Abstract
Background
Lecithin:cholesterol acyltransferase (LCAT) catalyzes the formation of plasma cholesteryl ester, plays a key role in high density lipoprotein (HDL) metabolism, and has been believed to be critical in the process of reverse cholesterol transport (RCT).
Method and Results
The role of LCAT in RCT from macrophages was quantitated using a validated assay involving intraperitoneal injection in mice of 3H-cholesterol-labeled J774 macrophages and monitoring appearance of tracer in plasma, liver, bile and feces. Human LCAT overexpression in human apoA-I transgenic mice substantially increased plasma HDL-C levels, but, surprisingly, did not increase macrophage RCT. Even in the setting of co-expression of SR-BI or CETP, both of which promoted the transfer of LCAT-derived HDL-CE to the liver, LCAT overexpression still had no effect on RCT. Serum from LCAT overexpressing mice had reduced ability to promote cholesterol efflux from macrophages ex vivo via ABCA1. To determine the effect of LCAT deficiency on macrophage RCT, LCAT-/- and LCAT+/- mice were compared to wild-type mice. Despite extremely low plasma levels of HDL-C, LCAT deficient mice had only a 50% reduction in RCT. LCAT+/- mice had normal RCT despite a significant reduction in HDL-C. Serum from LCAT deficient mice had increased ability to promote ABCA1-mediated cholesterol efflux from macrophages ex vivo.
Conclusion
These results demonstrate that LCAT overexpression does not promote an increased rate of macrophage RCT. While LCAT activity does become rate-limiting in the context of complete LCAT deficiency, RCT is reduced by only 50% even in the absence of LCAT. These data suggest that macrophage RCT may not be as dependent on LCAT activity as has been previously believed.
Keywords: apolipoproteins, atherosclerosis, lipids, metabolism
Introduction
Lecithin:cholesterol acyltransferase (LCAT) is a key enzyme in the metabolism of high density lipoproteins (HDL). It is responsible for the synthesis of cholesteryl esters (CE) in human plasma by catalyzing a reaction in which a fatty acyl residue from the sn-2 position of phosphatidylcholine is transferred to the 3-beta-hydroxy group of cholesterol, resulting in formation of CE (1). The hydrophobic CE moves to the core of the HDL particle, contributing to the generation of mature HDL particles and their progressive enlargement. The importance of LCAT in normal HDL metabolism is clear from the genetic conditions LCAT deficiency and fish-eye disease (2,3), both of which are associated with markedly reduced levels of plasma HDL cholesterol. Inability to synthesize cholesteryl ester via LCAT results in rapid catabolism of HDL-associated apolipoproteins apoA-I and apoA-II.
In addition to its role in HDL metabolism, LCAT has been proposed to have a critical and central role in reverse cholesterol transport (RCT), the process by which excess peripheral cholesterol is effluxed to HDL-based acceptors and returned to the liver for biliary excretion. Glomset proposed that LCAT was central to RCT by removing free cholesterol from the surface of HDL, thus helping to maintain a gradient of free cholesterol from cells to HDL (4). While this has been a widely accepted paradigm, there are several reasons to question the critical nature of LCAT in RCT. First, while passive diffusion was previously considered the dominant mechanism of cellular cholesterol efflux, it is now recognized that facilitated transport via ABCA1, ABCG1, and possibly SR-BI are quantitatively important and are likely to be less sensitive to a free cholesterol gradient. Second, neither LCAT deficient humans nor mice appear to be at the markedly increased risk of atherosclerosis that might be expected if they had a major defect in RCT. Given this uncertainty, we used a previously validated method for specifically assessing macrophage to feces RCT in mice (5-9) to address the role of LCAT in macrophage RCT in mice. Our conclusions are that neither LCAT over-expression nor loss-of-function have the expected effects on macrophage RCT based on the current paradigm, and suggest that LCAT may not be a critical regulator of RCT, at least from macrophages.
Methods
Vector Construction
The AAV8 TBG hLCAT vector contains the human LCAT cDNA insert followed by SV-40 poly A tail, and is driven by the liver-specific human TBG promoter. The AAV8 hLCAT were produced using a chimeric packaging construct in which the AAV2 rep gene is fused with the cap gene of serotype 8 (10,11).The control vector consisted of the LacZ gene packaged into serotype 8.
Plasma Lipid Analysis
Plasma total cholesterol, HDL cholesterol, and triglyceride were measured on a Cobas Fara, plasma 3H-cholesterol was counted by liquid scintillation counting. Pooled plasma (160 μL) from mice was analyzed by fast protein liquid chromatography (FPLC) gel filtration (Amersham Pharmacia Biotech, Piscataway, NJ). The cholesterol concentrations in the FPLC fractions were determined by an enzymatic assay (Wako Pure Chemical Industries Ltd, Osaka, Japan). Free cholesterol and esterified cholesterol in the samples were separated by Thin layer Chromatography (TLC) and quantified by liquid scintillation counting to determine %CE (12).
LCAT activity assay
Plasma Cholesterol Esterification Rate (CER) expressed in nmols/h/ml plasma was determined using a modification of the Stokke and Norum assay (13). Briefly, each plasma sample is equilibrated overnight (4°C) in a glass tube with a paper disc containing trace amount (0.3 μCi) of 3H-cholesterol, next day the reaction takes place during a 30 min incubation at 37°C and it is terminated by adding 1 ml of 100% ethanol. Following a 20 min centrifugation at 3200 rpm at RT the liquid phase is removed and evaporated to dryness under nitrogen gas. FC and CE in the samples are then separated by TLC.
Immunoblotting
5μl of pooled plasma or 2 μl of each fraction plasma per lane was used for immunoblotting. The plasma sample was resolved on NuPAGE 4-12% Bis-Tris SDS-PAGE (Invitrogen, Carlsbad, Calif) and transferred to ECL Hybond membrane (Amersham Pharmacia Biotech, Piscataway, NJ). The ApoA-1 was detected using an anti-human ApoA-1 primary antibody (Wako Pure Chemical Industries Ltd, Osaka, Japan) and horseradish peroxidase conjugated donkey anti-goat IgG. The LCAT was detected using an anti-LCAT primary antibody (NOVUS biologicals, Littleton, CO) and horseradish peroxidase conjugated donkey anti-rabbit IgG.
Cholesterol efflux studies
J 774 macrophages were plated in 12 well plate (0.14 × 106/ml) in RPMI 1640 supplemented with 10% (v/v) FBS + gentamycin. After one day, cells were labeled for 24h with 3μCi/ml of 3H-cholesterol in the presence of 5.0% FBS. The experiments were performed in the presence of 2μg/ml of the ACAT inhibitor CP113,818 to prevent cellular accumulation of CE. Cells were extensively washed with MEM Hepes with 1% BSA, and then J 774 macrophages were equilibrated with or without 0.3mM cAMP which activates mainly ABCA1 in 0.2% BSA containing medium for 14h (14). At the end of equilibration period, cell monolayers were washed once with MEM Hepes containing 1% BSA and once with MEM Hepes. Subsequently, efflux of cholesterol was induced by incubation for 4h with each pooled plasma diluted to 2.5%. FC efflux was obtained by measuring the release of radio labeled cholesterol into the medium, as previously described (15).
Bone marrow macrophages were isolated from human ApoA-1 tg (hApoA-1 tg) mice and plated. Cells were labeled with 3H-cholesterol (2 μCi/ml; Amersham Pharmacia Biotech, Piscataway, NJ) and loaded with or without 25 μg/ml acetyl LDL (ac-LDL) for 24 hours. Then cells were washed and equilibrated overnight in the presence of GW3965 (10μM) in serum-free medium. For cholesterol efflux, cells were treated with or without 10 μM probucol for 2 hours (16). After which 2% pooled plasma samples for ac-LDL loaded macrophage or 1.75% pooled plasma samples for ac-LDL unloaded macrophage were added to cells as acceptors. After 4 hours, aliquots of the medium were removed, and the 3H-cholesterol released was measured by liquid scintillation counting. The 3H-cholesterol present in the cells was determined by extracting the cell lipids in isopropanol (17).
RCT studies
RCT studies were performed as previously described (5-9). J774 cells were obtained from American Type Culture Collection (ATCC, Manassas, Va) and were grown in suspension in RPMI 1640 supplemented with 10% fetal bovine serum (FBS). Cells were radiolabeled with 5μCi/mL 3H-cholesterol and cholesterol enriched with 100 μg/mL of acetylated LDL for 48 hours. These foam cells were washed twice, equilibrated in medium with 0.2% bovine serum albumin (BSA) for 6 hours, spun down, and resuspended in RPMI medium immediately before use.
Independent experiments were performed in hApoA-1 transgenic mice (Jackson Laboratories, Bar Harbor, ME) injected 1×1012GC AAV8 hLCAT, 1×1010GC AAV8 hLCAT, 1×1010GC AAV8 hLCAT +1×1011GC AAV8 hCETP or 1×1010GC AAV8 hLCAT +1×1011GC AAV8 murin SR-B1 (mSR-B1) to determine the effect of LCAT over expression on RCT, and in LCAT-/- mice (in-house bred), LCAT+/- mice and WT (Jackson Laboratories, Bar Harbor, ME) mice to determine the effect of LCAT deficiency. All mice were fed a standard chow diet. In the initial experiment, mice were divided into 2 groups. The 1×1012GC AAV8 hLCAT (n=8) or AAV8 LacZ (n=7) were injected intraperitoneally for 12-16 week old hApoA-1 tg male mice, and on day 26, animals were injected intraperitoneally with 3H-Cholesterol labeled J774 cells as described previously (5), and caged individually with unlimited access to food and water. Blood was collected at 6, 24, and 48 hours, and plasmas were used for liquid scintillation counting. Feces were collected continuously from 0 to 48 hours and stored at 4°C before counted in liquid scintillation counting. At study termination (48 hours after injection), mice were exsanguinated and perfused with cold PBS, and portions of the liver were removed and flash-frozen for lipid extraction and gene expression analysis.
In sequential experiments, 1×1010GC AAV8 hLCAT (n=8) or LacZ (n=8), 1×1010GC AAV8 hLCAT +1×1011GC AAV8 hCETP (n=8) or 1×1010GC AAV8 LacZ +1×1011GC AAV8 hCETP (n=6), 1×1010GC AAV8 hLCAT +1×1011GC AAV8 mSR-B1 (n=8) or 1×1010GC AAV8 LacZ +1×1011GC AAV8 mSR-B1 (n=7) were injected intravenously for 12-16 week-old hApoA-1 tg male and on day 26, animals were injected intraperitoneally with 3H-Cholesterol labeled J774 cells and performed RCT study same as above. Furthermore, RCT study was performed in 12-16 week-old WT female mice (Jackson Laboratories, Bar Harbor, ME) (n=8), LCAT+/- female mice (in-house bred) (n=8) and LCAT-/- female mice (in-house bred) (n=8).
Liver, bile, and fecal analyses
Liver lipids were extracted according to the procedure of Bligh and Dyer (18). The lipid layer was collected, evaporated, resuspended in toluene, and counted in liquid scintillation counting. Results were expressed as a percentage of injected cpm/liver. The bile was diluted up to 200 μl with PBS, and counted in liquid scintillation counting. The total feces collected from 0 to 48 hours were weighed and soaked in distilled water (1 ml water /100 mg feces) overnight at 4°C. The next day, an equal volume of ethanol was added, and the samples were homogenized. 2 ml of the homogenized samples was combined with 2ml ethanol, and counted in liquid scintillation counting.
Statistical Analysis
Values are presented as mean ± SD. Results were analyzed with the use of GraphPad Prism Software. Results involving LCAT overexpressing mice compared with controls, including plasma lipid and tracer levels, fecal excretion of tracer, and assays of cholesterol efflux were analyzed by Student’s t test. Results involving LCAT homozygous and heterozygous knockout mice compared with controls, including the same parameters, were analyzed by one way ANOVA with Tukey’s multiple comparison test..
RESULTS
LCAT overexpression substantially increased HDL-C levels but not macrophage RCT in vivo
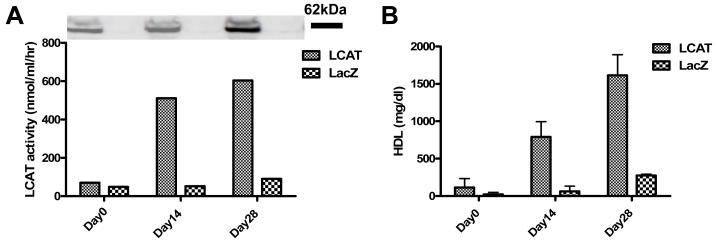
In a pilot study, adeno-associated viral vectors, with the liver-specific promoter TBG, encoding human LCAT (AAV8-TBG-hLCAT) or lacZ (AAV8-TBG-lacZ) were injected i.p. into hApoA-I transgenic mice at a dose of 1×1012 GC. Blood was drawn at baseline and 2 and 4 weeks after injection. Plasma LCAT protein and activity increased by two weeks after injection and were stable at 4 weeks (Figure 1A). Plasma HDL-C levels were also significantly increased at 2 weeks and stable at 4 weeks (Figure1B).
Figure 1.
HApoA-1 tg mice were injected 1×1012GC of hLCAT AAV8 or LacZ AAV (n=8/each group) and taken blood on day 0,14,and 28days. A, pooled plasma was used for LCAT protein expression level and LCAT activity at each time point. B, plasma HDL level of each time point was determined on a Cobas FARA. Data shown are mean ± SD.
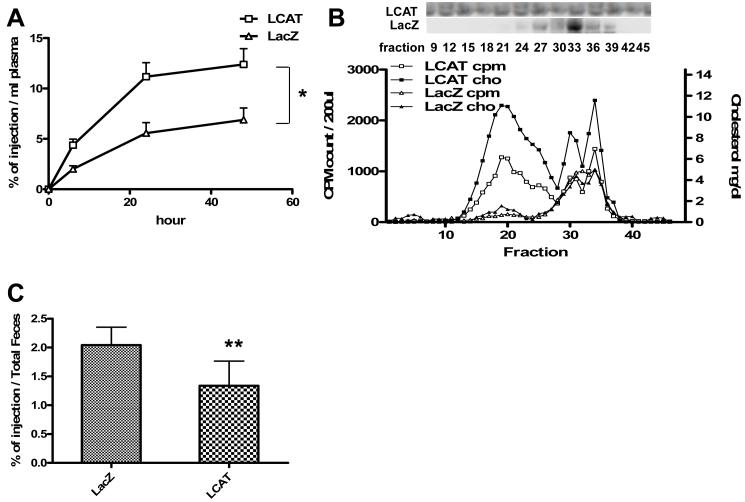
To determine the effect of LCAT overexpression on RCT, 1×1012GC of AAV8-TBG-hLCAT was injected intraperitoneally into hApoA-I transgenic mice and compared with the same dose of control AAV8-TBG-LacZ. 4 weeks after injection, plasma LCAT activity was 6.7-fold higher in the LCAT-expressing group compared with the control group (603.5 vs 90.3 nmol/ml/hr) resulting in a 5.8-fold increase in HDL-C levels (1614±86 vs 276±17 mg/dl). Cholesterol loaded and 3H-cholesterol labeled J774 macrophages were injected at 4 weeks in order to assess macrophage RCT. LCAT-overexpressing mice had higher plasma 3H-cholesterol counts at all time points compared with controls (p<0.05) (Figure 2A). FPLC analysis at 24 hours confirmed that the lipoprotein distribution of 3H-cholesterol in plasma was similar to that of cholesterol mass, and demonstrated markedly increased cholesterol mass and 3H-cholesterol counts particularly in a very large HDL fraction (Figure 2B). Despite the increase in plasma HDL cholesterol mass and tracer, there was a significant 20% decrease (5.48±0.9 vs 4.40±1.0 %of injection / total liver) in 3H-sterol in liver (p<0.05), a significant 66% decrease (0.034±0.005 vs 0.011±0.003 %of injection /□l of bile) in 3H-sterol in bile (p<0.01), and a significant 35% decrease in fecal 3H-sterol over the 48 hour period of the experiment (p<0.01) (Figure 2C).
Figure 2.
Macrophage RCT in hApoA-1 tg mice injected 1×1012GC hLCAT AAV8 (n=8) or LacZ as a control (n=7). A, the change of 3H-labeled cholesterol in plasma. B, 3H-labeled cholesterol lipoprotein profile, Cholesterol mass profile and Western blot of hApoA-1 using each fraction of pooled plasma samples drawn 48 hours after injection of J774 cells. C, 3H-labeled cholesterol in feces of each group. Data shown are mean ± SD.*P<0.05, **P<0.01.
We performed an experiment with more modest overexpression of human LCAT using injection of only 1×1010GC (2 orders of magnitude less) of AAV8-TBG-hLCAT into hApoA-I transgenic mice. Four weeks after injection, the plasma LCAT activity in LCAT-expressing mice was 2.1-fold higher than in control mice (348.7 vs 163.3 nmol/ml/hr) resulting in a more modest 2.9-fold increase in HDL-C (419±165 vs 145±7 mg/dl). Upon performance of the RCT study, LCAT-overexpressing mice had higher plasma 3H-cholesterol counts at all time points compared with controls (p<0.05) (Figure 3A). FPLC analysis confirmed substantially increased cholesterol mass and 3H-cholesterol counts in the HDL fraction in the LCAT group (Figure 3B). There was no significant change in 3H-sterol in bile and liver at 48 hours (data not shown), but there was a significant 24% decrease in feces over the 48 hour period (p<0.01) (Figure 3C). These results indicate that while both substantial as well as modest LCAT overexpression increased plasma HDL-C levels, it did not increase RCT from macrophages to feces in vivo.
Figure 3.
Macrophage RCT in hApoA-1 tg mice injected 1×1010GC hLCAT AAV8 (n=8) or LacZ as a control (n=8). A, the change of 3H-labeled cholesterol in plasma. B, 3H-labeled cholesterol lipoprotein profile, Cholesterol mass profile and Western blot of hApoA-1 using each fraction of pooled plasma samples drawn 48 hours after injection of J774 cells. C, 3H-labeled cholesterol in feces of each group. Data shown are mean ± SD.*P<0.05, **P<0.01.
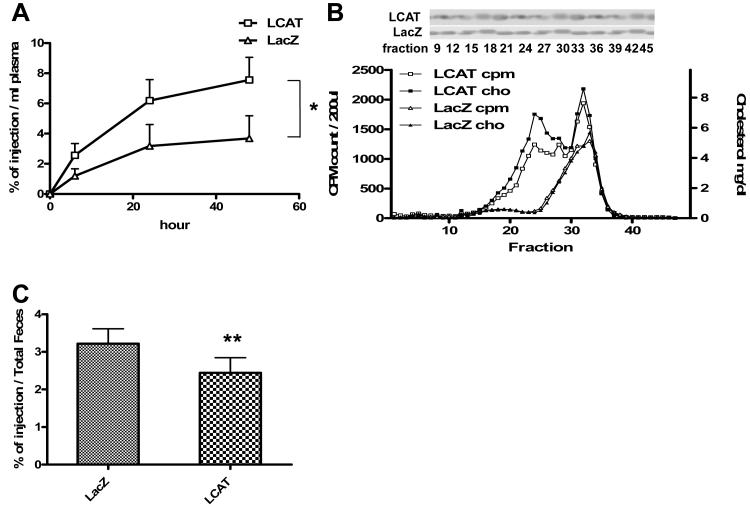
We hypothesized that cholesterol efflux via the ABCA1 pathway may have been reduced in LCAT overexpressing mice due to reduced availability of lipid-poor ApoA-I in the setting of increased cholesterol esterification and formation of mature HDL particles. To test this hypothesis, plasma from mice injected with 1×1012GC of AAV8-hLCAT was used for ex vivo cholesterol efflux studies compared to plasma from control AAV8-lacZ injected mice. Plasma from LCAT-overexpressing mice had significantly reduced capacity to promote ABCA1-specific efflux by 64% from J774 macrophages (p<0.01) (Fig 4A) and by 19% from cholesterol-loaded (p<0.01) or non-cholesterol-loaded (p<0.05) bone marrow macrophages (Fig. 4B, 4C). However, there was reciprocal increased capacity to promote non-ABCA1-mediated efflux (Fig. 4A-C), likely due to combination of ABCG1 mediated efflux and passive diffusion. Nevertheless, the reduced ABCA1-mediated cholesterol efflux may have contributed to the overall reduced macrophage RCT seen in the context of LCAT overexpression.
Figure 4.
Efflux study using pooled plasma taken from hApoA-1 tg mice injected 1×1012GC hLCAT AAV8 or LacZ as a control using J774 macrophage, and bone marrow macrophage. A, Total (with cAMP), ABCA1-independent (without cAMP), and ABCA1-dependent efflux in J774 macrophage. B, Total, ABCA1-independent (with probucol), and ABCA1-dependent efflux in BMM with ac-LDL. C, Total, ABCA1-independent (with probucol), and ABCA1-dependent efflux in BMM without ac-LDL. Data shown are mean ± SD. *P<0.05, **P<0.01.
LCAT overexpression did not promote macrophage RCT even in the setting of SR-BI overexpression or CETP expression
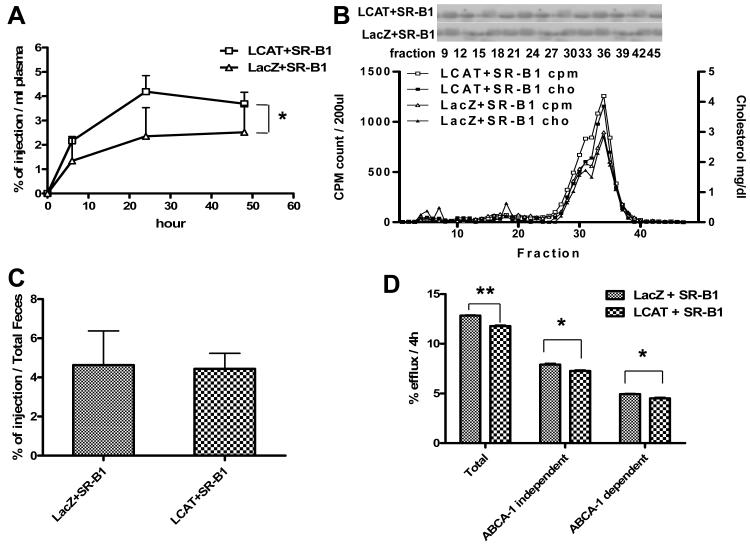
We previously demonstrated that hepatic SR-BI is an important determinant of macrophage RCT with increased RCT observed upon overexpression of SRB1(6). We therefore hypothesized that in the setting of LCAT overexpression hepatic SR-BI is rate-limiting in the RCT pathway. To test this hypothesis, we overexpressed LCAT in the setting of SRB1 overexpression in hApoA-I transgenic mice. On the background of SR-BI overexpression, LCAT overexpression resulted in a 168% increase in HDL-C level (96±6 mg/dl vs 36±13 mg/dl) but HDL-C levels were much lower than with LCAT overexpression alone. In the RCT study, on the background of SR-BI overexpression LCAT overexpression resulted in higher plasma 3H-cholesterol counts at all time points compared with controls (p<0.05) (Figure 5A). FPLC analysis demonstrated increased cholesterol mass and 3H-cholesterol counts in the HDL fraction in the LCAT expressing group (Figure 5B) but without evidence of the very large HDL particle seen with LCAT overexpression alone (Fig.3B). There were no significant differences in 3H-sterol in bile and liver at 48 hours (data not shown), or in feces collected over the 48 hour period (Figure 5C). Thus even in the setting of SR-BI coexpression, LCAT overexpession failed to promote RCT. However, overexpression of SR-BI did prevent the decrease in RCT observed with LCAT overexpression alone. Ex vivo plasma efflux experiments demonstrated that plasma from mice overexpressing LCAT and SR-BI had significantly reduced ABCA1-dependent (p<0.05) and total cholesterol efflux (p<0.01) compared with mice overexpressing only SR-BI (Figure 5D).
Figure 5.
Efflux and macrophage RCT in hApoA-1 tg mice injected 1×1010GC hLCAT AAV8 +1×1011GC m-SR-B1 AAV8 (n=8) or LacZ +1×1011GC m-SR-B1 AAV8 as a control (n=7). A, the change of 3H-labeled cholesterol in plasma. B, 3H-labeled cholesterol lipoprotein profile, Cholesterol mass profile and Western blot of hApoA-1 using each fraction of pooled plasma samples drawn 48 hours after injection of J774 cells. C, 3H-labeled cholesterol in Feces of each group. D, Total (with cAMP), ABCA1-independent (without cAMP), and ABCA1-dependent efflux in J774 macrophage. Data shown are mean ± SD.*P<0.05, **P<0.01.
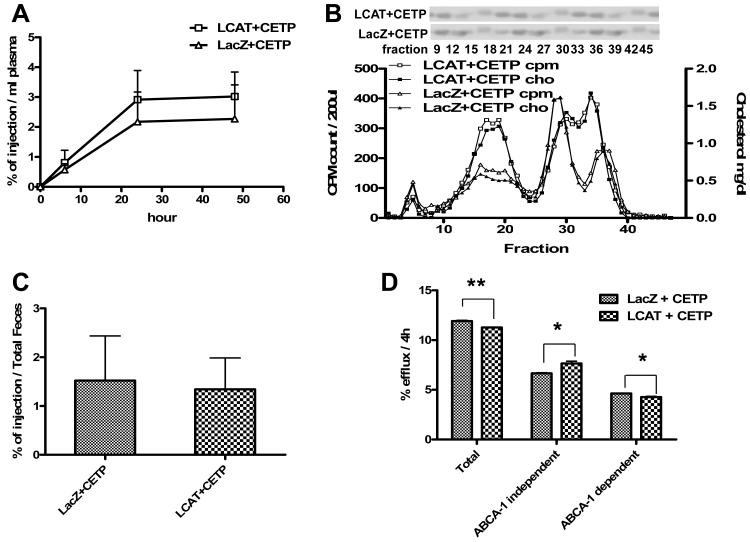
We previously showed that CETP expression promotes macrophage RCT in mice and that CETP expression restores to normal the impaired RCT in SR-BI deficient mice (9). We hypothesized that CETP expression might allow greater flux of cholesteryl esters from HDL to liver in the setting of LCAT overexpression and thus permit LCAT overexpression to promote RCT. In order to test this hypothesis, we expressed human CETP in the setting of human LCAT overexpression in hApoA-I transgenic mice. On the background of CETP expression, LCAT overexpression resulted in a 107% increase in HDL-C level (48±6 mg/dl vs 23±5 mg/dl) but HDL-C levels were much lower than with LCAT expression alone. In the RCT study, on the background of CETP expression, LCAT expression had no effect on plasma 3H-cholesterol counts compared with controls (Figure 6A). FPLC analysis demonstrated greatly increased cholesterol mass and 3H-cholesterol counts in both the LDL fraction and the small HDL fraction in the LCAT overexpressing group (Figure 6B). There were no significant differences in 3H-sterol in bile and liver at 48 hours (data not shown), or in feces collected over the 48 hour period (Figure 6C). Thus CETP expression did not have the effect of permitting LCAT overexpression to promote RCT but did prevent the decrease in RCT observed with LCAT overeexpression alone. Indeed, ex vivo plasma efflux experiments again demonstrated that plasma from mice expressing LCAT and CETP had significantly reduced ABCA1-dependent cholesterol efflux compared with mice expressing only CETP (p<0.05) (Figure 6D).
Figure 6.
Efflux and macrophage RCT in hApoA-1 tg mice injected 1×1010GC hLCAT AAV8 +1×1011GC hCETP AAV8 (n=8) or LacZ +1×1011GC hCETP AAV8 as a control (n=6). A, the change of 3H-labeled cholesterol in plasma. B, 3H-labeled cholesterol lipoprotein profile Cholesterol mass profile and Western blot of hApoA-1 using each fraction of pooled plasma samples drawn 48 hours after injection of J774 cells. C, 3H-labeled cholesterol in feces of each group. D, Total (with cAMP), ABCA1-independent (without cAMP), and ABCA1-dependent efflux in J774 macrophage. Data shown are mean ± SD.*P<0.05, **P<0.01.
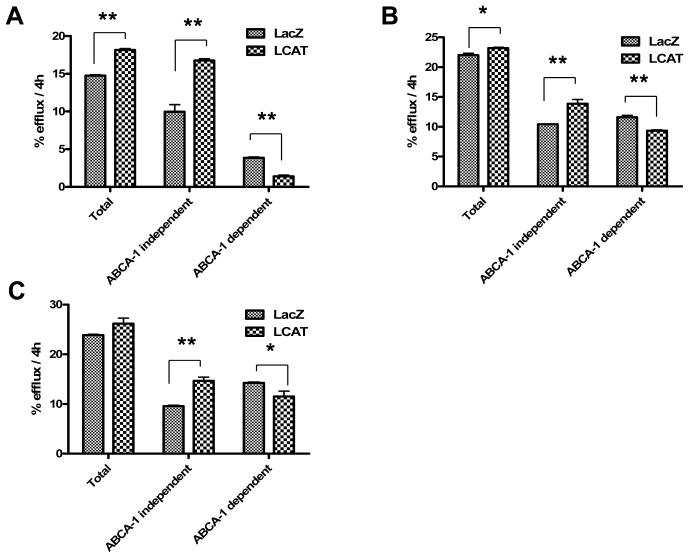
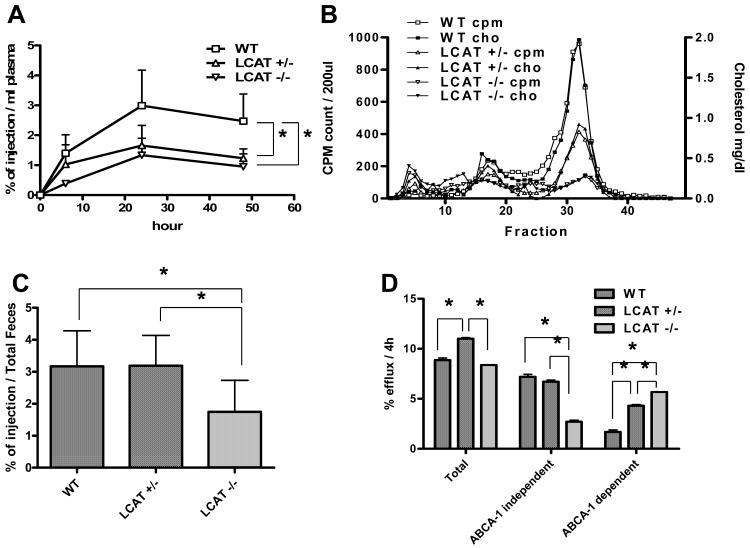
Homozygous LCAT null mice had 50% reduced and heterozygous LCAT null mice had normal macrophage RCT
If cholesterol esterification by LCAT is a critical component of the RCT pathway, then LCAT deficiency would be expected to result in severely reduced RCT. To test this hypothesis, WT mice, LCAT+/- mice, and LCAT-/- mice were used in an RCT study. HDL-C levels were 52±9 vs 38±3 vs 3.4±1.5 mg/dl (WT vs LCAT+/- vs LCAT-/-) and correlated with LCAT activity, 192.2 vs 148.6 vs 0.8nmol/ml/h (WT mice vs LCAT+/- mice vs LCAT-/- mice). In the in vivo RCT study, LCAT-/- mice had significantly decreased plasma 3H-cholesterol counts compared with wild-type controls (p<0.05), and LCAT+/- mice were intermediate (Figure 7A). The percent of 3H-cholesterol counts in cholesteryl ester in plasma was markedly reduced in LCAT-/- mice (23%) compared with 73% in LCAT+/- mice and 76% in WT mice. FPLC analysis confirmed that the 3H-cholesterol in plasma tracked closely with the cholesterol mass, demonstrating markedly decreased cholesterol mass and 3H-cholesterol counts in the HDL fractions in the LCAT-/- mice and intermediate levels in the LCAT+/- mice compared with controls (Figure 7B). There were no significant differences among the three groups in 3H-sterol in liver or bile at 48 hours (data not shown). Fecal excretion of 3H-sterol over 48 hours was significantly reduced by 45% in LCAT-/- mice (p<0.05), but was normal in LCAT+/- mice (Figure 7C). An ex vivo cholesterol efflux study using J774 cells demonstrated that plasma from LCAT-/- mice promoted total cholesterol efflux to the same extent as WT mice plasma and promoted significantly greater ABCA1-specific efflux. Plasma from LCAT+/- mice promoted more total efflux (p<0.05) and more ABCA1-specific efflux (p<0.05) compared with WT mice plasma (Figure 7D).
Figure 7.
Efflux and macrophage RCT in LCAT-/- KO mice (n=8), LCAT+/- KO mice (n=8) or WT mice (n=8). A, the change of 3H-labeled cholesterol in plasma. B, 3H-labeled cholesterol lipoprotein profile and Cholesterol mass profile of pooled plasma samples drawn 48 hours after injection of J774 cells. C, 3H-labeled cholesterol in feces of each group. D, Total (with cAMP), ABCA1-independent (without cAMP), and ABCA1-dependent efflux in J774 macrophage. Data shown are mean ± SD.*P<0.05.
DISCUSSION
In these studies, we used overexpression of human LCAT in hApoA-I transgenic mice as a model to assess effects of LCAT overexpression on macrophage RCT. We found that while both marked and moderate LCAT overexpression substantially raised levels of HDL-C as expected, they unexpectedly resulted in reduced macrophage RCT, accompanied by reduced ability of the plasma from LCAT-overexpressing mice to promote ABCA1-mediated efflux from macrophages. Even co-expression of SR-BI or CETP, intended to facilitate the return of LCAT-derived HDL-CE to the liver, failed to result in promotion of RCT by LCAT overexpression. In addition, while LCAT deficient mice did have reduced macrophage RCT, consistent with a role for LCAT in RCT, it was reduced by only 50% despite markedly reduced plasma HDL-C levels. LCAT heterozygotes had normal macrophage RCT despite significantly lower plasma HDL-C levels and plasma LCAT activity. Thus our results challenge the paradigm that LCAT plays a central role in modulating the rate of macrophage RCT, and suggest that therapeutic intervention to increase LCAT activity may not necessarily have an RCT-promoting and thus atheroprotective effect.
In this light, it is of interest to review the literature on the relationship between LCAT overexpression and atherosclerosis in animal models. In LCAT transgenic rabbits fed a cholesterol diet, HDL levels were significantly increased (19) and atherosclerotic lesions were significantly reduced (20). In contrast, using human LCAT transgenic mice fed an atherogenic diet, Berard et al reported that overexpression of human LCAT (50-116 fold) was associated with markedly increased atherosclerosis (21). In other studies in human LCAT transgenic mice fed an atherogenic diet by Mehlum et al, overexpression of LCAT (17-fold) was associated with no difference (22) or increased (23) atherosclerosis depending on the duration of the study. Furbee et al reported that 10-fold overexpression of human LCAT in transgenic mice fed an atherogenic diet did not result in increased aortic cholesterol deposition (24). Mertens et al used a recombinant adenovirus (5×108 pfu) encoding human LCAT in the LDLR-/- ob/ob double mutant mice fed a chow diet and reported there was no change of HDL level despite an increase in plasma LCAT activity and a 42% reduction in aortic root atherosclerosis (25). The inconsistency in the results may be related in part to varied levels of LCAT overexpression and possibly the specific murine models used.
In the current studies, we used an AAV vector to stably overexpress LCAT at two different doses, which increased plasma HDL-C levels in a dose-dependent fashion. Despite increases in HDL-C, we found no evidence of promotion of macrophage RCT by LCAT overexpression, largely consistent with the mouse atherosclerosis results. We initially hypothesized that LCAT overexpression, by generating large cholesterol-enriched HDL particles, may have resulted in a functional block in the efficient transfer of HDL-CE into liver. Indeed, when a human CETP transgene was introduced into the LCAT transgenic mice with increased atherosclerosis mentioned above (21), CETP expression reduced atherosclerosis. Importantly, atherosclerosis in the double transgenic mice was still greater than in control mice, indicating that even co-expression of LCAT and CETP was not atheroprotective. We previously showed that overexpression of either SR-BI or CETP, despite reducing HDL-C levels, promotes macrophage RCT (5, 9). Thus we tested whether uptake of HDL-CE into liver in LCAT-overexpressing mice was rate-limiting by co-expressing either SR-BI or CETP together with LCAT. While each reduced the plasma HDL-C level as expected, neither converted LCAT overexpression to an intervention that promoted macrophage RCT. We conclude that the inability of LCAT overexpression to promote macrophage RCT is not explained simply by the fact that hepatic uptake of LCAT-derived HDL-CE is rate-limiting in this setting.
Notably, LCAT deficient humans do not develop obviously premature atherosclerotic vascular disease. Reduced LCAT activity has been reported to be associated with increased intima-media thickness of the carotids (26), but this report is not definitive and more investigation of this issue is needed. Studies of the effects of LCAT deficiency on atherosclerosis in mice are discordant. Lambert et al showed that LCAT-/- mice in the C57Bl/6 or LDLr-/- background fed a cholic acid containing atherogenic diet had smaller atherosclerotic lesions compared with their counterparts with active LCAT (27). Consistent with that observation, Ng et al showed that aortic atherosclerotic lesions in male LCAT-/- mice on an apoE-/- background fed a chow diet had a 52% reduction in atherosclerosis; even LCAT+/- mice had a 24% reduction (28). In contrast, Furbee et al reported that LCAT deficiency in LDLr-/- and apoE-/- mice fed an atherogenic diet resulted in increased aortic cholesterol deposition (29). In the current study, we found that heterozygous deficiency of LCAT (LCAT+/- mice) was associated with normal macrophage RCT despite significantly reduced plasma HDL-C levels and plasma LCAT activity. Complete deficiency of LCAT, accompanied by marked 93% reduction in HDL-C levels, did result in a 50% reduction in RCT, indicating that LCAT does become rate limiting in the context of complete LCAT deficiency. However, substantial RCT from macrophage to feces still occurred in the absence of LCAT activity, highlighting the fact that LCAT is not required for RCT and indicating that substantial RCT can occur via unesterified cholesterol.
We considered the hypothesis that LCAT expression influences the generation of “pre-beta HDL” or lipid-poor apoA-I that serves as the acceptor for ABCA1-mediated cholesterol efflux. ABCA1 is a critical transporter that facilitates efflux of cellular cholesterol to lipid poor apoA-I; macrophage specific deficiency of ABCA1 resulted in significantly increased atherosclerosis in apoE-/- mice fed a chow diet (30) and in LDLR-/- mice fed a high cholesterol western type diet. (31). Our experiments using plasma from LCAT-overexpressing mice revealed that although there was only a modest change in total efflux to serum, the mechanism of efflux changed greatly. The ability to promote cholesterol efflux from macrophages via the ABCA1 pathway was significantly reduced by LCAT overexpression while ABCA1 independent efflux was increased. As expected, increased HDL-C levels in LCAT overexpression did increase efflux via “non-ABCA1” pathways (such as ABCG1 and possibly SR-BI). Conversely, plasma from LCAT deficient mice had a significantly greater capacity to promote ABCA1-mediated efflux.
In summary, stable LCAT overexpression failed to increase macrophage RCT despite substantially increasing HDL-C levels. Even in the setting of SR-BI or CETP co-expression, both of which increased the delivery LCAT-derived HDL-CE to the liver, LCAT overexpression failed to increase macrophage RCT. In the heterozygous state, moderate LCAT deficiency did not impair RCT despite lower HDL-C levels. Complete LCAT deficiency did reduce RCT by 50% but showed that substantial macrophage RCT can still occur in the absence of LCAT activity. These studies challenge the long-held belief that LCAT is critical for RCT and important in modulating its rate. While additional experiments are needed, these results bring into question whether pharmacologic LCAT activation would necessarily promote RCT and therefore be athero-protective.
Acknowledgments
We are indebted to Aisha Wilson, Edwige Edouard, MaoSen Sun, David Chang, Michelle Joshi, Debra Cromley, Sara Hayes, Sandhya Sankaran, Leticia Pruscino, Phyllis May, Anna DiFlorio, and Linda Morrell for their excellent technical assistance, to Hui Li for animal inventory management, and to Dawn Marchadier for lab management.
Funding Sources
This work was supported by P01-HL22633 and P01-HL59407 from the National Heart, Lung, and Blood Institute.
Daniel J Rader: DJR has been a consultant to and received research funding from Bristol Myers Squibb, Merck, and Pfizer, and has been a consultant to Roche.
Footnotes
Disclosures
Hiroyuki Tanigawa: none
Jeffrey T. Billheimer: none
Jun-ichiro Tohyama: none
Ilia V. Fuki: none
Dominic S Ng. DSN has been a consultant to GlaxoSmithKline and Merck Frosst.
George Rothblat: none
Clinical Perspective
Lecithin:cholesterol acyltransferase (LCAT) is a key enzyme in the metabolism of high density lipoproteins (HDL). It converts “free” cholesterol (form effluxed from macrophages) to cholesteryl ester, permitting formation and progressive enlargement of mature HDL particles. It has long been believed that LCAT is critical in facilitating the process of reverse cholesterol transport, leading to the concept that upregulation of LCAT activity is a therapeutic target for atherosclerosis, but this has never been experimentally proven. Using a validated assay of macrophage-specific reverse cholesterol transport in mice, we explored the effects of both LCAT overexpression (which raises HDL-C levels) and LCAT deficiency (which reduces HDL-C levels). Surprisingly, LCAT overexpression, despite markedly raising HDL-C, did not promote macrophage reverse cholesterol transport. Even co-expression of scavenger receptor BI (SR-BI) or cholesteryl ester transfer protein (CETP), both of which transfer CE out of HDL and facilitate its return to the liver, failed to convert LCAT overexpression into an intervention that promotes reverse cholesterol transport. Furthermore, complete LCAT deficiency, despite reducing HDL-C to < 5% of normal levels, only reduced reverse cholesterol transport by about 50% and moderate LCAT deficiency, despite moderately reducing HDL-C levels, had no effect on reverse cholesterol transport. These studies challenge the long-held belief that LCAT is critical for macrophage reverse cholesterol transport and bring into question whether LCAT activation would necessarily be an athero-protective intervention even though it raises HDL-C levels. The results are consistent with a growing trend focused on HDL quality and function rather than simply plasma HDL-C levels as a target for development of new therapies.
References
- 1.Glomset JA. The mechanism of the plasma cholesterol esterification reaction: plasma fatty acid transferase. Biochim Biophys Acta. 1962;65:128–135. doi: 10.1016/0006-3002(62)90156-7. [DOI] [PubMed] [Google Scholar]
- 2.Norum KR, Gjone E. Familial serum-cholesterol esterification failure. A new inborn error of metabolism. Biochim Biophys Acta. 1967;144:698–700. doi: 10.1016/0005-2760(67)90064-1. [DOI] [PubMed] [Google Scholar]
- 3.Carlson LA, Philipson B. Fish-eye disease. A new familial condition with massive corneal opacities and dyslipoproteinaemia. Lancet. 1979;2:922–924. [PubMed] [Google Scholar]
- 4.Glomset JA. The plasma lecithins:cholesterol acyltransferase reaction. J Lipid Res. 1968;9:155–167. [PubMed] [Google Scholar]
- 5.Zhang Y, Zanotti I, Reilly MP, Glick JM, Rothblat GH, Rader DJ. Overexpression of apolipoprotein A-I promotes reverse transport of cholesterol from macrophages to feces in vivo. Circulation. 2003;108:661–663. doi: 10.1161/01.CIR.0000086981.09834.E0. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Da Silva JR, Reilly M, Billheimer JT, Rothblat GH, Rader DJ. Hepatic expression of scavenger receptor class B type I (SR-BI) is a positive regulator of macrophage reverse cholesterol transport in vivo. J Clin Invest. 2005;115:2870–2874. doi: 10.1172/JCI25327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore RE, Navab M, Millar JS, Zimetti F, Hama S, Rothblat GH, Rader DJ. Increased atherosclerosis in mice lacking apolipoprotein A-I attributable to both impaired reverse cholesterol transport and increased inflammation. Circ Res. 2005;97:763–771. doi: 10.1161/01.RES.0000185320.82962.F7. [DOI] [PubMed] [Google Scholar]
- 8.Naik SU, Wang X, Da Silva JS, Jaye M, Macphee CH, Reilly MP, Billheimer JT, Rothblat GH, Rader DJ. Pharmacological activation of liver X receptors promotes reverse cholesterol transport in vivo. Circulation. 2006;113:90–97. doi: 10.1161/CIRCULATIONAHA.105.560177. [DOI] [PubMed] [Google Scholar]
- 9.Tanigawa H, Billheimer JT, Tohyama JI, Zhang Y, Rothblat G, Rader DJ. Expression of Cholesteryl Ester Transfer Protein in Mice Promotes Macrophage Reverse Cholesterol Transport. Circulation. 2007;116:1267–73. doi: 10.1161/CIRCULATIONAHA.107.704254. [DOI] [PubMed] [Google Scholar]
- 10.Kitajima K, Marchadier DH, Miller GC, Gao GP, Wilson JM, Rader DJ. Complete prevention of atherosclerosis in apoE-deficient mice by hepatic human apoE gene transfer with adeno-associated virus serotypes 7 and 8. Arterioscler Thromb Vasc Biol. 2006;26:1852–1857. doi: 10.1161/01.ATV.0000231520.26490.54. [DOI] [PubMed] [Google Scholar]
- 11.Gao G, Vandenberghe LH, Wilson JM. New recombinant serotypes of AAV vectors. Curr Gene Ther. 2005;5:285–297. doi: 10.2174/1566523054065057. [DOI] [PubMed] [Google Scholar]
- 12.Parks JS, Gebre AK, Furbee JW. Lecithin-cholesterol acyltransferase. Assay of cholesterol esterification and phospholipase A2 activities. Methods Mol Biol. 1999;109:123–131. doi: 10.1385/1-59259-581-2:123. [DOI] [PubMed] [Google Scholar]
- 13.Stokke KT, Norum KR. Determination of lecithin: cholesterol acyltransfer in human blood plasma. Scand J Clin Lab Invest. 1971;27:21–27. doi: 10.3109/00365517109080184. [DOI] [PubMed] [Google Scholar]
- 14.Sakr SW, Williams DL, Stoudt GW, Phillips MC, Rothblat GH. Induction of cellular cholesterol efflux to lipid-free apolipoprotein A-I by cAMP. Biochim Biophys Acta. 1999;1438:85–98. doi: 10.1016/s1388-1981(99)00041-4. [DOI] [PubMed] [Google Scholar]
- 15.Rothblat GH, de la Llera-Moya M, Favari E, Yancey PG, Kellner-Weibel G. Cellular cholesterol flux studies: methodological considerations. Atherosclerosis. 2002;163:1–8. doi: 10.1016/s0021-9150(01)00713-4. [DOI] [PubMed] [Google Scholar]
- 16.Favari E, Zanotti I, Zimetti F, Ronda N, Bernini F, Rothblat GH. Probucol inhibits ABCA1- mediated cellular lipid efflux. Arterioscler Thromb Vasc Biol. 2004;24:2345–2350. doi: 10.1161/01.ATV.0000148706.15947.8a. [DOI] [PubMed] [Google Scholar]
- 17.Wang X, Collins HL, Ranalletta M, Fuki IV, Billheimer JT, Rothblat GH, Tall AR, Rader DJ. Macrophage ABCA1 and ABCG1, but not SR-BI, promote macrophage reverse cholesterol transport in vivo. J Clinical Investigation. 2007;117:2216–2224. doi: 10.1172/JCI32057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bligh EG, Dyer WJ. A rapid method of total lipid extraction and purification. Can J Biochem Physiol. 1959;37:911–917. doi: 10.1139/o59-099. [DOI] [PubMed] [Google Scholar]
- 19.Hoeg JM, Santamarina-Fojo S, Berard A, Cornhill JF, Herderick E, Feldman S, Haudenschild C, Vaisman B, Hoyt RFJ, Demosky S. Overexpression of lecithin:cholesterol acyltransferase in transgenic rabbits prevents diet-induced atherosclerosis. Proc Natl Acad Sci USA. 1996;93:11448–11453. doi: 10.1073/pnas.93.21.11448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brousseau ME, Santamarina-Fojo S, Vaisman BL, Applebaum-Bowden D, Berard AM, Talley GD, Brewer HB, Jr, Hoeg JM. Overexpression of human lecithin:cholesterol acyltransferase in cholesterol-fed rabbits: LDL metabolism and HDL metabolism are affected in a gene dose-dependent manner. J Lipid Res. 1997;38:2537–2547. [PubMed] [Google Scholar]
- 21.Berard AM, Foger B, Remaley A, Vaisman BL, Talley G, Paigen B, Hoyt RFJ, Brewer HBJ, Santamarina-Fojo S. High plasma HDL concentration associated with enhanced atherosclerosis in transgenic mice overexpressing lecithin-cholesteryl acyltransferase. Nature Medicine. 1997;3:744–749. doi: 10.1038/nm0797-744. [DOI] [PubMed] [Google Scholar]
- 22.Mehlum A, Muri M, Hagve TA, Solberg LA, Prydz H. Mice overexpressing human lecithin: cholesterol acyltransferase are not protected against diet-induced atherosclerosis. APMIS. 1997;105:861–868. doi: 10.1111/j.1699-0463.1997.tb05095.x. [DOI] [PubMed] [Google Scholar]
- 23.Mehlum A, Gjernes E, Solberg LA, Hagve TA, Prydz H. Overexpression of human lecithin:cholesterol acyltransferase in mice offers no protection against diet-induced atherosclerosis. APMIS. 2000;108:336–342. doi: 10.1034/j.1600-0463.2000.d01-65.x. [DOI] [PubMed] [Google Scholar]
- 24.Furbee JW, Jr, Parks JS. Transgenic overexpression of human lecithin: cholesterol acyltransferase (LCAT) in mice does not increase aortic cholesterol deposition. Atherosclerosis. 2002;165:89–100. doi: 10.1016/s0021-9150(02)00201-0. [DOI] [PubMed] [Google Scholar]
- 25.Mertens A, Verhamme P, Bielicki JK, Phillips MC, Quarck R, Verreth W, Stengel D, Ninio E, Navab M, Mackness B. Increased low-density lipoprotein oxidation and impaired high-density lipoprotein antioxidant defense are associated with increased macrophage homing and atherosclerosis in dyslipidemic obese mice: LCAT gene transfer decreases atherosclerosis. Circulation. 2003;107:1640–1646. doi: 10.1161/01.CIR.0000056523.08033.9F. [DOI] [PubMed] [Google Scholar]
- 26.Hovingh GK, Hutten BA, Holleboom AG, Petersen W, Rol P, Stalenhoef A, Zwinderman AH, de Groot E, Kastelein JJ, Kuivenhoven JA. Compromised LCAT function is associated with increased atherosclerosis. Circulation. 2005;112:879–884. doi: 10.1161/CIRCULATIONAHA.105.540427. [DOI] [PubMed] [Google Scholar]
- 27.Lambert G, Sakai N, Vaisman BL, Neufeld EB, Marteyn B, Chan CC, Paigen B, Lupia E, Thomas A, Striker LJ. Analysis of glomerulosclerosis and atherosclerosis in lecithin cholesterol acyltransferase-deficient mice. J Biol.Chem. 2001;276:15090–15098. doi: 10.1074/jbc.M008466200. [DOI] [PubMed] [Google Scholar]
- 28.Ng DS, Maguire GF, Wylie J, Ravandi A, Xuan W, Ahmed Z, Eskandarian M, Kuksis A, Connelly PW. Oxidative stress is markedly elevated in lecithin:cholesterol acyltransferase-deficient mice and is paradoxically reversed in the apolipoprotein E knockout background in association with a reduction in atherosclerosis. J Biol Chem. 2002;277:11715–11720. doi: 10.1074/jbc.M112320200. [DOI] [PubMed] [Google Scholar]
- 29.Furbee JW, Jr, Sawyer JK, Parks JS. Lecithin:cholesterol acyltransferase deficiency increases atherosclerosis in the low density lipoprotein receptor and apolipoprotein E knockout mice. J Biol.Chem. 2002;277:3511–3519. doi: 10.1074/jbc.M109883200. [DOI] [PubMed] [Google Scholar]
- 30.Aiello RJ, Brees D, Bourassa PA, Royer L, Lindsey S, Coskran T, Haghpassand M, Francone OL. Increased Atherosclerosis in Hyperlipidemic Mice With Inactivation of ABCA1 in Macrophages. Arterioscler Thromb Vasc Biol. 2002;22:630–637. doi: 10.1161/01.atv.0000014804.35824.da. [DOI] [PubMed] [Google Scholar]
- 31.Van Eck M, Bos IST, Kaminski WE, Orso E, Rothe G, Twisk J, Bottcher A, Van Amersfoort ES, Christiansen-Weber TA, Fung-Leung WP. Leukocyte ABCA1 controls susceptibility to atherosclerosis and macrophage recruitment into tissues. PNAS. 2002;99:6298–6303. doi: 10.1073/pnas.092327399. [DOI] [PMC free article] [PubMed] [Google Scholar]