Abstract
Mechanical factors related to patellofemoral pain syndrome and maltracking are poorly understood. Clinically, the Q-angle, J-sign, and lateral hypermobility commonly are used to evaluate patellar maltracking. However, these measures have yet to be correlated to specific three-dimensional patellofemoral displacements and rotations. Thus, we tested the hypotheses that increased Q-angle, lateral hypermobility, and J-sign correlate with three-dimensional patellofemoral displacements and rotations. We also determined whether multiple maltracking patterns can be discriminated, based on patellofemoral displacements and rotations. Three-dimensional patellofemoral motion data were acquired during active extension-flexion using dynamic MRI in 30 knees diagnosed with patellofemoral pain and at least one clinical sign of patellar maltracking (Q-angle, lateral hypermobility, or J-sign) and in 37 asymptomatic knees. Although the Q-angle is assumed to indicate lateral patellar subluxation, our data supported a correlation between the Q-angle and medial, not lateral, patellar displacement. We identified two distinct maltracking groups based on patellofemoral lateral-medial displacement, but the same groups could not be discriminated based on standard clinical measures (eg, Q-angle, lateral hypermobility, and J-sign). A more precise definition of abnormal three-dimensional patellofemoral motion, including identifying subgroups in the patellofemoral pain population, may allow more targeted and effective treatments.
Introduction
Patellofemoral (PF) pain syndrome is one of the most common problems of the knee [6–8, 29, 33, 49]. Typical symptoms are anterior knee pain exacerbated by activities such as stair descent, prolonged sitting, and squatting. Patellar maltracking and malalignment generally are accepted as leading causes of PF pain [11, 15, 32, 46, 49]. However, the relationship between clinical pain and objective measures of patellar malalignment/maltracking is unclear. Clinical measures can provide static (eg, Q-angle [9, 13, 16, 17, 27, 32, 35, 45]) and dynamic (eg, lateral hypermobility, J-sign [10, 19, 30]) indicators of patellar malalignment/maltracking. Yet, clinical presentation is often subtle and inconsistent and these measures have yet to be correlated to specific three-dimensional (3D), objectively quantifiable displacement and rotations.
The Q-angle is one of the most frequently studied parameters in PF pain syndrome. A large Q-angle (≥ 15°–20º) is assumed to predispose an individual to PF pain owing to increased lateral patellar position (lateral subluxation) [4, 10, 35]. This angle is typically a static measurement taken with the patient in the supine position without quadriceps activation. Thus, a static measure is used to infer the dynamic condition of PF maltracking. Q-angle intrarater and interrater reliability has varied across studies, with intraclass correlation coefficients reported from 0.20 [12] to 0.70 [34]. Past studies have revealed a correlation [16] and no correlation [32] between Q-angle and PF pain syndrome. For these reasons, the clinical usefulness of the Q-angle remains controversial. It is further confounded by the fact that direct correlations between Q-angle and PF displacements and/or rotations have not been established. The one study, assessing the correlation between the Q-angle and two-dimensional (2D) static PF medial-lateral location, found no correlation [3].
The J-sign [9, 10, 19, 35] refers to the inverted J-path the patella takes in early flexion (or terminal extension) as the patella begins laterally subluxated and then suddenly shifts medially to engage with the femoral groove (or the reverse). It is likely a critical variable in evaluating suspected patellar maltracking because this dynamic marker can be “the most challenging to stabilize” [35]. Clinical evaluation of the J-sign is simple, but it is a subjective measure and its fundamental cause has not been established [10]. In published studies, the J-sign is assumed to be indicative of excessive lateral patellar shift in terminal extension [10, 35]. Yet, the term J-sign suggests a curved motion. Thus, varus rotation (rotation about the posterior-anterior axis, which causes the patellar superior pole to move laterally) likely influences its identification.
Numerous studies have compared PF alignment [1, 14, 22, 24, 26, 31] and PF displacements/rotations [5, 29, 39, 44, 48] in patients diagnosed with PF pain with asymptomatic controls. These studies typically reported variations in PF alignment, displacements, and/or rotations between the two populations, but the results are inconsistent across studies. In one study, no differences were reported [25], yet in another, differences in the majority of the 3D PF displacements and rotations were reported [39]. This variability is likely the result of differences in measurement techniques, variables measured, and the presence of various types of maltracking patterns in the omnibus term of patellar maltracking [37, 39]. For example, Schutzer et al. [37] identified three distinct malalignment patterns in patients with PF pain: excessive lateral tilt, lateral subluxation, and lateral subluxation with tilt. The ability to accurately define various types of PF maltracking patterns in the presence of PF pain should help optimize treatment by localizing the sources of pain.
Thus, our primary objective was to test the hypothesis that increased Q-angle, lateral hypermobility, and the presence of a J-sign are correlated with the patellar lateral position, relative to the femur, in terminal extension. As previous studies showed PF pain is associated with rotational and displacement variations in all three planes [39, 48], these correlations were expanded to include all 12 PF motion parameters (the value of PF medial, superior, and anterior displacement along with PF flexion, medial tilt, and varus rotation and the slopes of each of these variables relative to knee angle). The secondary objective was to explore whether more than one maltracking pattern could be discriminated, based on PF displacements and rotations. In addition, the ability of clinical markers to discriminate the same maltracking subgroups was tested.
Materials and Methods
Two cohorts were recruited. The first included 19 volunteers diagnosed with PF pain and suspected patellar maltracking, who were recruited from local orthopaedic clinics and ongoing National Institutes of Health studies. To be included in this first cohort, each knee had to be clinically diagnosed with PF pain syndrome with idiopathic anterior knee pain present for 1 year or longer. An in-house physiatrist using a physical examination and patient history excluded any knees having (1) prior surgery (including arthroscopy); (2) ligament, meniscus, iliotibial band, or cartilage damage; (3) other lower leg disorder or injury; or (4) traumatic onset of PF pain syndrome. In addition, a physical therapist (TJB) blinded to the PF displacement and rotational results examined each knee for evidence of maltracking: (1) Q-angle of 15º or greater; (2) a positive apprehension test; (3) patellar lateral hypermobility of 10 mm or greater; or (4) a positive J-sign. Any knee not exhibiting one or more of these four signs was excluded. Eight knees were excluded (one by the physiatrist and seven by the physical therapist). In total, 30 knees from the 19 volunteers diagnosed with PF pain were included in the final patient cohort. The second cohort was an asymptomatic population, consisting of 37 knees from 28 subjects, recruited from the greater Washington, DC, area population. This recruitment was web-based (http://clinicalresearch.nih.gov/), conducted through the National Institutes of Health Clinical Center Patient Recruitment and Public Liaison Office. Both knees were evaluated for the asymptomatic volunteer, if time permitted. All subjects in this cohort were asymptomatic with no history of lower leg abnormality, surgery, or major injury. For both cohorts, no subject was excluded owing to having an MRI contraindication. The inclusion and exclusion criteria were evaluated for all volunteers and patients at least three times: (1) after they had expressed interest, a phone interview was conducted; (2) before participation, an in-house history and physical examination were performed; and (3) all MR images were evaluated by a musculoskeletal radiologist. The demographics were similar in the two cohorts (Table 1). (All participants gave informed consent on entering this Institutional Review Board-approved study.)
Table 1.
Demographics and clinical scores for control subjects and maltracking subgroups*
| Item | Asymptomatic | Lateral | Nonlateral |
|---|---|---|---|
| Gender (female/male) | 22/15 | 14/3 | 12/1 |
| Age (years)† | 26.3 ± 8.9 | 29.3 ± 12.4 | 27.9 ± 10.0 |
| Height (cm)† | 169.4 ± 9.9 | 169.6 ± 6.9 | 168.9 ± 6.5 |
| Weight (kg)† | 66.5 ± 11.8 | 65.9 ± 15.3 | 66.6 ± 7.7 |
| Visual analog scale score (of 100)† | 40.1 ± 27.1 | 35.1 ± 26.5 | |
| Kujala score (of 100)† | 75.6 ± 10.4 | 72.1 ± 13.0 | |
| Q-angle (degrees)† | 15.4 ± 3.7 | 17.0 ± 2.0 | |
| Lateral hypermobility* (mm)† | 10.3 ± 4.8 | 5.8 ± 1.6 | |
| J-sign (present) | 9 | 5 | |
| Quantitative J-sign* (present) | 7 | 0 | |
| Length of pain (years)† | NA | 3.6 ± 2.9 | 2.7 ± 1.7 |
* The asymptomatic data were taken before the patellar maltracking data; thus, the clinical parameters were not collected for this cohort; for these measures, Student’s t test was used to compare means between groups; no differences (p ≥ 0.05) were found between the group demographics; lateral hypermobility and quantitative J-sign were different (p < 0.05) between the lateral and nonlateral maltracking groups; †values are expressed as mean ± standard deviation; NA = not applicable.
The pain in each knee was evaluated using a visual analog scale for pain and a Kujala score [23]. The Q-angle and lateral hypermobility were measured with the subject in a supine position with the knee and hip in the anatomically neutral position and with relaxed musculature. The Q-angle [10] was defined as the angle created by two vectors, both starting at the anterior center of the patella. One vector extended to the anterior-superior iliac spine (ASIS) and the other extended to the tibial tuberosity. Lateral hypermobility [10] was defined as the ability of the examiner to move the patella laterally by 10 mm or more (patellar glide test). This was evaluated by the examiner moving the patella medially with his thumbs, while stabilizing the leg (with their palms and fingers), until the end range of motion was reached. The distance traveled by the lateral edge of the patella was measured using a ruler with millimeter increments. To evaluate the J-sign [10], subjects were seated at the end of the table and the examiner evaluated patellar motion as the subject raised his/her leg into full extension. If the patella suddenly shifted laterally in terminal extension, creating an inverted J-path, the J-sign was considered present.
Complete 3D displacements and rotations for the PF joint were derived from fast-PC (dynamic) MR images. To acquire these images, subjects were placed supine in an MR imager (1.5 T; GE Medical Systems, Milwaukee, WI; or 3.0 T; Philips Electronics, Eindhoven, The Netherlands). A previous analysis determined the displacements and rotations obtained from the two imaging systems were not different. A cushioned wedge was placed under the thigh to slightly flex the hip. This provided the subjects with the ability to extend their leg from approximately 40º flexion to full extension. A full fast-PC MR image set (x, y, z velocity and anatomic images over 24 time frames) was acquired while the subjects cyclically extended and flexed their knee from maximum attainable flexion to full extension and back for approximately 2.5 minutes. The motion was guided by an auditory metronome [38]. Before data collection, subjects practiced the task until they could comfortably repeat the motion.
All displacements and rotations were defined relative to an anatomic coordinate system embedded in each bone [38]. The identification of these coordinate systems was completed for one time frame only and integration [51] of the 3D velocity data allowed displacements of the femur, tibia, and patella to be accurately tracked throughout the movement. For example, the femoral origin was defined as the deepest point in the femoral sulcus in the axial image at the level of the epicondyles, whereas the patellar origin was defined as the most posterior point on the patella in the midpatellar image (Fig. 1). Both points were identified in one time frame (full extension) and their location in all other time frames were determined analytically, based on the knowledge of how the entire bone displaced and rotated throughout the movement. Thus, the need to visually identify anatomic landmarks at multiple times, as has been necessary previously [5], was eliminated. This approach has high reported accuracy (< 0.5 mm [42]) and precision (< 1.16º [36]) in tracking 3D PF displacements and rotations.
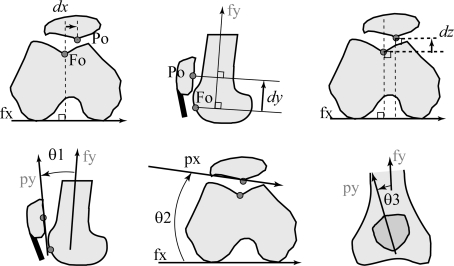
Fig. 1.
The diagrams illustrate 2D approximations of 3D translations and rotations. All rotations and translations are based on 3D kinematics using anatomic coordinate systems defined previously [38]. For example, the femoral x-axis (fx) is defined by the two most posterior points on the femoral condyles at the level of the epicondylar line and is directed medially. The femoral y-axis and z-axis (fy and fz) are calculated from the femoral x-axis and other landmarks. The patellar x-axis (px) is defined by the posterior lateral edge at the level of the midpatella and is directed medially. In the top row (only positive directions are shown), dx, dy, and dz refer to patellar medial, superior, and anterior displacement (with respect to the femur), respectively. Po and Fo indicate the origin of the patellar and femoral coordinates, respectively, and are pictured as dark-filled circles. In the bottom row (only positive directions are shown), θ1, θ2, and θ3 refer to patellar flexion, medial tilt, and varus rotation (with respect to the femur), respectively. Owing to the small angles, the 3D angles reported can be approximated by these 2D counterparts. Thus, the 3D lateral patellar tilt (θ2) is approximately equivalent to the clinical patellar tilt angle and patellar lateral shift (dx) is approximately equivalent to the bisect offset.
Once the displacement trajectories for a minimum of three noncolinear points were known, the bone’s complete 3D rotation matrix and translation trajectory were calculated [21, 43]. The rotation matrix was simplified to three Cardan rotation angles using an xyz body-fixed rotation sequence. This assumed the patella began aligned with the femur and arrived at its final alignment by first rotating about its lateral-medial (LM) axis, then about its inferior-superior (IS) axis, and finally about its posterior-anterior (PA) axis. These rotations were defined as extension-flexion (EF), PF LM tilt, and valgus-varus (VV) rotation. Because all these 3D angles tend to be small, they can be approximated by their 2D planar counterparts (Fig. 1) [40]. As varus rotation likely influences the identification of the clinical J-sign [10, 35], a new measure defined as the quantitative J-sign was created. A quantitative J-sign was present if the slope of the PF varus angle (Fig. 1) versus knee angle was outside the 95% confidence interval of the asymptomatic population (> 0.25º varus/º knee extension). The slope of the PF varus angle was calculated from the dynamic MR velocity data.
Owing to the dynamic nature of the MR acquisition, data were collected in even temporal, rather than even knee angle, increments during flexion and extension. Data were interpolated to single-degree knee angle increments and only the extension portion of the movement was used in the final analysis. Displacement and rotational comparisons were made based on two variables, value and slope. The magnitude of a displacement or rotational variable at 10º knee extension was defined as its value. The slope of each variable was defined by the linear best fit of each with knee angle. The validity of using a linear best fit has been documented [39].
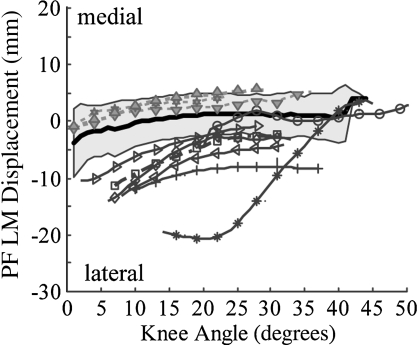
Maltracking subgroups were created by dividing the PF pain cohort into two groups based on PF LM displacement. The average PF LM displacement at 10º knee extension in the asymptomatic subjects was −0.45 mm. Thus, symptomatic knees medially displaced relative to the asymptomatic average (≥ −0.45 mm) with a LM displacement slope of 0.25 mm/º or less were defined as nonlateral maltrackers (n = 13). All others were defined as lateral maltrackers (n = 17). This definition was guided by a preliminary analysis of 10 subjects with PF pain. In this smaller cohort, two distinct patterns of PF LM displacement were easily identifiable (Fig. 2). Both groups were defined as maltrackers, as both had differences in 3D PF movement profile, from the asymptomatic average. The nonlateral maltrackers (of this smaller cohort) entered the study based solely on having PF pain and a Q-angle of 15º or greater, whereas the lateral maltrackers entered the study based on PF pain and at least one dynamic marker of maltracking (J-sign or lateral hypermobility). After this preliminary analysis, the PF cohort was expanded. A power analysis showed 10 subjects per group were required to detect a 3-mm difference in LM displacement assuming a two-sided Student’s t test with a power of 0.80 and a significance level of 0.05. The 3-mm difference was chosen based on previous work that found a 2.9-mm difference (statistically significant) in LM displacement between a cohort of patients with patellar maltracking and a cohort of asymptomatic volunteers [39].
Fig. 2.
A graph shows PF LM displacement versus knee angle. This preliminary analysis of 10 patients with PF pain demonstrated two distinct groups within the maltracking population. Three patients with PF pain were medial of the asymptomatic average (gray, filled symbols) and seven were lateral (black, unfilled symbols). The first group (nonlateral maltrackers) entered the study due to a Q-angle of 15º or greater (static marker) without lateral hypermobility or J-sign. The second group (lateral maltrackers) entered with at least one dynamic clinical inclusion criteria (either lateral hypermobility or J-sign). No other kinematic variable demonstrated two separate groups.
Correlations were sought in the patellar maltracking population between 12 PF motion parameters (the value and the slope of PF medial, superior, and anterior displacement along with tilt, flexion, and varus rotation) and the four markers of maltracking (Q-angle, lateral hypermobility, clinical J-sign, and quantitative J-sign). A one-way analysis of variance with the main effect factor being group (controls, nonlateral and lateral maltrackers) was used to compare PF displacement, PF rotations, and demographics across groups. If a difference (p < 0.05) was detected between groups, a Tukey post hoc analysis was performed to determine the group pair showing this difference. After the post hoc analysis, a Bonferroni-type false discovery rate procedure [20] was used to adjust the p values for multiple comparisons in each group pair.
A discriminant analysis (used to determine which variables differentiate between two or more naturally occurring groups) was used to validate the definition of subgroups based on LM displacement. As discriminant analyses typically provide clearer results if limited predicting variables are used, three sets of predicting variables were defined based on previous knowledge of PF pain and maltracking. The predicting variable sets were (1) the values and slopes of the variables primarily associated with patellar maltracking (LM displacement and tilt); (2) the values of LM displacement, IS displacement, EF and VV rotation along with the slopes of LM displacement, LM tilt, and VV rotation (these seven showed significant differences between a maltracking population and asymptomatic controls in a previous study [39]); and (3) Q-angle, lateral hypermobility, and J-sign. These three groups were defined as PK4 (four PF variables), PK7 (seven PF variables), and C3 (three clinical measures), respectively.
Results
The data did not support the hypothesis that increased Q-angle, lateral hypermobility, and the presence of a J-sign are correlated with the patellar lateral position, relative to the femur, in terminal extension (Table 2; Fig. 3). In fact, the opposite correlation was observed for the Q-angle, which was positively correlated with the value of medial displacement (p = 0.010) and negatively correlated with superior displacement (p = 0.026). This indicated a large Q-angle was associated with a more medially and inferiorly placed patella. Lateral hypermobility was correlated with the superior location of the patella (p = 0.036) and the slope of PF tilt (p = 0.035). The J-sign was correlated only with the slope of PF tilt (p = 0.017).
Table 2.
Correlations between clinical and patellofemoral displacement and rotational parameters for the patellofemoral pain population*
| Measure | Q-angle | Lateral hypermobility | Clinical J-sign | Quantitative J-sign | ||||
|---|---|---|---|---|---|---|---|---|
| r Value | p Value | r Value | p Value | s Value | p Value | r Value | p Value | |
| Q-angle | ||||||||
| Lateral hypermobility | ||||||||
| J-sign | ||||||||
| Quantitative J-sign | ||||||||
| Visual analog scale score | 0.56 | 0.003 | ||||||
| Kujala score | ||||||||
| LM value | 0.46 | 0.010 | 0.50 | 0.005 | ||||
| LM slope | −0.48 | 0.007 | ||||||
| IS value | −0.41 | 0.026 | 0.38 | 0.036 | −0.39 | 0.032 | ||
| PA slope | −0.53 | 0.002 | −0.43 | 0.017 | ||||
| Tilt value | 0.62 | < 0.001 | ||||||
| Tilt slope | 0.38 | 0.035 | 0.43 | 0.017 | −0.60 | < 0.001 | ||
| EF value | −0.37 | 0.046 | ||||||
* Pearson’s correlation coefficients (r) are listed and the Spearman’s correlation coefficient (s), along with their p values, are listed if there was a significant correlation between the row and column variables; any kinematic parameter that is not significantly (p ≥ 0.05) correlated with a clinical measure is not shown. The Kujala score and the visual analog scale score were strongly correlated to each other (r = −0.447); LM = lateral to medial; IS = inferior to superior; PA = posterior to anterior; tilt = lateral to medial tilt; EF = extension to flexion.
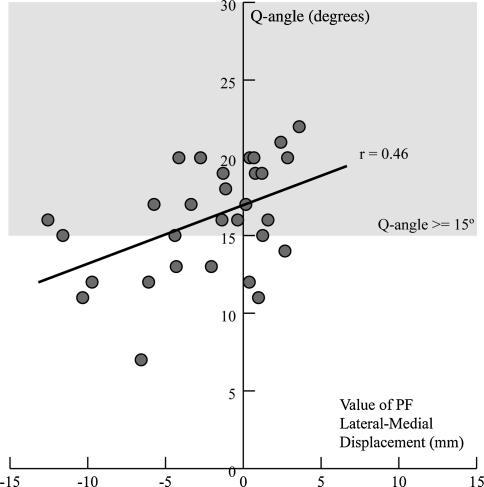
Fig. 3.
The graph shows the correlation of Q-angle with PF LM displacement for the PF pain group. The x-axis is the value of lateral (negative) to medial (positive) PF displacement at 10º knee flexion. The shaded grey area represents the Q-angle in the pathologic region (≥ 15º). The y-axis is the Q-angle. The best linear fit is shown with a solid black line. The linear correlation was significant (p < 0.05) and moderate [28], showing the Q-angle is correlated with medial, not lateral, PF displacement
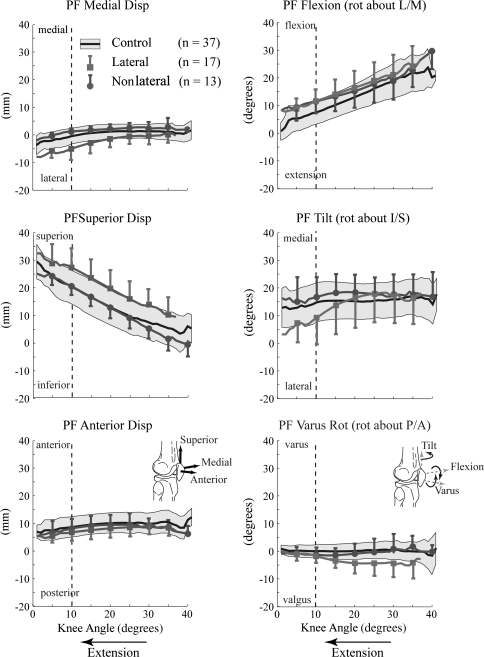
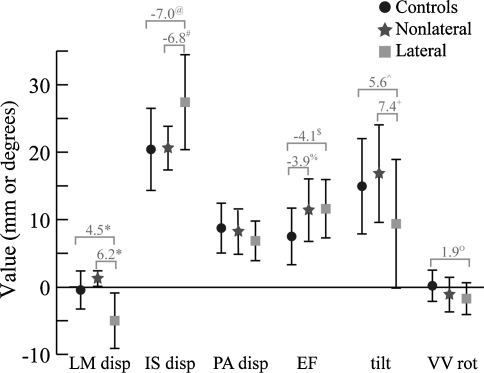
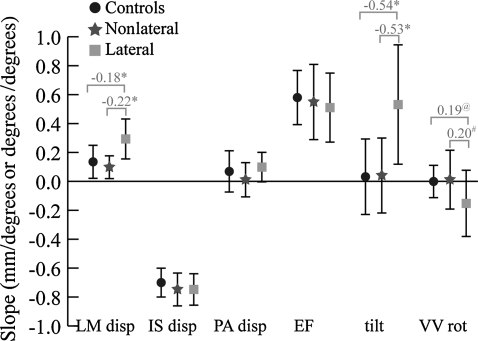
Two distinct groups of maltrackers (lateral and nonlateral) were distinguished based on PF LM displacement (Figs. 4, 5, 6). The discriminant analysis using PK4 and PK7 supported this definition of subgroups with 90.0% and 93.3% accuracy, respectively. Although the groups were divided based on LM displacement, the lateral group was 6.2 mm laterally displaced (p < 0.001), 7.4º laterally tilted (p = 0.032), and 6.8 mm superiorly displaced (p < 0.001), along with having increased slopes for lateral displacement (Δslope = 0.22, p < 0.001), lateral tilt (Δslope = 0.53, p < 0.001), and varus rotation (Δslope = −0.20, p = 0.013), compared with the nonlateral maltrackers (Figs. 5, 6). The lateral group differed from the asymptomatic group average for all PF value variables except PA displacement, whereas the nonlateral maltrackers differed from the asymptomatic group average for one variable only (increased PF flexion). As both groups had significant differences in 3D PF movement profiles from the asymptomatic average, the term “maltrackers” was maintained for both groups. Qualitatively, lateral tilt and displacement followed unique patterns in each maltracking group. For the lateral maltrackers, tilt and displacement had a small lateral change during early extension and an abrupt slope change at approximately 20º knee extension followed by a rapid lateral change in terminal extension. The nonlateral maltrackers had a small lateral change throughout extension. On average, the nonlateral group had less lateral hypermobility and fewer J-signs than the lateral group (Table 1).
Fig. 4.
The graphs show PF kinematics comparing symptomatic with lateral and nonlateral subgroups. The able-bodied (control) average (n = 37; black line, no symbol ± 1 standard deviation) is shown in gray shading. The lateral (nonlateral) maltracking group has squares (circles) placed at 5º-knee angle increments with a 1-standard deviation bar. The left column contains the three scaled translations and the right column contains the three rotations, which are based on a body-fixed xyz rotation sequence. The dotted line represents 10º knee extension, in which the statistical comparisons of value were made. To account for skeletal size variations across subjects, all translations were scaled by the ratio of the average epicondylar width from the asymptomatic population (77.3 mm) to the epicondylar width for each knee. The nonlateral group differed from the normative average for one variable only (increased PF flexion). The lateral group differed from the normative average for all PF value variables except PA displacement. Disp = displacement; rot = rotation.
Fig. 5.
A graph compares values of PF displacements and rotations between groups. If differences (p < 0.05) were found in the Tukey post hoc analysis of the analysis of variance, then a bar was placed to connect the groups with the difference and the average difference between the groups was placed above the bar. Patients who had medial displacement relative to the asymptomatic average (≥ −0.45 mm) with a LM displacement slope of 0.25 mm/º or less were defined as nonlateral maltrackers (stars). All others were defined as lateral maltrackers (squares). The superscript symbols after the average values indicate the following: *p < 0.001, @p = 0.001, #p = 0.008, $p = 0.0061, %p = 0.020, ^p = 0.049, +p = 0.032, Op = 0.023; disp = displacement; tilt = LM tilt; rot = rotation.
Fig. 6.
A graph compares slopes of PF displacements and rotations among groups. If differences (p < 0.05) were found in the Tukey post hoc analysis of the analysis of variance, then a bar was placed to connect the groups with the difference and the average difference between the groups was placed above the bar. Patients who had medial displacement relative to the asymptomatic average (≥ −0.45 mm) with a LM displacement slope of 0.25 mm/º or less were defined as nonlateral maltrackers (stars). All others were defined as lateral maltrackers (squares). The superscript symbols after the average values indicate the following: *p < 0.001, @p = 0.002, #p = 0.013; disp = displacement; tilt = LM tilt; rot = rotation.
Unlike the preliminary analysis, the subgroups for the larger cohort of patients with PF pain could not be defined accurately when using the three standard clinical measures (J-sign, Q-angle, lateral hypermobility) as predicting variables. Yet, a discriminant analysis using the continuous variables of Q-angle, lateral hypermobility, and quantitative J-sign could predict the groups to an accuracy of 90.6%. Thus, in general, the lateral maltrackers entered the study based on the presence of PF pain and at least one dynamic marker of maltracking (either patellar lateral hypermobility ≥ 10 mm, a positive quantitative J-sign, or both). This group had Q-angles greater and lesser than 15º. In general, the nonlateral maltrackers entered the study based solely on two factors: PF pain and a Q-angle of 15º or greater (static marker).
The clinical J-sign and the quantitative J-sign were not correlated with each other, but the quantitative J-sign was correlated with seven PF displacement and rotation variables (Table 2). Lateral hypermobility was correlated with the value of IS and the slope of PA displacement. Lateral hypermobility and LM displacement had the greatest influence in the discriminant analyses after all other factors were controlled for.
Discussion
Clinical measures such as the Q-angle, lateral hypermobility, and the clinical J-sign have been used to infer excessive lateral PF displacement. Unfortunately, these measures have not been correlated to specific 3D PF displacement and rotations in past studies. Thus, the association between these clinical measures and 12 parameters of PF motion was investigated. In addition, past studies have suggested the presence of subgroups with unique PF maltracking patterns in patients diagnosed with PF pain syndrome. Identifying these subgroups may play a critical role in providing more effective interventions.
The knee motion evaluated in this study was limited to partial range of motion with no externally applied load. This did not limit the study conclusions, as the patella is less engaged with the femoral sulcus and maltracking patterns typically are most evident [18] in this range of motion [39]. The required self-selected quadriceps activation during this free-kicking exercise likely further accentuated the maltracking patterns [5, 50]. Although insufficient power may have influenced the conclusions reached for certain variables, the between-group differences were small. Thus, the differences between these variables were likely clinically irrelevant. The clinical inclusion criteria were evaluated by one of the authors (KEA) for two knees with PF pain. A training session, held before data collection, ensured intraobserver and interobserver consistency. Removing these two knees from the analysis did not alter the final conclusions.
The finding that Q-angle is associated with medial and inferior PF displacement opposes the theory that a large Q-angle results in lateral subluxation [4, 10, 35]. Yet, in light of the work on the Q-angle’s basic geometry [13, 17], the results are logical. According to Grelsamer et al. [15], a 2-cm lateral shift in the ASIS results in a 2º increase in Q-angle. Accordingly, a more medially placed patella and a shorter patellar tendon result in a larger Q-angle; specifically, the same 2-cm shift applied medially to the patellar center results in an 18.2º increase in Q-angle (assuming the distance between the patellar center and the tibial tuberosity = 7 cm [41]). Therefore, a large Q-angle is more indicative of a medialized patella than a lateralized ASIS. Applying this reasoning to the maltracking population, it can be theorized a large Q-angle is indicative of a medially placed patella under static conditions. This medial placement is a result of passive constraints alone because muscle activity is not present when the Q-angle is measured. For the nonlateral maltrackers (all but two of whom had a Q-angle ≥ 15º), these passive constraints are capable of counteracting the lateral pull of the extensors during active contraction and maintaining a medialized patella.
The clinical J-sign primarily has been associated with PF lateral subluxation [19, 35] and vastus medialis oblique (VMO) deficiency [35]. The latter is unlikely because the VMO moment has a small varus component and a VMO/vastus lateralis imbalance would result in valgus rotation. Thus, the presence of a J-sign likely indicates a ligamentous problem or a small lateral trochlear inclination angle [2], explaining the difficulty in stabilizing a knee showing a positive J-sign. Unfortunately, the measure of quantitative J-sign is not a simple clinical measure nor does it correlate with the subjective clinical J-sign. Yet, based on the discriminant analysis, if a clinical measure could be established that precisely captures the change in PF varus rotation, there would be a set of clinical assessment tools (Q-angle, lateral hypermobility, quantitative J-sign) that together could distinguish the maltracking patterns observed in our study subjects.
Establishing the presence of subgroups in the umbrella diagnosis of PF pain with maltracking likely will enhance treatment by allowing for more targeted interventions. For example, when a patient does not exhibit the classic PF maltracking patterns (excessive lateral tilt and displacement), pain often is assumed to be from overuse [45]. Yet, PF pain may arise owing to alterations in the other PF displacements and rotations. For example, the nonlateral group had excessive PF flexion, which may decrease cartilage contact area, causing increased contact stress. In addition, the patella engages with the femoral sulcus further in terminal extension for this group, as compared with the lateral maltrackers (7-mm difference in PF superior displacement). Thus, the sulcus is more likely to provide the passive force, which maintains nearly normative axial plane movement. Excessive forces on the sulcus and patellar lateral edge are likely sources of pain. However, the lateral maltrackers had the classic PF maltracking patterns. In this group, the presence of patella alta reduces the overall PF contact area, causing increased stress and potentially PF pain [47]. Patella alta creates a situation in which the patella leaves the sulcus groove earlier in the extension cycle, causing a loss of bony constraints and resulting in greater tilt and subluxation. Thus, a secondary pain source may arise from the high forces required to reengage the patella into the sulcus during flexion.
The fact that three different discriminant analyses had greater than 90% agreement with the definition of the maltracking subgroups provides strong evidence for the existence of these subgroups. In future studies, it may be possible to further divide the nonlateral maltrackers into three subgroups (medial, normal, lateral tilt) and the lateral maltrackers into two subgroups (normal, lateral tilt). The presence of five subgroups was not investigated owing to sample size restrictions. Being able to further subdivide the group likely will lend support to the three subgroups (lateral placement, lateral tilt, lateral placement with lateral tilt) established by Schutzer et al. [37].
Q-angle, lateral hypermobility, and the clinical J-sign may not be accurate gauges of lateral subluxation during dynamic activity. Distinct maltracking subgroups do exist in the patellar maltracking population. The quantitative J-sign is highly correlated with 3D PF displacements and rotations. Lateral hypermobility is a critical clinical variable in that it is different between maltracking subgroups, is correlated with PF motion, and has the greatest influence on the discriminant analysis. Work is ongoing to establish a larger database to explore finer details in these subgroups.
Acknowledgments
We thank Ching-yi Shieh, PhD, and Elizabeth K. Rasch, PT, PhD, for support on the statistical analysis and Steven Stanhope, PhD, for guidance throughout the project. We also thank Bonnie Damaska, Jamie Fraunhaffer, Jere McLucas, Dr. Barry Boden, and the Diagnostic Radiology Department at the National Institutes of Health for their support and research time.
Footnotes
This research was supported in part by the Intramural Research Program of the National Institutes of Health (Clinic Center and National Institute of Child Health and Human Development).
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent and assent, if the subject was a minor, was obtained.
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author and do not necessarily reflect the views of the National Institutes of Health or the US Public Health Service.
References
- 1.Aglietti P, Insall JN, Cerulli G. Patellar pain and incongruence. I: Measurements of incongruence. Clin Orthop Relat Res. 1983;176:217–224. [PubMed] [Google Scholar]
- 2.Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Joint Surg Br. 2008;90:864–869. doi: 10.1302/0301-620X.90B7.20447. [DOI] [PubMed] [Google Scholar]
- 3.Biedert RM, Warnke K. Correlation between the Q angle and the patella position: a clinical and axial computed tomography evaluation. Arch Orthop Trauma Surg. 2001;121:346–349. doi: 10.1007/s004020000239. [DOI] [PubMed] [Google Scholar]
- 4.Bourne MH, Hazel WA, Jr, Scott SG, Sim FH. Anterior knee pain. Mayo Clin Proc. 1988;63:482–491. doi: 10.1016/s0025-6196(12)65646-8. [DOI] [PubMed] [Google Scholar]
- 5.Brossmann J, Muhle C, Schroder C, Melchert UH, Bull CC, Spielmann RP, Heller M. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 6.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582–585. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- 7.Cutbill JW, Ladly KO, Bray RC, Thorne P, Verhoef M. Anterior knee pain: a review. Clin J Sport Med. 1997;7:40–45. doi: 10.1097/00042752-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 9.Emami MJ, Ghahramani MH, Abdinejad F, Namazi H. Q-angle: an invaluable parameter for evaluation of anterior knee pain. Arch Iran Med. 2007;10:24–26. [PubMed] [Google Scholar]
- 10.Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85:234–243. doi: 10.1097/01.phm.0000200390.67408.f0. [DOI] [PubMed] [Google Scholar]
- 11.Fulkerson JP, Arendt EA. Anterior knee pain in females. Clin Orthop Relat Res. 2000;372:69–73. doi: 10.1097/00003086-200003000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Greene CC, Edwards TB, Wade MR, Carson EW. Reliability of the quadriceps angle measurement. Am J Knee Surg. 2001;14:97–103. [PubMed] [Google Scholar]
- 13.Grelsamer RP, Dubey A, Weinstein CH. Men and women have similar Q angles: a clinical and trigonometric evaluation. J Bone Joint Surg Br. 2005;87:1498–1501. doi: 10.1302/0301-620X.87B11.16485. [DOI] [PubMed] [Google Scholar]
- 14.Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;282:170–176. [PubMed] [Google Scholar]
- 15.Grelsamer RP, Weinstein CH, Gould J, Dubey A. Patellar tilt: the physical examination correlates with MR imaging. Knee. 2008;15:3–8. doi: 10.1016/j.knee.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Haim A, Yaniv M, Dekel S, Amir H. Patellofemoral pain syndrome: validity of clinical and radiological features. Clin Orthop Relat Res. 2006;451:223–228. doi: 10.1097/01.blo.0000229284.45485.6c. [DOI] [PubMed] [Google Scholar]
- 17.Herrington L, Nester C. Q-angle undervalued? The relationship between Q-angle and medio-lateral position of the patella. Clin Biomech (Bristol, Avon). 2004;19:1070–1073. doi: 10.1016/j.clinbiomech.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Inoue M, Shino K, Hirose H, Horibe S, Ono K. Subluxation of the patella: computed tomography analysis of patellofemoral congruence. J Bone Joint Surg Am. 1988;70:1331–1337. [PubMed] [Google Scholar]
- 19.Johnson LL, Dyk GE, Green JR, III, Pittsley AW, Bays B, Gully SM, Phillips JM. Clinical assessment of asymptomatic knees: comparison of men and women. Arthroscopy. 1998;14:347–359. doi: 10.1016/s0749-8063(98)70001-5. [DOI] [PubMed] [Google Scholar]
- 20.Jones HE, Ohlssen DI, Spiegelhalter DJ. Use of the false discovery rate when comparing multiple health care providers. J Clin Epidemiol. 2008;61:232–240. doi: 10.1016/j.jclinepi.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 21.Kane TR, Likins PW, Levinson DA. Spacecraft Dynamics. New York, NY: McGraw-Hill Book Co; 1983. [Google Scholar]
- 22.Kobayashi T, Fujikawa K, Nemoto K, Yamazaki M, Obara M, Sato S. Evaluation of patello-femoral alignment using MRI. Knee. 2005;12:447–453. doi: 10.1016/j.knee.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 24.Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res. 1979;144:16–26. [PubMed] [Google Scholar]
- 25.MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 26.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 27.Mizuno Y, Kumagai M, Mattessich SM, Elias JJ, Ramrattan N, Cosgarea AJ, Chao EY. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res. 2001;19:834–840. doi: 10.1016/S0736-0266(01)00008-0. [DOI] [PubMed] [Google Scholar]
- 28.Morton R, Hebel J, McCarter R, editors. Correlations. A Study Guide to Epidemiology and Biostatistics. 4. Aspen Publishers, Inc: Gaithersburg, MD; 2008. p. 92. [Google Scholar]
- 29.Muhle C, Brossmann J, Heller M. Kinematic CT and MR imaging of the patellofemoral joint. Eur Radiol. 1999;9:508–518. doi: 10.1007/s003300050702. [DOI] [PubMed] [Google Scholar]
- 30.Mulford JS, Wakeley CJ, Eldridge JD. Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br. 2007;89:709–716. doi: 10.1302/0301-620X.89B6.19064. [DOI] [PubMed] [Google Scholar]
- 31.Murray TF, Dupont JY, Fulkerson JP. Axial and lateral radiographs in evaluating patellofemoral malalignment. Am J Sports Med. 1999;27:580–584. doi: 10.1177/03635465990270050601. [DOI] [PubMed] [Google Scholar]
- 32.Naslund J, Naslund UB, Odenbring S, Lundeberg T. Comparison of symptoms and clinical findings in subgroups of individuals with patellofemoral pain. Physiother Theory Pract. 2006;22:105–118. doi: 10.1080/09593980600724246. [DOI] [PubMed] [Google Scholar]
- 33.Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858–864. doi: 10.1148/radiology.216.3.r00se38858. [DOI] [PubMed] [Google Scholar]
- 34.Piva SR, Fitzgerald K, Irrgang JJ, Jones S, Hando BR, Browder DA, Childs JD. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7:33–46. doi: 10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy. 1999;15:841–851. doi: 10.1053/ar.1999.v15.015084. [DOI] [PubMed] [Google Scholar]
- 36.Rebmann AJ, Sheehan FT. Precise 3D skeletal kinematics using fast phase contrast magnetic resonance imaging. J Magn Reson Imaging. 2003;17:206–213. doi: 10.1002/jmri.10253. [DOI] [PubMed] [Google Scholar]
- 37.Schutzer SF, Ramsby GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986;17:235–248. [PubMed] [Google Scholar]
- 38.Seisler AR, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng. 2007;54:1333–1341. doi: 10.1109/TBME.2007.890735. [DOI] [PubMed] [Google Scholar]
- 39.Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res. 2009;27:561–570. doi: 10.1002/jor.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheehan FT, Drace JE. Quantitative MR measures of three-dimensional patellar kinematics as a research and diagnostic tool. Med Sci Sports Exerc. 1999;31:1399–1405. doi: 10.1097/00005768-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Sheehan FT, Drace JE. Human patellar tendon strain (a non-invasive, in vivo study) Clin Orthop Relat Res. 2000;370:201–207. doi: 10.1097/00003086-200001000-00019. [DOI] [PubMed] [Google Scholar]
- 42.Sheehan FT, Zajac FE, Drace JE. Using cine phase contrast magnetic resonance imaging to non-invasively study in vivo knee dynamics. J Biomech. 1998;31:21–26. doi: 10.1016/S0021-9290(97)00109-7. [DOI] [PubMed] [Google Scholar]
- 43.Sheehan FT, Zajac FE, Drace JE. In vivo tracking of the human patella using cine phase contrast magnetic resonance imaging. J Biomed Eng. 1999;121:1–7. doi: 10.1115/1.2800868. [DOI] [PubMed] [Google Scholar]
- 44.Shih YF, Bull AM, Amis AA. The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc. 2004;12:300–306. doi: 10.1007/s00167-003-0414-3. [DOI] [PubMed] [Google Scholar]
- 45.Thomee R, Renstrom P, Karlsson J, Grimby G. Patellofemoral pain syndrome in young women. I. A clinical analysis of alignment, pain parameters, common symptoms and functional activity level. Scand J Med Sci Sports. 1995;5:237–244. [PubMed] [Google Scholar]
- 46.Tomsich DA, Nitz AJ, Threlkeld AJ, Shapiro R. Patellofemoral alignment: reliability. J Orthop Sports Phys Ther. 1996;23:200–208. doi: 10.2519/jospt.1996.23.3.200. [DOI] [PubMed] [Google Scholar]
- 47.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89:1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 48.Wilson NA, Press JM, Koh JL, Hendrix RW, Zhang LQ. In vivo and noninvasive evaluation of abnormal patellar tracking during squatting in patellofemoral pain. J Bone Joint Surg Am. 2009;91:558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilson T. The measurement of patellar alignment in patellofemoral pain syndrome: are we confusing assumptions with evidence? J Orthop Sports Phys Ther. 2007;37:330–341. doi: 10.2519/jospt.2007.2281. [DOI] [PubMed] [Google Scholar]
- 50.Witonski D, Goraj B. Patellar motion analyzed by kinematic and dynamic axial magnetic resonance imaging in patients with anterior knee pain syndrome. Arch Orthop Trauma Surg. 1999;119:46–49. doi: 10.1007/s004020050353. [DOI] [PubMed] [Google Scholar]
- 51.Zhu Y, Drangova M, Pelc NJ. Fourier tracking of myocardial motion using cine-PC data. Magn Reson Med. 1996;35:471–480. doi: 10.1002/mrm.1910350405. [DOI] [PubMed] [Google Scholar]