Article-at-a-Glance
Background
Hospitalized smokers are a large and important but undertreated population. Although effective strategies have been developed to enhance smoking cessation, many hospitalized smokers still fail to benefit from these services. A study was conducted to examine the reach of services within a hospital tobacco treatment program and to identify predictors of referral and treatment.
Methods
Electronic medical records were downloaded for all 3,600 smokers admitted to a 475-bed academic medical center hospital in a one-year period.
Results
More than one in four of identified smokers were referred to the specialty service and nearly one in five received treatment. Logistic regression models found that Joint Commission core measure status (heart failure, myocardial infarction, and pneumonia) was the strongest predictor of referral, followed by a history of smoking for more than 10 years. Conversely, smokers admitted for emergency medical services were less likely to be referred compared with those admitted electively. Patients treated on surgical, obstetric, and psychiatric services were less likely to be referred for tobacco treatment than those treated on medical services. Of those referred, smokers with longer lengths of stay and those admitted through the emergency department were more likely to actually receive services.
Discussion
To capitalize on hospitalization as a “teachable moment,” other subpopulations, such as psychiatric and obstetric patients, deserve attention. Tobacco treatment services must be fully integrated into hospital systems, configured to deliver care to all smokers, and reimbursed to ensure sustainability. This study’s identification of underserved groups, determination of potential roadblocks to delivery of services, and suggestion of ways to disseminate treatment equitably to all smokers should prove helpful to policymakers.
Hospitalization is an ideal time to encourage smokers to quit. During hospitalization, smokers are not allowed to smoke, are in contact with many health professionals, and may be more willing to accept assistance in quitting.1 Many smokers quit, unaided, following hospitalization.2 A meta-analysis also found that those who receive intensive treatment during hospitalization and outpatient follow-up treatment for at least one month are more likely to quit than smokers receiving no treatment.1,3
Yet, most hospitals do not systematically address tobacco. Where treatment is provided, it is not evidence-based. A pooled analysis of 33 hospital studies found that smoking status was assessed in 60% of patients, 42% of identified smokers were advised to quit, 14% were given or advised to use nicotine replacement, and 12% received referrals or follow-up.4 A study found that adding a tobacco treatment order set to an existing computerized order entry system increased identification, referral, and treatment of smokers, but referral and treatment rates remained low (2.1% and 2.5%, respectively).5 Even patients with tobacco-related illnesses fail to receive tobacco treatment. A test of quality care measures conducted among 83 hospitals in nine states found that only 65% of smokers with acute myocardial infarction (AMI), 39% of smokers with congestive heart failure (CHF), and 35% of smokers with community-acquired pneumonia (CAP) had received any form of counseling for smoking cessation during hospitalization.6 Accordingly, in 2004 The Joint Commission made smoking cessation advice and treatment a core quality measure for treating patients with these three diagnoses.7 Moreover, hospitals fail to treat important subpopulations. Data on patients with AMI from 400 hospitals suggest that blacks are less likely than whites to receive smoking cessation counseling.8 Psychiatric inpatients, who have a high prevalence of smoking, rarely receive tobacco treatment.9
Although formal surveys have not been done, anecdotal evidence from hospital associations, electronic mailing lists, and tobacco treatment specialist groups suggests that many hospitals are beginning to implement systematic treatment for patients who smoke. This treatment often takes the form of specialized services offered through respiratory therapy or other hospital departments. These services are likely a response to the Joint Commission mandate to treat patients for whom core measures have been released and are sometimes initiated after poor performance on the smoking cessation measures.10 There is also an emerging trend to designate entire hospital campuses smoke-free.11 A recent study indicated that by February 2008, 45% of hospitals in the United States had adopted a smoke-free campus policy, with another 15% reporting actively pursuing the adoption of such a policy.12
Instituting tobacco treatment services is often a part of this policy change.1 Elements of these evidence-based specialty services include the following:
Developing a team of trained tobacco treatment specialists
Implementing hospital systems for identifying smokers and referring them to the service
Providing inpatient treatment based on current treatment guidelines
Providing or facilitating follow-up treatment after discharge, often via fax referral to tobacco quit lines13
The promise of such services is that they will extend the reach and quality of tobacco treatment by having designated staff deliver care. Unfortunately, health care innovations may create greater service and health status disparities by failing to reach traditionally underserved populations. In this article, we describe a study in which we examined how well a specialty service in a large academic medical center reaches smokers and identified whether subpopulations remain underserved. To that end, we profiled all smokers who were admitted during a one-year period. We determined rates of referral to the service and rates of treatment by the service. We also identified factors that predict referral to the service, as well as factors that predict actual receipt of services. Although our findings are, to some extent, a product of our particular hospital’s culture and systems, we provide a model for monitoring delivery of services, and we believe that we uncovered important clues for other hospitals seeking to provide optimal services.
Methods
Setting
The University of Kansas Hospital (Kansas City, Kansas) is a 475-bed tertiary care hospital located in a large metropolitan area that admits more than 20,000 patients per year.
Sidebar 1. UKanQuit
Treatment by UKanQuit ideally occurs within 12 to 24 hours of admission. In practice, there are often delays between when patients arrive at the medical center (often through the emergency department), when they are admitted to a unit, and when the electronic admission forms are completed. Many patients are discharged in less than a day. Hence, hospital systems issues, patient characteristics, and patient preferences all figure into whether patients are referred to and whether patients receive treatment by UKanQuit.
UKanQuit staff consist of Ph.D.–and master-level counselors with specialized training in treating tobacco dependence. The staff provide treatment from 9:00 A.M. to 5:00 P.M. on weekdays. UKanQuit staff retrieve patient names from the electronic medical record and visit patients at their bedside. Counseling sessions typically last 15 to 30 minutes and include the following components:
Assessing withdrawal
Working with nurses and physicians to adjust nicotine replacement to keep the patient comfortable while in the hospital
Assessing patients’ interest in quitting smoking
Providing a brief motivational intervention to patients not interested in quitting
Providing assistance in quitting (developing a quit plan, arranging for medications on discharge) to patients interested in quitting
UKanQuit services provide Spanish-language counseling to Spanish speakers and utilize translators to counsel patients who speak other languages. Staff provide follow-up treatment after discharge by either directly providing counseling or through fax referral to the state tobacco quit-line. Staff also contact patients six months following inpatient treatment to assess outcomes and provide additional support and referral. To launch the service, program leadership [K.P.R., E.F.E.] gave brief (10–15-minute) presentations at nursing, medical, and ancillary provider staff meetings.
Referral to and Treatment in UKanQUit
The hospital’s specialty tobacco treatment service (UKanQuit), as described in Sidebar 1 (above), was implemented when the hospital campus went smoke-free on September 1, 2006. The current study, which was conducted to evaluate the UKanQuit program, was approved by the medical center’s Institutional Review Board.
Referral to UKanQuit is made via a required field in the hospital electronic medical record (EMR). As nurses record information from patients admitted to their units, the EMR requires them to identify the smoking status of all patients and to ask all smokers if they would like to talk to a tobacco treatment specialist during their hospital stay. The patients who respond “yes” are placed on an electronic list within the EMR. Nurses may complete items on behalf of patients who are sedated or in distress. Through the automated system, a consult e-mail is sent to the UKanQuit staff. UKanQuit staff then enter the patient’s name, unit, and room number into the UKanQuit database as a permanent record of referral. Ninety-seven percent (826) of the 853 patients in this study were referred through this method. The remaining 3% (27) were directly referred by physicians and other health care providers.
Patients
From November 2007 through January 2008, we reviewed EMRs and tobacco treatment data on patients admitted to the hospital between September 1, 2006, and August 31, 2007. Smoking status was recorded for 16,391 (76.8%) of the 21,356 patients admitted to the hospital. All smokers 12–89 years of age were included in this study. Patients were identified as smokers if they responded “yes” to two required fields in the EMR: “Have you smoked in the past year?” and “Have you smoked in the last 30 days?” Only patients who answered “yes” to both of these questions were included in these analyses.
Data Sources
Data were derived from the EMR and the UKanQuit treatment record. The EMR includes extensive information on all patients’ demographics, health status, treatment, and discharge disposition. Relevant data were downloaded from the EMR by the hospital’s department of organizational improvement, merged with the UKanQuit treatment record, and imported into SAS (SAS Institute, Inc., Cary, North Carolina) for analysis. Frequency and logic checks were conducted to identify outlying data and ensure that data on individual patients were appropriately matched. For patients who were admitted to the hospital more than once during the year, only data from the first admission in the year were included in analyses.
Measures
Main Outcome Measures
The main outcome measures were referral to UKanQuit, and among referred patients, receipt of treatment by UKanQuit. Patients were classified as not treated if they were identified as nonsmokers by the UKanQuit counselor, were discharged before an attempt to visit them, or for other reasons were not able to be seen.
Demographic Measures
The demographic measures were downloaded from the EMR and included age, gender, ethnicity, marital status, language, and insurance coverage. We collapsed language data into 3 major categories: English, Spanish, and other. We re-classified insurance coverage into Medicaid, Medicare, commercial, uninsured, and other. Dually eligible Medicare beneficiaries were classified as Medicare.
Smoking Behavior Measures
Also from the EMR we downloaded tobacco use data (number of years smoked, number of cigarette packs per day, and whether the patient lived with another smoker).
Diagnosis and Treatment Measures
We used the patient’s primary discharge diagnosis to determine whether or not they were subject to the Joint Commission core measures for AMI, CHF, and CAP. The hospital services that patients were admitted into were grouped into five categories—medical, surgical, obstetrics, psychiatric, and other. Patients were classified “yes” or “no” if admitted through the emergency department (ED) or not, respectively.
Data Analysis
We analyzed data using the SAS statistical package, version 9.1. We summarized the data using descriptive statistics and then identified predictors of referral and treatment using logistic regression. Categorical variables were summarized using frequencies and percentages, and continuous variables with means and standard deviations (if distributions were close to normal) or with medians and ranges (if distributions were skewed). In regression analyses, we first explored the effect of each individual factor on each outcome variable by simple logistic regression. Factors with p value < .25 were entered into multiple logistic regression models, which were built by full stepwise procedure. The final parsimonious models, whose goodness of fit was examined by the Hosmer and Lemeshow test, included factors significant at the .05 level.
Results
Hospital Smokers
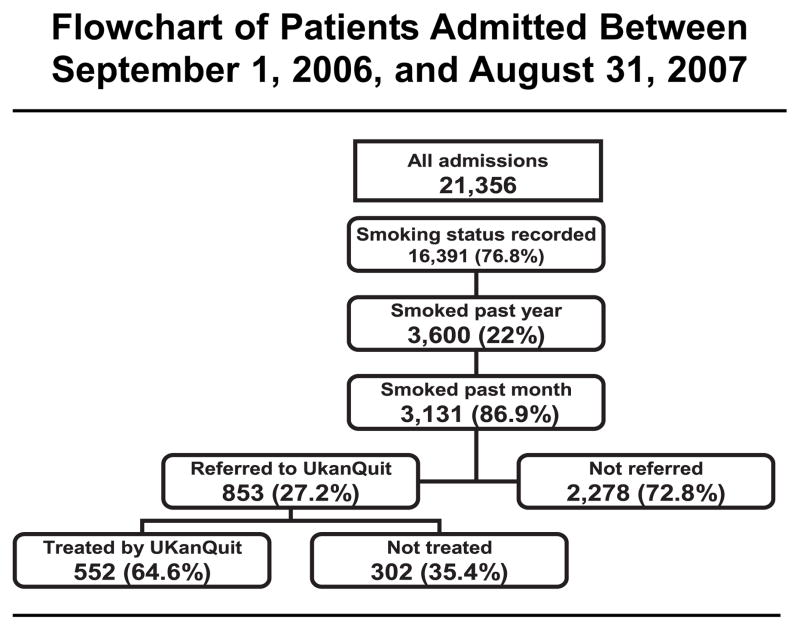
Of the 16,391 patients whose smoking status was recorded in the EMR during the study period, 3,600 (21.9%) smoked within the past year. Of these, 3,131 (87%) smoked within the past 30 days (current smokers) and were included in these analyses. Among current smokers, 853 (27%) were referred to UKanQuit. Among smokers referred to UKanQuit, 65% were treated by the service, resulting in 18% of all identified smokers receiving treatment by the service (Figure 1, page 554). Of the 301 who were not treated, 85 had specific reasons listed for not receiving treatment. One patient was discharged before an attempt by a UKanQuit counselor to see him or her, and 84 were categorized as “others,” which could include “patient was asleep,” “doctor in the room,” “out of bed for procedure,” and “unable to speak.” Patients who for these reasons were not suitable for treatment were classified as “not treated.” None of these patients refused to talk with a UKanQuit counselor.
Figure 1.
The flowchart for patients admitted to the University of Kansas Hospital within the one-year period is shown.
Appendix 1 (available in online article) displays the characteristics of all current smokers and those referred to UKanQuit. Current smokers were predominantly white and spoke English. Slightly more than half of smokers were men, and the mean age was 45 years. Most of the smokers had smoked more than 10 years, and one in five smoked more than one pack of cigarettes per day. Fewer than half lived with a significant other who smoked. More than half (53%) were admitted through the ED, with the majority admitted into the medical and surgical services. The median length of stay was three days. Taken together, 6% had diagnoses of AMI, CHF, or pneumonia.
Appendix 1.
Relationship Between Patient Characteristics and Referral to the UKanQuit Quit Smoking Service*
| Identified Smokers (n = 3,131) | Referred (n = 853) | Not Referred (n = 2278) | Crude OR (95% CI) | |
|---|---|---|---|---|
| Age mean (SD) | 45.5 (15.7) | 48.9 (13.7) | 44.2 (16.1) | |
| ≤33 (ref) | 806 (25.7) | 131 (15.4) | 675 (29.6) | 1.00 |
| 34–47 | 840 (26.8) | 240 (28.1) | 600 (26.3) | 2.06 (1.62,2.62) |
| 48–57 | 779 (24.9) | 252 (29.5) | 527(23.1) | 2.46 (1.94,3.13) |
| 58–89 | 706 (22.6) | 230 (24.0) | 476 (20.9) | 2.49 (1.95,3.18) |
| Sex n (%) | ||||
| Female (ref) | 1355 (43.5) | 383 (28.3) | 972(42.7) | 1.00 |
| Male | 1763 (56.5) | 458 (26.0) | 1305 (57.3) | 0.89 (0.76,1.04) |
| Ethnicity n (%) | ||||
| White (ref) | 2234 (71.4) | 628 (73.6) | 1606 (70.5) | 1.00 |
| Black | 561 (17.9) | 149 (17.5) | 412 (18.1) | 0.93 (0.75, 1.14) |
| Hispanic | 132 (4.2) | 20 (2.3) | 112(4.9) | 0.46 (0.28, 0.74) |
| Other | 203 (6.5) | 56 (6.6) | 147 (6.5) | 0.97 (0.71,1.34) |
| Language n (%) | ||||
| English Speaking (ref) | 2907 (97.1) | 814 (98.4) | 2093 (96.6) | 1.00 |
| Non English Speaking* | 87 (2.9) | 13 (1.6) | 74 (3.4) | 0.45 (0.25, 0.82) |
| Insurance coverage n (%) | ||||
| Commercial (ref) | 982 (31.4) | 267 (31.3) | 715 (31.4) | 1.00 |
| Medicaid | 671 (21.4) | 188 (22.0) | 483 (21.2) | 1.04 (0.84,1.30) |
| Medicare | 737 (23.5) | 228 (26.7) | 509 (22.3) | 1.20 (0.97, 1.48) |
| Uninsured | 422 (13.5) | 97 (11.4) | 325 (14.3) | 0.80 (0.61,1.04) |
| Other | 319(10.2) | 73 (8.6) | 246 (10.8) | 0.79 (0.59, 1.07) |
| Years smoked n (%) | ||||
| ≤ 10 years (ref) | 933 (30.2) | 151 (17.8) | 782 (34.8) | 1.00 |
| >10 years | 2162 (69.9) | 696 (82.2) | 1466 (65.2) | 2.46 (2.02, 3,0) |
| Cigarettes packs per day n (%) | ||||
| ≤ 1 pack/day (ref) | 2488 (80.3) | 647 (76.3) | 1841 (81.8) | 1.00 |
| > 1 pack /day | 611 (19.7) | 201 (23.7) | 410 (18.2) | 1.40 (1.15.1.69) |
| Living with other smoker n (%) | ||||
| No (ref) | 1932 (62.6) | 519 (61.4) | 1413 (63.0) | 1.00 |
| Yes | 1156(37.4) | 327 (38.6) | 829 (37.0) | 1.07 (0.91,1.26) |
| Admission service n (%) | ||||
| Medical (ref) | 1407 (45.0) | 536 (62.8) | 871 (38.2) | 1.00 |
| Surgical | 1242 (39.7) | 243 (28.5) | 999 (43.9) | 0.39 (0.33,0.47) |
| Obstetrics | 176 (5.6) | 31 (3.6) | 145 (6.4) | 0.35 (0.23,0.52) |
| Psychiatry | 302 (9.7) | 42 (4.9) | 260 (11.4) | 0.26 (0.19,0.37) |
| Other** | 4 (0.1) | 1 (0.1) | 3 (0.1) | |
| Admission through emergency | ||||
| No (ref) | 1394 (47.2) | 403 (51.5) | 991 (45.7) | 1.00 |
| Yes | 1559 (52.8) | 380 (48.5) | 1179 (54.3) | 0.79 (0.67,0.93) |
| Length of stay (days) | ||||
| Median (range) | 3.0 (148) | 3.0 (39) | 3.0 (148) | |
| < 3 days (ref) | 1160 (37.0) | 283 (33.2) | 877 (38.5) | 1.00 |
| ≥ 3 days | 1971 (63.0) | 570 (66.8) | 1401 (61.5) | 1.26 (1.07,1.49) |
| Diagnosis n (%) | ||||
| All other diagnosis (ref) | 2940 (94.0) | 745 (87.4) | 2195 (96.4) | 1.00 |
| Joint Commission core measure diagnosis | 189 (6.0) | 107 (12.6) | 82 (3.6) | 3.85 (2.85,5.19) |
Subsamples were slightly different from total n = 3131 due to missing data. For sex, n = 3118; for ethnicity, n = 3130; for language, n =2994; for years smoked, n = 3095; for cigarettes per day, n = 3099; for living with other smokers, n = 3088; for admission through emergency = 2953. Missing values were not included in calculation
87 non-English speaking = 89% non-English speaking spoke Spanish (n=79), 1 Hindi, 2 Laotian, and 5 spoke other language not specified
excluded from bivariate analysis
Referral to UKanQUit
Bivariate relationships
Factors associated with referral are shown in Appendix 1. Hispanics were less likely to be referred, as were non-English-speaking patients, than whites. Patients who smoked for more than 10 years, who smoked more than one pack of cigarettes per day, and who were in the hospital for ≥ 3 days were more likely to be referred. Compared with medical services, patients admitted to surgical, obstetrics, and psychiatry services were less likely to be referred. Similarly, patients admitted through the ED were less likely to be referred than elective admissions. Patients admitted with Joint Commission core measure diagnoses were almost three times more likely to be referred than patients without these diagnoses: 61% of patients with AMI, 49% with CHF, and 56% with CAP received a referral (data not shown).
Multivariate Relationships
In the final multivariate model (Table 1, page 555), significant predictors of referral included length of smoking history, admission service unit, and whether the admitting diagnosis was a core measure diagnosis.
Table 1.
Predictors of Referral to the UKanQuit Quit Smoking Service in the Final Logistic Regression Model*
| Adjusted OR (95% CI) | P Value | |
|---|---|---|
| Diagnosis, Joint Commission core measure diagnosis | 2.34 (1.69, 3.25) | < .0001 |
| Years smoked > 10 years | 2.10 (1.69, 2.61) | < .0001 |
| Admission through emergency | 0.79 (0.66, 0.95) | 0.01 |
| Admission service Surgical | 0.46 (0.38, 0.56) | < .0001 |
| Obstetrics | 0.60 (0.39, 0.92) | |
| Psychiatry | 0.35 (0.25, 0.50) |
OR, odds ratio; CI, confidence interval.
Treatment by UKanQuit
Bivariate Relationships
Appendix 2 (available in online article) displays the unadjusted odds of being treated by UKanQuit for subpopulations of smokers, compared to all smokers referred to UKanQuit. Patients admitted to the surgical service were less likely to be treated than patients admitted to the medical service. Conversely, patients in the hospital for ≥ 3 days were more likely to be treated compared to patients staying < 3 days. The proportions of referred smokers with AMI, CHF, and CAP who were treated by UKanQuit were 39%, 41%, and 44% respectively (data not shown).
Appendix 2.
Relationship Between Patient Characteristics and Treatment by the UKanQuit Quit Smoking Service*
| Referred (n = 853) | Treated (n = 552) | Not Treated (n = 301) | Crude OR (95% CI) | |
|---|---|---|---|---|
| Age mean (SD) | 48.9 (13.7) | 48.5 (13.6) | 49.5 (13.9) | |
| ≤ 33 (ref) | 131 (15.4) | 87 (15.8) | 44 (14.6) | 1.00 |
| 34–47 | 240 (28.1) | 164 (29.7) | 76 (25.3) | 1.09 (0.69,1.72) |
| 48–57 | 252 (29.5) | 155 (28.1) | 97 (32.2) | 0.81 (0.52,1.26) |
| 58–89 | 230 (27.0) | 146 (26.5) | 84 (27.9) | 0.88 (0.56,1.38) |
| Sex n(%) | ||||
| Female (ref) | 383 (45.5) | 238 (43.3) | 145 (49.8) | 1.00 |
| Male | 458 (55.5) | 312 (56.7) | 146 (50.2) | 1.30 (0.98,1.73) |
| Ethnicity n (%) | ||||
| White (ref) | 628 (73.6) | 395 (71.6) | 233 (77.4) | 1.00 |
| Black | 149 (17.5) | 103 (18.7) | 46 (15.3) | 1.32 (0.90,1.94) |
| Hispanic | 20 (2.3) | 14 (2.5) | 6 (2.0) | 1.38 (0.52,3.63) |
| Other | 50 (6.6) | 40 (7.3) | 16 (5.3) | 1.48 (0.81,2.69) |
| Insurance coverage n (%) | ||||
| Commercial (ref) | 267 (31.3) | 164 (29.7) | 103 (34.2) | 1.00 |
| Medicaid | 188 (22.0) | 123 (22.3) | 65 (21.6) | 1.19 (0.81,1.75) |
| Medicare | 228 (26.7) | 153 (27.7) | 75 (24.9) | 1.28 (0.89,1.86) |
| Uninsured | 97 (11.3) | 66 (12.0) | 31 (10.3) | 1.34 (0.82,2.19) |
| Other | 73 (8.6) | 46 (8.3) | 27 (9.0) | 1.07 (0.63,1.83) |
| Years smoked n (%) | ||||
| ≤ 10 years (ref) | 151 (17.8) | 103 (18.7) | 48 (16.2) | 1.00 |
| >10 years | 696 (82.2) | 448 (81.3) | 248 (83.8) | 0.84 (0.58,1.23) |
| Cigarettes packs per day n (%) | ||||
| ≤ 1 pack/day (ref) | 647 (76.3) | 417 (75.7) | 230 (77.4) | 1.00 |
| > 1 pack /day | 201 (23.7) | 134 (24.3) | 67 (22.6) | 1.10 (0.79,1.54) |
| Living with other smoker n (%) | ||||
| No (ref) | 519 (61.4) | 349 (63.3) | 170 (57.6) | 1.00 |
| Yes | 327 (38.7) | 202 (36.7) | 125 (42.4) | 0.79 (0.59,1.05) |
| Admission service n (%) | ||||
| Medical (ref) | 536 (62.9) | 363 (65.8) | 173 (57.5) | 1.00 |
| Surgical | 243 (28.5) | 143 (25.9) | 100 (33.2) | 0.68 (0.50,0.93) |
| Obstetrics | 31 (3.6) | 19 (3.4) | 12 (4.0) | 0.76 (0.36,1.59) |
| Psychiatry | 42 (4.9) | 27 (4.9) | 15 (5.0) | 0.86 (0.45,1.65) |
| Other | 1 (0.1) | 0 (0) | 1 (0.3) | |
| Admission through emergency | ||||
| No (ref) | 403 (51.5) | 248 (48.9) | 155 (56.2) | 1.00 |
| Yes | 380 (48.5) | 259 (51.1) | 121 (43.8) | 1.34 (1.00,1.80) |
| Length of stay (days) | ||||
| Median (range) | 3.0 (39) | 4.0 (39) | 3.0 (38) | |
| <3 days (ref) | 283 (33.2) | 156 (28.3) | 127 (42.2) | 1.00 |
| ≥ 3days | 570 (66.8) | 396 (71.7) | 174 (57.8) | 1.85 (1.38,2.49) |
| Diagnosis n (%) | ||||
| Other diagnosis (ref) | 745 (87.4) | 483 (87.7) | 262 (87.0) | 1.00 |
| Joint Commission core measure diagnosis | 107 (12.6) | 68 (12.3) | 39 (13.0) | 0.95 (0.62,1.44) |
Subsamples were slightly different from total n=853 due to missing data.. For sex, n = 841; for years smoked, n = 847; for cigarettes per day, n= 848; for living with other smokers, n = 846; for admission through emergency = 783
Missing values were not included in calculation
Multivariable Relationships
Only length of stay and admission through the ED remained as statistically significant predictors of treatment in the parsimonious model (Table 2, page 555). Patients who were in the hospital for ≥ 3 days were more likely to be treated compared with patients admitted for < 3days. Although patients admitted through the ED were less likely to be referred, they were more likely to receive treatment than patients admitted through other departments even after controlling for length of stay.
Table 2.
Predictors of Treatment by the UKanQuit Quit Smoking Service in the Final Logistic Regression Model*
| Adjusted OR (95% CI) | P Value | |
|---|---|---|
| Admission through emergency | 1.41 (1.03, 1.92) | 0.03 |
| Length of stay ≥ 3 days | 1.88 (1.37, 2.59) | .0001 |
OR, odds ratio; CI, confidence interval.
Discussion
The fact that the hospital smoking rates of 21.9% was somewhat higher than the Kansas smoking prevalence of 17.8%14 for a similar period is not surprising, given the adverse health effects of smoking. Overall health of nonsmokers is generally better than that of smokers, and smokers are more likely to be hospitalized than nonsmokers.15,16
We found that more than one in four identified current smokers admitted to the hospital were referred to our specialty service. Nearly one in five identified current smokers admitted to the hospital were treated by UKanQuit. If we assume the same smoking prevalence among the nearly 5,000 patients who had undocumented smoking status on admission, 25% of all smokers were referred, and approximately 14% were treated. Smokers with Joint Commission core measure diagnoses and those who had smoked for more than 10 years were much more likely to be referred than smokers with a shorter smoking history or without these diagnoses. Smokers admitted through the ED and those treated by surgical, obstetric, and psychiatric services were less likely to be referred for tobacco treatment compared with smokers admitted directly to the hospital or those treated by the medical service.
Smokers staying in the hospital for ≥ 3 days were more likely to receive treatment compared with patients discharged sooner. Contrary to referral, emergent patients were more likely to be treated than patients on elective admissions even after controlling for length of stay and other treatment factors.
The fact that psychiatric patients were less likely to be referred for smoking cessation treatment, consistent with Prochaska and colleagues’ findings,9 is problematic, given the high prevalence of smoking in this population.17 Future studies should examine the extent to which this is explained by patient characteristics, such as acute psychiatric co-morbidity versus unfavorable attitudes of health care providers toward treating tobacco dependence among people with mental illness.18–20 In addition, medical patients may be more likely than psychiatric patients to be admitted for a tobacco-related illness. Contrary to another study,8 which involved a nationally representative sample of cardiac patients from community, academic, and veteran administration hospitals, we did not find significant differences between rates of referral or treatment for black and white smokers. Our patients were admitted for a wide variety of conditions, whereas the other study was conducted among cardiac patients alone.
We are not sure why ED patients are more likely to be treated once they are referred to UKanQuit. The relatively low rate of referral for patients admitted through the ED makes sense if we can assume that many of these patients were too sick to benefit from tobacco treatment. Our multivariate analysis controlled for length of stay, as well as a host of other variables that could account for increased treatment rates among ED patients. The measures that we have instituted to increase our treatment rates should help reduce treatment disparities between emergent and nonemergent cases.
Finally, we found that having a Joint Commission core measure diagnosis increased the odds that patients would be referred to tobacco treatment, although referral rates for such patients were similar to previously reported rates of tobacco counseling for such patients.6,21 Yet, it is not clear what type of treatment or documentation met criteria for “tobacco cessation advice or counseling” in the previous study. In any case, our findings cannot be extrapolated to programs that do not follow evidence-based smoking cessation guidelines. There is a need to extend Joint Commission core measurements beyond simple quantitative reporting of smoking cessation to include qualitative or structural measures that assess the type of intervention that patients are actually receiving.
We achieved much higher hospitalwide referral rates than a study that examined the impact of instituting a computerized order set on referral and treatment of smokers.5 Koplan and colleagues found that hospitalwide tobacco treatment referral rates doubled from 0.8% to 2.1% and that nicotine replacement utilization increased from 1.6% to 2.5%.5 Koplan et al.’s study differed from ours in that they targeted only one service (the medical service) for intervention; among patients treated by that service however, the Joint Commission composite smoking measure that summarized all three measured diagnoses (AMI, CHF, and CAP) increased from 86% to 95%. Our study involved all admissions, because the nursing electronic admission procedures were the same across the entire hospital.
This is one of the first studies to examine predictors of referral to and treatment by an intensive hospital service, and the results describe the reach of a new type of tobacco treatment that is increasingly being provided in hospitals. Our program is tightly integrated into the hospital EMR and treatment systems, and our findings are already being used to create systems changes and referral campaigns to increase utilization. To improve referral rates to UKanQuit, in December 2008 we mounted a station at a required hospital nursing “capacity fair” at which we surveyed nurses on how to better solicit referrals and informed them of our services and how to request UKanQuit for patients. We have worked with the hospital EMR development team to revise our order sets to automatically order a UKanQuit consult whenever the form is used to order nicotine replacement for a patient. We have conducted similar manager/unitwide trainings in the ED and are incorporating orders for pharmacotherapy and UKanQuit counseling into their transitional care order sets for patients who are transferred to an observation unit before admission to the hospital. To improve referrals from the psychiatric unit, we have conducted an hour-long training with medical residents and have instituted biweekly groups with patients to provide information about smoking cessation and to enhance motivation to quit. To improve treatment rates, UKanQuit has expanded the number of hours per day that counselors are required to spend in the hospital and has set aside morning hours for seeing patients in for brief procedures to ensure that we reach them before discharge.
Study Limitations
Our study has several limitations. It was conducted in one hospital and may not be representative of what might happen in other hospitals. Further, it relies on patient self-report of smoking status and may exclude patients who were unable or unwilling to divulge their smoking status to the admitting nurse. In addition, hospital records failed to document smoking status in 23% of patients. This was a surprising finding. Although smoking status was a required field, nurses were able to skip this item when they were unable to assess the smoking status of the patients at the time of admission, for example, if the patient was unconscious or mentally unstable. This is an important issue, given that the Joint Commission requires identification of all smokers and provision of in-patient smoking cessation advice as part of hospital core measurement.7 Configuring the EMR system in such a way that further data entry would not be permitted without completing the smoking status section could eliminate this issue. However, this could impede treatment of seriously ill patients who cannot respond to this question. Nevertheless, patients with undocumented smoking status may differ systematically from those with documentation in ways that could affect our findings. Future studies should examine the extent to which this occurs in hospitals, identify differences between patients who have documented versus undocumented smoking status, and identify ways to increase documentation of smoking status in hospital practice. System changes are needed to ensure that smoking status not captured during initial admission is collected at another time during the patients’ hospital stay.
The results of the multivariate analysis should be interpreted with caution because the strength of association was presented as odds ratios. The reader should be mindful of the fact that odds ratio is an overestimation of risk ratio when the prevalence of a condition (in our study, referral and treatment) is not a rare event.
Implications
The findings have a number of implications for improving the reach and quality of referral and treatment. It is possible to configure EMRs to automatically refer all smokers to tobacco treatment services. In the case of our hospital, this would provide the opportunity to treat more than 3,000 smokers per year. This systems change would be consistent with many hospital services that are ordered for patients without asking their permission, including respiratory therapy, social work, and physical therapy. It raises the question of how to pay for these services. At present, our program, like many other programs, is paid for by general hospital funds and falls under the Diagnosis-Related Group (DRG)–based reimbursement for the care of patients’ major diagnoses. Nurses are prompted to offer nicotine replacement to smokers (after consultation with physicians) on discharge but provide minimal behavioral intervention. In some hospitals, tobacco treatment services have provided intensive training to nurses to increase their ability to provide effective brief intervention, have instituted standing orders for pharmacotherapy, and receive referral for the subset of patients who report they are ready to quit. Such a system is designed to deliver brief intervention to all patients and intensive intervention to those ready to quit. Some hospitals employ advanced-practice nurses to deliver intensive intervention, which is eligible for payment outside DRG–related reimbursement. However, most smokers (80%) report they are not ready to quit smoking.22 To increase their readiness to quit, the least motivated patients may require the most skilled behavioral and pharmacological intervention. Identifying the optimal mix of strategies to motivate and assist hospitalized smokers to quit is an important area for future research.
Patients with a shorter smoking history, who can gain much by quitting early, should be a target for increased referral and treatment. Likewise, surgical, obstetrical, and psychiatric services should be encouraged to opt into tobacco treatment. It will be important to identify ways to enhance treatment for ED patients, many of whom are never even admitted to the hospital or who are in the ED for many hours before being admitted and referred to treatment. Finally, the patient attrition between referral and treatment is strongly linked to duration of stay. This can be addressed by expanding the hours during which tobacco treatment is provided.
Conclusion
This study provides important information to policymakers by identifying underserved groups, determining roadblocks to delivery of services, and suggesting ways for disseminating treatment equitably to all smokers. To ensure sustainability, tobacco treatment services must be fully integrated into hospital systems, configured to deliver care to all smokers, and reimbursed. Additional studies in other hospital settings are needed to develop systems models for increasing the reach of hospital tobacco treatment services.
Acknowledgments
The authors gratefully acknowledge the contributions of the following in the planning and development of this manuscript: Margaret Turner (Senior Coordinator, UkanQuit), Genevieve Casey (UkanQuit Counselor), Theresa Jackson (Director of Medical Records), Gail Sahlfeld (Decision Support Manager, Organizational improvement), Chip Hulen (Decision Support Systems Specialist, Organizational Improvement), Grace Legaspi (Quality Outcomes Coordinator, Organizational Improvement), Brad House (Clinical Analyst, Advanced Clinical Information System), Kathy Wright (SMS Application Analyst), Christopher Ruder (Vice President, Patient Care Services), Karen Wray (Director, Acute Care Services), Lila Martin (Director, Perioperative Service) and Danford Wilson (Consultant for Graduate Medical Education). This work was performed at the University of Kansas Medical School, Kansas City, Kansas, with support from the National Cancer Institute (R01 CA091912). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Babalola Faseru, Research Assistant Professor, Department of Preventive Medicine and Public Health, University of Kansas Medical Center and School of Medicine, Kansas City, Kansas
Hung-Wen Yeh, Assistant Professor, Department of Biostatistics, University of Kansas School of Medicine
Edward F. Ellerbeck, Sosland Professor and Chair of the Department of Preventive Medicine and Public Health, University of Kansas Medical Center and School of Medicine and Medical Director, UKanQuit, and Director, Cancer Control & Population Health Research Program, University of Kansas Cancer Center
Christie Befort, Assistant Professor, Department of Preventive Medicine and Public Health, University of Kansas Medical Center and School of Medicine
Kimber P. Richter, Associate Professor, Department of Preventive Medicine and Public Health, University of Kansas Medical Center and School of Medicine, and Clinical Director, UKanQuit.
References
- 1.Rigotti N, Munafo M, Stead L. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2007:CD001837. doi: 10.1002/14651858.CD001837.pub2. [DOI] [PubMed] [Google Scholar]
- 2.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: The case of smoking cessation. Health Educ Res. 2003 Apr;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 3.Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: A systematic review. Arch Intern Med. 2008 Oct 13;168:1950–1960. doi: 10.1001/archinte.168.18.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freund M, et al. Smoking care provision in hospitals: A review of prevalence. Nicotine Tob Res. 2008;10:757–774. doi: 10.1080/14622200802027131. [DOI] [PubMed] [Google Scholar]
- 5.Koplan KE, et al. A computerized aid to support smoking cessation treatment for hospital patients. J Gen Intern Med. 2008 Aug;23:1214–1217. doi: 10.1007/s11606-008-0610-4. Epub May 9, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Joint Commission. [last accessed Sep. 16, 2009];A Comprehensive Review of Development and Testing for National Implementation of Hospital Core Measures. 2002 http://www.jointcommission.org/NR/rdonlyres/48DFC95A-9C05-4A44-AB05-1769D5253014/0/AComprehensiveReviewofDevelopmentforCoreMeasures.pdf.
- 7.The Joint Commission. [last accessed Sep. 16, 2009];Performance Measurement Initiatives. 2004 http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement.
- 8.Sonel AF, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: Insights from CRUSADE (Can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines?) Circulation. 2005 Mar 15;111:1225–1232. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- 9.Prochaska JJ, Gill P, Hall SM. Treatment of tobacco use in an inpatient psychiatric setting. Psychiatr Serv. 2004 Nov;55:1265–1270. doi: 10.1176/appi.ps.55.11.1265. [DOI] [PubMed] [Google Scholar]
- 10.Rigotti N. Massachusetts General Hospital & Partners HealthCare System Model: Treatment for hospitalized smokers. In Hospital Systems for Treating Tobacco Dependence Among Hospital Inpatients. Proceedings of the Annual National Conference on Tobacco or Health; Minneapolis. Oct. 2007.p. 43. Abstract book. [Google Scholar]
- 11.The Joint Commission. The Joint Commission releases Improving America’s Hospitals: The Joint Commission’s Annual Report on Quality and Safety 2007. Jt Comm Perspect. 2007 Dec;27:1–3. [PubMed] [Google Scholar]
- 12.Wiliams SC, et al. The adoption of smoke-free hospital campuses in the United States. Tob Control. 2009 Aug 20; doi: 10.1136/tc.2009.030494. [DOI] [PubMed] [Google Scholar]
- 13.Richter KP, et al. Hospital Systems for Treating Tobacco Dependence Among Inpatients. Abstract, 2007 National Conference on Tobacco or Health; Minneapolis. Oct. 25, 2007; [last accessed Sep. 17, 2009]. http://ncth.confex.com/ncth/2007/techprogram/P14216.HTM. [Google Scholar]
- 14.Kansas Department of Health and Environment. Kansas Health Statistics Report. Kansas City, Kansas: Kansas Department of Health and Environment; 2007. [Google Scholar]
- 15.Centers for Disease Control and Prevention. [last accessed Sep. 2009];The 2004 Surgeon General’s Report: The Health Consequence of Smoking: What It Means to You. http://www.cdc.gov/tobacco/data_statistics/sgr/2004/pdfs/whatitmeanstoyou.pdf.
- 16.Chen Y, Dales R, Krewski D. Asthma and the risk of hospitalization in Canada: The role of socioeconomic and demographic factors. Chest. 2001 Mar;119:708–713. doi: 10.1378/chest.119.3.708. [DOI] [PubMed] [Google Scholar]
- 17.Hughes JR, et al. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry. 1986 Aug;143:993–997. doi: 10.1176/ajp.143.8.993. [DOI] [PubMed] [Google Scholar]
- 18.Mester R, et al. Survey of smoking habits and attitudes of patients and staff in psychiatric hospitals. Psychopathology. 1993;26:69–75. doi: 10.1159/000284802. [DOI] [PubMed] [Google Scholar]
- 19.Brown C. [last accessed Sep. 16, 2009];Tobacco and Mental Health: A Literature Review. http://www.ashscotland.org.uk/ash/files/tobacco%20and%20mental%20health.pdf.
- 20.McNally L, et al. A survey of staff attitudes to smoking-related policy and intervention in psychiatric and general health care settings. J Public Health (Oxf) 2008 Sep;28:192–196. doi: 10.1093/pubmed/fdl029. Epub Jun. 29, 2006. [DOI] [PubMed] [Google Scholar]
- 21.Williams SC, et al. Quality of care in U.S. hospitals as reflected by standardized measures, 2002–2004. N Engl J Med. 2005 Jul 21;353:255–264. doi: 10.1056/NEJMsa043778. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults in the United States, 2000. MMWR Morb Mortal Wkly Rep. 2002 Jul;51(29):642–645. [PubMed] [Google Scholar]