Abstract
Stability is a key issue in treating supination-external rotation ankle fractures, but we do not know how it affects functional outcome and subsequent development of radiographic osteoarthritis. With a systematic literature review, we identified 11 clinical studies (Level IV evidence) published in peer-reviewed journals reporting on at least 10 ankles. Followup was at least 1 year. Two authors independently scored the quality of the studies using the modified Coleman Methodology Score; the mean score was 58 of 100, with substantial agreement between the two examiners. Four studies used a general health assessment questionnaire. Several literature limitations (debatable fracture stability criteria, few cohort studies with heterogeneous methodology, small patient numbers and limited followup in some studies) do not allow definitive conclusions. Of 213 stable fractures treated nonoperatively, 2.8% of ankles had radiographic osteoarthritis develop (18 years’ mean followup) and 84% were free of symptoms. The incidence of radiographic osteoarthritis in 420 unstable fractures treated operatively was 20.9% at 5.5 years versus 65.5% at 6.8 years in 137 ankles treated nonoperatively. The complication rate in 355 operatively treated fractures was 10.4%. A medial malleolus fracture, female gender, older age, higher American Society of Anesthesiologists grade, smoking, and lower educational level negatively influenced general health outcome, physical function, and pain.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Malleolar fractures range from an isolated distal fibular fracture with minimal displacement to a trimalleolar fracture with dislocation and vascular compromise [1, 24]. Three classification systems are most commonly used. The Lauge-Hansen system [22] classifies fracture patterns based on the mechanism of injury. The Danis-Weber classification [10, 43] is based on the level of the distal fibula fracture and the importance of damage to the lateral structures for ankle mortise stability [45]. The Orthopaedic Trauma Association/American Orthopaedic Association classification [1, 24] combines elements of the Lauge-Hansen [22] and Danis-Weber [10, 43] classification systems, taking into account the level of the fibula fracture in relation to the syndesmosis, and the fact that insufficiency of the medial structures can lead to degeneration of the joint if biomechanical (dynamic) stability is not restored [27, 36, 42]. Stable injuries are those that cannot be displaced by physiologic forces, whereas unstable fractures easily displace when physiologic forces are applied [41]. Based on this concept, manual [33, 47] and gravity stress radiographic tests [15, 29] have been introduced to identify unstable fractures. A medial clear joint space (space between the medial malleolus and the talus) greater than 4 mm is considered abnormal by many authors [7, 11, 12, 15, 19, 25, 33, 41].
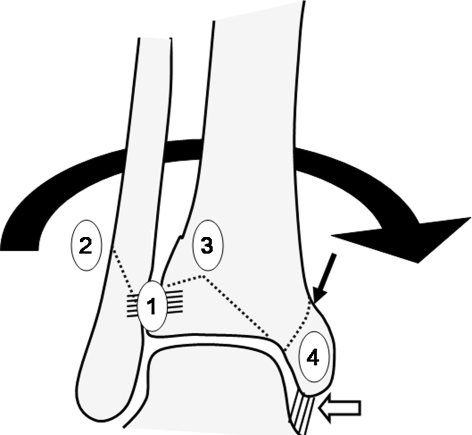
The most common injury pattern occurs with axial loading of a supinated foot. Because of its complex axis of movement [23], the subtalar joint acts as an angled hinge, so calcaneus inversion causes the talus to rotate externally (supination-external rotation [SER] mechanism). If excessive, the external rotation causes damage to the anterior tibiofibular ligament, and a sequence of injuries can follow (Fig. 1). Completion of the sequence of traumatic events on the medial side characterizes an unstable fracture pattern (Fig. 2) [1, 24, 26]. Based on the stability concept, nonoperative treatment seems appropriate for stable injuries, whereas maintenance of reduction of unstable fractures without operative fixation is difficult to achieve [1, 41].
Fig. 1.
Initially, the anterior tibiofibular ligament fails (1) (Stage I) and then an oblique fracture of the fibula starting at the level of the ankle and passing posteriorly occurs (2) (Stage II; Lauge-Hansen [22]). This may remain nondisplaced or minimally displaced if the deforming force stops at this point and the mortise remains stable. This is the most common type of fracture, classified as supination-external rotation II (SER-II). Progression of the deforming force (talar rotation) causes posterior and proximal displacement of the fibular fracture. Further talar rotation results in a fracture of the posterior articular lip of the tibia (3) (Stage III), and as the talus leaves the mortise posteriorly, a medial injury occurs (4) (Stage IV) at the deltoid ligament (white arrow) or at the medial malleolus (black arrow).
Fig. 2A–B.
(A) Anteroposterior and (B) lateral radiographs show an isolated distal fibula fracture with markedly increased medial joint space (between the talus and medial malleolus) indicative of failure of the deep deltoid ligament and fracture instability.
We raised several questions: (1) Does internal fixation of stable SER ankle fractures lead to reduced incidence of radiographic osteoarthritis compared with nonoperative treatment? (2) Does nonoperative treatment of unstable SER ankle fractures lead to occurrence of radiographic osteoarthritis and symptoms? (3) How common is radiographic osteoarthritis and the presence of symptoms after operative treatment of unstable SER ankle fractures? (4) Do other factors (eg, comorbidities, social factors) influence general health outcome, physical function, and pain? (5) How common are injuries to the syndesmosis requiring surgery in SER ankle fractures? (6) What is the complication rate after operative treatment?
Search Strategy and Criteria
We conducted a comprehensive literature search using MEDLINE®, EMBASE™, Cochrane, CINAHL®, and Google™ Scholar, with no restriction to time or language, on October 5, 2008. Database searches were performed using the following combinations of key words: (1) ankle and fractures and supination external rotation, (2) ankle and fractures and fixation, and (3) ankle and fractures and outcome. Abstracts were scanned by two of the authors (NG, AK) and articles relevant to the subject were retrieved and their bibliographies searched by hand to identify additional references. Articles reporting fractures in specific patient population groups (eg, elderly, diabetics) were excluded [17, 44], as comorbidities could have influenced the decision on fracture treatment method and its outcome. Included were original studies published in peer-reviewed journals, reporting on at least 10 closed SER ankle fractures in skeletally mature patients followed for more than 1 year. From a total of 697 references initially retrieved, 236 were identified as being relevant to the subject. Abstracts were scanned, and applying the exclusion criteria, 65 studies were processed for further evaluation. Full papers were examined, and 11 studies met the inclusion criteria. Pooling of data was possible to calculate followup periods and data regarding absence of symptoms and radiographic findings of posttraumatic osteoarthritis.
Two authors (NG, AK) independently scored the quality of the studies using the Coleman Methodology Score (CMS) [8, 39]. The CMS allows analysis of the quality of the studies reviewed, is accurate and reproducible in systematic reviews, and has been used for several years. The CMS was adapted (Table 1) to evaluate studies reporting on ankle fractures. A score approaching 100 indicates the study has a robust design and largely avoids chance, various biases, or confounding factors. The subsections that compose the CMS are based on the subsections of the CONSORT statement (for randomized, controlled trials) [30] but are modified to allow for other trial designs. Each investigator scored the quality of the studies twice with an interval of 3 weeks between scoring sessions. Intraobserver and interobserver reliability were examined. Where differences were encountered, agreement was achieved by consensus. The presented scores are those set by agreement of both examiners. We collected data for year of publication, type of study, patient numbers, gender, mechanism of injury, followup, type of fracture, interventions, complications, and outcome.
Table 1.
Criteria used to compute the Coleman Methodology Score for studies reporting outcomes of SER ankle fractures
| Criterion | Category | Score |
|---|---|---|
| Part A: only one score to be given for each of the seven sections | ||
| 1. Study size | < 25 | 0 |
| 25–49 | 4 | |
| 50–74 | 7 | |
| ≥ 75 | 10 | |
| 2. Mean followup | < 2 years | 0 |
| 2–4 years | 4 | |
| 5–10 years | 7 | |
| > 10 years | 10 | |
| 3. Number of different fracture management methods used | ||
| Not stated, unclear, or < 90% of subjects receiving the same management modality | 0 | |
| More than one implant version, but ≥ 90% of subjects receiving one technique | 7 | |
| One technique used | 10 | |
| 4. Type of study | ||
| Retrospective cohort study | 0 | |
| Prospective cohort study | 10 | |
| Randomized, controlled trial | 15 | |
| 5. Description of indications/diagnosis (eg, fracture type) | ||
| No | 0 | |
| Yes | 5 | |
| 6. Descriptions of management method(s) | ||
| Inadequate (not stated, unclear) | 0 | |
| Adequate (details of protocol/procedure given) | 5 | |
| 7. Rehabilitation protocol described | ||
| Yes | 10 | |
| No | 0 | |
| Part B: scores may be given for each option in each of the three sections if applicable | ||
| 1. Outcome criteria | ||
| Outcome measures clearly defined | 2 | |
| Timing of outcome assessment clearly stated | 2 | |
| Use of outcome criteria that has reported reliability | 3 | |
| General health measure included | 3 | |
| 2. Procedure of assessing outcomes | ||
| Subjects recruited | 5 | |
| Investigator independent of surgeon | 4 | |
| Written assessment | 3 | |
| Completion of assessment by patients themselves with minimal investigator assistance | 3 | |
| 3. Description of subject selection process | ||
| Selection criteria reported and unbiased | 5 | |
| Recruitment rate reported ≥ 80% | 5 | |
| Recruitment rate reported < 80% | 0 | |
SER = supination-external rotation; (The original description of the Coleman Methodology Score was published by Wiley Interscience in: Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2–11.)
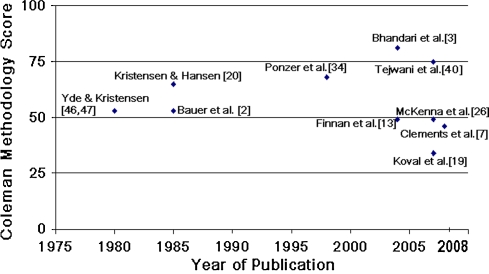
From 11 clinical studies fulfilling our criteria, four were retrospective and seven were prospective investigations (all Level IV evidence) [5]. The mean CMS was 57.8 of a possible total of 100 (standard deviation [SD], 14; range, 34–81) (Fig. 3). The intraobserver Spearman-Brown coefficient was 0.92 for Examiner A and 0.89 for Examiner B (substantial agreement) [21]. The values of the second assessment for each examiner were included for further evaluation. The mean CMS was similar (p = 0.73) between the two examiners (57.8 versus 57.4). The intraclass correlation was 0.95, indicative of substantial agreement [21]. Five studies were performed in institutions in the United States, three in Denmark, two in Sweden, and one in Ireland. No randomized, controlled trials were found. There were no studies investigating different forms of nonoperative treatment (eg, cast versus functional brace).
Fig. 3.
The distribution of quality of the studies according to the CMS throughout the last three decades.
Results
Three prospective long-term outcome studies from Scandinavia [2, 20, 46] reported on 213 SER-II (stable) ankle fractures treated from 1950 to 1976. Although anatomic reduction was not always achieved after nonoperative treatment after a mean followup of 17.9 years, similar percentages (p = 0.53) of patients/ankles treated nonoperatively and operatively were symptom free: 148 of 178 (83.1%) and 30 of 34 (88.2%), respectively (Table 2). Posttraumatic osteoarthritis seen on followup radiographic examination occurred in a similar (p = 0.21) percentage of patients undergoing nonoperative and operative treatment (five of 178, or 2.8%, versus one of 34, or 2.9%, respectively).
Table 2.
Management and results of SER ankle fractures
| Study | Classification and fracture type* | Interventions | Followup (years)† | Outcome assessment‡ | Results | Conclusion(s) |
|---|---|---|---|---|---|---|
| Yde and Kristensen [46] | L-H SER-II | 34 ORIF vs 35 nonoperative | 6 (3–10) | Radiographic: | No need for surgery for stable isolated fibula SER fractures | |
| Anatomic reduction (Cedell) | 28/34 ORIF vs 1/35 nonoperative (p = 0.73) | |||||
| Arthritis | 1/34 ORIF vs 4/35 nonoperative (p = 0.36) | |||||
| Clinical (Cedell) | Good result in 30/34 ORIF vs 34/35 nonoperative | |||||
| Yde and Kristensen [47] | L-H SER-IV | 60 ORIF vs 29 nonoperative | 5.6 (3–10) 6.8 (3–10) |
Radiographic | Operative management showed better results or SER-IV ankle fractures | |
| Anatomic reduction (Cedell) | 42/60 (70%) ORIF vs 0/29 nonoperative | |||||
| Arthritis | 12/60 (20%) ORIF vs 19/29 (66%) nonoperative (p < 0.001) | |||||
| Clinical (Cedell) | Good result in 50/60 (83%) ORIF vs 16/29 (55%) nonoperative | |||||
| Kristensen and Hansen [20] | L-H SER-II | 94 nonoperative | 21 (16–25) | Radiographic | Good results with nonoperative management of SER-II fractures | |
| Reduction (Cedell) | Nonanatomic 89/94 | |||||
| Arthritis | None | |||||
| Clinical | Symptom-free: 73/94 Negligible symptoms: 16/94 Moderate symptoms: 5/94 Reduced capacity to work or exercise: none | |||||
| Bauer et al. [2] | L-H SER-II and SER-IV | 49 nonoperative 38 nonoperative | 29 (25–34) | Subjective outcome (Cedell) | 47/49 (96%) good, 2/49 (4%) medium, 1/49 (2%) not good | Not all ankle fractures need anatomic reduction |
| Symptoms | 29/38 (76%) symptom-free | |||||
| Arthritis | 14/38 (37%) | |||||
| Ponzer et al. [34] | OTA/AO 44-B | 53 ORIF (variable techniques) | > 2 | 41 patients > 2 years’ followup, 36 available | SF-36 is a useful outcome measure; self-perceived limitations in everyday life is common after B-type ankle fractures | |
| SF-36, VAS (mental and physical) | ||||||
| OMA score | 84 (SD = 22.5), 64% of patients > 90 8/9 B1 (stable) fractures scored > 90 B3 (bimalleolar) worse than B2 | |||||
| Residual tenderness | 15/36 (42%) | |||||
| Reduced ROM | 24/36 (67%) | |||||
| Incomplete recovery | 23/36 (64%) | |||||
| Limitations in sports | 22/36 (61%) | |||||
| Limitations at work | 16/36 (44%) | |||||
| Correlations: | ||||||
| OMA vs SF-36 | Significant for subscores for physical functioning, physical and emotional role functioning, social functioning, pain | |||||
| OMA vs VAS (physical) | Significant | |||||
| OMA vs VAS (mental) | Nonsignificant | |||||
| SF-36 vs VAS (physical) | Significant, all SF-36 subscores | |||||
| SF-36 vs VAS (mental) | Significant except for the SF-36 subscores for pain and physical role functioning | |||||
| Bhandari et al. [3] | OTA/AO 44-B | 30 (25 bimalleolar) ORIF | 2 | SF-36 VAS pain scale | Role–physical and physical function domains of SF-36 lower than US norms (p < 0.01) Smoking and alcohol negatively affected general health outcomes Smoking was predictor of physical function summary score VAS pain scale correlated with bodily pain SF-36 subscores | Social factors may be important determinants of outcome in patients with fractures |
| Finnan et al. [13] | L-H SER-IV | 156 ORIF 26 responded | 5.2 (0.6–8.9) | SMFA questionnaire | No significant effect on 5 of 6 SMFA domains Negative impact on the mobility index scores | Suboptimal surgical reduction was associated with a negative effect on quality of life and ambulation |
| Arthritis | 6/26 (23%) | |||||
| Correlation of operative reduction with results | Anatomic reduction in 19/26: no arthritis, good functional result Suboptimal reduction: fair/poor results | |||||
| McKenna et al. [26] | OTA/AO 44-B | 25 ORIF with plate vs 25 ORIF with lag screws | 1.1 | Infections | Plate: 4/16, lag screws: 0/18 | Lag screw fixation was safe, allowing stable fracture fixation, without failures |
| AOFAS | Plate: 76, lag screws: 86 (p = 0.02) | |||||
| Questionnaire (16 from the plate group and 18 from the lag screws group responded) | ||||||
| Palpable hardware | 8/16 (50%) plate group vs 0/18 lag screws group | |||||
| Lateral ankle pain lasting > 3 months | More common (p = 0.004) in plate group | |||||
| Koval et al. [19] | OTA/AO 44-B | 19 nonoperative (intact deep deltoid on MRI) | 1.8 | AOFAS (15/19 available) | 14/15 had score 100, 1/15 had 85 | Nonoperative management might be an option for SER-IV ankle fractures with medial space widening if the deep deltoid ligament is intact |
| VAS pain (0–10) | 0.87 (range, 0-3) | |||||
| SF-36 | Comparable to general population | |||||
| Patients satisfied with outcome | 14/15 | |||||
| Patients satisfied with decision of conservative management | 15/15 | |||||
| Tejwani et al. [40] | OTA/AO 44-B2, 44-B3 (SER-IV) | 266 ORIF | 1 | 213 available (80%) | Bimalleolar fractures were more common in women and patients with higher ASA | At 1 year, most patients have little or mild pain; bimalleolar fractures had worse outcomes than medial ligamentous injuries |
| SMFA | Worse for B3 vs B2 fracture | |||||
| AOFAS | Pain scores were comparable | |||||
| Regression analysis, controlled for age, gender, and ASA class | Poorer outcome for patients with bimalleolar fractures | |||||
| Clements et al. [7] | OTA/AO SER-IV (unimalleolar) | 51 nonoperative | 2.2 | AOFAS | 84.2 (all ankles) | Medial tenderness and ecchymosis are not sufficient to meet operative criteria; MCS of ≤ 4 mm was associated with excellent functional outcomes |
| Correlation of MCS with AOFAS | ||||||
| MCS 4 mm | 90.2 | |||||
| MCS 5 mm | 89.4 | |||||
| MCS 6 mm | 72.0 | |||||
| MCS 7 mm | 63.2 | |||||
| 4 mm vs 6 or 7 mm | Significant difference | |||||
| 5 mm vs 6 or 7 mm | Significant difference |
* Classification and fracture type include Lauge-Hansen (L-H) [22] and Orthopaedic Trauma Association/American Orthopaedic Association (OTA/AO) [1, 24]; †values expressed as means, with ranges in parentheses; ‡outcome assessments include Cedell criteria [4], SF-36 (mental and physical) [31], visual analog scale (VAS) [34], Olerud Molander Ankle (OMA) score [32], Short Musculoskeletal Function Assessment (SMFA) questionnaire [38], and American Orthopaedic Foot Ankle Score (AOFAS) [18]; SER = supination-external rotation; ORIF = open reduction and internal fixation; SD = standard deviation; ROM = range of motion; ASA = American Society of Anesthesiology; MCS = medial clear space (space between talus and medial malleolus on stress radiographs).
Two studies [2, 47], both published in the 1980s, showed, after nonoperative treatment of 67 SER-IV (unstable) ankle fractures, 42 (62.7%) were asymptomatic and 33 (49.3%) had some degree of osteoarthritis after a mean followup of 19.4 years.
In two studies, posttraumatic osteoarthritis was observed radiographically after operative treatment of unstable SER ankle fractures in 18 of 86 ankles (20.9%) after a mean followup of 5.5 years [13, 47]. Clinical evaluation showed 64 of 96 ankles (66.7%) were asymptomatic at a mean of 4.4 years after operative fixation of SER-IV ankle fractures [34, 47]. Correlation of clinical and radiographic findings was not reported in the original studies.
Three studies [3, 19, 34] used a general health assessment questionnaire (Table 2). A fracture of the medial malleolus, female gender, older age, higher American Society of Anesthesiologists grade, smoking, and lower educational level negatively influenced general health outcome, physical function, and pain.
Injury of the syndesmosis was recorded in only two studies. Bhandari et al. [3] suggested none of the 30 ankles required transsyndesmotic fixation after intraoperative stressing. Koval et al. [19] used MRI and reported two of 19 ankles had a syndesmosis injury.
Five studies [3, 13, 26, 34, 40] on operative treatment recorded 37 complications in 355 ankles (10.4%), including thromboembolic events, hardware failure, nonunions, and infections. One patient died of fatal pulmonary embolism.
Discussion
SER injuries, the most common pattern of ankle fractures, are treated either with closed reduction and cast immobilization or with operative fixation [1, 24, 27, 41]. We investigated which SER ankle fractures would benefit from operative treatment, regarding clinical outcome and development of osteoarthritis. Orthopaedic surgeons seem to advocate operative treatment for unstable SER ankle fractures.
While addressing our questions, we noted substantial limitations in the literature. First, there is no consensus regarding the definition of stability and descriptions of clinical outcome evaluation methodologies were heterogeneous. These are major limitations in comparing and combining data from different publications and extrapolating their results reliably. Second, the lack of randomized, controlled trials, or high-quality prospective studies, and the heterogeneity in the design and mode of outcome presentation do not provide strong evidence regarding the outcome of SER ankle fractures. Future studies should consider reporting results according to fracture type to enhance comparability across publications. Third, although some cohort studies have reported the incidence of radiographic osteoarthritis, it is unclear whether this was related to patients’ symptoms. Fourth, length of followup in some studies probably is inadequate to assess osteoarthritis, particularly clinically evident osteoarthritis, which typically takes decades to develop. Fifth, loss to followup in trauma populations (which probably is inevitable) may underestimate complications and unfavorable results of treatment. Finally, the small sample sizes in some studies limit the validity of their findings.
Given the literature limitations, we found nonoperative treatment of stable SER ankle fractures resulted in a similarly low (< 3%) incidence of radiographic osteoarthritis, compared with operative treatment, whereas greater than 80% of patients were asymptomatic regardless of the treatment received. Surgery for unstable SER ankle fractures, however, resulted in reduced incidence of radiographic osteoarthritis and better clinical outcomes according to the Cedell criteria [4], compared with nonoperative treatment (Table 2). The distinction between stable and unstable SER ankle fractures is an issue of controversy, and to our knowledge, there are no pathognomonic clinical or radiographic signs. Clinical signs (medial tenderness, swelling, bruising) are not reliable predictors of instability [11] and do not predict widening of the medial clear space on stress radiographs [12]. Bruising and tenderness could result from superficial deltoid ligament injury, whereas the deep deltoid remains intact providing stability [19]. Furthermore, radiographic criteria (talar tilt and medial clear space) probably are not well defined. In fact, osseous injury and radiographs did not predict the patterns of ligamentous injuries in 53% of ankles examined with MRI [14]. A dynamic examination (stress radiographs) could be of value. Stress radiographs [12, 25, 34] and the gravity stress test [15, 29] are methods proposed to distinguish between stable and unstable fracture patterns (Fig. 4). A medial clear joint space greater than 5 mm probably is predictive of instability [7, 33, 42]. The value of MRI [19] and ultrasound [6] in the diagnosis of complete deltoid ligament ruptures has been investigated and preliminary results are indicative of their accuracy. Additional research and long-term clinical followup are needed to establish criteria for instability of isolated distal fibular fractures and guide treatment.
Fig. 4A–B.
(A) A radiograph shows an isolated lateral malleolus fracture. Is it a stable injury or not? (B) A gravity stress radiograph shows a medial clear space opening greater than 5 mm and is indicative of an unstable fracture pattern.
Lauge-Hansen [22] suggested, more than 60 years ago, (stable) SER-II ankle fractures (approximately 30% of all ankle fractures [46]) do not require anatomic reduction, and optimal function can be expected. Long-term outcome studies [2, 46] have confirmed this. Clinical trials comparing operative with nonoperative treatment should consider including nonoperative treatment with a functional brace versus cast.
Nonoperative treatment of (unstable) SER-IV ankle fractures, however, has been associated with inferior results compared with operative treatment [28]. Our review suggests the incidence of radiographic changes of posttraumatic osteoarthritis in unstable SER ankle fractures treated nonoperatively approaches 50% at an average of 19 years’ followup (range, 3–34 years) [2, 47]. Individual studies [2, 20, 46, 47] did not clarify, however, whether radiographic evidence of osteoarthritis correlated with clinical outcome.
Anatomic reduction is essential for good outcomes of unstable SER ankle fractures [13]. The data we found in the literature suggest an incidence of 20% of radiographic joint degeneration at 5.5 years and presence of symptoms in 33% of ankles at 4.4 years in ankles treated operatively. However, the lack of rigorous validated outcome measures does not allow definite conclusions regarding the longer-term outcomes of these injuries. Furthermore, although trauma is the most common cause of ankle arthritis [35], the ankle has distinctive mechanical, biochemical, and anatomic characteristics making it resilient to aging and trauma [9]. Therefore, radiographic findings may correlate poorly with clinical symptoms [16].
Some studies [3, 19, 26, 34] reported outcomes of operative treatment of ankle fractures classified as Orthopaedic Trauma Association/American Orthopaedic Association B [1, 24], without clarifying whether these were unstable. Possibly, the inclusion of the B1 subgroup of stable fractures, which are associated with better outcomes [34], has influenced results. Additional research needs to confirm whether the results of operative treatment of isolated distal fibula fractures are better because of inclusion of some stable injuries.
Other factors (eg, social and educational status, smoking, alcohol consumption, medical comorbidities, age, gender) also are important [3, 35, 40], and their influence on outcome should be investigated further. Interpretation of outcome studies should take into account factors other than the fracture pattern.
The incidence of syndesmotic injuries, which can be as much as 39% [37] in unstable SER ankle fractures, and how it affects outcome did not receive adequate attention in the included studies. This should be an objective of future research.
Although surgery for ankle fractures is considered a routine procedure, it carries a remarkable risk of complications (10.4% in the studies reviewed). Therefore, it is important to accurately identify stable injuries and avoid unnecessary operations. Additional studies comparing operative with nonoperative treatment should be conducted with particular attention to methodology to avoid bias.
There is adequate evidence that nonoperative treatment is appropriate for stable SER ankle fractures. Unstable fractures appear best treated surgically but still are associated with symptoms and osteoarthritis. The current literature does not allow one to identify the responsible factors (eg, patient demographics, social factors, fracture characteristics, treatment methods, adequacy of fracture reduction). Multicenter prospective studies to evaluate factors influencing general health outcomes are needed.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This work was performed at Centre for Sports and Exercise Medicine and Frimley Park Hospital.
References
- 1.AO Surgery reference. Available at: http://www.aofoundation.org. Accessed November 14, 2008.
- 2.Bauer M, Jonsson K, Nilsson B. Thirty-year follow-up of ankle fractures. Acta Orthop Scand. 1985;56:103–106. doi: 10.3109/17453678508994329. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari M, Sprague S, Hanson B, Busse JW, Dawe DE, Moro JK, Guyatt GH. Health-related quality of life following operative treatment of unstable ankle fractures: a prospective observational study. J Orthop Trauma. 2004;18:338–345. doi: 10.1097/00005131-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Cedell CA. Is closed treatment of ankle fractures advisable? Acta Orthop Scand. 1985;56:101–102. doi: 10.3109/17453678508994328. [DOI] [PubMed] [Google Scholar]
- 5.Centre for Evidence-Based Medicine. Levels of evidence and grades of recommendation. Available at: http://www.cebm.net/index.aspx?o=1025. Accessed May 18, 2009.
- 6.Chen PY, Wang TG, Wang CL. Ultrasonographic examination of the deltoid ligament in bimalleolar equivalent fractures. Foot Ankle Int. 2008;29:883–886. doi: 10.3113/FAI.2008.0883. [DOI] [PubMed] [Google Scholar]
- 7.Clements JR, Motley TA, Garrett A, Carpenter BB. Nonoperative treatment of bimalleolar equivalent ankle fractures: a retrospective review of 51 patients. J Foot Ankle Surg. 2008;47:40–45. doi: 10.1053/j.jfas.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 9.Daniels T, Thomas R. Etiology and biomechanics of ankle arthritis. Foot Ankle Clin. 2008;13:341–352, vii. [DOI] [PubMed]
- 10.Danis R. Les fractures malleolaires. In: Danis R, ed. Theorie et Pratique de l’Osteosynthese. Paris, France: Masson et Cie; 1949:133–165.
- 11.DeAngelis NA, Eskander MS, French BG. Does medial tenderness predict deep deltoid ligament incompetence in supination-external rotation type ankle fractures? J Orthop Trauma. 2007;21:244–247. doi: 10.1097/BOT.0b013e3180413835. [DOI] [PubMed] [Google Scholar]
- 12.Egol K, Amirtharajah M, Tejwani NC, Capla EL, Koval KJ. Ankle stress test for predicting the need for surgical fixation of isolated fibular fractures. J Bone Joint Surg Am. 2004;86:2393–2398. doi: 10.2106/00004623-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Finnan R, Funk L, Pinzur MS, Rabin S, Lomasney L, Jukenelis D. Health related quality of life in patients with supination-external rotation stage IV ankle fractures. Foot Ankle Int. 2005;26:1038–1041. doi: 10.1177/107110070502601207. [DOI] [PubMed] [Google Scholar]
- 14.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma. 2006;20:267–272. doi: 10.1097/00005131-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Gill JB, Risko T, Raducan V, Grimes JS, Schutt RC., Jr Comparison of manual and gravity stress radiographs for the evaluation of supination-external rotation fibular fractures. J Bone Joint Surg Am. 2007;89:994–999. doi: 10.2106/JBJS.F.01002. [DOI] [PubMed] [Google Scholar]
- 16.Huch K, Kuettner KE, Dieppe P. Osteoarthritis in ankle and knee joints. Semin Arthritis Rheum. 1997;26:667–674. doi: 10.1016/S0049-0172(97)80002-9. [DOI] [PubMed] [Google Scholar]
- 17.Jones KB, Maiers-Yelden KA, Marsh JL, Zimmerman MB, Estin M, Saltzman CL. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br. 2005;87:489–495. doi: 10.2106/JBJS.D.02436. [DOI] [PubMed] [Google Scholar]
- 18.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 19.Koval KJ, Egol KA, Cheung Y, Goodwin DW, Spratt KF. Does a positive ankle stress test indicate the need for operative treatment after lateral malleolus fracture? A preliminary report. J Orthop Trauma. 2007;21:449–455. doi: 10.1097/BOT.0b013e31812eed25. [DOI] [PubMed] [Google Scholar]
- 20.Kristensen KD, Hansen T. Closed treatment of ankle fractures: stage II supination-eversion fractures followed for 20 years. Acta Orthop Scand. 1985;56:107–109. doi: 10.3109/17453678508994330. [DOI] [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 22.Lauge-Hansen N. Fractures of the ankle. III. Genetic roentgenologic diagnosis of fractures of the ankle. Am J Roentgenol Radium Ther Nucl Med. 1954;71:456–471. [PubMed] [Google Scholar]
- 23.Lundberg A, Goldie I, Kalin B, Selvik G. Kinematics of the ankle/foot complex: plantarflexion and dorsiflexion. Foot Ankle. 1989;9:194–200. doi: 10.1177/107110078900900409. [DOI] [PubMed] [Google Scholar]
- 24.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 25.McConnell T, Creevy W, Tornetta P., III Stress examination of supination external rotation-type fibular fractures. J Bone Joint Surg Am. 2004;86:2171–2178. doi: 10.2106/00004623-200410000-00007. [DOI] [PubMed] [Google Scholar]
- 26.McKenna PB, O’shea K, Burke T. Less is more: lag screw only fixation of lateral malleolar fractures. Int Orthop. 2007;31:497–502. doi: 10.1007/s00264-006-0216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michelson JD. Fractures about the ankle. J Bone Joint Surg Am. 1995;77:142–152. doi: 10.2106/00004623-199501000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Michelson JD, Magid D, McHale K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma. 2007;21:307–315. doi: 10.1097/BOT.0b013e318059aea3. [DOI] [PubMed] [Google Scholar]
- 29.Michelson JD, Varner KE, Checcone M. Diagnosing deltoid injury in ankle fractures: the gravity stress view. Clin Orthop Relat Res. 2001;387:178–182. doi: 10.1097/00003086-200106000-00024. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Schulz KF, Altman DG; CONSORT. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol. 2001;1:2. [DOI] [PMC free article] [PubMed]
- 31.Naughton MJ, Anderson RT. Outcomes research in orthopaedics: health-related quality of life and the SF-36. Arthroscopy. 1998;14:127–129. doi: 10.1016/s0749-8063(98)70029-5. [DOI] [PubMed] [Google Scholar]
- 32.Olerud C, Molander H. A scale for symptom evaluation after ankle fractures. Arch Orthop Trauma Surg. 1984;103:190–194. doi: 10.1007/BF00435553. [DOI] [PubMed] [Google Scholar]
- 33.Park SS, Kubiak EN, Egol KA, Kummer F, Koval KJ. Stress radiographs after ankle fracture: the effect of ankle position and deltoid ligament status on medial clear space measurements. J Orthop Trauma. 2006;20:11–18. doi: 10.1097/01.bot.0000189591.40267.09. [DOI] [PubMed] [Google Scholar]
- 34.Ponzer S, Nåsell H, Bergman B, Törnkvist H. Functional outcome and quality of life in patients with Type B ankle fractures: a two-year follow-up study. J Orthop Trauma. 1999;13:363–368. doi: 10.1097/00005131-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46. [PMC free article] [PubMed] [Google Scholar]
- 36.Sneppen O. Long-term course in 119 cases of pseudarthrosis of the medial malleolus. Acta Orthop Scand. 1969;40:807–816. doi: 10.3109/17453676908989545. [DOI] [PubMed] [Google Scholar]
- 37.Stark E, Tornetta P, III, Creevy WR. Syndesmotic instability in Weber B ankle fractures: a clinical evaluation. J Orthop Trauma. 2007;21:643–646. doi: 10.1097/BOT.0b013e318157a63a. [DOI] [PubMed] [Google Scholar]
- 38.Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short musculoskeletal function assessment questionnaire: validity, reliability, and responsiveness. J Bone Joint Surg Am. 1999;81:1245–1260. doi: 10.1302/0301-620X.81B6.9794. [DOI] [PubMed] [Google Scholar]
- 39.Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy: a critical review. Am J Sports Med. 2001;29:315–320. doi: 10.1177/03635465010290031101. [DOI] [PubMed] [Google Scholar]
- 40.Tejwani NC, McLaurin TM, Walsh M, Bhadsavle S, Koval KJ, Egol KA. Are outcomes of bimalleolar fractures poorer than those of lateral malleolar fractures with medial ligamentous injury? J Bone Joint Surg Am. 2007;89:1438–1441. doi: 10.2106/JBJS.F.01006. [DOI] [PubMed] [Google Scholar]
- 41.Tile M. Fractures of the ankle. In: Schatzker J, Tile M, eds. The Rationale of Operative Fracture Management. Ed. New York, NY: Springer; 2005:551–590.
- 42.Bekerom MP, Mutsaerts EL, Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2009;129:227–235. doi: 10.1007/s00402-008-0768-6. [DOI] [PubMed] [Google Scholar]
- 43.Weber BG. Die Verletzungen des oberen Sprunggelenkes. Bern, Switzerland: Huber Verlag; 1972. [Google Scholar]
- 44.Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am. 2008;90:1570–1578. doi: 10.2106/JBJS.G.01673. [DOI] [PubMed] [Google Scholar]
- 45.Yablon IG, Heller FG, Shouse L. The key role of the lateral malleolus in displaced fractures of the ankle. J Bone Joint Surg Am. 1977;59:169–173. [PubMed] [Google Scholar]
- 46.Yde J, Kristensen KD. Ankle fractures: supination-eversion fractures of stage II: primary and late results of operative and non-operative treatment. Acta Orthop Scand. 1980;51:695–702. doi: 10.3109/17453678008990863. [DOI] [PubMed] [Google Scholar]
- 47.Yde J, Kristensen KD. Ankle fractures: supination-eversion fractures of stage IV: primary and late results of operative and non-operative treatment. Acta Orthop Scand. 1980;51:981–990. doi: 10.3109/17453678008990904. [DOI] [PubMed] [Google Scholar]