Abstract
Despite substantial advances in primary TKA, numerous studies using historic TKA implants suggest only 82% to 89% of primary TKA patients are satisfied. We reexamined this issue to determine if contemporary TKA implants might be associated with improved patient satisfaction. We performed a cross-sectional study of patient satisfaction after 1703 primary TKAs performed in the province of Ontario. Our data confirmed that approximately one in five (19%) primary TKA patients were not satisfied with the outcome. Satisfaction with pain relief varied from 72–86% and with function from 70–84% for specific activities of daily living. The strongest predictors of patient dissatisfaction after primary TKA were expectations not met (10.7× greater risk), a low 1-year WOMAC (2.5× greater risk), preoperative pain at rest (2.4× greater risk) and a postoperative complication requiring hospital readmission (1.9× greater risk).
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Total knee arthroplasty (TKA) has revolutionized the care of patients with end-stage knee arthritis [1–3, 6, 8, 9, 13, 16, 17, 21]. Despite substantial advances in primary TKA patient selection, surgical technique, and implant design, numerous studies indicate only 82% to 89% of patients were satisfied with their primary total knee arthroplasty [2, 9, 11, 12, 14, 22, 23, 26]. These reports suggest that TKA is not achieving its goal of relieving pain and restoring function in a substantial proportion of patients.
Patient satisfaction is an important outcome measure because there is a well-documented discrepancy between clinician and patient ratings of health status [15, 21]. Mahomed et al. developed a validated, self-administered satisfaction scale (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) which assessed overall satisfaction as well as that of pain relief and the ability to perform daily and leisure activities [19, 20]. Wylde et al. utilized this satisfaction scale in a comparison of fixed- versus mobile-bearing total knee arthroplasties (n = 250 knees) [25, 26]. While the authors found no satisfaction differences between the implant types, they did note surprisingly low satisfaction with specific activities (ie, 66% “very satisfied” with pain relief, 52% with return to normal activities of daily living and 44% with the ability to perform leisure activities).
To confirm the limited literature on patient satisfaction after primary total knee arthroplasty we determined (1) functional scores to ensure our patient population was similar to that in the literature; (2) the overall level of satisfaction; then (3) which of a number of preoperative and operative factors might predict patient satisfaction and dissatisfaction.
Patients and Methods
In a study approved by our research ethics board, we reviewed prospectively collected data on 1703 eligible patients who underwent primary TKA from June 2001 to December 2005. These patients were a subset of patients from a prospective study conducted by the Ontario Joint Replacement Registry that evaluated the relationship between severity at decision for surgery, waiting times for surgery, and 1-year outcomes [7]. To be included, consenting patients needed to be booked for a planned primary total knee arthroplasty. We excluded patients with revision arthroplasties, patients “on sick leave” or “on disability,” and those with a second total knee arthroplasty during the study period. WOMAC scores were collected for 2051 primary total knee arthroplasty patients. One year later, these patients were mailed followup questionnaires, which included a 1-year WOMAC score and a satisfaction score [3–5, 19]. Dillman procedures were utilized to maximize the response rate [10]. First, a prenotice letter was sent, followed by the questionnaire and then a reminder postcard. Nonrespondents were sent two additional mailings including the questionnaire: 1703 patients (83%) returned completed questionnaires, 123 (6%) were dropped due to incomplete answers, and 225 (11%) did not respond.
The enrolled cohort of 1703 primary total knee arthroplasty patients had a mean age of 69 ± 9 years (range, 27–88 years); 60% were female, the mean body mass index was 32 ± 6, and 92% had a primary diagnosis of osteoarthritis (4% rheumatoid arthritis, 2% posttraumatic osteoarthritis, 2% other). Fifty-two percent had a flexion contracture, 12% had a valgus deformity, and 71% a varus deformity. Comorbidity according to the American Society of Anesthesiologists scale revealed 37% at levels 3 or 4. Twenty-two percent of patients were working, 19% lived alone, 16% depended on someone else for activities of daily living, and 12% had someone who depended on them. Forty-four percent of patients were reassessments and 11% were new referrals. Eleven percent of patients had flexion less than 90°. Preoperative WOMAC outcome scores were: pain, 43.4 ± 16.8 (mean ± SD); joint stiffness, 40.2 ± 20.3; function, 42.4 ± 16.2; and total, 42.4 ± 16.2. Fifty-three percent had a cruciate-sparing design and 47% a cruciate-sacrificing design. Seventy-four percent had a patellar resurfacing performed.
Data were collected by participating surgeons, their staff, and field staff of the Ontario Joint Replacement Registry [7]. Preoperatively, at the decision date for surgery, the following demographic and clinical data were collected: age, gender, side, primary diagnosis, reassessment versus new referral, deformity (flexion contracture, varus, valgus), knee flexion, body mass index (BMI), American Society of Anesthesiologists Physical (ASA) status score [1], employment status (working full time, working part time, homemaker, retired, unemployed looking for work, not working for another reason), living status (live alone: yes/no), and independence with activities of daily living. A preoperative WOMAC questionnaire (Likert version 3.1) was also collected at decision date [3–5]. In surgery, it was noted whether a posterior cruciate-substituting or -retaining implant was used and whether the patella was resurfaced.
The satisfaction questionnaire included three questions: (1) Overall, how satisfied are you with the results of your knee replacement surgery? (2) How satisfied are you with your most recent knee replacement surgery for reducing your pain (walking on a flat surface, going up or down stairs, sitting or lying down)? and (3) How satisfied are you with your most recent knee replacement surgery for improving your ability to perform five functions (going up stairs, getting in/out of a car or on/off a bus, rising from bed, lying in bed, performing light domestic duties) [16]? Patients were asked to grade their level of satisfaction for each question (ie, very dissatisfied, dissatisfied, neutral, satisfied, or very satisfied). The overall satisfaction question was used to determine a two-category satisfaction outcome by combining patients who answered very dissatisfied, dissatisfied, or neutral into one group, and patients who answered satisfied or very satisfied into the second group. This two-category outcome (satisfied, not satisfied/neutral) was used as the measure of overall satisfaction for all statistical analyses. Patient satisfaction or dissatisfaction were our primary variables.
WOMAC scores were reverse scored and standardized to a score from 0 to 100 (worst to best) [3–5]. The WOMAC change score was determined by subtracting the decision date WOMAC from the 1-year WOMAC. Missing WOMAC (one pain, < four function) items were input as suggested by Bellamy [3–5]. Questionnaires with more missing items were excluded from the analysis (n = 123 [6%]).
Preoperative, intraoperative and postoperative variables were explored between the satisfied and dissatisfied total knee replacement groups to determine where statistical differences may exist [24]. Categorical variables (gender, comorbidity, employment status, live alone, dependence on others, primary diagnosis, reassessment, presence of preoperative deformities, preoperative flexion less than 90 degrees, preoperative extreme pain, prosthesis cruciate design, patella resurfacing, complications, willingness to have surgery again and expectations) were tested using cross tabulation with chi-square (Table 1). Scale variables (age, BMI, preoperative, 1-year and change WOMAC scores) were tested for significance using Kolmogorov-Wilcoxon for nonparametric data (Table 1). Forward stepwise logistic regression was performed to establish factors that substantially determined patient satisfaction (Table 2). Major (age, preoperative flexion less than 90°, preoperative extreme pain while sitting or lying, complications, 1-year WOMAC pain, joint stiffness and function, expectations not met and those that had no expectations) and other variables that were deemed clinically important (valgus deformity, varus deformity, preoperative WOMAC function) were introduced into two separate regression models (Table 1). Prior to inclusion, variables were tested for interdependence through correlations and those that were highly correlated were excluded from the regression models (1-year WOMAC total, change WOMAC domains and total score). In the first model, only preoperative variables were included (age, varus deformity, valgus deformity, flexion less than 90°, extreme preoperative pain and low WOMAC function). In the second model, in addition to the preoperative variables used in the first model, postoperative variables were introduced to the regression model (complication, low 1-year WOMAC domain scores, expectations not met, and had no expectations). This approach to the analysis allowed us to identify variables that may be used to predict satisfaction (preoperative variables in model one) and to observe the effect that postoperative variables inevitably have on patient satisfaction (model two). Odds ratios were reported for significant variables. All statistical analyses were performed with SPSS version 16 (SPSS Inc, Chicago, Ill.), SAS version 8 (SAS Institute Inc, Cary, NC), and MedCalc for Windows, version 9.3.6.0 (MedCalc Software, Mariakerke, Belgium).
Table 1.
Univariate statistical analysis results between satisfaction outcome groups; dissatisfied/neutral and satisfied, divided by time of availability to surgeon (A: preoperative variables; B: surgical variables; C: postoperative variables)*
| Preoperative variables | Dissatisfied/neutral (n = 328) | Satisfied (n = 1375) | Significance (p) |
|---|---|---|---|
| Sociodemographic | |||
| Age (mean ± SD) | 70 ± 9 | 68.8 ± 8.67 | 0.012 |
| BMI (mean ± SD) | 32.2 ± 6.5 | 31.6 ± 6.1 | 0.306 |
| Female | 62.2% | 59.5% | 0.380 |
| Comorbidity (ASA 3/4) | 39% | 36.4% | 0.408 |
| Employed (FT/PT) | 19.5% | 22% | 0.369 |
| Live alone | 24.1% | 18% | 0.013 |
| Depend on someone for ADL | 19.5% | 15.4% | 0.080 |
| Depended on by someone for ADL | 11.3% | 12.5% | 0.575 |
| Degenerative arthritis | 93.3% | 91.1% | 0.226 |
| Clinical assessment | |||
| Reassessment | 48.5% | 42.3% | 0.047 |
| Any flexion contracture | 49.7% | 52.1% | 0.461 |
| Any valgus deformity | 9.5% | 12.6% | 0.130 |
| Any varus deformity | 69.8% | 71.5% | 0.542 |
| Preop flexion ROM < 90 | 7.5% | 12% | 0.022 |
| Extreme pain while lying or sitting | 11% | 4.7% | 0.000 |
| Preoperative WOMAC | |||
| Pain (mean ± SD) | 41.7 ± 16.8 | 43.8 ± 16.8 | 0.152 |
| Joint stiffness (mean ± SD) | 39.3 ± 19.7 | 40.4 ± 20.5 | 0.442 |
| Function (mean ± SD) | 41.1 ± 16.1 | 42.7 ± 16.3 | 0.083 |
| Total (mean ± SD) | 41.1 ± 15.5 | 42.7 ± 15.5 | 0.083 |
| Surgical Variables | |||
| Prosthesis cruciate design | |||
| Cruciate sparing prosthesis | 54.6% | 52.1% | 0.458 |
| Cruciate sacrificing prosthesis | 45.4% | 47.9% | |
| Patella resurfaced | 76.8% | 73.7% | 0.261 |
| Postoperative Variables | |||
| Complications | 10.4% | 3.1% | 0.000 |
| One year WOMAC | |||
| Pain (mean ± SD) | 72.1 ± 22.1 | 89.6 ± 12.4 | 0.000 |
| Joint stiffness (mean ± SD) | 66.2 ± 25.1 | 82.6 ± 16.7 | 0.000 |
| Function (mean ± SD) | 66.1 ± 22.5 | 84.4 ± 14.1 | 0.000 |
| Total (mean ± SD) | 67.3 ± 21.8 | 85.34 ± 13 | 0.000 |
| Change WOMAC | |||
| Pain (mean ± SD) | 30.4 ± 22.6 | 45.8 ± 18.9 | 0.000 |
| Joint stiffness (mean ± SD) | 26.9 ± 27.3 | 42.2 ± 23.9 | 0.000 |
| Function (mean ± SD) | 25 ± 22.6 | 41.8 ± 19.1 | 0.000 |
| Total (mean ± SD) | 26.3 ± 21.6 | 42.6 ± 17.9 | 0.000 |
| Surgery again | |||
| Not have surgery again | 19.6% | 1.3% | 0.000 |
| Would still have surgery | 62.4% | 95.5% | |
| Uncertain to have surgery again | 18% | 3.2% | |
| Expectations | |||
| Expectations met | 34.5% | 78.5% | 0.000 |
| Expectations not met | 49.4% | 5.8% | |
| Had no expectations met | 16.2% | 15.7% | |
* Percent within satisfaction group quoted for categorical variables; mean ± SD quoted for continuous variables. Variables are significant when < 0.05.
Table 2.
Odds of being dissatisfied arranged by availability to surgeon. Odd ratios were obtained through logistic regression analysis
| Variables | Time | |
|---|---|---|
| Preoperative (Model 1) | Postoperative (Model 2) | |
| Age | 1.02 | 1.03 |
| Any valgus deformity | 0.47 | —* |
| Any varus deformity | 0.69 | — |
| Flexion ROM < 90° | 0.55 | — |
| Baseline extreme pain while sitting or lying | 2.29 | 2.36 |
| Baseline WOMAC function | — | 1.01 |
| Complication | 1.86 | |
| Low 1-year WOMAC pain | 2.45 | |
| Low 1-year WOMAC joint stiffness | −0.64 | |
| Low 1-year WOMAC function | 2.46 | |
| Expectations not met | 10.66 | |
| Had no expectations | 1.77 | |
* Odds ratios for variables that were nonsignificant (p > 0.05) predictors of dissatisfaction in each regression model are not reported.
Results
The mean WOMAC subscales and total scales improved one year postoperatively from preoperatively. The mean 1-year WOMAC pain score was 86.2 ± 16.3 with a change score of 42.9 ± 20.6. The mean 1-year WOMAC joint stiffness score was 79.4 ± 19.7 with a change score of 39.6 ± 25.4. The mean 1-year WOMAC function score was 80.9 ± 17.7, representing an average improvement of 38.5 ± 20.9. The average total 1-year WOMAC score was 81.9 ± 16.6 with an average change of 39.5 ± 19.8. Five percent of patients (76) reported a complication on the self-assessment questionnaire. The commonest complications requiring hospital readmission were infection (15%), blood clot (9%), or other (38%).
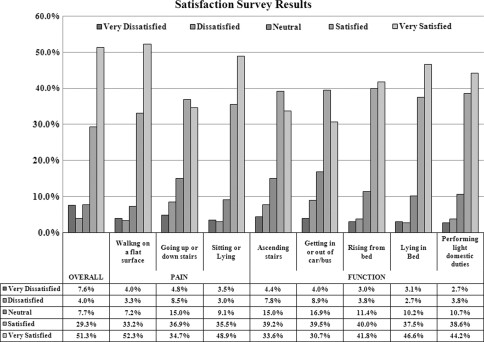
Overall satisfaction, which was used as a proxy for the satisfaction outcome, revealed that 81% (n = 1375) of patients claimed that they were satisfied or very satisfied while 19% (n = 328) were very dissatisfied, dissatisfied, or neutral. Satisfaction with pain relief and function with activities of daily living varied between 72% and 86% and 70% and 84% respectively (Fig. 1). Satisfaction did not vary by type of prosthesis (eg, posterior cruciate-retaining versus -sacrificing prosthesis) nor by whether the patella was resurfaced (Table 1).
Fig. 1.
Satisfaction after primary total knee replacement 1 year after surgery was assessed by overall satisfaction and satisfaction with pain relief and activities function for daily living are shown.
For pain relief, only 72% were satisfied with their ability to go up or down stairs as compared to 85% with walking on a flat surface and 84% with sitting or lying. For restored function, patients were least satisfied with getting in or out of a bus or car (70%) and ascending stairs (73%), as compared to rising from a bed (82%), lying in a bed (84%), and performing light domestic duties (83%). For overall satisfaction, which was used as the proxy for the satisfaction outcome, 81% (1375) of patients claimed that they were satisfied or very satisfied while 19% (328) were very dissatisfied, dissatisfied, or neutral.
Dissatisfied primary total knee arthroplasty patients were older (70 ± 9 versus 69 ± 9 years), lived alone (24% versus 18%), were more often a reassessment rather than a new patient referral at decision date for surgery (49% versus 42%), less likely to have less than 90° preoperative flexion (8% versus 12%), have extreme pain on the WOMAC pain score while lying or sitting (11% versus 4%), have a lower 1-year WOMAC (67 versus 85), have a lower WOMAC change score (26 versus 43), not be willing to have surgery again (20% versus 1%), and had expectations which were not met (49% versus 6%) as compared to satisfied patients (Table 1). The odds ratios of the variables predicting patient dissatisfaction after primary total knee arthroplasty changed as new variables were introduced into the model (Table 2). In the final regression model (Table 2, model 2), significant variables for patient dissatisfaction were advancing age, preoperative extreme pain on the WOMAC pain score while sitting or lying, a low baseline WOMAC function score, the presence of a postoperative complication necessitating hospital admission, a low 1-year WOMAC score, and expectations not met. The strongest contributing variables to patient dissatisfaction after primary total knee arthroplasty using odds ratios were expectations not met (10.7×), a low 1-year WOMAC (2.5×), a low preoperative WOMAC pain score while sitting or lying (2.4×), and a complication requiring hospital admission (1.9×).
Discussion
Numerous reports have noted that not all patients are satisfied after their primary total knee replacement with only 82–89% expressing satisfaction [2, 9, 11, 12, 14, 22, 23, 26]. In this study, we have determined that contemporary TKA implants do not seem to have improved patient satisfaction levels. We have confirmed that meeting patient expectations is of the utmost importance in achieving patient satisfaction after primary TKA [9, 14, 15, 20, 22]. In addition, certain preoperative factors (advancing age, living alone, less than 90° flexion and pain at rest) and postoperative factors (a complication requiring hospital readmission and a low 1-year WOMAC) were associated with dissatisfied primary TKA patients.
We note several limitations. First, only 83% of eligible patients completed all required forms. While we believe this response rate acceptable, it does raise the risk of bias being entered into the study should the responder and nonresponder populations be different [10]. On the other hand, we had a relatively large cohort (n = 1703) of primary total knee arthroplasty patients representative of urban versus rural, community versus academic, and high-volume versus low-volume surgical practices, as well as a wide range of contemporary primary total knee arthroplasty designs. Second, we only assessed patient satisfaction 1 year postoperatively and retrospectively assessed patient expectations by asking whether or not expectations had been met (met, not met, had none). Mahomed et al. [20] did assess patient expectations preoperatively in 103 THA and 89 TKA primary procedures. Seventy-six percent of patients expected to have no pain after recovery from surgery, but only 40% expected to have no functional limitations. When comparing high- versus low-expectation patients, there were no differences in age or gender. Multivariate analyses 6 months after surgery revealed that greater patient expectations predicted higher outcomes for WOMAC pain, WOMAC physical function, and SF-36 physical function. Our data support these observations in that 70% of patients felt that their expectations were met, but from the 1-year postoperative vantage point, 18% of our patients reported that their expectations were too high and 69% stated that their expectations were just right. Third, we did not evaluate patient mental well being but acknowledge that mental health is associated with patient satisfaction [2].
The outcomes of total knee arthroplasty patients have been traditionally assessed by surgeons using unvalidated scoring systems in which the patient was asked about their level of pain and return to specific activities, followed by the surgeon objectively measuring range of motion and joint stability. Increasing evidence is emerging that patients and doctors do not always agree on quality-of-life improvements after therapeutic interventions [9, 15, 21, 22]. Our study reinforces the importance of assessing patient satisfaction and expectations to predict functional outcomes and supports the observations of Katz et al. [18] and Noble et al. [22].
Overall, patient satisfaction after primary total knee arthroplasty was 81% in our study. This level of satisfaction is at the low end of published satisfaction rate studies (Table 3), but this might partly be explained by differing numbers of patients being assessed, differing lengths of followup, differing patient ages, and mixed diagnoses. Robertsson et al. reported on 27,372 knee arthroplasties with 2 to 17 years’ followup in the Swedish Knee Arthroplasty Register [23]. They found patient satisfaction was remarkably constant in patients not requiring revision procedures for all followup periods. As in our study, Robertsson et al. [23] reported a correlation between satisfaction and improvements in both pain and physical function outcomes (ie, WOMAC, Oxford-12). We found a weak correlation for poorer satisfaction with advancing age (odds ratio 1.03), whereas Robertsson et al. [23] found no correlation between satisfaction and age for patients with osteoarthritis; but a correlation for poorer satisfaction with advancing age in patients with rheumatoid arthritis. Our results are consistent with those of Noble et al. [22] that patient satisfaction decreases with advancing age, residual symptoms, expectations not met and less functional improvement.
Table 3.
Comparison of published satisfaction percentages after primary total knee replacement
Consistent with the literature, we found that only 81% of patients expressed overall satisfaction with their primary total knee arthroplasty, and when asked about satisfaction with pain relief and function for activities of daily living these varied between 72% and 86%, and 70% and 84%, respectively [2, 9, 11, 12, 15–17, 19, 20, 22, 23]. The most significant factors associated with primary total knee arthroplasty patient dissatisfaction were expectations not met (10.7 times greater risk), a low 1-year WOMAC score (2.5 times greater risk), a low preoperative WOMAC score (2.4 times greater risk), and a complication requiring hospital readmission (1.9 times greater risk).
Although primary total knee arthroplasty has revolutionized the care of patients with end-stage arthritis, our study confirms the findings of others that 11% to 19% of primary TKA patients are not satisfied with their surgical intervention [2, 9, 12, 16–20, 23] (Table 3). Our data help identify patients at risk and areas in need of further study. The impact of patient expectations on satisfaction is profound. Obviously, it would be wise for orthopaedic surgeons and patients to discuss expectations before TKA surgery to assure that these are realistic. In addition, identifying a low preoperative WOMAC score as a risk factor for patient dissatisfaction should be discussed with the patient. Finally, this study confirms the impact of a complication requiring hospital admission as an important factor in patient dissatisfaction.
Acknowledgments
We thank the Ontario orthopaedic surgeons who entered data into the Ontario Joint Replacement Registry (OJRR) and the Ontario Ministry of Health and Long Term Care who funded the project.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.American Society of Anesthesiologists (ASA) Web site: Physical Status Score. Available at: http://www.asahq.org/physicalstatus.htm. Accessed Feb. 21, 2006.
- 2.Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty. 1996;11:831–840. doi: 10.1016/S0883-5403(96)80183-5. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N. WOMAC Osteoarthritis Index: A User’s Guide IX. Brisbane, Australia: The University of Queensland; 2008. p. 176. [Google Scholar]
- 4.Bellamy N. WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29:2473–2476. [PubMed] [Google Scholar]
- 5.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 6.Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J. Influence of patient factors on TKA outcomes at 5 to 11 years followup. Clin Orthop Relat Res. 2007;464:27–31. doi: 10.1097/BLO.0b013e318159c5ff. [DOI] [PubMed] [Google Scholar]
- 7.Bourne RB, Sibbald WJ, Doig G, Lee L, Adolph S, Robertson D, Provencher M. The Southwestern Ontario Joint Replacement Pilot Project: electronic point-of-care data collection. Southwestern Ontario Study Group. Can J Surg. 2001;44:199–202. [PMC free article] [PubMed] [Google Scholar]
- 8.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. doi: 10.1097/01.blo.0000148594.05443.a3. [DOI] [PubMed] [Google Scholar]
- 9.Chesworth BM, Mahomed NN, Bourne RB, Davis AM. Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol. 2008;61:907–918. doi: 10.1016/j.jclinepi.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Dillman D. Mail and Electronic Surveys: The Tailored Design Method. New York, NY: Wiley; 2000. [Google Scholar]
- 11.Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from the Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83:339–344. doi: 10.1302/0301-620X.83B3.11134. [DOI] [PubMed] [Google Scholar]
- 12.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. J Bone Joint Surg Am. 1998;80:163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Hawker G, Wright J, Coyte P, Williams J, Harvey B, Glazier R, Badley E. Differences between men and women in the rate of use of hip and knee arthroplasty. N Eng J Med. 2000;342:1016–1022. doi: 10.1056/NEJM200004063421405. [DOI] [PubMed] [Google Scholar]
- 14.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998;356:93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Janse AJ, Gemke RJ, Uiterwaal CS, Tweel I, Kimpen JL, Sinnema G. Quality of life: patients and doctors don’t always agree: a meta-analysis. J Clin Epidemiol. 2004;57:653–661. doi: 10.1016/j.jclinepi.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 16.Jorn LP, Johnsson R, Toksvig-Larsen S. Patient satisfaction, function and return to work after knee arthroplasty. Acta Orthop Scand. 1999;70:343–347. doi: 10.3109/17453679908997822. [DOI] [PubMed] [Google Scholar]
- 17.Kane R, Saleh K, Wilt T, Bershadsky B, Cross III W, MacDonald R, Rutks I. Total knee replacement. Evidence report. Technology Assessment (Prepared by the Minnesota Evidence—Based Practice Center, Minneapolis, MN). AHRQ Publication, No. 04-E006-2; 2003;8:1–8. [PMC free article] [PubMed]
- 18.Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, Lingard EA, Harris WH, Poss R, Lew RA, Guadagnoli E, Wright EA, Losina E. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560–568. doi: 10.1002/art.10754. [DOI] [PubMed] [Google Scholar]
- 19.Mahomed N, Sledge C, Daltroy L, Fossel A, Katz J. Self-administered satisfaction scale for joint replacement arthroplasty. J Bone Joint Surg Br. 1998;80(Suppl 1):9. [Google Scholar]
- 20.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 21.Mantyselka P, Kumpusalo E, Ahonen R, Takala J. Patients’ versus general practitioners’ assessments of pain intensity in primary care patients with non-cancer pain. Br J Gen Pract. 2001;51:995–997. [PMC free article] [PubMed] [Google Scholar]
- 22.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 23.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27, 372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 24.Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–1293. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- 25.Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14:417–423. doi: 10.1016/j.knee.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 26.Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br. 2008;90:1172–1179. doi: 10.1302/0301-620X.90B9.21031. [DOI] [PubMed] [Google Scholar]