Abstract
The scientific discovery of novel training paradigms has yielded better understanding of basic mechanisms underlying cortical plasticity, learning and development. This study is a first step in evaluating Tai Chi (TC), the Chinese slow-motion meditative exercise, as a training paradigm that, while not engaging in direct tactile stimulus training, elicits enhanced tactile acuity in long-term practitioners, The rationale for this study comes from the fact that, unlike previously studied direct-touch tactile training paradigms, TC practitioners focus specific mental attention on the body’s extremities including the fingertips and hands as they perform their slow routine.
To determine whether TC is associated with enhanced tactile acuity, experienced adult TC practitioners were recruited and compared to age-gender matched controls. A blinded assessor used a validated method (Van Boven, Hamilton, Kauffman, Keenan, & Pascual-Leone, 2000) to compare TC practitioners’ and controls’ ability to discriminate between two different orientations (parallel and horizontal) across different grating widths at the fingertip. Study results showed TC practitioners’ tactile spatial acuity was superior to that of the matched controls (p<.04). There was a trend showing TC may have an enhanced effect on older practitioners (p<.066), suggesting TC may slow age related decline in this measure. To the best of our knowledge, this is the first study to evaluate a long-term attentional practice’s effects on a perceptual measure. Longitudinal studies are needed to examine whether TC initiates or is merely correlated with perceptual changes and whether it elicits long-term plasticity in primary sensory cortical maps. Further studies should also assess whether related somatosensory attentional practices (such as Yoga, mindfulness meditation and Qigong) achieve similar effects.
Keywords: touch, tactile acuity, Tai Chi, attention, aging
BACKGROUND
In numerous experimental studies in humans and non-human primates, training in sensory tasks has produced gains in acuity associated with changes in low-level sensory cortical maps (Crist, Kapadia, Westheimer, & Gilbert, 1997; G. Recanzone, Merzenich, MM, Jenkins, WM, Grajski, KA, Dinse, HR, 1992; G. H. Recanzone, Schreiner, & Merzenich, 1993; Sathian & Zangaladze, 1997; Schoups, Vogels, Qian, & Orban, 2001; Wright & Sabin, 2007). Less common are studies showing that self-initiated long-term sensory training practices such as Braille and musical training may also produce perceptual learning: blind Braille readers perform at a higher level than normals in a tactile grating orientation task; musicians perform better at 2-point discrimination (Ragert, Schmidt, Altenmuller, & Dinse, 2004; Van Boven et al., 2000)..
Top-down attentional processes exert control over training-based improvements in performance in low-level perceptual tasks (Ahissar, 1993). Attentional focus increases the efficacy of auditory, visual, and tactile perceptual training regimens through top-down cortical regulation (Seitz & Dinse, 2007). Only recently have investigators begun to evaluate whether attentional training alone, in the absence of directly applied sensory stimuli, can elicit gains in a measure of low-level perception. One multi-session experimental study found that visual attentional training carried out with only minimal use of a directly targeted visual stimulus enhanced visual spatial acuity (Dupuis-Roy & Gosselin, 2007). To our knowledge, no study has assessed whether long-term training in a sensory attentional practice carried out in the absence of a direct stimulus training regimen effects changes in a measure of low level sensory perception.
The rationale for investigating TC is that, unlike previously studied paradigms, it does not use a direct sensory stimulus training regimen. Instead, without engaging in direct tactile training, TC practitioners learn a meditative slow motion exercise routine known as the Tai Chi form (in this case, the “wu-style” form). They also spend significant time in class and at home performing adjunctive practices, especially static standing meditation postures (which can be thought of as analogous to the weight training regimens or repetitive drills used by athletes to improve performance in sports such as golf and tennis). The stated goal of these exercises is to teach practitioners to perceive how the body feels “from the inside out.” To facilitate this goal of body awareness, during both the Tai Chi form and adjunctive meditative practice, practitioners are encouraged to focus attention on the extremities including the fingertips as a method for cultivating the ability to sense the entire body, from the core to the extremes. By focusing somatosensory attention on nearly in-detectible feelings in the palms and fingertips (while the eyes are gazing in an unfocused, relaxed manner at a point several feet in front of the practitioner, not looking directly at the fingers or hands), practitioners report being able to sense how a feeling in the palm or fingertip may be related to feelings in the rest of the body; in this manner, the practice is said to cultivate a real-time relaxed sense of whole body awareness. Frantzis (1993; 2006) offers an in-depth description of the practice studied here
The main goal of this study is to discover whether practitioners’ specific attention to the body’s extremities, including the fingertips, as they perform their slow-motion and static meditative exercises produces enhanced tactile spatial acuity in the absence of any direct touch-based tactile training.
Because tactile spatial acuity has been strongly associated with cortical plasticity in primary somatosensory cortex and other early sensory maps, any differences observed should be reflected in sensory cortical measures. The specific measure studied here, tactile spatial acuity at the fingertip, is correlated with cortical measures [see especially, remodeling of primary sensory maps as reported by Hodzic and colleagues (2004) and by Sathian and colleagues (2002)]. More generally, it is known that short-term attentional focus on the fingers facilitates changes in S1 cortical somatotopic map (Braun et al., 2002; Noppeney, Waberski, Gobbele, & Buchner, 1999). A positive finding would suggest that practitioners’ long-term focus of a specific attentional “spotlight” on the fingertips increases the gain of neuronal responses (e.g., amplifies the attended inputs) and evokes cortical remodeling in early sensory maps.
An alternative to the view that TC works as an attentional practice via a cortical mechanism merits consideration: if TC elicits changes in tactile acuity, it may do so through its role as a non-specific slow-motion, low-intensity exercise that increases peripheral blood flow. In this case, tactile acuity should be associated with cumulative lifetime and/or current intensity of exercise in both the TC group and the control group since exercise is a potent modulator of peripheral blood flow (although a null correlation between exercise and tactile acuity has been previously reported (Stevens, Alvarez-Reeves, Mack, & Green, 2003).
TC, tactile acuity, and aging
A secondary aim in this study is to compare the effects of TC in younger versus older practitioners. The rationale for this aim comes from three sets of observations: (1) Tactile acuity declines sharply with age. (2) TC has demonstrated beneficial effects on age-related changes in the sensorimotor system including falls and fall risk (Wolf et al., 2003). (3) ) Tactile acuity in the elderly may be associated with factors related to fall risk including the ability to stabilize balance when it is perturbed by using a steadying light touch as the fingertip contributes sensory signals that improve balance (Lackner, Rabin, & DiZio, 2001). A positive finding would suggest that older TC practitioners who retain tactile acuity at the fingertip may be able to use light touch more effectively for stabilization and would thus be less susceptible to falling (Tremblay, Mireault, Dessureault, Manning, & Sveistrup, 2004, 2005).
METHODS
Participants
14 TC practitioners were recruited from a local TC studio (Brookline TC) where instruction is offered in a standardized curriculum. 14 control participants were recruited from the community and matched for gender and age (+/− 2 years). In both groups, exclusion criteria included factors known to elicit changes in tactile acuity: calluses at the test site (the right index finger), dyslexia, blindness, history of rheumatologic disorder, neurological disorder, or recent trauma to the right upper extremity. To qualify for the TC subject group, practitioners were required to have studied TC for over two years with an average of at least 3 sessions per week with each session lasting 40 minutes or more. The study was approved by the Beth Israel Deaconess Medical Center Internal Review Board and took place at the General Clinical Research Center; informed consent was received from all study participants.
Design and procedure
The tactile spatial acuity threshold was determined by carrying out a Grating Orientation Test (GOT) of the right index finger in a testing session lasting approximately 20 minutes using procedures as described by Van Boven (Van Boven et al., 2000; Van Boven & Johnson, 1994). The study was designed so that the tester responsible for all of the assessments was blinded to whether a subject was a TC practitioner or control: the unblinded research assistant (AK) or the principal investigator (CK) arranged the subject’s appointment, greeted the subject (with the reminder that the subject was not to unblind the tester as to whether he/she was a Tai Chi practitioner) and led the subject to the area where the blinded tester carried out the test. Participants were tested in a quiet room with the hand resting comfortably in a supine position. The fingernail of the index finger was affixed to a stable surface held by double-sided adhesive tape. Each subject was blindfolded. A series of grooved dome shaped pieces of plastic (JVP tactile domes, Stoelting Company [Wood Dale, IL]) were presented to the subject’s fingertip. Each dome was presented 20 times to the subject with either a parallel or perpendicular orientation;, resulting in 10 presentations at each orientation given in pseudorandom order (using MATLAB random number generator). The dome was applied for up to 2.5 seconds with a forced-choice protocol as participants identified the grating orientation as either parallel or perpendicular. Domes were manually administered with even, consistent moderate force that was judged by the participant to be comfortable and painless: during training the tester was taught to deliver more than 50 gms of force; 30 validation trials were performed (using a Salter-Brecknell scale) under true testing conditions (eg., test subject was blindfolded and performed the discrimination task) while tester was kept blind to force measures that were recorded by an RA who was otherwise not connected with the study. Across two different subjects, only one trial (3.3%) fell below the 50g of force threshold under which tactile grating orientation becomes sensitive to variations of force (Gibson & Craig, 2006). The tester was careful to monitor finger movement and trials contaminated by finger movement were rejected. The testing session began with a thorough 10–15 minute orientation and training in the tactile protocol as subjects were tested on the largest dome slowly with clear feedback about whether their responses were correct. The purpose of this familiarization procedure was to ensure that subjects understood the task clearly before beginning the formal test procedure. The actual test of the right index finger began with the largest grating width (3.0 mm) for 20 trials per grating width and continued with decreasing grating widths (2.0, 1.5, 1.2, 1.0, .75, .5, .35) until the subject could no longer perceive the grating orientation at which point the test was discontinued. Each participant’s threshold was identified as the grating width at which they correctly perceived 75% of trials so that the threshold is halfway between 100% accuracy and 50% accuracy (i.e., chance). If the 75% threshold (5 incorrect responses) occurred between two dome grating widths, the two groove widths spanning the 75% response were interpolated. If a participant scored less than 75% correctly with the widest grating, the threshold was taken to be 3.00 mm.
Statistical analysis
The primary aim was to compare mean tactile acuity between groups. A secondary aim was to evaluate the strength of the effect of TC across different age groups, since age is known to exert strong negative effects on tactile acuity. A 2-way ANOVA allowed the evaluation of (1) main effects for TC, and AGE (2) interactive effect of TC × AGE.
RESULTS
Background and demographics
14 age-gender matched pairs were recruited (10 female pairs, 28 –68 years; average = 53.3 years). There were only very minor differences in the demographics of race or ethnicity between the two groups (TC: 13 Caucasians, 1 Asian-American Control: 11 Caucasians, 2 Asian-Americans, 1 African American). There was no significant difference in incomes (TC: average income = 53, 860 USD; Control: 48, 125 USD; 2 tailed t test p<.53). There was a trend towards a difference between TC and control in education (2-tailed t test, p<.07) with members of both groups, on average, completing at least a 4-year college degree (TC: 5.9; Control: 5.1. 5 = 4 year college graduate; 6 = Professional training beyond college). Ages of practitioners and normal controls were successfully matched to within 24 months (mean age difference= 14.4 months, SD= 5.23 months). TC practitioners: mean rate of practice = 7.25 hours/week (range = 2.5–15.8 hours/week); mean hours of lifetime practice = 2957 (range = 718–7576 hours)
Main study outcomes
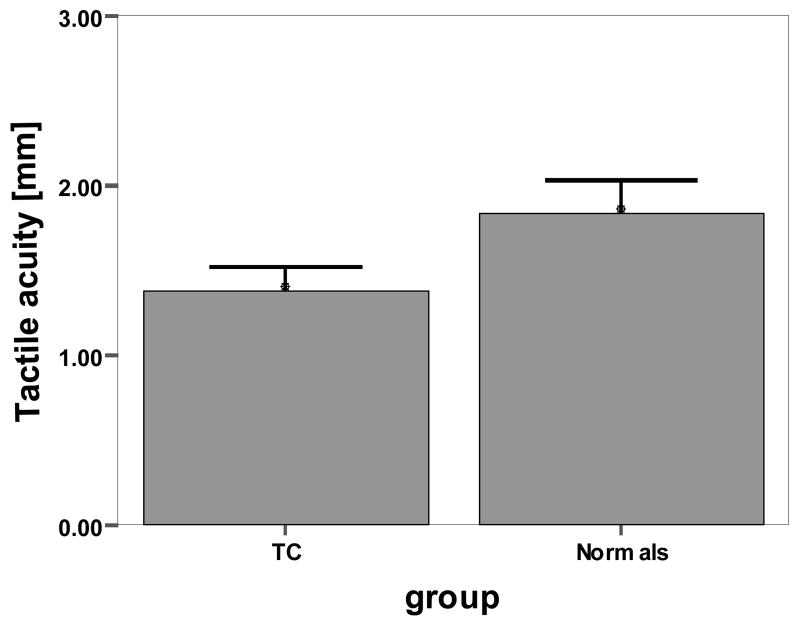
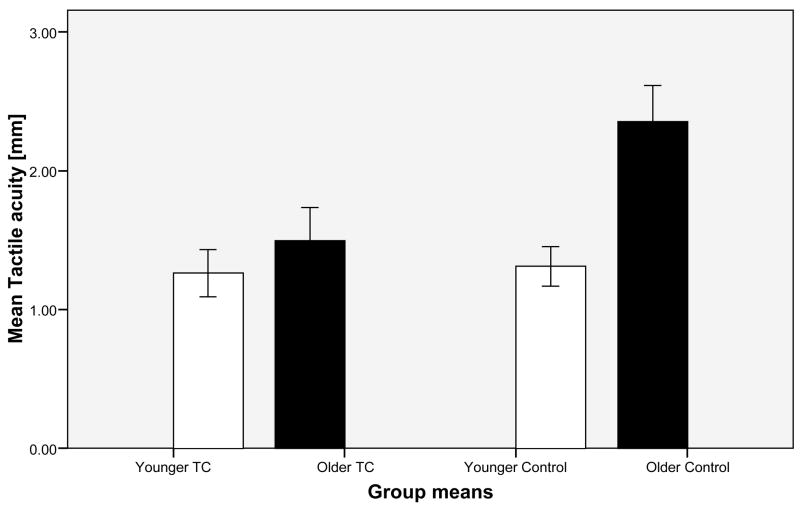
A 2×2 ANOVA was conducted with treatment group (14 TC subjects vs. 14 controls) and age (14 older subjects vs. 14 younger subjects as defined by a median split) as the independent variables and tactile acuity as the dependent variable. As predicted, there was a significant main effect for group (F(1,24) = 4.67, p = .04), with the TC group showing greater tactile acuity than the control group (1.38 vs. 1.83mm, respectively). As expected, there was also a significant main effect for age (F(1,24) = 9.3, p = .006), with the group of younger subjects (n=14) exhibiting greater tactile acuity than older subjects (n=14) regardless of their membership in either TC or control group (1.29 vs. 1.93mm, respectively). Using Cohen’s (1988) method, the standardized effect size for the main effect of TC over control was d = .68, which is conventionally deemed between a medium and large effect. For the main effect of age, the effect size was d = 1.03, which is conventionally deemed a large effect size. Finally, there was a trend toward significance for the interaction of age and treatment group (F(1,24) = 3.7, p=.066) (n=7 subjects in each subgroup [TC-younger, TC-older, Control-younger, Control-older]). The interaction trend is illustrated in Figure 1B, which shows that the effect of TC seems to be greater for older subjects as compared to younger ones.
Figure 1. Mean tactile acuity.
Figure 1A. Mean tactile acuity in TC versus Normal groups. 1.38mm vs. 1.83mm grating width (smaller represents better tactile acuity). Error bars represent 1 SEM.
Figure 1B. Mean tactile acuity of younger versus older participants in TC and normal groups (each group n=7). Error bars represent +/− 1 SEM
Effect of exercise, TC practice on tactile acuity
Regression analysis found no significant effect of exercise (measured in hours/week) on tactile acuity (beta=−.189, p=.411) across the entire sample. The study also found no effect of TC practice (measured in hours/week), on tactile acuity in TC practitioners (beta=.391, p=.26).
DISCUSSION
In this sample, there was a main effect of TC: practitioners had significantly sharper tactile acuity than age-matched controls. There was a main effect of age: younger participants demonstrated better acuity than older participants. There was a trend towards an interactive effect, suggesting TC may have a stronger impact on acuity in older practitioners. There was no relation between current exercise and tactile acuity across the entire sample; in the TC group, there was no association between tactile acuity and cumulative amount or current intensity of TC practice. The significance of these findings is discussed below.
The failure to find an association between exercise and tactile acuity is inconsistent with the blood flow hypothesis which theorizes that TC enhances tactile acuity in a non-specific manner by increasing peripheral blood flow; this null result is in accord with a large study by Stevens et al (2003) which found both cumulative exercise and current hours-per-week to be unrelated to tactile spatial acuity.
It is less clear how to interpret the failure to find an association between TC practice variables (practice rate/week and total lifetime practice hours) and tactile acuity. On the one hand, the sample size for this test was low and the relationship was strong enough (beta = +39) that it might reach significance with a more fully powered study. On the other hand, several studies of tactile acuity in blind Braille readers have reported a similar result, finding no relationship between practice variables (e.g., being an early blind subject or being an avid present day Braille reader) and better tactile acuity (Goldreich & Kanics, 2003, 2006; Van Boven et al., 2000).
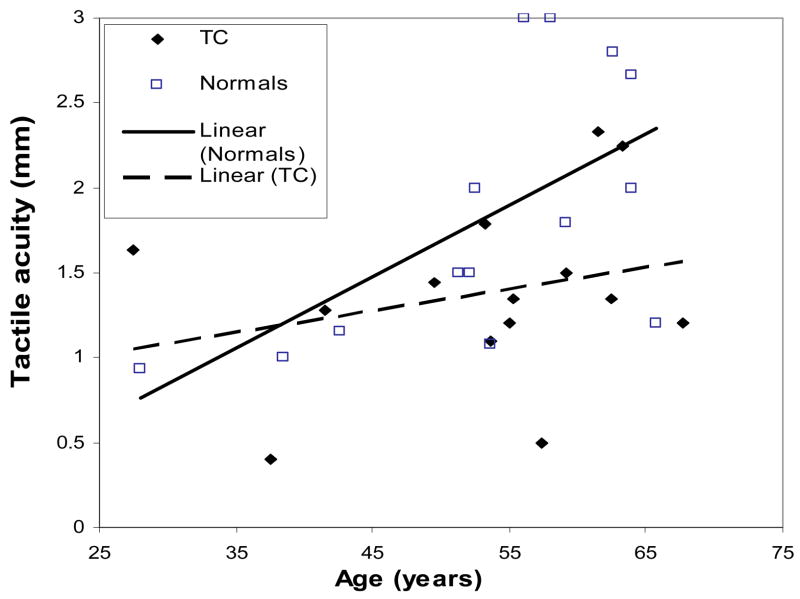
The question of whether the amount or intensity of practice leads to a better outcome is related to a larger question: in TC, what is the time course for the development of improved tactile acuity? Does change come quickly and then plateau or does it follow a more linear path? Studies of TC looking at change over time in tactile acuity (and the brain areas that subserve tactile function) will help shed light on this question. An alternative interpretation of the failure to relate TC practice variables to tactile acuity could be that enhanced acuity is associated more with age than with time spent practicing: older practitioners in this study may have experienced disproportionate benefits in tactile acuity because age-related losses of acuity in normal healthy people are so severe. TC may protect older people from this loss.
This study has important limitations. Because it is cross-sectional, we cannot draw any causal conclusions about the relationship between Tai Chi and tactile acuity. The effect could be explained by a self-selection bias: people with high tactile acuity may be drawn to Tai Chi. Further, it is plausible that this self-selection bias might be stronger in older practitioners: healthy, active people may be more likely to seek out TC practice. Several points, however, weigh against this possibility: (1) Our healthy control sample is notable for its relative physical vigor: 5/7 older control participants reported vigorous walking or fitness-related regimens (including yoga, pilates, weight training, jogging, and trampoline training). (2) Neurological, rheumatologic and other diseases that might affect tactile acuity (e.g., diabetes, peripheral neuropathy) were excluded suggesting that a pre-existing health differential between TC practitioners and controls may not account for the difference in tactile acuity.
A further limitation of this study comes from the fact that the TC practitioners studied here were only recruited from one TC school: the effects observed may be due to the particular type of TC being studied rather than to TC in general. More broadly, this study’s focus on a low level measure of sensory acuity does not rule out the possibility that in TC, complex motor processes are used to facilitate a specific attentional focus on the fingertips and a more generalized sense of body awareness. Further studies disaggregating the different mechanisms underlying TC will help address the complex sensorimotor processes that likely contribute to TC’s effects on tactile acuity.
Evidence for the validity of this data comes from the fact that the acuity thresholds observed in the control group are in line with those seen in previous published studies using the same psychophysical method (Tremblay, Wong, Sanderson, & Cote, 2003; Vega-Bermudez & Johnson, 2004). A longitudinal randomized trial could assess more definitively whether TC causes or is merely correlated with enhanced tactile acuity. Such a trial could also evaluate the effects of TC on different age groups.
This study has shown that TC, a somatosensory attentional training practice, is associated with gains in a low-level measure of sensory perception. The study found a trend showing TC may have a stronger effect on older versus younger practitioners, suggesting the practice of TC may slow age related decline in this measure. To the best of our knowledge, this is the first study to assess the effects of long-term attentional practice on a perceptual measure. Further research is needed to evaluate a possible central mechanism in TC involving somatosensory attentional modulation and long-term cortical plasticity in early sensory maps. Further studies should also assess whether related somatosensory attentional practices (such as Yoga, mindfulness meditation and Qigong) achieve similar effects.
Figure 2. The Effect of Age on Tactile Acuity.
Acknowledgments
The lead author (CK) is supported by NIH NCCAM career award K01 AT003459-01. The research was carried out at the Harvard-Thorndike General Clinical Research Center at the Beth Israel Deaconess Medical Center, which is funded by grant M01 RR01032. The authors are grateful to Christopher Moore for his mentorship and guidance, to Robert Van Boven for his technical assistance with the JVP domes, to Dan Kleiman, Alan Dougall and Marie Helene Jouvin from Brookline Tai Chi for their work in orienting the scientific team to the practice of Tai Chi, to Alfred Luk for his assistance in conducting the research, and to Christina Tognoni for her role in proofreading the manuscript.
References
- Braun C, Haug M, Wiech K, Birbaumer N, Elbert T, Roberts LE. Functional organization of primary somatosensory cortex depends on the focus of attention. Neuroimage. 2002;17(3):1451–1458. doi: 10.1006/nimg.2002.1277. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2 1988. [Google Scholar]
- Crist RE, Kapadia MK, Westheimer G, Gilbert CD. Perceptual learning of spatial localization: specificity for orientation, position, and context. J Neurophysiol. 1997;78(6):2889–2894. doi: 10.1152/jn.1997.78.6.2889. [DOI] [PubMed] [Google Scholar]
- Dupuis-Roy N, Gosselin F. Perceptual learning without signal. Vision Res. 2007;47(3):349–356. doi: 10.1016/j.visres.2006.10.016. [DOI] [PubMed] [Google Scholar]
- Frantzis B. Opening the Energy Gates of Your Body. Berkeley, California: North Atlantic Books; 1993. [Google Scholar]
- Frantzis B. Tai Chi: Health for Life. Fairfax, California: Energy Arts; 2006. [Google Scholar]
- Gibson G, Craig J. The effect of force and conformance on tactile intensive and spatial sensitivity. Exp Brain Res. 2006;170(2):172–181. doi: 10.1007/s00221-005-0200-1. [DOI] [PubMed] [Google Scholar]
- Goldreich D, Kanics IM. Tactile acuity is enhanced in blindness. J Neurosci. 2003;23(8):3439–3445. doi: 10.1523/JNEUROSCI.23-08-03439.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldreich D, Kanics IM. Performance of blind and sighted humans on a tactile grating detection task. Percept Psychophys. 2006;68(8):1363–1371. doi: 10.3758/bf03193735. [DOI] [PubMed] [Google Scholar]
- Hodzic A, Veit R, Karim AA, Erb M, Godde B. Improvement and decline in tactile discrimination behavior after cortical plasticity induced by passive tactile coactivation. Journal of Neuroscience. 2004;24(2):442–446. doi: 10.1523/JNEUROSCI.3731-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackner JR, Rabin E, DiZio P. Stabilization of posture by precision touch of the index finger with rigid and flexible filaments. Exp Brain Res. 2001;139(4):454–464. doi: 10.1007/s002210100775. [DOI] [PubMed] [Google Scholar]
- Noppeney U, Waberski T, Gobbele R, Buchner H. Spatial attention modulates the cortical somatosensory representation of the digits in humans. Neuroreport. 1999;10(15):3137–3141. doi: 10.1097/00001756-199910190-00003. [DOI] [PubMed] [Google Scholar]
- Ragert P, Schmidt A, Altenmuller E, Dinse HR. Superior tactile performance and learning in professional pianists: evidence for meta-plasticity in musicians. Eur J Neurosci. 2004;19(2):473–478. doi: 10.1111/j.0953-816x.2003.03142.x. [DOI] [PubMed] [Google Scholar]
- Recanzone G, Merzenich MM, Jenkins WM, Grajski KA, Dinse HR. Topographic reorganization of the hand representaiton in cortical area 3b owl monkeys trained in a frequency discrimination task. Journal of neurophysiology. 1992;67(5):1031–1056. doi: 10.1152/jn.1992.67.5.1031. [DOI] [PubMed] [Google Scholar]
- Recanzone GH, Schreiner CE, Merzenich MM. Plasticity in the frequency representation of primary auditory cortex following discrimination training in adult owl monkeys. J Neurosci. 1993;13(1):87–103. doi: 10.1523/JNEUROSCI.13-01-00087.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathian K, Zangaladze A. Tactile learning is task specific but transfers between fingers. Percept Psychophys. 1997;59(1):119–128. doi: 10.3758/bf03206854. [DOI] [PubMed] [Google Scholar]
- Sathian K, Zangaladze A. Feeling with the mind’s eye: contribution of visual cortex to tactile perception. Behav Brain Res. 2002;135(1–2):127–132. doi: 10.1016/s0166-4328(02)00141-9. [DOI] [PubMed] [Google Scholar]
- Schoups A, Vogels R, Qian N, Orban G. Practising orientation identification improves orientation coding in V1 neurons. Nature. 2001;412(6846):549–553. doi: 10.1038/35087601. [DOI] [PubMed] [Google Scholar]
- Seitz AR, Dinse HR. A common framework for perceptual learning. Curr Opin Neurobiol. 2007;17(2):148–153. doi: 10.1016/j.conb.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Stevens J, Alvarez-Reeves MDL, Mack G, Green B. Decline of tactile acuity in aging: a study of body site, blood flow, and lifetime habits of smoking and physical activity. Somatosensory and Motor Research. 2003;20(3–4):271–279. doi: 10.1080/08990220310001622997. [DOI] [PubMed] [Google Scholar]
- Tremblay F, Mireault AC, Dessureault L, Manning H, Sveistrup H. Postural stabilization from fingertip contact: I. Variations in sway attenuation, perceived stability and contact forces with aging. Exp Brain Res. 2004;157(3):275–285. doi: 10.1007/s00221-004-1830-4. [DOI] [PubMed] [Google Scholar]
- Tremblay F, Mireault AC, Dessureault L, Manning H, Sveistrup H. Postural stabilization from fingertip contact II. Relationships between age, tactile sensibility and magnitude of contact forces. Exp Brain Res. 2005;164(2):155–164. doi: 10.1007/s00221-005-2238-5. [DOI] [PubMed] [Google Scholar]
- Tremblay F, Wong K, Sanderson R, Cote L. Tactile spatial acuity in elderly persons: assessment with grating domes and relationship with manual dexterity. Somatosens Mot Res. 2003;20(2):127–132. doi: 10.1080/0899022031000105154. [DOI] [PubMed] [Google Scholar]
- Van Boven R, Hamilton R, Kauffman T, Keenan J, Pascual-Leone A. Tactile spatial resolution in blind braille readers. Neurology. 2000;54(12):2230–2236. doi: 10.1212/wnl.54.12.2230. [DOI] [PubMed] [Google Scholar]
- Van Boven R, Johnson K. A psychophysical study of the mechanisms of sensory recovery following nerve injury in humans. Brain. 1994;117( Pt 1):149–167. doi: 10.1093/brain/117.1.149. [DOI] [PubMed] [Google Scholar]
- Vega-Bermudez F, Johnson KO. Fingertip skin conformance accounts, in part, for differences in tactile spatial acuity in young subjects, but not for the decline in spatial acuity with aging. Percept Psychophys. 2004;66(1):60–67. doi: 10.3758/bf03194861. [DOI] [PubMed] [Google Scholar]
- Wright BA, Sabin AT. Perceptual learning: how much daily training is enough? Exp Brain Res. 2007;180(4):727–736. doi: 10.1007/s00221-007-0898-z. [DOI] [PubMed] [Google Scholar]