Abstract
While the occurrence of periprosthetic fractures around total knee arthroplasties (TKAs) is well know, little is known about intraoperative fractures that occur during TKA. We describe the incidence, location, and outcomes of iatrogenic intraoperative fracture during primary TKA. We reviewed 17,389 primary TKAs performed between 1985 and 2005 and identified 66 patients with 67 intraoperative fractures including 49 femur fractures, 18 tibia fractures, and no patella fractures. There were 12 men and 54 women with a mean age of 65.2 ± 16 years. Of the 49 femur fractures, locations included medial condyle (20), lateral condyle (11), supracondylar femur (eight), medial epicondyle (seven), lateral epicondyle (two), and posterior cortex (one). Tibia fractures (18) included lateral plateau (six), anterior cortex (four), medial plateau (three), lateral cortex (three), medial cortex (one), and posterior cortex (one). Twenty-six fractures occurred during exposure and preparation, 22 while trialing, 13 during cementation, and three while inserting the polyethylene spacer. The minimum followup was 0.15 years (mean, 5.1 years; range, 0.15–15.4 years). All fractures healed clinically and radiographically. Knee Society scores and function scores improved from 46.4 and 34.6 to 79.5 and 61, respectively. Fourteen of the 66 (21%) patients were revised at an average of 2.8 years. Intraoperative fracture is an uncommon complication of primary TKA with a prevalence of 0.39%. Intraoperative fracture occurred more commonly in women (80.6%) and in the femur (73.1%). The majority of fractures occurred during exposure and bone preparation and trialing of the components.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The occurrence of postoperative fractures around knee prostheses is well known. Risk factors of periprosthetic fractures include osteoporosis, anterior cortical notching, chronic steroid use, advanced age, female gender, and neurologic disorders [1, 3–5, 7, 12, 16]. More recently, with the increased use of computer-assisted TKA, cortical defects from navigation pins have led to some postoperative fractures [11, 17]. Fractures can potentially occur at any stage of the TKA including exposure, bone preparation, placement of trial components, cementation, insertion of the final components, and seating of the polyethylene insert. Options for treatment include observation, internal fixation, the use of stems and augments, increasing constraint of the prosthesis, and modifying the postoperative rehabilitation. The outcomes of iatrogenic intraoperative fractures, however, are not well described in the literature.
We therefore identified the incidence, steps during surgery when the fractures occurred, location and relationship to type of implant, treatments instituted, and clinical and radiographic outcome of these fractures.
Materials and Methods
From our database of 17,389 primary TKAs performed between 1985 and 2005 we identified and reviewed the records of 66 patients with 67 intraoperative fractures including 49 femur fractures, 18 tibia fractures, and no patella fractures. Nine patients had bilateral TKAs under the same anesthetic; one of the patients undergoing bilateral TKAs sustained bilateral fractures, one in the femur and one in the tibia. There were 12 men and 54 women with a mean age of 65.2 ± 16 years, a majority of whom (57%) had osteoarthritis. Underlying diagnoses leading to recalcitrant arthritis included primary osteoarthritis (57.4%), posttraumatic arthritis (11.8%), and rheumatoid arthritis (11.8%) (Table 1). The average body mass index was 29.25 ± 6.08 (range, 17.59–49.87). From the medical records we recorded demographic data including site of fracture, steps during surgery when the fracture occurred, type of implant, treatment, and outcome were documented; no patients were seen in followup specifically for this study. Twenty of the 66 patients died at a mean of 3.9 years after index TKA and had well-functioning arthroplasties at the time of last clinical followup. The minimum followup was 0.15 years (mean, 5.1 years; range, 0.15–15.4 years). We obtained prior Institutional Review Board approval.
Table 1.
Underlying diagnoses leading to end-stage knee arthritis
| Underlying diagnosis | Number (%) | |
|---|---|---|
| Fracture group | Sample population | |
| Osteoarthritis | 39 (57.3%) | 14,654 (84.2%) |
| Posttraumatic arthritis | 8 (11.76%) | 1195 (6.88%) |
| Rheumatoid arthritis | 8 (11.76%) | 640 (3.69%) |
| Osteonecrosis | 3 (4.41%) | 409 (2.36%) |
| Prior arthrodesis | 2 (2.9%) | 37 (0.21%) |
| Juvenile rheumatoid arthritis | 2 (2.9%) | 44 (0.25%) |
| Charcot arthropathy | 1 (1.5%) | 5 (0.028%) |
| Dwarfism: Morquio’s syndrome | 1 (1.5%) | 4 (0.023%) |
| Failed prior surgery: osteotomy | 1 (1.5%) | 3 (0.017%) |
| Osteogenesis imperfecta | 1 (1.5%) | 3 (0.017%) |
| Psoriatic arthritis | 1 (1.5%) | 24 (0.14%) |
| Systemic lupus erythematosus | 1 (1.5%) | 3 (0.017%) |
We recorded the preoperative and postoperative clinical function from the records using the Knee Society criteria [9]. Two of us (KA, WD; neither treating physicians) determined the state of fracture healing using the most recent available radiographs, classifying as healed (radiographic evidence of bony trabeculation across fracture site), not healed, or indeterminate. All patients with intraoperative fractures had serial postoperative radiographs followed either until death of the patient or need for revision surgery. Component fixation using the Knee Society radiographic criteria was also assessed [6].
Statistical analysis was performed using the two-sample test or Wilcoxon rank sum test for comparison of continuous variables. Changes in the continuous variables were assessed using the paired t tests or signed rank test. Comparison of proportions between groups was made with the χ2 test or Fisher exact test [10].
Results
We identified 66 patients with 67 intraoperative fractures, an incidence of 0.39% from among the 17,389 TKAs. We identified 64 of the 67 fractures intraoperatively. Three (4%) fractures were nondisplaced, not detected intraoperatively, and were diagnosed after obtaining postoperative radiographs. All three of these patients were treated with touch weight bearing for 6 weeks.
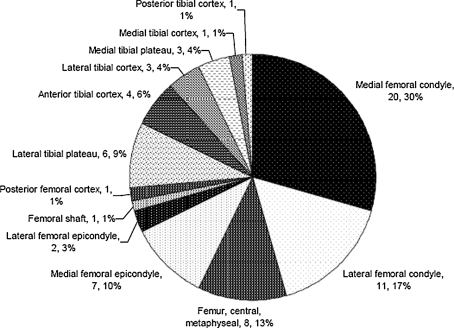
There were 49 femur fractures, 18 tibia fractures, and no patella fractures. Fractures occurred in 29 left knees and 38 right knees. Of the 49 femur fractures, locations included medial condyle (20), lateral condyle (11), supracondylar femur (eight), medial epicondyle (seven), lateral epicondyle (two), and posterior cortex (one). Tibia fractures (18) included lateral plateau (six), anterior cortex (four), medial plateau (three), lateral cortex (three), medial cortex (one), and posterior cortex (one). Twelve patients had at least one ipsilateral surgical procedure before the primary TKA including five open reduction-internal fixations, five distal osteotomies, one arthrodesis, and one patellectomy.
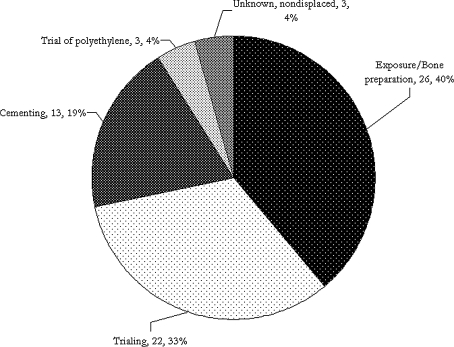
The majority of fractures occurred during exposure and bone preparation (26, or 39%) and trialing of the components (22, or 33%) (Fig. 1). Twenty-six fractures occurred during exposure and preparation, 22 while trialing, 13 during cementation, and three while inserting the polyethylene spacer.
Fig. 1.
A pie chart illustrates the timing of intraoperative fractures during primary TKA; values are expressed as number of fractures and percentage of total fractures.
All implants were cemented and of a condylar-type design. Forty-eight were posterior-stabilized implants and nine were cruciate-retaining. The remainder (10 TKAs) included additional constraint, namely hinged components and one distal femoral replacement. The relative risk calculation demonstrated a femur fracture associated with a posterior-stabilized TKA (37 femur fractures in 8854) compared to a femur fracture in a cruciate-retaining TKA (seven in 7950) was 4.74. Of the nine fractures in the cruciate-retaining group, four occurred in the central metaphyseal region of the femur, two in the medial femoral condyle, one in the lateral femoral condyle, one in the anterior tibial cortex, and one in the medial tibial plateau (Fig. 2). Of the 48 fractures in the posterior-stabilized group, 15 occurred in the medial femoral condyle, nine in the lateral femoral condyle, seven in the medial femoral epicondyle, three in the central metaphyseal femur, two in the lateral femoral epicondyle, and one in the posterior femoral cortex. With respect to the tibial fractures in the posterior-stabilized group, the distribution included six in the lateral tibial plateau, two in the medial tibial plateau, one in the anterior tibial cortex, one in the medial tibial cortex, and one in the posterior tibial cortex. In the group undergoing constrained TKAs, there were three fractures in the medial femoral condyle, one in the lateral femoral condyle, one in the central metaphyseal femur, three in the lateral tibial cortex, and two in the anterior tibial cortex. One patient undergoing a posterior-stabilized TKA sustained a fracture through the medial femoral condyle and was converted intraoperatively to a hinged implant.
Fig. 2.
A pie chart illustrates the location of fractures during TKA; values are expressed as number of fractures and percentage of total fractures.
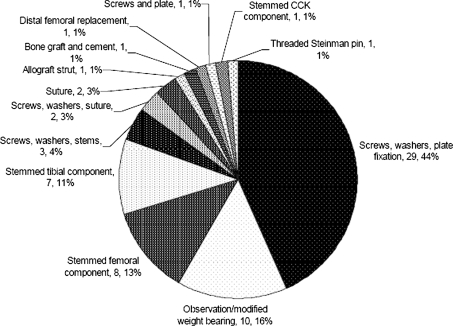
Ten of our 67 fractures were considered stable and treated with observation, while the remainder had additional intraoperative treatment. Treatment options varied, including screws, washers, and plate fixation (29); observation/modified weightbearing (10); stemmed femoral components (eight); stemmed tibial components (eight); screws, washers, stems (three); screws, washers, suture (two); suture (two); allograft strut (one); bone graft and cement (one); distal femoral replacement (one); screws and plate (one); stemmed constrained condylar knee component (one); and threaded Steinman pin (one) (Fig. 3). Some fractures were treated with combinations of the above (Figs. 4, 5).
Fig. 3.
A pie chart illustrates the treatment of fractures during TKA; values are expressed as number of fractures and percentage of total fractures; CCK = constrained condylar knee.
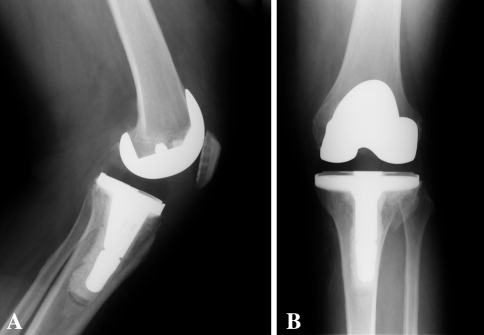
Fig. 4A–B.
(A) Anteroposterior and (B) lateral radiographs show an intraoperative medial femoral condyle fracture treated with plates and screws.
Fig. 5A–B.
(A) Anteroposterior and (B) lateral radiographs show an intraoperative lateral tibial plateau fracture treated with a stemmed tibial component.
All fractures healed clinically and radiographically. Knee extension improved from 7.1° preoperatively to 1.8° postoperatively. Knee flexion remained unchanged at 103°. The mean Knee Society score improved from 46.4 preoperatively to 79.5 postoperatively. The mean Knee Society function score increased from 34.5 preoperatively to 61 postoperatively.
Fourteen of the 66 patients (21%) underwent revision arthroplasty at an average of 2.8 years (range, 2 months to 12 years) after the index TKA. These 14 patients had an average age of 57 years (range, 15–87 years). We performed revisions for instability (four knees), loosening and osteolysis (four), infection (two), anterior knee pain in an unresurfaced patella (one), patellar maltracking (one), stiffness (one), and progression of metastatic disease (one). In the patients who underwent revision, fractures were located in the lateral femoral condyle (six), medial femoral condyle (four), medial femoral epicondyle (one), central metaphyseal femur (one), lateral tibial cortex (one), and lateral tibial plateau (one).
Discussion
The occurrence of postoperative fractures around knee prostheses is well known. The outcomes of iatrogenic intraoperative fractures, however, are not well described in the literature. We therefore documented the incidence, location, timing, and outcomes of intraoperative fracture during TKA.
Retrospective reviews have some inherent limitations but these are outweighed, we believe, by the large cohort of patients studied. Due to the small number of fractures relative to the total cohort it was not possible to assess the influence of medical comorbidities on the propensity for fracture.
Iatrogenic intraoperative fracture during primary TKA has received little attention in the orthopaedic literature. This may in part be due to the relative infrequency of such fractures. Intraoperative patella fractures have been reported during revision surgery [8] in patients with already thinned bone weakened by osteolysis, avascular necrosis, or comorbid conditions including osteoporosis and/or rheumatoid arthritis. Stuart and Hanssen [16] reported four intraoperative fractures of the lateral tibial cortex during primary TKAs associated with placement of the final components. Lombardi et al. [12] reviewed the complications of intraoperative distal femur intercondylar fractures, reporting 40 fractures in 898 primary posterior-stabilized TKAs (4.4%). The authors attribute this high fracture rate to intercondylar box cuts, which were slightly narrow or placed excessively medial or lateral, thereby weakening the respective condyle. This rate decreased to 0.2% (one of 532 TKAs) when they changed to a different implant and technique. In their series, 10 cases (0.07%) of iatrogenic intraoperative fracture during primary TKA were identified, but few details and little outcome data were reported in this subgroup.
We found an incidence of 0.39% for intraoperative fractures during primary TKA in a large series of patients. The majority of these occurred in women (80.6%) and in the femur (73.1%). Most often affected were the medial femoral condyle (30%) and lateral femoral condyle (17%), suggesting an excessive box cut associated with posterior-stabilized TKA may result in a fractured condyle in women with weakened bone. Our relative risk analysis demonstrated an increased risk of femur fracture with posterior-stabilized femoral components (relative risk of 4.74). The most common time for fracture was during exposure and bone preparation (39%) and while testing the trial components (33%). It has been postulated osteoporosis, female gender, chronic steroid use, advanced age, rheumatoid arthritis, and neurologic disorders predispose to postoperative periprosthetic fracture and may be factors important in intraoperative fractures [1, 4, 7, 12, 16].
Component design may additionally influence intraoperative fracture, as suggested by Lombardi et al. [12]. In their study, the authors suggest the box cut associated with the posterior-stabilized Insall-Burstein Constrained Condylar Knee II design (Zimmer, Inc, Warsaw, IN) may predispose to condylar fracture. Although the incidence of intraoperative fracture in our study was low, a majority occurred in posterior-stabilized TKAs, further suggesting caution with the box cut of the femoral component is warranted.
The plethora of fracture locations and diversity of treatment algorithms suggests it is difficult to recommend any particular treatment approach. However, most were individualized to the patient based on surgeon experience, fracture pattern, and bone quality. In general, fracture and arthroplasty principles should be followed to achieve stable fracture fixation and defects should be bypassed as necessary with stems.
The mean Knee Society scores improved from 46.4 to 79.5 and the mean Knee Society functional scores improved from 34.6 to 61. Two long-term followup studies of TKA using the Knee Society scores report mean clinical scores of 93 and 92 and mean functional scores of 71 and 78 [2, 15]. While the increase in scores was substantial in these patients, the intraoperative fracture may have influenced the overall lower score relative to previous studies. The reason for this may be multifactorial. Many of these patients were older than 75 years with other comorbidities.
Furthermore, the majority had their postoperative course altered secondary to the fracture. Fourteen of the 66 patients (21%) eventually underwent revision TKA. This relatively high revision rate may be due in part to this particular subset of patients in this study since they represent a population of patients more susceptible to perioperative complications and thus poorer outcomes. Of the patients who underwent revision TKAs, seven had previous knee surgery including three with prior tibial or femoral osteotomies, procedures generally associated with poorer outcome [13, 14]. In addition, two of the patients with prior osteotomies had severe bony deformities secondary to underlying diagnoses of osteogenesis imperfecta and Morquio’s syndrome.
Although we did not directly study ways to avoid intraoperative fractures, the following are reasonable things to do to hopefully minimize this complication from occurring. In patients with osteopenic bone, perform a liberal exposure freeing the medial and lateral gutters prior to flexing the knee. Perform a large medial release in varus knees prior to flexing the knee to ease tension on the medial collateral ligament with external rotation of the foot during flexion. If using a PS designed knee, be careful with medial-lateral placement to avoid a thin column of bone medially or laterally. Be gentle when performing trial reductions and during insertion of components in the presence of weak bone.
We found an incidence of intraoperative fracture during TKA of 0.4%. Fractures occurred more commonly in women, in posterior-stabilized designs, in the femur, and during exposure and bone preparation.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Mayo Clinic, Rochester, MN.
References
- 1.Chmell MJ, Moran MC, Scott RD. Periarticular fractures after total knee arthroplasty: principles of management. J Am Acad Orthop Surg. 1996;4:109–116. doi: 10.5435/00124635-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Colizza WA, Insall JN, Scuderi GR. The posterior stabilized total knee prosthesis: assessment of polyethylene damage and osteolysis after a ten-year-minimum follow-up. J Bone Joint Surg Am. 1995;77:1713–1720. doi: 10.2106/00004623-199511000-00011. [DOI] [PubMed] [Google Scholar]
- 3.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2007;165:1–209. [PubMed]
- 4.Dennis DA. Periprosthetic fractures following total knee arthroplasty. J Bone Joint Surg Am. 2001;83:120–130. doi: 10.1302/0301-620X.83B1.10632. [DOI] [PubMed] [Google Scholar]
- 5.Engh GA, Ammeen DJ. Periprosthetic fractures adjacent to total knee implants: treatment and clinical results. Instr Course Lect. 1998;47:437–448. [PubMed] [Google Scholar]
- 6.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 7.Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;345:113–124. doi: 10.1097/00003086-199712000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Gelinas JJ, Ries MD. Treatment of an intraoperative patellar fracture during revision total knee arthroplasty. J Arthroplasty. 2002;17:1066–1069. doi: 10.1054/arth.2002.34813. [DOI] [PubMed] [Google Scholar]
- 9.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 10.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 11.Li CH, Chen TH, Su YP, Shao PC, Lee KS, Chen WM. Periprosthetic femoral supracondylar fracture after total knee arthroplasty with navigation system. J Arthroplasty. 2008;23:304–307. doi: 10.1016/j.arth.2006.12.049. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Mallory TH, Waterman RA, Eberle RW. Intercondylar distal femoral fracture: an unreported complication of posterior-stabilized total knee arthroplasty. J Arthroplasty. 1995;10:643–650. doi: 10.1016/S0883-5403(05)80209-8. [DOI] [PubMed] [Google Scholar]
- 13.Nelson CL, Saleh KJ, Kassim RA, Windsor R, Haas S, Laskin R, Sculco T. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am. 2003;85:1062–1065. doi: 10.2106/00004623-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am. 2004;86:474–479. doi: 10.2106/00004623-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Ranawat CS, Luessenhop CP, Rodriguez JA. The press-fit condylar modular total knee system: four-to-six-year results with a posterior-cruciate-substituting design. J Bone Joint Surg Am. 1997;79:342–348. doi: 10.2106/00004623-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Stuart MJ, Hanssen AD. Total knee arthroplasty: periprosthetic tibial fractures. Orthop Clin North Am. 1999;30:279–286. doi: 10.1016/S0030-5898(05)70082-1. [DOI] [PubMed] [Google Scholar]
- 17.Wysocki RW, Sheinkop MB, Virkus WW, Della Valle CJ. Femoral fracture through a previous pin site after computer-assisted total knee arthroplasty. J Arthroplasty. 2008;23:462–465. doi: 10.1016/j.arth.2007.03.019. [DOI] [PubMed] [Google Scholar]