Introduction
It is widely accepted that America is in the midst of an obesity pandemic (1,2). Substantial research is directed toward both understanding how and why this has occurred and toward identifying effective ways to prevent and treat obesity. Permanent behavior change is required for any change in body weight, but the extent of behavior change needed varies with the desired outcome. The term “energy gap” was coined to estimate the change in energy intake and energy expenditure behaviors required to achieve different body weight outcomes in individuals and populations (3). Since the original article about the energy gap, the term has become widely used (and misused) by researchers interested in both prevention of weight gain and treatment of obesity (3-14). It has been argued that the energy gap fails to consider that energy stores continue to increase with weight gain so that there is a cumulative energy gap that builds over time between obese and non-obese individuals so that small changes in eating and physical activity would be insufficient to reverse the obesity pandemic (13,14). The purpose of this commentary is to more precisely clarify the concept of the energy gap (or energy gaps) and discuss how the concept can be properly used as a tool to help understand and address obesity.
How did the obesity pandemic develop?
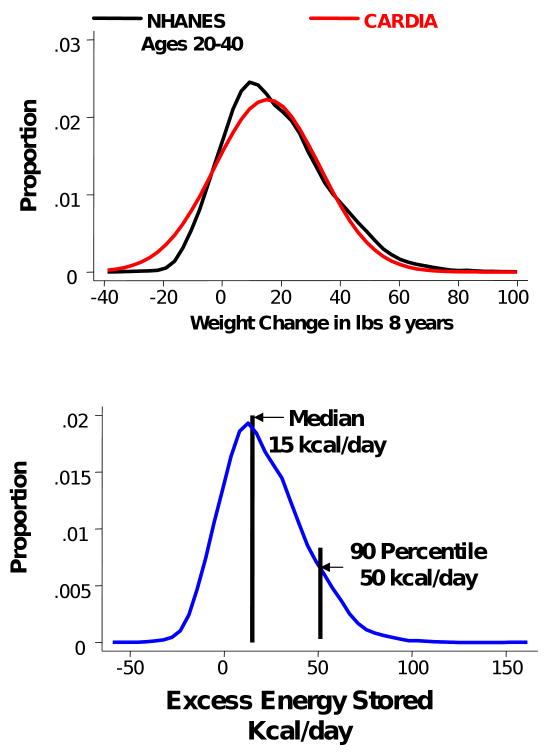
The concept for an energy gap arose subsequent to research to better understand how the high prevalence of obesity might have arisen in the U.S. Longitudinal (CARDIA study) data and cross-sectional (NHANES) data sets that covered a period of about 8 years were analyzed to determine the distribution of weight gain over time (3). Results showed that most people were gaining weight gradually over time, with the average American adult gaining 0.5-1 kg/year. The population distribution for rate of accumulation of excess body energy was assessed by assuming that one pound of added body weight represents an extra 3500 kcal of body energy. Figure 1 shows the distributions for weight change (top) and excess energy accumulation (bottom) in the U.S. adult population over 8 years. Most of the U.S. population is gradually gaining weight and the difference between energy intake and energy expenditure that produces the observed population rate of weight gain is small on a daily basis. It is not certain that people experience positive energy balance every day; however, it does appear that the relatively modest .5-1 kg median yearly weight gain can be explained by a relatively small average daily positive energy imbalance.
Figure 1.
This figure shows the distribution of weight gain (top) and estimate energy accumulation (bottom) over 8 years in the U.S. adult population. Reprinted with permission from reference #3.
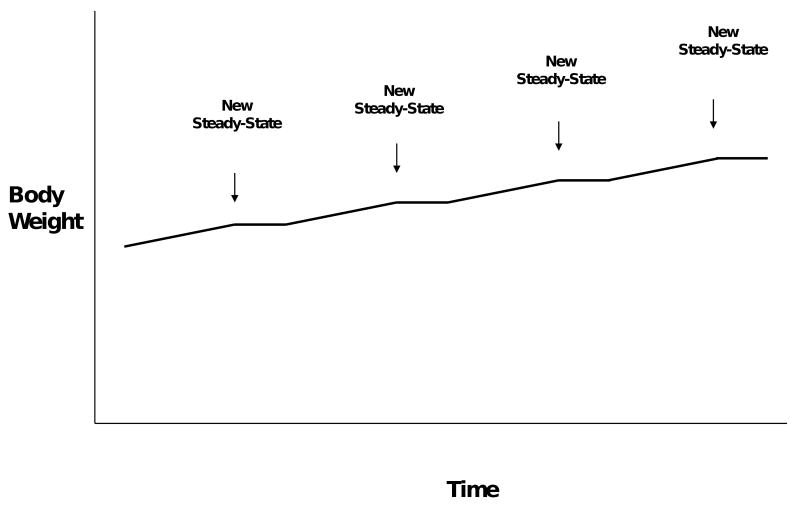
Eating an extra 100 kcal/day over current energy needs today will not lead to continuous weight gain. This is because weight gain is accompanied by increased energy requirements (14) which will eventually offset the increased energy intake, leading to a new steady state of energy balance. Eating an extra 100 kcal/day would lead to a small amount of weight gain and reestablishment of energy balance at this new, slightly higher, body weight. The higher energy requirement, in turn, likely leads to increased energy intake and thus may create a “ratchet” effect where people gain weight because of a small, acute energy imbalance, reach a new steady state of energy balance at the higher weight for a period of time, and then experience additional positive energy balance and more weight gain (see Figure 2).
Figure 2.
Continued weight gain in the population have occurred in a “ratchet” fashion where periods of slight positive energy balance are followed achieving a new steady-state of energy balance, followed by other periods of slight positive energy balance.
The rate of weight gain and energy accumulation has now been estimated for many different adult populations, and found to be small in all instances (see Table 1). This suggests that gradual weight gain, subsequent to a small, consistent degree of positive energy balance is a reasonable hypothesis for how the obesity pandemic has emerged globally.
Table 1. The rate of energy accumulation and the estimated energy gap for prevention of weight gain in different populations.
| Population | Energy Accumulation (kcal/day) | Energy Gap (kcal/day) |
|---|---|---|
| U.S. Adults (3) | 15; 50 for 90th percentile | 30; 100 for 90th percentile |
| Australian Women (4) | 10.5 | 21 |
| Chinese Adults (5) | 22.5 | 45 |
| Adult Pima Indians (6) | 30.6 | 61.2 |
| Scottish Adults (7) | 11.5 23 |
23 for 42.2% of population; 46 for 17% of population |
| Swedish Adults (8) | 4.1 6.2 |
8.2 for men 12.4 for women |
| Chilean Women (9) aged 40-53 years | 16.8 | 33.6 |
Research investigations have also begun to provide insight into the way that obesity develops in children and adolescents. It appears that children and adolescents are growing at an excessive rate and it is possible to estimate the degree of positive energy balance that is responsible for the excessive rate of weight gain. Only a few studies have been conducted in these populations and the estimated energy gap producing weight gain ranges from 22 to 165 kcal/day (10-12).
The persistent population-wide weight gain phenomenon suggests that achieving energy balance and weight stability is not the norm and most people continue to consume slightly more energy than they expend, even as their energy requirements increase following weight gain. While some people within populations are gaining weight at a very high rate and may be consuming hundreds of calories per day above energy needs, the published data are most consistent with lesser degrees of positive energy balance for most of the population.
The concept of the energy gap
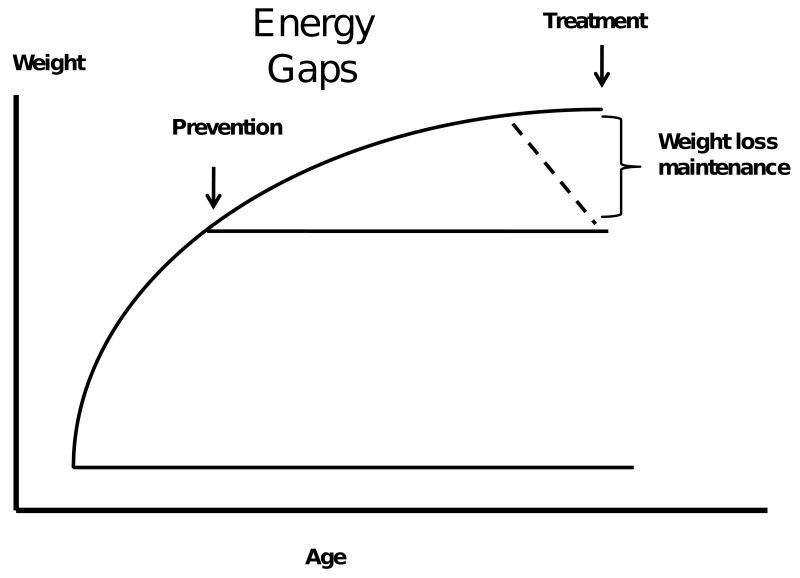
The term “energy gap” was coined to estimate the degree of change in the energy balance point (the absolute energy intake and expenditure at which balance is reached) required for success in body weight goals. The two primary strategies that are especially relevant to the energy gap, in concept, are prevention of excessive weight gain and maintenance of weight loss (Figure 3).
Figure 3.
The energy gap for prevention of weight gain is the change in energy balance required to prevent further weight gain while the energy gap for weight loss maintenance is the change in energy balance required to permanently maintain a lower body weight.
The energy gap for weight gain prevention is the amount of change in the energy balance point needed to prevent further weight gain, regardless of current body weight or body mass index (BMI), at any given point in time. The energy gap for weight gain prevention in the U.S. adult population was estimated as double the daily energy accumulation, taking into consideration that excess energy is not stored with 100% efficiency. This is most likely a conservative estimate (15). The median energy gap in the U.S. for prevention of weight gain would be 30 kcal/day (2 × 15 kcal/day) and the energy gap for the 90th percentile of weight gain would be 100 kcal/day (2 × 50 kcal/day) (3). An estimated 100 kcal/day change in the population energy balance point (produced by any combination of decreases in energy intake and increases in energy expenditure) could theoretically prevent weight gain (not restore normal weight) in 90% of the U.S. adult population.
The energy gap for prevention of weight gain can be calculated for any population where weight gain over time is known. Further, it can be calculated for different subgroups within those populations. The energy gap associated with rate of weight gain is shown for various adult populations around the world in Table 1. In every case, the energy gap in other countries where data are available is lower than in the U.S. These data suggest that small changes in behavior that lead to small changes in the energy balance point could be sufficient to avoid additional weight gain for individuals and populations.
The energy gap for weight loss maintenance
The energy gap for weight loss maintenance was defined as the amount of change in the energy balance point needed to maintain a specific amount of weight loss (16). Because energy requirements decrease proportionally with a decrease in body mass, energy requirements are lower after weight loss than before. The energy gap for weight loss maintenance is a tool that provides an estimate of how much energy requirements change with weight loss, which in turn, provides an estimate of how much energy balance must be changed to maintain the new, lower body weight. This can, for example, provide an estimate of how much behavior change is required to maintain a given amount of weight loss.
The energy gap for weight loss maintenance can be calculated or measured. It can be calculated using any of several regression equations linking energy requirements with body weight (14,17,18). Using this method, the change in energy requirements for any amount of change in weight could be estimated. This provides an indication of how much the energy balance point must change to maintain a weight loss. Using such regression equations, it has been pointed out that the energy gap required to go from a very obese state to a non-obese state is extremely large (13,14).
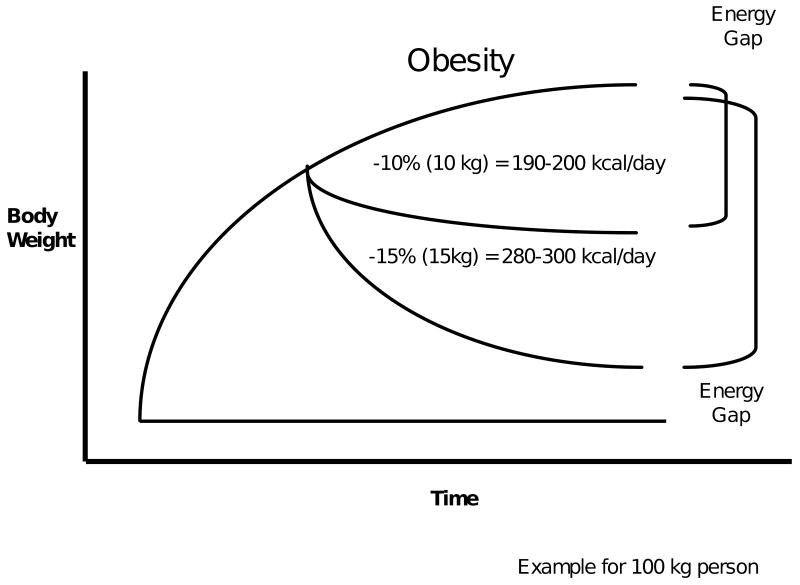
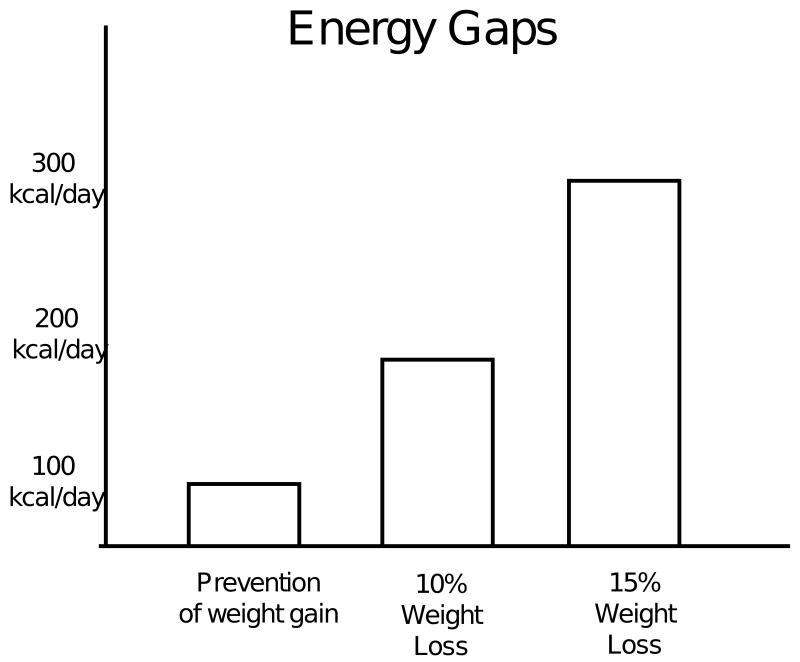
One interesting question is whether treatment of obesity could be achieved by simply reversing the amount of positive energy balance that caused weight gain or whether, as suggested by some human (19,20) and rodent (21,22) studies, the obese state produces metabolic alterations that serve to protect the obese state. If this is the case, then estimates of the energy gap from regression equations could underestimate the true energy gap. Whole room calorimetry has been used to measure energy expenditure before and after weight loss and have developed prediction equations for estimating the energy gap (unpublished results). The way the studies were done accounted for changes in energy expenditure due to resting metabolism, energy expenditure of physical activity and the thermic effect of food. These formulas would predict an energy gap of 190-200 kcal/day for a 100 kg person losing 10% of body weight and an energy gap of 280-300 kcal/day for this same person losing 15% of body weight (Figure 4). The energy gap for weight loss maintenance can provide an estimate of how much behavior change is required to maintain a given amount of weight loss. This analysis indicates that in order to create and maintain significant body weight loss (i.e. obesity treatment) large behavioral changes are needed. This is in stark contrast to primary obesity prevention in which small behavioral changes can eliminate the small energy imbalance that occurs before the body has gained significant weight. Because the body has not previously stored this “new” excess energy, it does not defend against the behavioral strategies as happens when the body loses weight.
Figure 4.
This figure shows our estimates of how much change in energy balance would be required for a 100 kg person to maintain a 10 and a 15% weight loss. Modified with permission from reference #33.
Using the energy gap to guide strategies to address obesity
The energy gap for weight loss maintenance can be a useful tool to help with obesity treatment. A great deal of effort is devoted to developing better interventions to treat obesity. With the exception of bariatric surgery, there has not been a great deal of success in helping people maintain significant weight losses. Many people can achieve significant weight losses with our current interventions, but very little of this weight loss seems to be maintained by most people over the long-term (23,24). The energy gap can help estimate the degree of behavior change that must be maintained to keep a given amount of weight off for any individual. For example, if the energy gap for a given weight loss maintenance is estimated to be 300 kcal/day, this can lead to a specific goal for changing diet and physical activity rather than generic advice to eat less and exercise more. This could be 300 kcal/day of additional physical activity, a reduction of 300 kcal/day from usual energy intake or a combination of tactics such as adding 150 kcal/day of physical activity and reducing 150 kcal/day from usual energy intake. In this case, the energy gap is a useful tool to individualize behavioral strategies for weight loss maintenance.
It is important to note that the energy gap for weight loss maintenance compares the changes needed to go from one steady state (the obese state) to another (maintenance of weight at a reduced level). Weight loss can be successfully achieved slowly by imposing a small degree of negative energy balance or more quickly by imposing a larger degree of negative energy balance. While achieving weight loss can be accomplished in most individuals, our challenge is in maintaining changes in diet and physical activity over the long-term to keep the weight off. We are not very successful in doing this for weight losses of 10% or greater.
Large vs small behavior changes to address obesity
Figure 5 shows estimates of the energy gaps for prevention of weight gain and for maintenance of 10 and 15% weight loss. Obviously it would be desirable to produce and maintain large changes in diet and physical activity in order to treat existing obesity and efforts should continue to develop better ways to accomplish this. But, what is achievable with current effirts to sustain behavior change should further be explored. Not all efforts should be devoted to obesity treatment when it may be possible, using a small changes approach, to prevent further weight gain in those already overweight or obese and to prevent millions of people from becoming overweight or obese.
Figure 5.
The energy gap for prevention of weight gain is compared to the energy gaps for maintaining a 10 and 15% weight loss.
Small behavior changes
The relatively small energy gap for preventing weight gain suggests that significant success in addressing obesity could be achieved with small behavioral changes, but effective approaches to produce and sustain these changes are still needed. There is accumulating evidence that small behavior changes, on the order of 100 kcal/day or less can be achieved and sustained by many people. For example, Bravata et al. reviewed studies using pedometers to increase physical activity (25). Providing pedometers and step goals was associated with an increase of about 2500 steps/day which roughly translates into 100 kcal/day. Similarly, small changes in energy intake appear to be achievable (26,27). Finally, it has been demonstrated that the small behavior change approach could be used to reduce excessive weight gain in overweight and obese children when provided with a small changes program aimed at families (28,29).
It has been previously argued that a small changes approach could be one effective tool in addressing obesity prevention (3,30). Small behavior changes are insufficient to maintain substantial weight loss but could prevent additional weight gain in adults regardless of BMI, and could prevent excessive weight gain in children. At a minimum, this strategy could help stabilize obesity rates and prevent the pandemic from worsening. Over long periods of time, this prevention of weight gain strategy could actually reduce obesity prevalence. For example, if everyone stopped gaining excess weight today, within one generation the obesity problem could be significantly reduced as today's children would not become any more obese and the next generation of children would not gain excess weight at all. Given the extent and adverse health consequences of the expanding pandemic, it would seem the most effective ways to reduce the population prevalence of obesity is to pursue both prevention and treatment simultaneously. Finally, the small change approach could, in fact, be a means of achieving larger behavior changes. It may be possible, for example, to achieve more sustained increases in diet and physical activity by starting with helping people make small behavior changes and gradually adding more and more such changes increasing in cumulative impact. This strategy deserves additional evaluation.
What would it take to improve obesity treatment?
If it was true that, with the exception of bariatric surgery, current strategies are not sufficient to produce and sustain the changes in energy balance required to restore normal weight in the population, it would be important to ask what it would take to improve obesity treatment. Obesity has been described as a mismatch between human physiology and the environment in which we live (31). Better treatment of obesity may require modifying human physiology, modifying the environment in which we live, or both.
A better understanding of how obesity affects human physiology could lead to more effective ways to modify human physiology through pharmacological therapy. For example, animal models have identified several physiological and metabolic factors in the reduced-obese state that appear to predispose the animal toward weight regain (21,22). If such mechanisms also exist in humans, they could be either a cause or a consequence of obesity. Nonetheless, these provide potential targets for pharmacological interventions that might lessen the drive toward weight regain following weight loss. Current medications appear to add only modestly to weight loss produced by behavioral strategies (32). This suggests that there is yet to be an effective approach towards translating current knowledge of human physiology into strategies to permanently alter body weight.
Another way to increase the effectiveness of behavioral strategies is to modify the food and physical activity environments. Over the past decade, much has been written about how the environment in which we live encourages overeating and discourages physical activity (33,34). It may be possible to change the environment to one that encourages less overeating and more physical activity. While many ways of doing this have been suggested, we have not yet demonstrated any large scale success with this approach. Part of the problem may be that as a species, the construction of food and physical activity environments occurred to provide the things most desired such as easy accessibility to low cost, good tasting food and a life that does not require high levels of physical exertion (3,30,31,33,34). It does not seem surprising that people have found it difficult to drastically modify the food and physical activity environments in their communities as such changes may be fighting innate biological drives for eating and inactivity.
The small change approach can also be applied to environmental modification (30). In order to produce and maintain the amount of behavior change required to treat obesity, large environmental changes are likely needed as well. Small environmental changes may be more feasible and could have important effects over time. Further, these changes could potentially be produced without the need for conscious behavior change. For example, based on work of Barbara Rolls and colleagues (35), we suggested that a small change in the energy density of packaged foods (done by the food industry) could produce a reduction in energy intake in the population on the order of 50-100 kcal/day. Such a small change would likely be undetectable by consumers. Altering the energy density of packaged foods to produce sufficient decreases in energy intake to treat obesity would require a much larger change. It is likely that such large changes would be detectable, and possibly not acceptable, by consumers. A similar argument can be applied to portion sizes. It may be much more acceptable to reduce portion sizes gradually over time (and without conscious efforts by consumers) than all at once. Such a strategy could be very helpful for prevention of weight gain but may not be sufficient for obesity treatment.
Should we focus on changing food intake or physical activity?
Unfortunately, there is still some debate about whether modifying food intake or physical activity is more critical for addressing obesity. Swinburn et al. recently suggested that the obesity epidemic in the U.S population can be explained entirely by increases in food intake (14). This analysis fails to appreciate that much of the increase in food intake in the population may be subsequent to weight gain, which, in turn, may be subsequent to reductions in physical activity that have occurred over decades as our current modern lifestyle was evolving during the 20th century. Further, there are data to suggest that appetite regulation (matching energy intake to energy expenditure) is less precise under conditions of low physical activity (36). If true, the probability of excess energy consumption could be increased below some minimal level of physical activity, consistent with a greater risk of overweight and obesity in sedentary individuals. Low levels of physical activity are permissive and may in fact be necessary for food intake to drive obesity. Under conditions in which sedentary behavior is the norm, weight gain would appear to be driven entirely by food intake. Part of the reason that some suggest that declining levels of physical activity are not causal is because activity has not dropped dramatically (based on existing measurement capabilities) in the past few decades when obesity was expanding rapidly. Physical activity levels are already much lower than they were at the beginning of the 20th century and most people are engaged in much more sedentary occupations and lifestyles. It would seem implausible that physical activity could drop much further from current levels, making it appear that food intake is solely responsible for expanding waistlines. Finally, high levels of physical activity appear to be the strongest predictor of success in long-term weight loss maintenance (37,38). A focus on food intake or physical activity alone is not useful and fails to adequately appreciate the complex interplay between energy intake and energy expenditure both for controlling appetite and the temporal displacement between when physical activity levels declined as lifestyles changed and the later expansion in the availability of inexpensive, convenient food (3,30,31,33,34). Both food intake and physical activity patterns have changed over the past century in ways that promote obesity, and it will be necessary to alter both behaviors if we have a chance of reversing the pandemic.
Summary
The global obesity pandemic has arisen from small imbalances in energy intake and expenditure that have accumulated over time. For primary obesity prevention, the energy gap in the U.S. is less than 100 kcal/day for 90% of the population, meaning that relatively small changes in energy intake and expenditure adding up to 100 kcal/day could arrest excess weight gain in most people. Preventing further weight gain in the population could substantially reduce the prevalence of obesity within one generation. The energy gap is even smaller in other countries that have made similar analyses.
The energy gap for weight reduction and maintenance (i.e., obesity treatment) is much larger than 100 kcal/day owing to the increased energy demands of maintaining a larger body. Thus, the magnitude of behavioral changes required to restore the current population to normal weight is much larger than that required to prevent further weight gain. At this point in time, efforts to create and sustain such large changes in behavior, either at the individual or population level, have been unsuccessful.
Focusing solely on trying to address the large energy gap associated with obesity treatment seems unsatisfactory and unhelpful as it both overlooks the tangible progress that could be made against preventing primary weight gain and it seems tantamount to suggesting that attempts to deal with obesity should only be initiated once it is established. The notion that the obesity pandemic is exclusively due to increased food intake is also not helpful in finding a solution. While it is certainly easier to find a villain to blame for increased food intake (the food industry) than it is to assign ownership for sedentariness (e.g., progress, technology), it ignores the evidence that increased levels of physical activity are essential for effectively balancing energy intake and expenditure at a healthy weight.
In order to restore conditions under which human physiology evolved and developed mechanisms for balancing energy intake and expenditure, it will require both finding effective ways to assure a reasonable level of daily physical activity AND reducing energy intake. At this time, small changes in both intake and expenditure may be sufficient to prevent further population weight gain and support energy balance at a healthy weight. It will take a concerted effort by both public and private interests to accomplish even this goal. Restoring normal body weights among those already obese would likely require more dramatic intervention including pharmacological and surgical treatment. A small changes approach must be included in public health strategies and in public policies to address obesity.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
James O. Hill, Center for Human Nutrition, University of Colorado Denver, Campus Box C263, 4455 E. 12th Avenue, Denver, CO 80220, Phone: 303-315-9974; Fax: 303-315-9976; james.hill@ucdenver.edu.
John C. Peters, Personal Health Care, The Procter & Gamble Company, 8700 Mason Montgomery Rd, Mason, OH 45040, Phone: 513-698-7645; Fax: None; peters.jc.1@pg.com.
Holly R. Wyatt, Division of Endocrinology, Metabolism, and Diabetes, University of Colorado Denver, Campus Box C263, Center for Human Nutrition, 4455 E. 12th Avenue, Denver, CO 80220, Phone: 303-315-9004; Fax: 303-315-9976; holly.wyatt@ucdenver.edu.
References
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 2.International Obesity Task Force prevalence data. [7 July 2009]; International Association for the Study of Obesity: http://www.iotf.org/database/index.asp.
- 3.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–5. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 4.Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005;13:1431–41. doi: 10.1038/oby.2005.173. [DOI] [PubMed] [Google Scholar]
- 5.Zhai FY, Wang HJ, Wang ZH, Chen CM. Control the increasing of the prevalence of overweight and obesity by covering the energy gap of Chinese population. Wei Sheng Yan Jiu. 2006;35:72–6. in Chinese. [PubMed] [Google Scholar]
- 6.Tataranni PA, Harper IT, Snitker S, Del Parigi A, Vazarova B, Bunt J, Bogardus C, Ravussin E. Body weight gain in free-living Pima Indians: effect of energy intake vs expenditure. Int J Obes. 2003;27:1578–83. doi: 10.1038/sj.ijo.0802469. [DOI] [PubMed] [Google Scholar]
- 7.Ebrahimi-Mameghani M, Scott JA, Der G, Lean MEJ, Burns CM. Changes in weight and waist circumference over 9 years in a Scottish population. Eur J Clin Nutr. 2008;62(10):1208–14. doi: 10.1038/sj.ejcn.1602839. [DOI] [PubMed] [Google Scholar]
- 8.Berg C, Rosengren A, Aires N, Lappas G, Torén K, Thelle D, Lissner L. Trends in overweight and obesity from 1985 to 2002 in Göteborg, West Sweden. Int J Obes. 2005;29:916–24. doi: 10.1038/sj.ijo.0802964. [DOI] [PubMed] [Google Scholar]
- 9.Blumel JE, Castelo-Branco C, Rocangliolo ME, Bifas L, Tacla X, Mamani L. Changes in body mass index around menopause: a population study of Chilean woman. Menopause. 2001;8:239–44. doi: 10.1097/00042192-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics. 2006;118:e1721–33. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 11.Goran MI, Shewchuk R, Gower BA, Nagy TR, Carpenter WH, Johnson RK. Longitudinal changes in fatness in white children: no effect of childhood energy expenditure. Am J Clin Nutr. 1998;67:309–16. doi: 10.1093/ajcn/67.2.309. [DOI] [PubMed] [Google Scholar]
- 12.Plachta-Danielzik S, Landsberg B, Bosy-Westphal A, Johannsen M, Lange D, Muller MJ. Energy gain and energy gap in normal-weight children: longitudinal data of the KOPS. Obes. 2008;16:777–783. doi: 10.1038/oby.2008.5. [DOI] [PubMed] [Google Scholar]
- 13.Bouchard C. The magnitude of the energy imbalance in obesity is generally underestimated. Int J Obes. 2008;32:879–80. doi: 10.1038/sj.ijo.0803796. [DOI] [PubMed] [Google Scholar]
- 14.Swinburn BA, Sacks G, Lo SK, Westerterp Kr, Rush EC, Rosenbaum M, Luke A, Schoeller DA, DeLany JP, Butte NF, Ravussin E. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009;89:1723–1728. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. American Journal of Clinical Nutrition. 1995;62:19–29. doi: 10.1093/ajcn/62.1.19. [DOI] [PubMed] [Google Scholar]
- 16.Hill JO, Thompson H, Wyatt HR. Weight maintenance: What's missing? J Am Diet Assoc. 2008;105(5) 1:S63–66. doi: 10.1016/j.jada.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Mifflin MD, Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 18.Ravussin E, Lillioja S, Anderson TE, Christin L, Bogardus C. Determinants of 24-hour energy expenditure in man: Methods and Results Using a Respiratory Chamber. J Clin Invest. 1986;78:1568–78. doi: 10.1172/JCI112749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leibel RL, Rosenbaum M, Hirsch J. Changes in Energy Expenditure Resulting from Altered Body Weight. N Eng J Med. 1995;332:621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 20.Rosenbaum M, Vandenborne K, Goldsmith R, Simoneau JA, Heymsfield S, Joanisse DR, Hirsch J, Murphy E, Matthews D, Segal KR, Leibel RL. Effects of experimental weight perturbation on skeletal muscle work efficiency in human subjects. Am J Physiol. 2003;285:R183–R192. doi: 10.1152/ajpregu.00474.2002. [DOI] [PubMed] [Google Scholar]
- 21.MacLean PS, Higgins J, Johnson GC, Fleming-Elder BK, Peters JC, Hill JO. Metabolic adjustments with the development, treatment, and recurrence of obesity in obesity-prone rats. Am J Physiol. 2004;287:R288–R297. doi: 10.1152/ajpregu.00010.2004. [DOI] [PubMed] [Google Scholar]
- 22.MacLean P, Higgins J, Jackman M, Johnson G, Fleming-Elder B, Wyatt H, Melanson EL, Hill JO. Peripheral metabolic responses to prolonged weight reduction that promote rapid, efficient regain in obesity-prone rats. Am J Physiol. 2006;290:R1577–R1588. doi: 10.1152/ajpregu.00810.2005. [DOI] [PubMed] [Google Scholar]
- 23.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–84. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 24.Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med. 2005;142:56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 25.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Stave CD, Olkin I, Sirard JR. Using pedometers to increase physical activity and improve health. JAMA. 2007;298:2296–304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 26.Donahoo W, Wyatt HR, Kriehn J, Stuht J, Dong F, Hosokawa P, Grunwald GK, Johnson SL, Peters JC, Hill JO. Dietary fat increases energy intake across the range of typical consumption in the U.S. Obesity. 2008;16:64–69. doi: 10.1038/oby.2007.31. [DOI] [PubMed] [Google Scholar]
- 27.Stroebele N, de Castro J, Stuht J, Catenacci V, Wyatt HR, Hill JO. A small-changes approach reduces energy intake in free-living humans. J Am Coll Nutr. 2009;28:63–68. doi: 10.1080/07315724.2009.10719763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodearmel SJ, Wyatt HR, Barry M, Dong F, Pan D, Israel RG, Cho SS, McBurney MI, Hill JO. A family-based approach to preventing excessive weight gain. Obesity. 2006;14:1392–401. doi: 10.1038/oby.2006.158. [DOI] [PubMed] [Google Scholar]
- 29.Rodearmel SJ, Wyatt HR, Stroebele N, Smith SM, Ogden LG, Hill JO. Small changes in dietary sugar and physical activity as an approach to preventing excessive weight gain: the America On the Move family study. Pediatrics. 2007;120:e869–79. doi: 10.1542/peds.2006-2927. [DOI] [PubMed] [Google Scholar]
- 30.Hill JO. Can a small changes approach help address the obesity epidemic? A report of the Joint Taskforce of the America Society for Nutrition (ASN), Institute of Food Technologists (IFT), and the International Food Information Council (IFIC) Am J Clin Nutr. 2009;89:1–8. doi: 10.3945/ajcn.2008.26566. [DOI] [PubMed] [Google Scholar]
- 31.Peters JC, Wyatt HR, Donahoo WT, Hill JO. From instinct to intellect: the challenge of maintaining healthy weight in the modern world. Obes Rev. 2002;3:69–74. doi: 10.1046/j.1467-789x.2002.00059.x. [DOI] [PubMed] [Google Scholar]
- 32.Bessesen DH. Update on obesity. J Clin Endocrin Metab. 2008;93:2027–2034. doi: 10.1210/jc.2008-0520. [DOI] [PubMed] [Google Scholar]
- 33.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–4. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 34.Wadden TA, Brownell KD, Foster GD. Obesity. Responding to the global epidemic. J Consult Clin Psych. 2002;70:510–525. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- 35.Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc. 2005;105:S98–103. doi: 10.1016/j.jada.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 36.Blundell JE, King NA. Physical activity and regulation of food intake: current evidence. Med Sci Sports Ex. 1999;31:S573–583. doi: 10.1097/00005768-199911001-00015. [DOI] [PubMed] [Google Scholar]
- 37.Wing RR, Hill JO. Successful weight loss maintenance. Ann Rev Nutr. 2001;21:323–341. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 38.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med. 2008;168:1550–1559. doi: 10.1001/archinte.168.14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]