R, Charron MJ. Cardiac and adipose tissue abnormalities but not diabetes in mice deficient in GLUT4. Nature. 1995;377:151–155. doi: 10.1038/377151a0. [DOI] [PubMed] [Google Scholar]
- 14.Vuguin P, Raab E, Liu B, Barzilai N, Simmons R. Hepatic insulin resistance precedes the development of diabetes in a model of intrauterine growth retardation. Diabetes. 2004;53:2617–2622. doi: 10.2337/diabetes.53.10.2617. [DOI] [PubMed] [Google Scholar]
- 15.Capozza F, Combs TP, Cohen AW, Cho YR, Park SY, Schubert W, Williams TM, Brasaemle DL, Jelicks LA, Scherer PE, Kim JK, Lisanti MP. Caveolin-3 knockout mice show increased adiposity and whole body insulin resistance, with ligand-induced insulin receptor instability in skeletal muscle. Am J Physiol Cell Physiol. 2005;288:C1317–C1331. doi: 10.1152/ajpcell.00489.2004. [DOI] [PubMed] [Google Scholar]
- 16.van de Wall E, Leshan R, Xu AW, Balthasar N, Coppari R, Liu SM, Jo YH, MacKenzie RG, Allison DB, Dun NJ, Elmquist J, Lowell BB, Barsh GS, de Luca C, Myers MG, Jr, Schwartz GJ, Chua SC., Jr Collective and individual functions of leptin receptor modulated neurons controlling metabolism and ingestion. Endocrinology. 2008;149:1773–1785. doi: 10.1210/en.2007-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ranalletta M, Du XQ, Seki Y, Glenn AS, Kruse M, Fiallo A, Estrada I, Tsao TS, Stenbit AE, Katz EB, Charron MJ. Hepatic response to restoration of GLUT4 in skeletal muscle of GLUT4 null mice. Am J Physiol Endocrinol Metab. 2007;293:E1178–E1187. doi: 10.1152/ajpendo.00628.2006. [DOI] [PubMed] [Google Scholar]
- 18.Biddinger SB, Almind K, Miyazaki M, Kokkotou E, Ntambi JM, Kahn CR. Effects of diet and genetic background on sterol regulatory element-binding protein-1c, stearoyl-CoA desaturase 1, and the development of the metabolic syndrome. Diabetes. 2005;54:1314–1323. doi: 10.2337/diabetes.54.5.1314. [DOI] [PubMed] [Google Scholar]
- 19.Lin J, Yang R, Tarr PT, Wu PH, Handschin C, Li S, Yang W, Pei L, Uldry M, Tontonoz P, Newgard CB, Spiegelman BM. Hyperlipidemic effects of dietary saturated fats mediated through PGC-1beta coactivation of SREBP. Cell. 2005;120:261–273. doi: 10.1016/j.cell.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 20.Siemelink M, Verhoef A, Dormans JA, Span PN, Piersma AH. Dietary fatty acid composition during pregnancy and lactation in the rat programs growth and glucose metabolism in the offspring. Diabetologia. 2002;45:1397–1403. doi: 10.1007/s00125-002-0918-2. [DOI] [PubMed] [Google Scholar]
- 21.Srinivasan M, Katewa SD, Palaniyappan A, Pandya JD, Patel MS. Maternal high-fat diet consumption results in fetal malprogramming predisposing to the onset of metabolic syndrome-like phenotype in adulthood. Am J Physiol Endocrinol Metab. 2006;291:E792–E799. doi: 10.1152/ajpendo.00078.2006. [DOI] [PubMed] [Google Scholar]
- 22.Sekiya N, Anai T, Matsubara M, Miyazaki F. Maternal weight gain rate in the second trimester are associated with birth weight and length of gestation. Gynecol Obstet Invest. 2007;63:45–48. doi: 10.1159/000095286. [DOI] [PubMed] [Google Scholar]
- 23.Taylor PD, Khan IY, Lakasing L, Dekou V, O’Brien-Coker I, Mallet AI, Hanson MA, Poston L. Uterine artery function in pregnant rats fed a diet supplemented with animal lard. Exp Physiol. 2003;88:389–398. doi: 10.1113/eph8802495. [DOI] [PubMed] [Google Scholar]
- 24.Jones HN, Woollett LA, Barbour N, Prasad PD, Powell TL, Jansson T. High-fat diet before and during pregnancy causes marked up-regulation of placental nutrient transport and fetal overgrowth in C57/BL6 mice. FASEB J. 2009;23:271–278. doi: 10.1096/fj.08-116889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luther J, Aitken R, Milne J, Matsuzaki M, Reynolds L, Redmer D, Wallace J. Maternal and fetal growth, body composition, endocrinology, and metabolic status in undernourished adolescent sheep. Biol Reprod. 2007;77:343–350. doi: 10.1095/biolreprod.107.061440. [DOI] [PubMed] [Google Scholar]
- 26.Remacle C, Bieswal F, Reusens B. Programming of obesity and cardiovascular disease. Int J Obes Relat Metab Disord. 2004;28:S46–S53. doi: 10.1038/sj.ijo.0802800. [DOI] [PubMed] [Google Scholar]
- 27.Jansson T, Powell TL. Role of the placenta in fetal programming: underlying mechanisms and potential interventional approaches. Clin Sci (Lond) 2007;113:1–13. doi: 10.1042/CS20060339. [DOI] [PubMed] [Google Scholar]
- 28.Ericsson A, Hamark B, Powell TL, Jansson T. Glucose transporter isoform 4 is expressed in the syncytiotrophoblast of first trimester human placenta. Hum Reprod. 2005;20:521–530. doi: 10.1093/humrep/deh596. [DOI] [PubMed] [Google Scholar]
- 29.Vuguin PM. Animal Models for Small for Gestational Age and Fetal Programing of Adult Disease. Horm Res. 2007;68:113–123. doi: 10.1159/000100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Blasio MJ, Gatford KL, Robinson JS, Owens JA. Placental restriction of fetal growth reduces size at birth and alters postnatal growth, feeding activity, and adiposity in the young lamb. Am J Physiol Regul Integr Comp Physiol. 2007;292:R875–R886. doi: 10.1152/ajpregu.00430.2006. [DOI] [PubMed] [Google Scholar]
- 31.Crowther NJ, Cameron N, Trusler J, Toman M, Norris SA, Gray IP. Influence of catch-up growth on glucose tolerance and beta-cell function in 7-year-old children: results from the birth to twenty study. Pediatrics. 2008;121:e1715–e1722. doi: 10.1542/peds.2007-3147. [DOI] [PubMed] [Google Scholar]
- 32.Rodrigues AL, de Moura EG, Passos MC, Dutra SC, Lisboa PC. Postnatal early overnutrition changes the leptin signaling pathway in the hypothalamus-pituitary-thyroid axis of young and adult rats. J Physiol. 2009;587:2647–2661. doi: 10.1113/jphysiol.2009.169045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt I, Fritz A, Scholch C, Schneider D, Simon E, Plagemann A. The effect of leptin treatment on the development of obesity in overfed suckling Wistar rats. Int J Obes Relat Metab Disord. 2001;25:1168–1174. doi: 10.1038/sj.ijo.0801669. [DOI] [PubMed] [Google Scholar]
- 34.Mueller BR, Bale TL. Sex-specific programming of offspring emotionality after stress early in pregnancy. J Neurosci. 2008;28:9055–9065. doi: 10.1523/JNEUROSCI.1424-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vige A, Gallou-Kabani C, Junien C. Sexual dimorphism in non-Mendelian inheritance. Pediatr Res. 2008;63:340–347. doi: 10.1203/PDR.0b013e318165b896. [DOI] [PubMed] [Google Scholar]
- 36.Knudsen VK, Orozova-Bekkevold IM, Mikkelsen TB, Wolff S, Olsen SF. Major dietary patterns in pregnancy and fetal growth. Eur J Clin Nutr. 2008;62:463–470. doi: 10.1038/sj.ejcn.1602745. [DOI] [PubMed] [Google Scholar]


