Abstract
Prophylactic antibiotics are frequently withheld until cultures are obtained in revision total knee arthroplasty (TKA). We undertook a prospective study to determine whether prophylactic preoperative intravenous antibiotics would affect the results of cultures obtained intraoperatively. We enrolled 25 patients with 26 infected TKAs, a known preoperative infecting organism, and no recent antibiotic therapy. Reaspiration of the infected TKA was performed after anesthesia and sterile preparation. Intravenous antibiotic prophylaxis was then administered and the tourniquet inflated. Intraoperative culture swabs and tissue were obtained at arthrotomy. The timing of events was recorded. Pre- and postantibiotic culture data were analyzed to determine the effect of intravenous preoperative prophylactic antibiotics on cultures obtained intraoperatively. Infections were acute postoperative (four), chronic (19), and acute hematogenous (three). The most common infecting organism was cloxacillin-sensitive Staphylococcus aureus (nine knees [35%]). Preoperative prophylactic antibiotics did not affect the results of intraoperative cultures and we therefore believe should not be withheld before surgery for an infected TKA when an organism has been identified on aspiration preoperatively, and there has been no recent (4 weeks) antimicrobial therapy.
Level of Evidence: Level II, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The routine use of preoperative antibiotic prophylaxis decreases the incidence of postoperative wound infections and has become the standard of care in TKA [6, 8, 10]. Antibiotic prophylaxis consisting of a first-generation cephalosporin is routinely used in TKA [10]. In institutions with a high rate of wound infections with methicillin-resistant organisms (MRSA), the addition of intravenous vancomycin is recommended preoperatively [10]. In addition to history, physical examination, and radiographs, synovial fluid aspiration with cell count and differential, aerobic and anaerobic cultures, and erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are routinely used [2, 6, 13, 14]. In patients who have a negative joint aspiration and cultures, on occasion, there may still be a major concern about indolent infection based on clinical findings, radiographs, or other laboratory results [4]. Cultures obtained intraoperatively are critical for selecting antibiotic therapy to treat these infections.
In patients presenting with a clinically infected TKA and a known infecting organism established on aspiration culture, antibiotics are routinely administered before surgery to reduce the burden of infection and sepsis. However, there has been concern in revision TKA that the use of preoperative antibiotic prophylaxis that is routinely given just before surgery will result in false-negative intraoperative culture results in patients with a presumed infected TKA if there has been no established preoperative culture result [13]. These false-negatives would thus result in suboptimal diagnosis and treatment of infection for these patients. Frequently, preoperative antibiotics are withheld by orthopaedic surgeons in patients undergoing revision knee arthroplasty until cultures are obtained intraoperatively [9].
The purposes of our study were to (1) determine whether the administration of routine prophylactic preoperative intravenous antibiotics would affect the accuracy of cultures obtained intraoperatively during revision TKA for infection; (2) determine the associated microbiology of the TKA infections; (3) evaluate the laboratory parameters (ESR, CRP, synovial fluid analysis); and (4) report the time of antibiotic administration to tourniquet inflation and to obtaining the intraoperative cultures.
Patients and Methods
In September 2005, we developed a prospective clinical study protocol to determine the effect of preoperative intravenous prophylactic antibiotics on intraoperative microbiology culture results in infected revision TKA. To adequately study this effect, we considered all patients presenting with an infected TKA and a known infecting organism from previous aspiration for enrollment in the study. Over a 36-month period (November 2005 to October 2008), we prospectively considered all patients presenting with an infected TKA for enrollment in the study. TKA infections were classified using the system of Segawa et al. [12]: Type 1, a positive intraoperative culture noted immediately after revision; Type 2, an acute postoperative infection (14 days postoperatively or less); Type 3, a late chronic infection (longer than 2 weeks); and Type 4, an acute hematogenous infection (from an identified distant host location). The study criteria for enrollment included TKA Type 2, 3, or 4 infections with a known infecting organism before undergoing revision surgery (recent aspiration culture performed), the pathogen cultured on solid media, confirmatory laboratory testing (ESR, CRP, complete blood cell count), not having received any form of oral or intravenous antibiotic for a minimum of 4 weeks for any reason (ie, antibiotic therapy for an infection involving the knee, urinary tract, wound, or any other source), and patients who were in agreement to participate in the approved prospective study protocol. All knees underwent ESR and CRP at our own institution preoperatively regardless of a prior outside laboratory result, to eliminate laboratory error and reference range differences between laboratory results. A normal ESR at our institution is a value 20 mm/hr or less and CRP 5 mg/L or less. Patients identified in the postoperative period with a positive intraoperative culture (Type 1 infection) after a revision TKA were excluded from the study, because they did not have a known infecting organism preoperatively. Other study exclusion criteria included recent treatment (within 4 weeks) with any antibiotic for any duration (related or unrelated to the TKA). All patients were consented by a clinical research study coordinator (SAG) other than the two treating surgeons. If a patient presented after hours, or on a weekend or legal holiday, the consent was obtained preoperatively by one of the two treating surgeons (RSB, RLB). We recorded routine demographic data, including age, gender, date of index TKA (or most recent TKA procedure), infecting organism and date of preoperative aspiration, and referred patients versus our own TKA patient population. The prospective study protocol was approved by the Institutional Review Board at our institution in November 2005. All enrolled patients completed a preoperative informed consent to participate in the study.
During the 3-year study enrollment, 717 knee procedures were performed relating to TKA. Five hundred five primary TKAs (70% of knee arthroplasty-related procedures) and 155 revision TKAs (noninfected; 22%) were performed. Thirty-seven knees (5%) underwent a two-stage reimplantation protocol for infection and 10 knees (1.4%) underwent irrigation and débridement with liner exchange and retention of components, also for sepsis. Five knees (0.7%) underwent knee arthrodesis for salvage of infection, and another five knees (0.7%) required above-knee amputation for failed attempts at salvage of periprosthetic sepsis. Infection-related procedures (57 knees) thus comprised 27% of all revision-related knee procedures and 8% of all combined knee arthroplasty-related procedures during the 3-year study period. Forty-seven knees presented with TKA sepsis during the study period; 21 knees were excluded from participating in the study (18 knees with recent or ongoing antibiotic therapy, three knees with no preoperative organism identified on culture). This left 25 patients (26 knees) who met the inclusion criteria, all of whom agreed to participate. No patients were lost to followup, and complete pre- and postoperative data were available for all 26 knees. One patient presented with a bilateral acute hematogenous infection of both TKAs. The demographic data (Table 1) revealed females outnumbered males by a ration of 3:1, whereas 24 of 26 knees (92%) were referred to our center by other orthopaedic surgeons for management of TKA infection. The mean time to developing TKA sepsis confirmed by a positive aspiration culture (and to study enrollment) from the most recent TKA procedure (primary or revision) was approximately 3 years (158 weeks). The actual time to developing an infection based on clinical symptoms alone was more difficult to determine from patient history, especially in chronically infected TKAs, and thus we have used the first positive aspiration culture in each knee as the time to infection. Type 3 (chronic infections: 19 knees [73%]) represented the majority of cases (Table 2).
Table 1.
Patient demographics (n = 26 knees)
| Category | Measurement |
|---|---|
| Gender | 20 female (77%)/6 male |
| Mean age | 66 years (range, 49–83 years) |
| Referred from other institution | 24 knees |
| Infected primary/revision TKA | 20/6 knees (77% versus 23%) |
| Mean time to septic TKA | 158 weeks (range, 3 weeks to 7.6 years) |
Table 2.
Classification of infected TKAs
| Infection type | Number of knees (n = 26) | Percent |
|---|---|---|
| Type 2 (acute postoperative) | 4 | 15 |
| Type 3 (chronic) | 19 | 73 |
| Type 4 (acute hematogenous) | 3 | 12 |
All surgery was performed by one of two surgeons (RSB, RLB) fellowship-trained in joint arthroplasty. After routine anesthesia, the operative knee was prepped with a sterile chlorhexidine-alcohol solution. Before any antibiotics were administered, the affected knee was aspirated, labeling the specimen “preantibiotic aspiration in the OR.” Time zero was recorded at the time of aspiration of the infected TKA before formal prepping and draping and before antibiotic prophylaxis infusion. The fluid was sent for a nucleated cell count with differential aerobic, anaerobic, mycobacterium, and fungal cultures in all cases. If there was a draining sinus, the aspiration was performed as far away as possible from the location of the sinus. The gross appearance and color of the synovial fluid was classified as normal (serous yellow), cloudy, serosanguinous, bloody, or purulent (frank pus). The timing of events was recorded on the data collection sheet by the circulating nurse in the operating room for the aspiration and for all further study events in the operating room. After aspiration of the joint, routine intravenous prophylactic antibiotics were administered immediately by the anesthesiologist. At our institution, this included a first-generation cephalosporin (cefazolin) and vancomycin (the use of these two agents was standard practice as recommended by our hospital infection control committee and microbiologists based on the hospital surgical site infection data reported for our institution and the increasing incidence of surgical site MRSA infections). The cephalosporin was routinely infused (“pushed”) rapidly over 1 to 2 minutes. The vancomycin infusion was started immediately (also after the aspiration) and completed infusion over the next 30 minutes. The exact times for antibiotic infusion start and end were recorded. If the known preoperative infecting organism was sensitive to an antibiotic that was preferable to either of these two agents, the organism-specific antibiotic was administered in addition to Ancef and vancomycin, intravenously, after the knee aspiration. The surgeon and team then scrubbed and the leg and surgical site preparation, then proceeded as we routinely perform for all TKAs. A nonsterile pneumatic tourniquet was applied to the upper thigh. The extremity, including the foot, was prepped and draped in the usual sterile fashion with a chlorhexidine-alcohol solution and the leg wrapped in a sterile impermeable stockinet. The skin over the knee was covered with a sterile impermeable iodine wrap barrier. The leg was then elevated but not exsanguinated and the time was recorded for tourniquet inflation. Deep exposure/arthrotomy was then immediately performed in a routine fashion using a medial parapatellar arthrotomy. Three sets of joint culture arthrotomy swabs were then taken for routine culture and another two for fungal and mycobacteria (five arthrotomy cultures total). We also sent a synovial tissue specimen in a representative area of membrane for separate microbiology culture. The planned surgical procedure then proceeded, which depended on the classification of the infection and the stability/fixation of the TKA implants. Patients with Type 2 and 4 infections underwent irrigation and débridement (I&D) with a modular polyethylene liner exchange when the infection and symptoms were acute (less than 2 weeks) and when the infecting organism and host status permitted intravenous postoperative antibiotic therapy for 6 weeks postoperatively. Patients with Type 3 infections (or Type 4 infections that were greater than 2 weeks in duration) underwent explantation/removal of the TKA, I&D, and insertion of a static/nonarticulating antibiotic-impregnated spacer and received a minimum of 6 weeks of intravenous antibiotic therapy. Any patient with septic loosening of any of the TKA implants underwent explantation, I&D, and insertion of an antibiotic spacer.
We recorded intraoperative data for all patients in a similar fashion on our study data collection sheet. Pre- and postoperative microbiology culture results were recorded once the final culture results had been reported by the in-hospital microbiology laboratory. Patients were not blinded to the pre- and postoperative study results. The two treating surgeons also were not blinded to the pre- or postoperative infecting organism and culture results, because this would have affected early antibiotic treatment. The comparison of pre- and postoperative culture results and the collection of data were performed by the study coordinator and an independent orthopaedic surgeon (AA, JTM, PMM) other than the two treating surgeons (RSB, RLB).
Results
In all 26 knees the organism(s) cultured on the preoperative aspiration and from the operating room cultures before antibiotic infusion, were the same organism(s) cultured at the time of arthrotomy despite the routine infusion of antibiotics. All organisms grew on solid media with two or more specimens positive for the same organism(s).
The microbiology culture results obtained before antibiotic infusion at the time of intraoperative aspiration (Table 3) revealed infection with Staphylococcus aureus (cloxacillin-sensitive) was most common, occurring in approximately one-third of knees (nine knees [35%]). The second most common infecting organism was MRSA, which occurred in five knees (19%) and in all cases was sensitive to the vancomycin infusion administered in the operating room. In one knee that grew Candida albicans at the time of aspiration in the operating room, this organism was not known to be present preoperatively but grew on both the aspiration and the arthrotomy cultures. This patient was also growing coagulase-negative staphylococcus preoperatively, which was presumed to be the infecting organism. In two knees with Gram-negative organisms (pseudomonas) known to be growing in the knee preoperatively, an organism-specific antibiotic agent (tobramycin) was infused in the operating room in addition to the routine cefazolin and vancomycin, at the recommendation of the infectious disease consultation obtained preoperatively. In one knee with a chronic Type 3 infection (6 years from index TKA), the preoperative organism isolated was S. aureus, and the aspirate was “grossly purulent” with a nucleated cell count of 114,500 cells × 106/L (differential 97% neutrophils). Only one of the arthrotomy cultures grew this organism on solid media, whereas the other two routine cultures processed grew the same organism on two separate specimens, but in broth only. Based on the clinical findings, laboratory parameters (ESR 85 mm/hr, CRP 96 mg/L), and aspiration cell-count, we considered these three arthrotomy cultures to all be true-positives after consultation and review of the specimens with our microbiologist.
Table 3.
Preoperative TKA aspiration culture results obtained before antibiotic infusion in the operating room
| Organism(s) | Number of knees |
|---|---|
| Staphylococcus aureus (cloxacillin-sensitive) | 9 |
| Methicillin-resistant S. aureus | 5 |
| Coagulase-negative Staphylococcus species | 4 |
| Streptococcus species | 3 |
| Gram-negative species | 2 |
| Mixed (greater than two organisms) species or Candida species | 3 |
Blood laboratory (Table 4) and knee aspiration data (Table 5) were available for all patients. ESR and CRP parameters were abnormally elevated in all 26 knees preoperatively. One chronic Type 3 infection had a normal ESR of 7 mm/hr with an elevated CRP value of 26.2 mg/L. The CRP level was elevated above normal in all 26 knees (100%). Twenty-five of 26 knees had a preoperative CRP level elevated at least four times above normal (ie, greater than 20 mg/L). One patient with a chronic Type 3 infection had a CRP level of 11.4 mg/L; however, the ESR was elevated at 65 mm/hr. The mean preoperative white blood cell count of the CBC was 9.2 × 10−9/L, which was within the normal reported reference range for our laboratory (normal range, 4–10.5 × 10−9/L) in 21 (81%) of 26 knees. In the five knees with an elevated white blood cell count in the CBC, the mean preoperative value was 12.3 × 10−9/L (range, 10.9–14.9 × 10−9/L). The qualitative appearance of the aspirated synovial fluid recorded in the operating room was “grossly purulent” in six knees, “bloody” or “bloody-serous” in 10 knees, “serous cloudy” in seven knees, and “serous” with any discoloration in three knees. Of the six knees that had a purulent appearing aspirate, one knee was from our own practice with an acute postoperative infection at 6 weeks (S. aureus, methicillin-sensitive), three knees (two patients; one bilateral TKA infection at 2 years) had developed acute hematogenous infections at 2 and 7 years postoperatively (S. aureus methicillin-sensitive grew in both knees of the bilateral patient; two organisms [pseudomonas and S. aureus methicillin-sensitive] in the other patient), respectively. Two other knees had “purulent”-appearing synovial fluid; one grew two organisms, including enterococcus species and coagulase-negative staphylococcus, and the other MRSA.
Table 4.
Blood laboratory data (n = 26 knees)
| Parameter | Mean value (range) | Standard deviation |
|---|---|---|
| Erythrocyte sedimentation rate (mm/hr) | 78 (7–237) | 56 |
| C-reactive protein (mg/L) | 79 (11–307) | 76 |
| White blood cell count (cells × 10−9/L) | 9.2 (3.7–14.9) | 3.3 |
Table 5.
Knee aspiration data
| Parameter | Mean value (range) | Standard deviation |
|---|---|---|
| Nucleated cell count (cells × 106/L) | 86,480 (300–371,000) | 94,414 |
| Neutrophil differential (%) | 93 (65–100) | 9.8 |
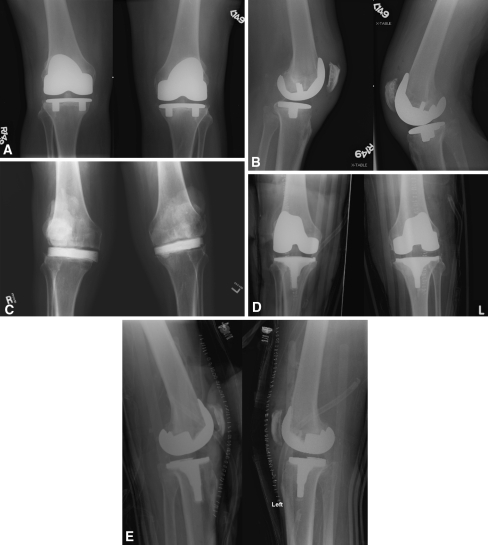
The time from antibiotic administration to arthrotomy cultures ranged from 18 to 33 minutes (Table 6). In the one patient who underwent surgery for bilateral infected TKAs (Fig. 1) under the same anesthetic performed sequentially (ie, not simultaneously), the antibiotic circulation time and time to arthrotomy were recorded for both knees separately from infusion start to arthrotomy for data collection purposes. However, the time to arthrotomy on the second knee in this patient was excluded from calculation of the mean time to arthrotomy, because it was a bilateral case.
Table 6.
Timing of events in the operating room (time zero = time antibiotic infusion begins)
| Parameter | Mean value (range) |
|---|---|
| Time to tourniquet inflation after antibiotics administered (minutes) | 15 (10–24) |
| Time to arthrotomy and intraoperative cultures (minutes) | 25 (18–33) |
Fig. 1A–E.
A 66-year-old man presented with bilateral infected TKA at 20 weeks (chronic Type 3 infection) after primary TKAs. Preoperative and operative cultures both grew Staphylococcus aureus sensitive to cloxacillin despite administration of intraoperative antibiotics. (A) Preoperative anteroposterior (AP) radiographs of bilateral TKA suggest septic loosening of both tibial cementless components. (B) Preoperative lateral radiographs are shown. (C) Bilateral AP radiographs after explantation of femoral, tibial, and patellar irrigation and débridement of the infected TKAs are shown. A static antibiotic-loaded cement spacer has been inserted bilaterally. The patient was treated with 6 weeks of intravenous antibiotics. The erythrocyte sedimentation rate and C-reactive protein normalized, and both knees were reaspirated at 10 weeks with no growth of bacteria. (D) Bilateral second-stage reimplantation TKAs were performed at 12 weeks after the explant procedure as shown in AP radiographs. (E) Bilateral lateral postoperative radiographs are shown.
Discussion
Preoperative antibiotics are routinely administered before surgery to reduce the burden of infection and sepsis in patients presenting with a clinically infected TKA and a known infecting organism. However, many surgeons are concerned that in revision TKA with presumed infection but no established preoperative culture the use of preoperative antibiotic prophylaxis routinely given just before surgery will result in false-negative intraoperative culture results [13]. These false-negatives would thus result in suboptimal diagnosis and treatment of infection for these patients. Frequently, preoperative antibiotics are withheld by orthopaedic surgeons in patients undergoing revision knee arthroplasty until cultures are obtained intraoperatively [9]. Were therefore (1) determined whether the administration of routine prophylactic preoperative intravenous antibiotics would affect the accuracy of cultures obtained intraoperatively during revision TKA for infection; (2) determined the associated microbiology of the TKA infections; (3) evaluated the laboratory parameters (ESR, CRP, synovial fluid analysis); and (4) determined the time of antibiotic administration to tourniquet inflation and to obtaining the intraoperative cultures.
The limitations of the current study first include the relatively small sample size (n = 26 knees) and the selection criteria, which only included cases with a preoperatively known infecting organism. It would obviously be preferable to study this subject in a much larger, prospective, clinical trial, which would require a multicenter study, because few centers are performing high volumes of surgery on infected TKAs. Such a trial would ideally include all revision TKA cases prospectively using an aspiration protocol and administration of prophylactic preoperative antibiotics in knees with or without a known infecting organism. Thus, the extrapolation of the results of this series of infected TKA to the general TKA revision population (without clinical infection) should be made with caution. However, the current study cohort provides an ideal control for isolating the effect of administering preoperative antibiotics in patients with a known infecting organism. Second, performing the arthrotomy, taking cultures within a few minutes, and then administering intravenously antibiotics (with the tourniquet down) might be just as effective at isolating cultures while providing antibiotic coverage, and this algorithm is useful when an organism has not been isolated preoperatively. This technique, however, was not performed in the current study. There are several strengths to the current study. It is a prospective clinical study, which has been controlled to isolate the important effect of the use of preoperative intravenous prophylactic antibiotics on revision TKA for infection. Additionally, two surgeons from the same institution with the same clinical pathways and protocols and the same laboratory participated in the study, which may help to reduce bias from laboratory and procedural differences between institutions and practice patterns.
We recognize it is common practice to withhold administration of antibiotics before obtaining intraoperative cultures during revision joint arthroplasty. The potential advantage is demonstrating a new pathogen that was not known through preoperative aspiration. The disadvantage is that patients are deprived of the benefit of prophylactic antibiotics before skin incision, which has been called the greatest single contribution to minimizing infection in total joint surgery [11]. This a particular disadvantage in revision TKA in which infection rates are much higher than primary TKA with an incidence of 5.6% in one review [7]. One study has reported an infection rate as high as 10% in revision TKA surgery [15]. In addition, a tourniquet is used and if antibiotics are withheld, there may well not be bactericidal antibiotic levels in the wound until the end of the case. The routine use of preoperative antibiotic prophylaxis has become the standard of care in primary joint arthroplasty and is now defined as quality measure numbers 20, 21, and 22 in the Physician Quality Reporting Initiative (PQRI) by the Center for Medicare and Medicaid Services (CMS) [1]. Cultures obtained intraoperatively during revision surgery have become critical to the optimal tailoring of antibiotic therapy for treatment of infections. In the current study, all patients had a known infecting organism isolated from a preoperative culture. However, there has been concern that the use of preoperative antibiotic prophylaxis will result in false-negative intraoperative culture in patients with a presumed infected total joint arthroplasty and negative preoperative cultures. These false-negatives may result in suboptimal therapy for these patients. Frequently, preoperative antibiotics are withheld in patients undergoing revision arthroplasty until cultures are obtained based on these concerns. The incidence of true infections in this cohort of patients is low. The vast majority of these patients inappropriately did not receive preoperative antibiotic prophylaxis based on the chance that they might have an infection and further that the use of preoperative antibiotics would result in a false-negative culture result.
In a recently reported retrospective analysis [5] of 171 patients with known total knee infections based on widely accepted criteria, 72 knees received preoperative prophylaxis, whereas in 99, antibiotics were withheld based on surgeon preference. Similar percentages of false-negatives occurred in patients who received antibiotics compared with those whose antibiotics were withheld (nine of 72 or 12.5% versus eight of 99 or 8%, respectively). In addition, when antibiotics were withheld, a second organism was demonstrated as often as when prophylactic antibiotics were administered (four of 99 or 4% versus one of 72 or 1.4%). Also, all but one of these “additional organisms” was Staphylococcus epidermidis, which grew on broth only with the only additional organism growing on solid media being a sensitive streptococcus species. No clinically useful benefit, therefore, could be attributed to withholding prophylactic antibiotics in the study.
Accurate diagnosis of periprosthetic infection often requires the use of a combination of tests and a strong clinical suspicion [3]. Serologic tests, including measurements of white blood cell count, ESR, and CRP, represent first-line investigations and generally have a high sensitivity but lower specificity. Synovial fluid aspiration has a higher specificity and is especially valuable for diagnosis of suspected infection of the knee. When cell count and differential values are combined, a higher sensitivity, specificity, and accuracy may be attained than aspiration culture result alone in diagnosing infection after TKA. The intraoperative culture of tissue and/or fluid obtained during revision TKA is considered the gold standard for determining the presence or absence of periprosthetic infection. However, these tests may yield false-negative and false-positive results. Organisms are not always isolated from cultures, yet the implant ultimately proves to be infected. In addition, positive cultures of specimens from periprosthetic tissue may not represent false-positives because specimens may become contaminated when tissue is harvested during transport or in the laboratory.
In summary, the exclusion of infection as a cause of TKA failure is imperative to determine the management at revision TKA. Accurate diagnosis often requires the use of a combination of tests and a strong clinical suspicion. Intraoperative cultures, although considered the gold standard, are also subject to false-positive and false-negative results. Our study shows that in patients presenting with an infected TKA with a known infecting organism, the routine administration of prophylactic preoperative intravenous antibiotics will not adversely affect the result of intraoperatively obtained cultures in revision joint arthroplasty by resulting in false-negative results. Thus, the authors recommend that preoperative antibiotics should not be withheld before surgery in revision for an infected TKA provided an organism has been cultured preoperatively. Patients should not be deprived of potential benefits of preoperative antibiotic prophylaxis in cases with known infection or those without clinical evidence of infection. The single scenario in which withholding antibiotic prophylaxis may be of benefit is in those with clinical suspicion of infection in which preoperative aspirations have been negative. This should, however, represent only a small minority of patients. Even in these select cases, the practice of withholding prophylactic antibiotics remains theoretical and warrants further study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at The Washington University School Department of Orthopaedic Surgery and Barnes-Jewish Hospital, St Louis, MO, USA.
Contributor Information
R. Stephen J. Burnett, Email: stephen.burnett@viha.ca.
Robert L. Barrack, Email: barrackr@wustl.edu, Email: pouchera@wustl.edu.
References
- 1.American Academy of Orthopaedic Surgeons (AAOS). Physician Quality Reporting Initiative, Orthopaedic Specific Measures; Clinical Measures, page 1; numbers 20, 21, 22. Available at: http://www.aaos.org/research/committee/evidence/pqri_measures.asp. Accessed October 29, 2008.
- 2.Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson H, Peto TE, McLardy-Smith P, Berendt AR. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. The OSIRIS Collaborative Study Group. J Clin Microbiol. 1998;36:2932–2939. doi: 10.1128/jcm.36.10.2932-2939.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer TW, Parvizi J, Kobayashi N, Krebs V. Diagnosis of periprosthetic infection. J Bone Joint Surg Am. 2006;88:869–882. doi: 10.2106/JBJS.E.01149. [DOI] [PubMed] [Google Scholar]
- 4.Della Valle CJ, Bogner E, Desai P, Lonner JH, Adler E, Zuckerman JD, Di Cesare PE. Analysis of frozen sections of intraoperative specimens obtained at the time of reoperation after hip or knee resection arthroplasty for the treatment of infection. J Bone Joint Surg Am. 1999;81:684–689. doi: 10.2106/00004623-199905000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Ghanem E, Parvizi J, Clohisy J, Burnett S, Sharkey PF, Barrack R. Perioperative antibiotics should not be withheld in proven cases of periprosthetic infection. Clin Orthop Relat Res. 2007;461:44–47. doi: 10.1097/BLO.0b013e318065b780. [DOI] [PubMed] [Google Scholar]
- 6.Hanssen A, Osmon D, Nelson C. Prevention of deep periprosthetic joint infection. Instr Course Lect. 1997;46:555–567. [PubMed] [Google Scholar]
- 7.Hanssen A, Rand J. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999;48:111–122. [PubMed] [Google Scholar]
- 8.Hanssen AD, Osmon DR. The use of prophylactic antimicrobial agents during and after hip arthroplasty. Clin Orthop Relat Res. 1999;369:124–138. doi: 10.1097/00003086-199912000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Lonner JH. Staged revision of the infected TKA. In: Lotke PA, Lonner JH, editors. Master Techniques in Orthopaedic Surgery: Knee Arthroplasty. 2. Philadelphia, PA: Lippincott Williams &Wilkins; 2003. [Google Scholar]
- 10.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132. doi: 10.1016/S0196-6553(99)70088-X. [DOI] [PubMed] [Google Scholar]
- 11.Mulvey T, Thornhill T. Infected total knee arthroplasty. In: Insall JN, Scott WN, editors. Surgery of the Knee. 3. Philadelphia, PA: Churchill Livingstone; 2001. [Google Scholar]
- 12.Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81:1434–1445. doi: 10.2106/00004623-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Spangehl MJ, Masri BA, O’Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999;81:672–683. doi: 10.2106/00004623-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am J Med. 2004;117:556–562. doi: 10.1016/j.amjmed.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 15.Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80:1770–1774. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]