Abstract
When the superficial fibers of the medial collateral ligament of the knee are torn without tearing of the deep fibers, the anterior superficial fibers may displace over the pes anserinus tendons, so that healing back to the tibial insertion site may be jeopardized. As only the anterior superficial and not the posterior superficial or deep fibers are disrupted, the knee will not have increased valgus laxity in extension whereas there is not a firm end point in 30° flexion. The clinical findings could be confused with those of a Grade 2 medial collateral ligament sprain that generally is not associated with displacement of the anterior fibers over the pes anserinus tendons. We describe the diagnostic findings confirmed with surgical exploration of two Stener-like disruptions of the medial collateral ligament of the knee.
Introduction
Medial collateral ligament (MCL) sprains are common injuries of the knee. Most often these injuries are caused by a valgus force applied to the lower leg leading to rupture of the MCL fibers at the tibial insertion site. These MCL injuries have been graded as Grade 1 to 3 sprains [6]. Grades 1 and 2 tears are incomplete with maximally 5 and 10 mm of joint line opening in 30° flexion, whereas the joint line opens greater than 10 mm without a firm end point in Grade 3 tears, which are considered complete [6]. Most MCL sprains do not warrant surgical treatment [1, 2, 5]. However, numerous authors have suggested specific locations of rupture may warrant different treatment regimens [1, 2, 4, 5].
Disruption of the distal insertion site of the ulnar collateral ligament of the first metacarpophalangeal (MCP) joint and displacement over the adductor aponeurosis were described by Stener [8] in 1962. Some surgeons believe the Stener lesion, also known as a skier’s or gamekeeper’s thumb, warrants surgery to restore the laxity and preserve the functional stability of the first MCP joint [3, 8].
We have observed an analogous lesion in the knee where the anterior fibers of the superficial MCL were displaced over the pes anserinus tendons. In this report, we describe the clinical, radiographic, and surgical findings of a Stener-like lesion of the MCL in two patients.
Case Reports
The first patient was a 42-year-old woman who was a recreational-level competitive athlete who was referred to our clinic 3 weeks after a skiing accident. She had sustained a valgus trauma of the left knee. She was unable to bear weight on the involved leg and was using crutches and was treated with a valgus constrained brace and antiinflammatory medication. The proximal tibia and medial joint line were swollen, ecchymotic, and very tender to palpation. A valgus load was applied with the knee in extension. This did not show any abnormal opening of the medial joint line, but the maneuver was very painful. When the valgus load was applied with the knee in 30° flexion, there was a 5 to 10 mm increased opening of the medial joint line and no firm end point. There was no tenderness, ecchymosis, or laxity of the posteromedial corner. The McMurray maneuver resulted in pain over the medial meniscus. The anterior drawer and Lachman test showed a 5- to 10-mm anterior laxity. The pivot shift test was too painful to conduct. Based on the clinical findings, we suspected a Grade 2 MCL sprain and an ACL rupture. MRI was done to confirm an ACL tear and evaluate the MCL given it was very painful on testing. The MRI identified a bunched MCL with displacement of the tibial insertion site over the pes anserinus tendons (Fig. 1A). We observed no injuries or edema of the posteromedial soft tissue corner. The proximal MCL insertion site was intact (Fig. 1B). The diagnoses of a torn posterior horn of the medial meniscus and ruptured ACL were confirmed with edema and disrupture of the ACL fibers at the femoral insertion site. The patient was scheduled for a two-stage treatment: an arthroscopic resection of the posterior horn of the medial meniscus and surgical exploration of the MCL followed by ACL reconstruction after full range of motion (ROM) was regained.
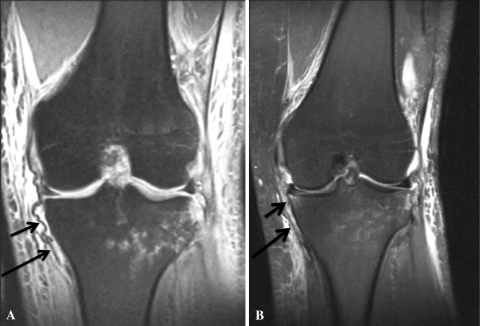
Fig. 1A–B.
MRI findings of the left knee of the first patient are shown. (A) The typical bunched MCL fibers are obvious on this T2-weighted MR image of the left knee (small arrow). The fibers are short and abruptly jump over the semitendinosus tendon (large arrow). Contrecoup edema is evident in the lateral tibia plateau. The femoral insertion site remained intact. (B) The semitendinosus tendon is apparent (large arrow). The bunched MCL fibers run from the femur under the tendon and disappear from the image halfway down (small arrow). This shortened and bunched appearance of the MCL on the coronal MR images can be considered pathognomonic for the Stener-like lesion of the MCL.
The second patient was a 15-year-old male, high-level athlete who injured his right knee during a landing maneuver while ski jumping. Initially the patient was treated by another physician with a valgus constrained brace, partial weightbearing, rest, and antiinflammatory medication. The patient was seen in our sports medicine clinic after 1 week. There was localized, extremely painful swelling and ecchymosis over the tibial insertion site of the MCL and the medial joint line. Similar to the first patient, the clinical laxity testing showed a normal laxity in extension and a 5- to 10-mm opening of the joint line in 30° flexion with no firm end point. The posteromedial corner and the ACL did not show any abnormal laxity. A clinical Grade 2 MCL sprain was diagnosed. MRI was performed to exclude an ACL tear and evaluate the swelling over the medial joint line. MRI showed findings of the MCL identical to those of the first patient. We identified no other structural lesions and scheduled the patient for surgical exploration.
We operated on both patients 4 weeks after injury. The patients were positioned supine and were administered general anesthesia to have their knee laxity reevaluated. Special attention was given to the posteromedial capsule. No additional laxity was found and the clinical findings were identical to those of the preoperative examination. We did not exsanguinate the leg to avoid stretching and tensioning of the hamstrings.
The knees were evaluated arthroscopically to inspect the intraarticular part of the posteromedial corner and capsule. This was performed without using a pressure fluid pump. The capsular findings appeared normal. The torn fragment of the medial meniscus and the remnants of the ACL were removed in the first patient.
After the arthroscopy, we made a 5- to 7-cm longitudinal incision over the medial joint line with the involved foot leaning against the contralateral leg and the hip in external rotation and abduction (ie, the leg was in a figure four position). The skin was reflected and the fascia was exposed. The fascia was incised with a gentle curve from distal to the vastus medialis fibers to the insertion site of the pes. Retraction of the fascia exposed the pes tendons and showed the superficial portion of the MCL displaced over the tendons (Fig. 2). The femoral insertion of the superficial MCL portion was inspected and was judged intact. The pes tendons were inspected and were not injured. With the knee flexed, the tendons were retracted from the operation field using two retractors (Fig. 3). The displaced MCL fibers were relocated underneath the pes tendons with an arthroscopic grasper clamp. The posteromedial corner was inspected carefully for any ligamentous or capsular disruptions. No gap or abnormal injury to the deep MCL or the posteromedial corner was found. A valgus stress again was applied to the knee in extension under direct observation and palpation, and this did not open the medial joint line or the posteromedial capsule. Displacement of the superficial MCL fibers under a valgus load in 30° flexion was obvious. Given it appeared only the superficial MCL portion had been ruptured off the insertion site, which we then identified based on the length of the fibers, and with blunt dissection using a sponge, a trough was made in the insertion site using an osteotome (Fig. 4). Two Mitek™ anchors (DePuy, Brussels, Belgium) were introduced into the bone and the nonabsorbable suture wires were sutured through the torn MCL with Bunnell-type stitches (Fig. 3). Finally, the sutures were tightened with the knee in 30° flexion (Fig. 5). We closed the wound using absorbable Vicryl® 3/0 subdermal and Monocryl® 3/0 intradermal sutures (Ethicon, Brussels, Belgium).
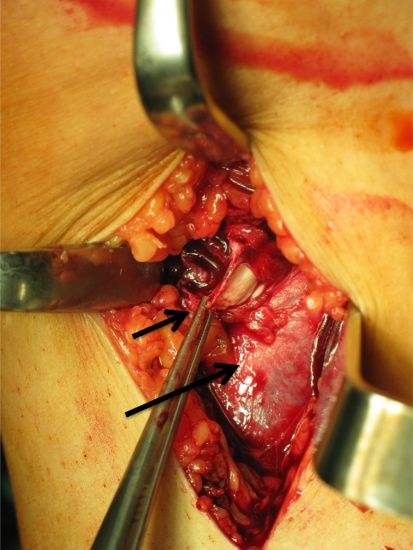
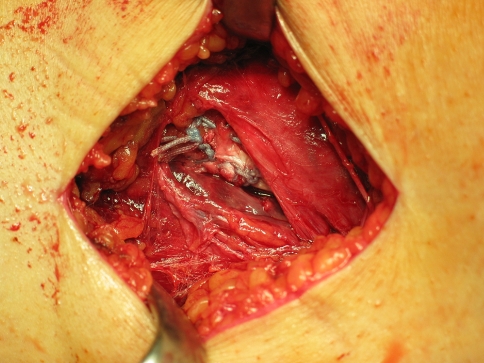
Fig. 2.
The surgical findings confirmed the MRI findings in the right knee of the second patient. Retraction of the superficial fascia exposed the pes tendons (underneath the forceps, large arrow). The superficial portion of the MCL was displaced over the pes tendons and was grasped with the forceps (small arrow).
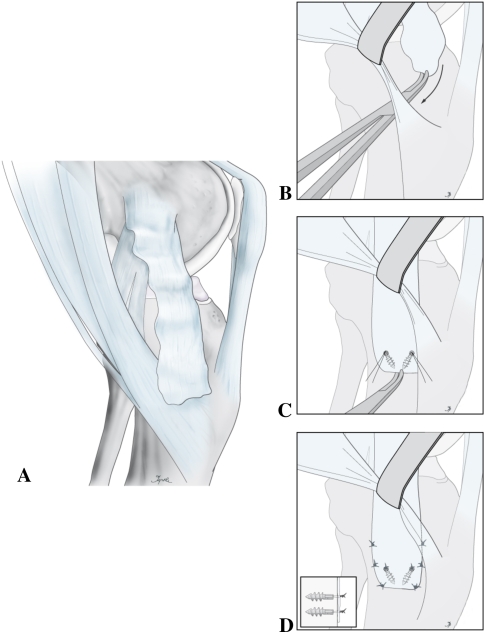
Fig. 3A–D.
The surgical technique is shown. (A) The diagram shows the preoperative injury. (B) First, the tendons were retracted from the operation field using two retractors. The MCL fibers were retracted underneath the pes tendons with an arthroscopic grasping clamp. The native tibial insertion site of the MCL was identified with blunt dissection using a sponge and a trough was made using an osteotome. (C) Then, two Mitek™ anchors were introduced and the nonabsorbable suture wires were sutured through the torn MCL with Bunnell-type stitches. (D) Finally, the MCL fibers were tightened and sutured to the remaining soft tissues in 30° flexion.
Fig. 4.
After retraction of the pes tendons, a trough was made at the tibial insertion site of the MCL with an osteotome as seen in this intraoperative photograph of the second patient.
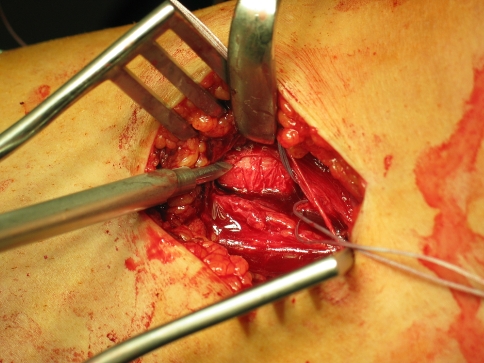
Fig. 5.
An intraoperative photograph of the second patient shows the final result after tightening the sutures. The MCL fibers were retracted underneath the pes tendons (above) and tightened and sutured to the remaining soft tissues in 30° flexion.
The patients were treated at different institutions for different injuries and therefore the rehabilitation program was slightly different. For immobilization of their knees, both patients wore a brace fixed in 30° flexion for 5 (first patient) and 4 (second patient) weeks. Full ROM was allowed from then on. Isometric quadriceps and hamstring exercises were initiated the first postoperative day. For the first 3 weeks, the patients were not allowed to bear weight, followed by 2 weeks of partial weightbearing. In both patients, at 5 weeks after surgery, full ROM, full weightbearing wearing a brace, and closed-chain exercises of the quadriceps and hamstrings were allowed.
In the first patient, the brace was not removed for normal daily activities before the ACL reconstruction. Three months after surgery, full ROM was regained and the ACL was reconstructed with a gracilis and semitendinosus autograft. The intraoperative findings of the MCL at the time of autograft preparation showed a well-integrated, stable, and nicely fixed MCL. The gracilis and semitendinosus tendons were scarred down, requiring meticulous attention when releasing them. They were cut approximately 1 cm from their tibial insertion site. The ACL reconstruction was performed without any intraoperative or postoperative complications. The patient followed a standard ACL rehabilitation protocol with closed-chain quadriceps and hamstrings strengthening and ROM exercises. In the second patient, the brace was removed at 8 weeks for normal daily activities. Training activities wearing the brace were allowed at this point. Three months after surgery, the patient was completely pain free, had regained his muscle strength, and had normal clinical laxity testing. Competitive skiing without the brace was allowed.
At final followup at 18 months, both patients had regained normal stability of the MCL without any increased joint line opening in extension and 30° flexion in comparison to the contralateral knee. The anterior drawer and Lachman tests had returned to normal in comparison to the contralateral knee in the first patient. Both patients were completely pain free and did not have any complaints of instability. Both patients resumed skiing activities. High-level, competitive skiing was resumed without any complaints in the second patient.
Discussion
Sprains of the MCL are common and represent the most frequent ligamentous injury of the knee. We describe here Stener-like lesions of the MCL. We suspect these lesions are rare and could be considered Grade 4 MCL sprains as they warrant special attention and approach.
The most remarkable clinical findings were the ecchymosis and abnormally marked and very tender swelling over the medial joint line. In addition, other clinical findings were not conclusive and the clinical laxity testing was confusing and misleading. Grades 1 and 2 sprains of the MCL present with a clinically increased valgus laxity in 30° flexion but not in extension. We observed similar findings in our patients, but importantly there was no firm end point in 30° flexion. Treatment of these sprains generally is successful with a protective brace for 6 to 9 weeks in combination with ROM and closed-chain exercises [6]. Most commonly [1, 2, 5], and in our respective institutions, surgical treatment of MCL sprains is reserved only for Grade 3 sprains with an increased valgus laxity in extension and in 30° flexion because the deep fibers have been disrupted and often other ligaments such as the ACL or PCL have been injured. The clinical findings were confusing because the intact deep and superficial posterior fibers of the MCL formed a restraint to increased opening in extension whereas the absence of a firm end point in 30° flexion was caused by the disrupture of the superficial anterior fibers. We suggest performing MRI if the patient is clinically diagnosed as having a Grade 1 or 2 MCL sprain but if the pain and swelling on the medial side of the knee are not in proportion to the suspected injury. Moreover, the absence of a firm end point in 30° flexion seems an important indicator for major ligament injury such as a Grade 3 or Stener-like lesion of the MCL. Although our experience is limited to two patients and we do not know the natural history of these injuries, we suspect a Stener-like MCL injury warrants a treatment plan different from that for Grade 2 sprains.
MRI was performed to evaluate the ACL but also because of the remarkable swelling and the extensive pain over the medial joint line. The MCL had a typical appearance on MRI that was confirmed during explorative surgery. The distal MCL was twisted proximally and therefore was short, bunched, and folded on consecutive coronal images. A thorough evaluation of the posteromedial capsule and the deep MCL portion did not reveal any injury. It therefore was confirmed only the anterior fibers had been torn. Nevertheless, we would advise always checking for integrity of the posteromedial corner.
The appearance of this lesion was similar to that of the displaced lesion of the ulnar collateral ligament of the first MCP joint over the adductor aponeurosis, as described by Stener [8]. As with the Stener lesion, direct healing of the displaced MCL fibers to the bony insertion site of the tibia was presumed impossible, thereby possibly leading to persistent valgus laxity and residual functional instability. Surgical repair or at least relocation of the MCL should be considered in our opinion.
A two-stage approach with immediate reinsertion was used in the first patient to prevent the MCL from scarring down and retracting thereby possibly compromising reinsertion onto the tibia. The MCL repair was protected with a brace for 5 weeks without ROM exercises. Once ROM of the knee had been fully regained (at 3 months), the ACL reconstruction with a semitendinosus and gracilis autograft was successfully performed. The intraoperative findings of the MCL at the time of autograft preparation showed a well-integrated and stable MCL. It has been suggested the MCL does not need to be repaired in combination with ACL injuries [7], but especially in these cases, we suspect residual displacement of the MCL fibers bears a higher risk of reconstruction failure owing to possibly increased risk of residual valgus laxity.
The surgical findings of both patients were similar. Our surgical technique was similar to that for Grade 3 MCL tear reinsertions but was limited to the anterior fibers. We note several details of our procedures. First, the tourniquet was inflated without prior exsanguination of the leg, thereby preventing the tendons from becoming tensed and stretched, leaving it more difficult to retract them away from the tibial insertion site. Second, the knee was held in a flexed position during the procedure to relax the tendons and to move the tibial insertion site more proximally. Third, in both patients, the ligament had been torn off the tibia in one piece without the end of the ligament being frayed. Nevertheless, we suggest anticipating a possible MCL reconstruction in the case of a frayed and irreparable ligament. In these cases, an Achilles tendon allograft or a semitendinosus autograft reconstruction [1] might be useful.
Stener-like lesions of the MCL are rare, but they do exist and should be suspected in the presence of a remarkable, abnormally tender swelling and ecchymosis over the medial joint line and proximal tibia. Valgus laxity testing is not conclusive and MRI findings of a short, bunched MCL can be considered highly suspicious for a Stener-like lesion of the MCL, which can be treated with surgical exploration and refixation to the tibial insertion site.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Catholic University Hospitals and Facharzt für Unfallchirurgie und Sporttraumatologie.
References
- 1.Azar FM. Surgical treatment of ACL/PCL/medial-side knee injuries. Oper Tech Sports Med. 2003;11:248–256. doi: 10.1016/S1060-1872(03)00048-0. [DOI] [Google Scholar]
- 2.Azar FM. Evaluation and treatment of chronic medial collateral ligament injuries of the knee. Sports Med Arthrosc. 2006;14:84–90. doi: 10.1097/01.jsa.0000212311.77817.c8. [DOI] [PubMed] [Google Scholar]
- 3.Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5:224–229. doi: 10.5435/00124635-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Kim SJ, Lee DH, Kim TE, Choi NH. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br. 2008;90:1323–1327. doi: 10.1302/0301-620X.90B10.20781. [DOI] [PubMed] [Google Scholar]
- 5.Lonergan KT, Taylor DC. Medial collateral ligament injuries of the knee: an evolution of surgical reconstruction. Tech Knee Surg. 2002;1:137–145. [Google Scholar]
- 6.Noyes FR, Grood ES, Torzilli PA. Current concepts review: the definitions of terms for motion and position of the knee and injuries of the ligaments. J Bone Joint Surg Am. 1989;71:465–472. [PubMed] [Google Scholar]
- 7.Pressman A, Johnson DH. A review of ski injuries resulting in combined injury to the anterior cruciate ligament and medial collateral ligaments. Arthroscopy. 2003;19:194–202. doi: 10.1053/jars.2003.50054. [DOI] [PubMed] [Google Scholar]
- 8.Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpo-phalangeal joint of the thumb: a clinical and anatomical study. J Bone Joint Surg Br. 1962;44:869–879. [Google Scholar]