Abstract
The range of motion after TKA depends on many patient, surgical technique, and implant factors. Recently, high-flexion designs have been introduced as a means of ensuring or gaining flexion after TKA. We therefore evaluated factors affecting postoperative flexion to determine whether implant design influences longterm flexion. We prospectively collected data on patients receiving a primary Genesis II™ total knee replacement with a minimum of 1-year followup (mean, 5.4 years; range, 1–13 years). We recorded pre- and postoperative outcome measures, patient demographics, and implant design (cruciate retaining [CR, n = 160], posterior stabilized [PS, n = 1177], high-flex posterior stabilized [HF-PS, n = 197]). Backward stepwise linear regression modeling identified the following factors affecting postoperative flexion: preoperative flexion, gender, body mass index, and implant design. Independent of gender, body mass index, and preoperative flexion, patients who received a HF-PS and PS design implant had a mean of 8° and 5° more flexion, respectively, than those who received a CR implant. Patients with low flexion preoperatively (< 100°) were more likely to gain flexion, whereas those with high flexion preoperatively (> 120°) were most likely to maintain or lose flexion postoperatively. Controlling for implant design, patients with high flexion preoperatively (> 120°) were more likely to gain flexion with the HF-PS design implant (HF-PS = 32.0%; PS = 15.1%; CR = 4.5%).
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Although knee arthroplasty is highly successful by providing considerable relief of pain, improving function, and restoring quality of life, some patients remain dissatisfied with TKA. Robertsson et al. [30] reported a substantial number of patients (approximately 20%), based on Swedish knee registry data, remain either unsatisfied or uncertain of the benefits of their TKA [30]. Similarly, 17% of patients undergoing TKA in the Ontario Joint Replacement Registry remain uncertain or not satisfied with their TKA [1]. Although the reasons for patient dissatisfaction are varied, poor range of motion (10%) and anterior knee pain (5%–10%) were listed as leading causes of dissatisfaction [1].
The range of motion after TKA depends on many patient, surgical technique, and implant factors, the most important of which is likely the preoperative range of motion [8, 9, 15, 19, 24, 33]. Although it remains controversial whether knee design, specifically posterior cruciate retaining or sacrificing knees, are superior with respect to range of motion [6, 7, 9, 15, 18, 25, 33], there have been several design changes aimed at improving knee flexion. These include changes in the polyethylene geometry, changes in the posterior femoral condylar offset and geometry, changes to the cam/post engagement in posterior stabilized knee designs, or a combination of these [2–4, 14, 23, 29, 36].
One approach has been to modify the tibial polyethylene insert to enhance both range of motion and minimize extensor mechanism impingement, a potential cause of anterior knee pain. We hypothesized maximum postoperative flexion would correlate with preoperative flexion but that polyethylene/knee design would have little or no influence on flexion. In other words, after accounting for the role of preoperative flexion and other potential variables, there would be little or no difference among cruciate retaining (CR), posterior stabilized (PS) and high flexion (HF-PS) knee replacements. However, if knee design is a major factor, we sought to explore whether this relationship was dependent on preoperative flexion. In other words, would patients with a certain preoperative flexion benefit most from a certain polyethylene design?
Our purpose was therefore to determine which if any factors influence postoperative range of motion and if polyethylene type within a single knee design influenced postoperative flexion.
Patients and Methods
We retrospectively reviewed the prospectively collected data of 1282 patients (1534 knees): 160 with CR implant, 1177 with a PS implant, and 197 with a HF-PS implant, all part of the Genesis II™ total knee system (Smith & Nephew, Memphis, TN). Four surgeons (RWM, SJM, RBB, DDN) have used this system since 1996. During this time, preoperative and postoperative outcome data have been collected prospectively in our arthroplasty database. Specifically, range-of-motion data were measured by the consultant surgeon, fellow, or study nurse using a goniometer. All data were transferred from customized data capture forms to the database by a dedicated data entry clerk. The database, used since 1996, is now an internationally recognized data capture system for leading healthcare organizations (Ortech Data Centre Inc, London, Ontario, Canada). All surgeons are high-volume arthroplasty surgeons (each performing more than 100 TKAs per year) working in a teaching hospital environment.
All surgeons used a standard medial parapatellar approach and balance the knee with flexion/extension spacers. Initially, both a CR and PS femoral implant and corresponding polyethylene were used at the discretion of the individual surgeons. In the early years (1996–2002), CR and PS knees were performed in relatively equal numbers in which PS implants were reserved for knees with greater deformity (greater than 15°), posterior cruciate ligament deficiency, patients with rheumatoid arthritis, and after high tibial osteotomy or patellectomy. From 2002 onward, the PS knee design was the implant of choice for the majority of TKAs. Beginning in December 2004, the Genesis II HF-PS polyethylene design has been available for implantation at our institution. Initially, the HF-PS inserts were used as part of a randomized, controlled trial comparing the results with the standard PS inserts [26]. In the past several years, it has become the predominant polyethylene for PS knee replacements.
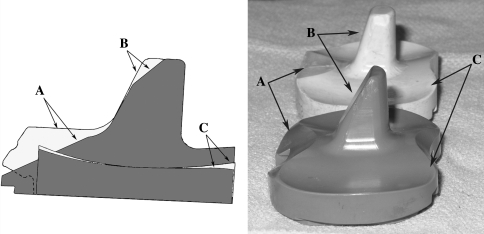
The high-flex knee system uses the standard PS femoral component and a dedicated high-flex polyethylene insert. The high-flex insert has several key design changes. There is a cutout or recession of the polyethylene along the anterior aspect of the insert and the proximal anterior portion of the post to decrease the potential for impingement of either the patella or extensor mechanism with high degrees of flexion. In addition, there are changes in the radius of curvature of the posterior portion of the articulating surface of the polyethylene to allow better femoral rollback (Fig. 1).
Fig. 1.
Schematic showing differences between standard posterior stabilized (white, background) and high-flex posterior stabilized (gray, foreground) polyethylene inserts. (A) The cutout of polyethylene at the anterior aspect of the inserts is shown. (B) The slope of the polyethylene at the proximal anterior portion of the post is demonstrated. (C) Changes in the radius of curvature of the posterior portion of the articulating surfaces are shown.
Our orthopaedic database was queried to identify those cases with a primary Genesis II TKA (CR, PS, or HF-PS polyethylene) with a minimum 1-year postoperative followup. To be included in the final analysis, the following information was required for each case: primary TKA with Genesis II implant (CR, PS, HF-PS), minimum 1-year followup, preoperative flexion measurement, postoperative flexion measurement, preoperative WOMAC outcome score, and known gender, age, and body mass index (BMI).
Based on our inclusion criteria, we included 1534 cases in the regression model and other analyses: CR (n = 160), PS (n = 1177), and HF-PS (n = 197). We observed no preoperative differences in patient demographics between groups (Table 1). Similarly, we found no difference in preoperative flexion between groups. However, on average, there was a slight loss in knee flexion (−0.4 ± 14.1°, mean ± SD) for the CR patients compared with an average gain of knee flexion for both the PS and HF-PS groups (7.4° ± 16.0° and 9.7° ± 20.3°, respectively, p < 0.0001; Table 1).
Table 1.
Demographic and flexion variables grouped by TKA implant design
| Demographic and flexion variables | CR | PS | HF-PS | Significance |
|---|---|---|---|---|
| Number (n) cases | 160 | 1177 | 197 | NA |
| Male:female (n, %) | 61 (38%):99 (62%) | 495 (42%):682 (58%) | 84 (43%):113 (57%) | 0.615 |
| Diagnosis of osteoarthritis (n,%) | 147, 92% | 1076, 91% | 177, 90% | 0.161 |
| Age (years, mean ± SD) | 67.47 ± 8.44 | 67.82 ± 9.66 | 65.93 ± 10.54 | > 0.056 |
| Height (cm, mean ± SD) | 164.89 ± 8.28 | 165.07 ± 10.88 | 165.54 ± 10.36 | > 0.890 |
| Weight (kg, mean ± SD) | 87.28 ± 14.78 | 89.19 ± 19.62 | 89.66 ± 21.20 | > 0.378 |
| Body mass index (mean ± SD) | 32.12 ± 5.15 | 32.76 ± 6.76 | 32.71 ± 7.25 | > 0.410 |
| Preoperative flexion (degrees, mean ± SD) | 112.17 ± 13.46 | 109.40 ± 16.13 | 109.98 ± 17.54 | > 0.054 |
| Postoperative flexion (degrees, mean ± SD) | 111.78 ± 11.11*1,2 | 116.78 ± 11.51*1 | 119.65 ± 12.59*2 | p < 0.0001*1,2 |
| Change in flexion (degrees, mean ± SD) | −0.39 ± 14.05*1,2 | 7.38 ± 15.98*1 | 9.67 ± 20.37*2 | p < 0.0001*1,2 |
* Significant variables determined by analysis of variance with Bonferroni or Tamhane’s post hoc method for continuous variables and crosstabulation with chi square for categorical variables; level of significance set at 0.05; for postoperative flexion and change in flexion, CR was significantly lower than both PS and HF-PS; CR = cruciate retaining; PS = posterior stabilized; HF = high flex; NA = not applicable.
We used univariate analysis to explore any differences among the three Genesis II™ knee design groups. For continuous variables (ie, height, age, BMI, preoperative flexion, postoperative flexion, change in flexion), analysis of variance was used with either Bonferroni or Tamhane’s post hoc tests. Categorical variables (ie, gender, primary diagnosis) were analyzed using crosstabulation with chi square. We then conducted a multivariate analysis (backward stepwise linear regression) to determine which variables influenced postoperative flexion and to determine if implant design was among these variables. To accommodate categorical variables in the model (ie, gender, polyethylene design), dummy coding was used. For gender, male is tested in the regression model with female being the reference category. For polyethylene design, HF-PS and PS are represented in the model and CR was the reference design. Variables that were nonsignificant predictors of the flexion outcome were eliminated in a backward stepwise fashion until only those that were significant remained. Thus, variables included in the final linear regression model were all significant copredictors of postoperative flexion.
We believed it was important to further explore the relationship between preoperative flexion and postoperative flexion outcome (based on the presumption that preoperative flexion would not have a linear affect on postoperative flexion) as well as to further understand how the influence of a specific implant design may differ depending on the patient’s preoperative motion. In other words, regardless of implant type, did patients with poor preoperative flexion (or high preoperative flexion) tend to lose, gain, or stay the same with respect to postoperative flexion? In addition, what, if any, was the influence of implant type based on the patient’s preoperative flexion? To accommodate this analysis, preoperative flexion was divided into equal quartiles (based on the 25th, 50th, and 75th percentiles of the preoperative flexion data) resulting in four preoperative flexion groups: < 100°; 100°–110°; 110°–120°; and ≥ 120°. Similarly, postoperative flexion outcome was divided into three groups: those who lost flexion (> 5° or more loss from preoperative); those who maintained flexion (± 5° of preoperative flexion); and those who gained flexion (> 5° gain from preoperative). Crosstabulation with chi square was then used for all analyses in which the level of significance was set to 0.05. All statistical analyses were performed with SPSS Version 17 (SPSS Inc, Chicago, IL).
Results
Gender, BMI, preoperative flexion, and implant design predicted flexion outcome in the linear regression model (Table 2). Specifically, increasing preoperative flexion correlated with increased postoperative flexion. Male gender was also associated with higher postoperative flexion, whereas increasing BMI was associated with decreased postoperative flexion. Independent of gender, BMI, and preoperative flexion, the use of a HF-PS and PS design implant resulted in a postoperative flexion increase of 8.2° and 5.6°, respectively, compared with a CR implant (β values) (Table 2). Interpretation of the standardized coefficients in the regression model, which are a measure of each variable’s effect on the dependent variable, revealed preoperative flexion had the strongest effect on postoperative flexion, closely followed by implant design, then BMI, and lastly, gender (Table 2).
Table 2.
Variables significant to 1 year flexion outcome
| Variables in linear regression | β Coefficient | 95% C.I. for β | Standardized coefficient | Significance | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender (male) | 1.675 | 0.529 | 2.820 | 0.070 | 0.004 |
| Body mass index | −0.197 | −0.283 | −0.111 | −0.112 | < 0.0001 |
| Preoperative flexion | 0.209 | 0.173 | 0.245 | 0.286 | < 0.0001 |
| HF-PS implant compared with CR | 8.199 | 5.900 | 10.499 | 0.232 | < 0.0001 |
| PS implant compared with CR | 5.613 | 3.799 | 7.428 | 0.201 | < 0.0001 |
β = unstandardized coefficients of independent variables to post operative flexion; HF-PS = high-flex posterior stabilized; CR = cruciate retaining; C.I. = Confidence Interval.
Regardless of implant type used, increasing preoperative flexion was associated with an increased probability (p < 0.0001) of a loss in flexion (Table 3). In other words, patients with the lowest preoperative flexion (0°–100°) improved the most postoperatively, whereas patients with high preoperative flexion (> 120°) were the most likely to stay the same or lose flexion. When the influence of knee implant design was added to the analysis (Table 4), the use of a HF-PS implant was associated with the greatest percentage of patients who gained flexion postoperatively in each of the preoperative flexion groups (except for the low flexion group in which implant type had no effect). In other words, the use of a HF-PS implant was most associated with an improvement in postoperative flexion (32%) in those patients with higher preoperative flexion (> 120°). In contrast, the use of a CR implant in these patients with high flexion was most often associated with loss of flexion (60%).
Table 3.
Cross tabulation of preoperative flexion quartiles to flexion outcome group
| Preoperative flexion quartiles | Loss in flexion (< −5) | No change in flexion | Gain in flexion (> 5) |
|---|---|---|---|
| 0–25th percentile(< 100°) | 2.2% | 11.1% | 89.7% |
| 25th–50th percentile (100°–110°) | 4.3% | 21.9% | 73.8% |
| 50th–75th percentile (110°–120°) | 11.7% | 38.4% | 49.9% |
| 75th percentile (≥ 120°) | 76.5% | 55.7% | 12.8% |
Crosstabulation with Pearson chi square was highly significant (p < 0.0001) , suggesting as preoperative flexion quartile increases, there is a significant decrease in the percentage of those that gain flexion postoperatively.
Table 4.
Cross tabulation of preoperative flexion quartiles and flexion outcome group to TKA implant design group
| Preoperative flexion quartiles | Postoperative flexion outcome | CR | PS | HF-PS | Significance |
|---|---|---|---|---|---|
| 0–25th percentile (< 100°) | Loss in flexion | 0.0% | 2.7% | 0.0% | |
| No change in flexion | 13.0% | 10.5% | 14.0% | 0.684 | |
| Gain in flexion | 87.0% | 86.8% | 86.0% | ||
| 25th–50th percentile (100°–110°) | Loss in Flexion | 6.9% | 4.5% | 0.0% | |
| No change in flexion | 41.4% | 20.1% | 12.0% | 0.031 | |
| Gain in flexion | 51.7% | 75.4% | 88.0% | ||
| 50th– 75th percentile (110°–120°) | Loss in flexion | 26.8% | 10.0% | 9.3% | |
| No change in flexion | 51.2% | 38.3% | 29.6% | 0.001 | |
| Gain in flexion | 22.0% | 51.7% | 61.1% | ||
| 75th percentile (≥ 120°) | Loss in flexion | 59.7% | 31.3% | 28.0% | |
| No change in flexion | 35.8% | 53.6% | 40.0% | < 0.0001 | |
| Gain in flexion | 4.5% | 15.1% | 32.0% |
Underlined value within each preoperative flexion quartile are those that are highest in each postoperative flexion category; note that in the 2nd through 4th quartiles, the HF-PS demonstrates the greatest percentage of subjects gaining flexion; significance tested with crosstabulation with chi square method; significance within each preoperative flexion quartile suggests the distribution of the data across flexion outcome and polyethylene design is not to chance, therefore verifying that polyethylene design has an effect on flexion outcome; CR = cruciate retaining PS = posterior stabilized; HF-PS = high-flex posterior stabilized.
Discussion
The range of motion after TKA depends on many patient, surgical technique, and implant factors. Recently, high-flexion designs have been introduced as a means of ensuring or gaining flexion after TKA. Our purpose was therefore to investigate which factors influence postoperative range of motion and, specifically, if the polyethylene type within a single knee implant design influenced motion. We hypothesized postoperative flexion would correlate with preoperative flexion and that polyethylene/knee design would have little or no influence. However, if knee design is a major factor, we sought to explore whether patients with a certain preoperative flexion would benefit most from a certain polyethylene design.
We acknowledge several limitations. First, we included patients from four surgeons that may introduce some selection bias and/or subtle differences in surgical technique (although it could be considered an advantage because it resulted in a “better mix” of our sample and may strengthen the external validity). Second, there are disparate numbers of patients in each group (the vast majority being PS knees) representing differences in surgical practice and implant availability over the period of study. However, the large numbers in each group provided adequate statistical power. Third, we somewhat arbitrarily categorized the preoperative and postoperative flexion data (based on equal quartiles of the preoperative data and clinically relevant postoperative groupings), which may have influenced the results. However, we had relatively large numbers, prospectively collected data, and a single implant design (ie, Genesis II™). Finally, although not a randomized trial, the cohorts were essentially identical preoperatively (with respect to demographics and range of motion).
Postoperative flexion after TKA is undoubtedly related to several patient, surgical technique, and implant design factors. The results of our linear regression analysis confirmed our initial hypothesis that preoperative flexion was an important determinant of postoperative flexion. This was not unexpected because there is substantial previous work demonstrating the importance of preoperative flexion [9, 15, 19, 24, 33]. Also important to the model were the patient’s gender (male gender associated with increased postoperative flexion) and BMI (increasing obesity associated with decreased postoperative flexion). The positive effect of male gender is difficult to explain clinically and, although statistically significant, the effect was relatively small (based on the variable’s standardized beta coefficient within the model) and we are unaware of other literature reporting this finding. On the other hand, the negative effect of increasing BMI is much easier to understand in the clinical setting and is supported by several studies [10, 11, 16, 27, 28, 34, 38].
Contrary to our initial hypothesis, the linear regression model analysis demonstrated the polyethylene type/design did influence the postoperative flexion. In particular, independent of gender, BMI, and preoperative flexion, the use of a HF-PS and PS design implant resulted in a postoperative flexion increase of 8.2° and 5.6°, respectively, compared with a CR implant. Similarly, comparison of preoperative to postoperative flexion for each patient demonstrated those patients receiving a CR knee had, on average, no improvement in flexion (−0.4° ± 14.0°, mean ± SD) compared with an average increase of 7.4° ± 16.0° and 9.7° ± 20.4° for PS and HF-PS knees, respectively. The positive benefit to a PS knee design (over CR) was not completely expected because previous work remains controversial whether CR or PS knees are advantageous with respect to postoperative range of motion [6, 7, 9, 15, 18, 25].
Categorization of the preoperative and postoperative flexion into groups revealed the use of a HF-PS implant was associated with the greatest percentage of patients who gained flexion postoperatively in each of the preoperative flexion groups (except for the low flexion group in which implant type had no effect). The fact that all forms of analysis in this study demonstrated a potential advantage to the HF-PS design was somewhat surprising because a recently published randomized, controlled trial (comparing 50 PS with 50 HF-PS Genesis II™ knees) performed at our institution failed to show a difference in postoperative range of motion between groups [26]. It is likely our randomized, controlled trial was underpowered to demonstrate the findings of this large database review series.
Other clinical results in the literature for high-flexion knee replacements have been quite variable. Several studies have demonstrated improved range of motion when comparing standard PS or CR with HF designs [5, 12, 17, 22, 37]. In contrast, other studies, including several randomized, controlled trials, have demonstrated little or no difference between high-flex and conventional knee designs [8, 20–22, 31, 32, 35, 39]. The potential downside of a high-flexion knee design is well illustrated in a paper from Han et al. [13], who reported on a 38% aseptic loosening and 21% revision rate in 72 high-flexion knees. Their paper demonstrated a clear association of loosening with those patients who achieved high flexion.
In summary, our data demonstrate postoperative range of motion after TKA is related to several factors, confirming the important role of the patient’s preoperative range of motion. In addition, our review suggests knee design and, in particular, the use of a so-called “high-flexion” PS polyethylene design may be advantageous in maintaining or improving flexion postoperatively, especially in those patients with good preoperative range of motion.
Footnotes
The institution of the authors has received funding from Smith & Nephew (Memphis TN) for some of the patients included in this analysis who were part of a randomized controlled study. One of more of the authors (RWM, RBB, DDN) act as consultants for Smith & Nephew (Memphis, TN) although no payments were received related to this work.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anderson CK, Bourne RB, Chesworth BM, Cipriano LM, Warner S, Zaric GS. Looking Forward to 2015: Comparing Wait List Management Options. London, Ontario: Ontario Joint Replacement Registry; March 2006.
- 2.Arabori M, Matsui N, Kuroda R, Mizuno K, Doita M, Kurosaka M, Yoshiya S. Posterior condylar offset and flexion in posterior cruciate-retaining and posterior stabilized TKA. J Orthop Sci. 2008;13:46–50. doi: 10.1007/s00776-007-1191-5. [DOI] [PubMed] [Google Scholar]
- 3.Argenson JN, Scuderi GR, Komistek RD, Scott WN, Kelly MA, Aubaniac JM. In vivo kinematic evaluation and design considerations related to high flexion in total knee arthroplasty. J Biomech. 2005;38:277–284. doi: 10.1016/j.jbiomech.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 4.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620X.84B1.12432. [DOI] [PubMed] [Google Scholar]
- 5.Bin SI, Nam TS. Early results of high-flex total knee arthroplasty: comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–355. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhary R, Beaupre LA, Johnston DW. Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am. 2008;90:2579–2586. doi: 10.2106/JBJS.G.00995. [DOI] [PubMed] [Google Scholar]
- 7.Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D. Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res. 2001;392:208–212. doi: 10.1097/00003086-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Dennis DA, Komistek RD, Scuderi GR, Zingde SM. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007;464:53–60. doi: 10.1097/BLO.0b013e31812f785d. [DOI] [PubMed] [Google Scholar]
- 9.Dennis DA, Komistek RD, Stiehl JB, Walker SA, Dennis KN. Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty. 1998;13:748–752. doi: 10.1016/S0883-5403(98)90025-0. [DOI] [PubMed] [Google Scholar]
- 10.Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004;86:1609–1615. doi: 10.2106/00004623-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19:817–824. doi: 10.1016/j.arth.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS. The PFC sigma RP-F TKA designed for improved performance: a matched-pair study. Orthopedics. 2006;29(Suppl):S49–S52. [PubMed] [Google Scholar]
- 13.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89:1457–1461. doi: 10.1302/0301-620X.89B11.19840. [DOI] [PubMed] [Google Scholar]
- 14.Hanratty BM, Thompson NW, Wilson RK, Beverland DE. The influence of posterior condylar offset on knee flexion after total knee replacement using a cruciate-sacrificing mobile-bearing implant. J Bone Joint Surg Br. 2007;89:915–918. doi: 10.1302/0301-620X.89B7.18920. [DOI] [PubMed] [Google Scholar]
- 15.Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD. Midterm comparison of posterior cruciate-retaining versus -substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee. 2008;15:217–221. doi: 10.1016/j.knee.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: a minimum of 2 years of follow-up. J Arthroplasty. 2005;20:674–679. doi: 10.1016/j.arth.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs WC, Clement DJ, Wymenga AB. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop. 2005;76:757–768. doi: 10.1080/17453670510045345. [DOI] [PubMed] [Google Scholar]
- 19.Kawamura H, Bourne RB. Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci. 2001;6:248–252. doi: 10.1007/s007760100043. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Choi Y, Kwon OR, Kim JS. Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am. 2009;91:753–760. doi: 10.2106/JBJS.H.00805. [DOI] [PubMed] [Google Scholar]
- 21.Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475. doi: 10.2106/JBJS.D.02707. [DOI] [PubMed] [Google Scholar]
- 22.Laskin R. The effect of a high-flex implant on postoperative flexion after primary total knee arthroplasty. Orthopedics. 2007;30(Suppl):86–88. [PubMed] [Google Scholar]
- 23.Maloney WJ, Schurman DJ. The effects of implant design on range of motion after total knee arthroplasty. Total condylar versus posterior stabilized total condylar designs. Clin Orthop Relat Res. 1992;278:147–152. [PubMed] [Google Scholar]
- 24.Malviya A, Lingard EA, Weir DJ, Deehan DJ. Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc. 2009;17:491–498. doi: 10.1007/s00167-008-0712-x. [DOI] [PubMed] [Google Scholar]
- 25.Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:349–353. doi: 10.1016/j.arth.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 26.McCalden RW, Macdonald SJ, Bourne RB, Marr JT. A randomized controlled trial comparing ‘high-flex’ vs ‘standard’ posterior cruciate substituting polyethylene tibial inserts in total knee arthroplasty. J Arthroplasty. 2009 May 14 [Epub ahead of print]. [DOI] [PubMed]
- 27.Pritchett JW, Bortel DT. Knee replacement in morbidly obese women. Surg Gynecol Obstet. 1991;173:119–122. [PubMed] [Google Scholar]
- 28.Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23:795–800. doi: 10.1016/j.arth.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Ranawat CS. Design may be counterproductive for optimizing flexion after TKR. Clin Orthop Relat Res. 2003;416:174–176. doi: 10.1097/01.blo.0000093028.56370.46. [DOI] [PubMed] [Google Scholar]
- 30.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27, 372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 31.Seon JK, Park SJ, Lee KB, Yoon TR, Kozanek M, Song EK. Range of motion in total knee arthroplasty: a prospective comparison of high-flexion and standard cruciate-retaining designs. J Bone Joint Surg Am. 2009;91:672–679. doi: 10.2106/JBJS.H.00300. [DOI] [PubMed] [Google Scholar]
- 32.Seon JK, Song EK, Lee JY. Comparison of range of motion of high-flexion prosthesis and mobile-bearing prosthesis in total knee arthroplasty. Orthopedics. 2005;28(Suppl):s1247–s1250. doi: 10.3928/0147-7447-20051002-08. [DOI] [PubMed] [Google Scholar]
- 33.Shi MG, Lu HS, Guan ZP. Influence of preoperative range of motion on the early clinical outcome of total knee arthroplasty [in Chinese] Zhonghua Wai Ke Za Zhi. 2006;44:1101–1105. [PubMed] [Google Scholar]
- 34.Stickles B, Phillips L, Brox WT, Owens B, Lanzer WL. Defining the relationship between obesity and total joint arthroplasty. Obes Res. 2001;9:219–223. doi: 10.1038/oby.2001.24. [DOI] [PubMed] [Google Scholar]
- 35.Suggs J, Kwon Y-M, Durbhakula S, Hanson G, Li G. In vivo flexion and kinematics of the knee after TKA: comparison of a conventional and a high flexion cruciate-retaining TKA design. Knee Surg Sports Traumatol Arthrosc. 2009;17:150–156. doi: 10.1007/s00167-008-0637-4. [DOI] [PubMed] [Google Scholar]
- 36.Sultan PG, Most E, Schule S, Li G, Rubash HE. Optimizing flexion after total knee arthroplasty: advances in prosthetic design. Clin Orthop Relat Res. 2003;416:167–173. doi: 10.1097/01.blo.0000081937.75404.ee. [DOI] [PubMed] [Google Scholar]
- 37.Weeden SH, Schmidt R. A randomized, prospective study of primary total knee components designed for increased flexion. J Arthroplasty. 2007;22:349–352. doi: 10.1016/j.arth.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 38.Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80:1770–1774. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Wohlrab D, Ditl J, Herrschelmann R, Schietsch U, Hein W, Hube R. Does the NexGen LPS flex mobile knee prosthesis offer advantages compared to the NexGen LPS?—A comparison of clinical and radiological results. Z Orthop Ihre Grenzgeb. 2005;143:567–572. doi: 10.1055/s-2005-836828. [DOI] [PubMed] [Google Scholar]