Abstract
Objective
To assess health care disparities among black and Latino adults with schizophrenia receiving services during the period July 1994–June 2006, and to evaluate trends in observed disparities.
Data Sources
Administrative claims data from the Florida Medicaid program. Data sources included membership files (demographic information), medical claims (diagnostic, service, and expenditure information), and pharmacy claims (prescriptions used and expenditures).
Study Design
We identified adults with at least two schizophrenia claims during a fiscal year. We used generalized estimating equation models to estimate disparities in spending on psychotropic drugs, psychiatric inpatient services, all mental health services, and all health services.
Principal Findings
Spending on psychotropic drugs, mental health, and all health was 0.9–70 percent lower for blacks and Latinos than for whites. With the exception of blacks with substance use disorder comorbidity, minorities were less likely than whites to use psychiatric inpatient services. Psychiatric inpatient spending among users did not differ by race/ethnicity. With the exception of psychiatric inpatient utilization/spending, trend analyses showed no change or modest reductions in disparities.
Conclusions
Black and Latino Medicaid recipients diagnosed with schizophrenia experience health care disparities. Some but not all disparities narrowed modestly over the study period.
Keywords: Racial/ethnic disparities, schizophrenia, quality of care, trends, Medicaid
Schizophrenia affects only 0.7 percent of the U.S. population (2 million adults) (Saha et al. 2005), yet because of its early age of onset, chronicity, significant disability, and premature mortality, this severe mental illness is responsible for 5 percent of all burden of disease (Murray and Lopez 1996). Although U.S. community-based prevalence studies have generated little evidence on comparative rates for Latinos and non-Latino whites (Karno et al. 1987; Dassori, Miller, and Saldana 1995;), they suggest that blacks have a higher prevalence of schizophrenia than whites (Robins and Regier 1991; Kendler et al. 1996;). A recent California cohort study conducted in an insured population showed that the incidence of schizophrenia is three times higher among blacks than whites, the association partly mediated by socioeconomic status (Bresnahan et al. 2007). Although these studies employed standardized diagnostic methods, a previously documented tendency to overdiagnose schizophrenia in black adults may have played a role in these epidemiological findings (Williams and Earl 2007).
The armamentarium of effective treatments for adults with schizophrenia has grown substantially in the past several decades. Even so, the quality of care typically received by people diagnosed with this severe psychiatric illness in the United States falls short of optimal (Lehman 1999). Moreover, quality of schizophrenia care varies depending on the race and ethnicity of patients. Relative to whites, blacks are more likely to use inpatient and emergency services (Snowden and Holschuh 1992) and less likely to receive outpatient care and a variety of recommended interventions (Wang, Demler, and Kessler 2002; Barrio et al. 2003;). Further, during a period when prevailing norms of good care favored atypical (over conventional) and oral (over long-acting injectable) antipsychotic medications, blacks had lower use rates of atypical antipsychotics and higher use rates of injectable antipsychotics than whites (Kuno and Rothbard 2002; Kreyenbuhl et al. 2003;). The evidence is substantially sparser and less consistent for Latinos (Vega et al. 2007).
Despite rising awareness of the significance of disparities, some efforts to eradicate them, and isolated reports of improvements (Trivedi et al. 2005), disparities in health care for blacks and Latinos persist (Brady et al. 2007). For mental health care overall, studies have found either no change (Stockdale et al. 2008) or worsening health care disparities over time (Zuvekas 2005; Cook, McGuire, and Miranda 2007;). However, little is known about the care of minorities with schizophrenia. Daumit et al. (2003) used data on physician office and hospital outpatient department visits from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey to assess use of atypical antipsychotics by race/ethnicity during the period 1992–2000. Among subjects with psychotic disorders, the minority-white disparities in atypical antipsychotic use narrowed during the period 1992–2000, closing for Latinos yet persisting for blacks (Daumit et al. 2003).
In sum, previous research on disparities in schizophrenia care has focused on specific levels of care or specific interventions and little is known about broader patterns of care. Further, little is known about the health care experience of Latinos, or about temporal trends in disparities within the evolving treatment patterns for schizophrenia.
The overall purpose of this study was to study disparities among Medicaid recipients with schizophrenia receiving health care in Florida. We focused on Medicaid because most people in the United States with schizophrenia rely on Medicaid (Frank and Glied 2006), and we chose Florida because of its size and racially and ethnically diverse population. Further, availability of 12 years of data enabled us to evaluate trends in health care disparities. Consistent with the definition proposed by the Institute of Medicine, we define disparities as differences in care not explained by differences in health status or need for services (Smedley, Stith, and Nelson 2003). On the basis of past research, we expected to find racial/ethnic disparities. We hypothesized that because minorities are less likely to receive regular care and atypical antipsychotics, their spending on psychotropic drugs would be lower than that of whites. We further hypothesized that as a result of poorer access to high-quality care, minorities would have a higher likelihood of using psychiatric inpatient services, and as a result of nonclinical considerations, minorities would have higher psychiatric inpatient spending with respect to whites. Since these use patterns work in opposing directions we had no expectation on how total mental health and total health spending might differ among groups. Lastly, on the basis of limited research to date, we hypothesized that observed disparities would diminish over time.
METHODS
We studied health care disparities among adult Medicaid recipients with schizophrenia by contrasting spending levels and trends over time for black, Latino, and whites who were comparable with respect to need-related variables. Within a single payment system with fixed prices, expenditures are equivalent to a “quantity index” measuring the aggregate value of services received. We assessed disparities in ambulatory use of psychotropic drugs and in use of psychiatric inpatient services. We also assessed disparities in total use at two levels of aggregation (all mental health and all health). Because of the skewness in expenditure distributions, we used logarithmic transformation for all spending analyses and a two-part model for analyses of inpatient data. We used generalized estimating equations to obtain estimates of coefficients and the corresponding standard errors for all regressions. Lastly, we used the All-Items Consumer Price Index to adjust expenditures to 2005 dollars (USBLS 2008).
Data Sources and Study Population
We used enrollment files and medical and pharmacy claims from the Florida Medicaid program for fiscal years (FYs) 1995–2006 to create a cohort of continuously enrolled adults aged 18–64 years who had at least two claims with a diagnosis of schizophrenia (International Classification of Diseases, Ninth Revision [ICD-9], diagnostic code 295.xx) recorded on two different service dates during the FY. We defined continuous enrollment as having no more than 2 consecutive months of lapsed enrollment and at least 9 months of enrollment per FY. Our source for demographic information was the Medicaid membership files, and our source for ICD-9 diagnoses, expenditures, and procedures, coded according to Current Procedural Terminology (CPT-4), was the medical claims. Pharmacy claims supplied information on prescription drugs dispensed, classified by National Drug Code (NDC), and on prescription drug expenditures. We excluded data for subjects with Medicare and Health Maintenance Organization coverage because we could not observe all the care they had received.
Measures
Outcomes
Our outcome variables were spending on ambulatory psychotropic drugs; use of psychiatric inpatient services, and for inpatient users only, levels of psychiatric inpatient spending; total mental health spending; and total health spending.
For psychotropic drug spending, we only included expenditures tied to pharmacy claims for classes of medications primarily used to manage psychiatric or substance use disorders (SUDs; list of drugs available upon request). For psychiatric inpatient spending we included inpatient claims with a psychiatric or SUD as primary diagnosis. For total mental health spending we included all expenditures tied to claims that had a psychiatric or SUD as primary diagnosis. For total health spending we included expenditures for all diagnoses.
We selected these measures because while sustained psychotropic treatment with antipsychotic medications is a critical ingredient of high-quality schizophrenia care, poorer quality of care is associated with greater use of psychiatric inpatient services (Lehman 1999; Lehman et al. 2004a; Weiden et al. 2004; dosReis et al. 2008;). In addition, we sought to capture overall patterns of spending.
Explanatory Variables
Our main explanatory variables of interest were indicators of race/ethnicity (black, Latino, white). The Florida Medicaid program uses a racial classification that describes recipients as white, black, Hispanic, Oriental, American Indian, or Other. In any year of the study period, <0.7 percent and <0.2 percent of the people in our cohort were classified as Oriental or American Indian, respectively. Between 36.5 and 44.4 percent of our subjects were classified as whites. While the percent of people who were classified as black varied little over the study period, the percent of people classified as Other and Hispanic varied dramatically due to changes in data recording. An analysis of individuals classified as Other in FY 2005 who were also observed in FY 2006 (n=3,280) revealed that 71 percent were re-classified as Hispanic in FY 2006. No other classification (Oriental, black, or white) received a meaningful number of members. It is likely that many of the 27 percent who remained Other were also Hispanic. Furthermore, a follow-back analysis of all individuals observed in FY 2005 and 2006 revealed that 92 percent of individuals classified as Hispanic in FY 2006 were previously classified as Other. Therefore, we regarded all other groups as Hispanic. As a result of this decision, we have some minor misclassification in our racial/ethnic groups, and very small numbers of Oriental and American Indian people are grouped with Hispanics. We use the term Latino to refer to people classified or re-classified as Hispanic.
Other subject characteristics included in our multivariate model were two demographic variables (age and sex) and four dichotomous measures of need for health services. Need variables were three measures of comorbidity (psychiatric, medical, and SUD) and a social security insurance (SSI) eligibility indicator variable—included because SSI eligibility suggests a more chronic and disabling illness.
The comorbidity measures included conditions whose co-occurrence with a schizophrenia diagnosis may affect the course or management of schizophrenia and as result, increase patients' use of mental or general health services. Psychiatric comorbidity was coded as present if we observed at least two claims recorded on two different service dates with an ICD-9 diagnosis of psychiatric disorders such as major depression, dysthymia, panic disorder, obsessive-compulsive disorder, and specific personality disorders. Medical comorbidity was coded as present if we observed at least one claim with an ICD-9 diagnosis of qualifying medical conditions. Cardiovascular and cerebrovascular disorders; hepatic disorders; hypertension; diabetes, hyperlipidemia, and obesity; and chronic viral infections were among the conditions included in this variable. SUD was coded as present if we observed at least one claim with an ICD-9 diagnosis of abuse of drugs other than tobacco or of alcohol and drug dependence. ICD-9 codes used are available from the authors upon request. The SSI indicator variable was coded as “yes” if we observed a plurality of months during the FY where eligibility was tied to SSI versus other benefit mechanisms.
Statistical Analyses
Our unit of observation was the person-FY. We used a generalized estimating equation approach to account for the clustering and autocorrelation inherent in these longitudinal data (Zeger and Liang 1986). We used a two-part model to analyze the highly skewed inpatient utilization data, an approach that first models the likelihood of using any psychiatric inpatient services and subsequently models levels of spending among users (Duan et al. 1983). We evaluated time trends by interacting race/ethnicity with FY, a linear time variable.
We computed percent differences (Δ) in spending levels and likelihood of use between blacks or Latinos and whites as ((exponentiated β) minus 1)*100, where β is the coefficient for blacks or Latinos. For the parametric trend analyses, we computed minority-white percent differences (Δ) in rates of change over time as β*100, where β is the coefficient for the interaction between blacks or Latinos and the continuous time variable (FY).
Our empirical model included demographic and need variables. We evaluated if estimates of disparities in spending levels or likelihood of use differed according to SUD comorbidity status by including an interaction term for race/ethnicity and SUD comorbidity.
We used a critical value of 0.05 to evaluate statistical significance.
RESULTS
Sociodemographic and Clinical Characteristics of the Racial/Ethnic Groups
We observed the care received by at least 10,000 Medicaid recipients each year, for a total of 143,856 person years during the period July 1994–June 2006. Our sample included 26 percent blacks, 33 percent Latinos, and 41 percent whites. Table 1 shows that the three racial/ethnic groups differed with regard to all the variables included in our multivariate models. We note here that blacks had less psychiatric comorbidity, but they had more SUD comorbidity than their peers. For their part, Latinos had more medical comorbidity than their peers.
Table 1.
Sample Characteristics, by Racial/Ethnic Group: Demographic, Need, and Geographic Variables
| Variable | All | Blacks | Latinos | Whites | p Value |
|---|---|---|---|---|---|
| Age, mean | 43.4 | 41.6 | 44.5 | 43.7 | <.0001 |
| Female (%) | 51.8 | 49.9 | 55.9 | 49.7 | <.0001 |
| Any psychiatric comorbidity (%) | 21.6 | 16.3 | 24.0 | 23.1 | <.0001 |
| Any SUD comorbidity (%) | 12.9 | 15.2 | 11.4 | 12.7 | <.0001 |
| Any medical comorbidity (%) | 57.7 | 54.6 | 65.1 | 53.7 | <.0001 |
| SSI (%) | 93.7 | 95.5 | 94.7 | 91.8 | <.0001 |
| Total person years (%) | 143,856 (100.0) | 37,668 (26.2) | 47,020 (32.7) | 59,168 (41.1) |
Spending Patterns
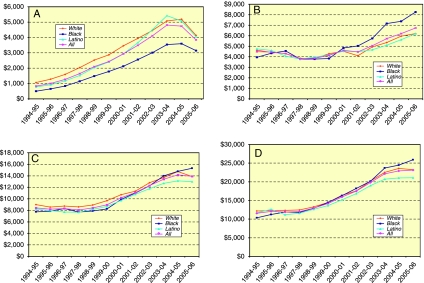
For all outcome measures, mean annual spending grew steadily over the study period, peaking at or near study end (Figure 1A–D).
Figure 1.
Unadjusted Mean Annual Spending by Race/Ethnicity and for All (FY 1995–2006). (A) Psychotropic Drugs. (B) Psychiatric Inpatient. (C) Total Mental Health. (D) Total Health
Unadjusted Results: Spending Differences
Blacks had lower mean annual psychotropic drug spending than whites throughout the entire period (Figure 1A). Mean annual psychiatric inpatient spending was comparable for blacks and whites between FY 1996 and FY 2001, yet blacks outspent whites in the latter part of the study period (Figure 1B). While at the beginning of the study period total mental health and total health spending were lower for blacks than whites, eventually blacks overtook whites (Figure 1C and D). For their part, Latinos tended to have mostly similar or slightly lower spending than whites in all categories (Figure 1A–D).
Results from Multivariate Analyses: Spending Disparities
Table 2A shows that after adjusting for demographic and need variables, minority-white spending differences (Δ) on psychotropic drugs, total mental health services, and total health services were negative and statistically significant. Across these outcomes, blacks and Latinos had between 0.9 and 70 percent lower spending levels than whites. The largest disparities were for psychotropic drug spending: the size of the disparity was 70 percent for blacks and whites with SUD comorbidity, and 26 percent for Latinos and whites without SUD comorbidity. With only one exception (psychotropic drug spending by blacks and whites), disparities were larger among people without SUD comorbidity than among people with SUD comorbidity.
Table 2.
Disparities Analyses (FY 1995–2006): Percent Difference (Δ) in Spending or Likelihood of Use, Blacks or Latinos versus Whites, Stratified by SUD Comorbidity Status
| Psychotropic Drugs |
Total Mental Health |
Total Health |
||||
|---|---|---|---|---|---|---|
| Group by SUD Comorbidity Status | Δ | β | Δ | β | Δ | β |
| A. Psychotropic drugs, total mental health, and total health: levels of spending | ||||||
| Blacks | ||||||
| Without SUD | −67** | −1.114 | −24** | −0.276 | −19** | −0.206 |
| With SUD | −70** | −1.203 | −1** | −0.009 | −2** | −0.020 |
| Latinos | ||||||
| Without SUD | −26** | −0.303 | −26** | −0.301 | −13** | −0.140 |
| With SUD | −20** | −0.218 | −17** | −0.189 | −7** | −0.067 |
| Likelihood of Use |
Levels of Spending |
|||||
| Group by SUD Comorbidity Status | Δ | β | Δ | β | ||
| B. Inpatient psychiatric: likelihood of use and levels of spending among users | ||||||
| Blacks | ||||||
| Without SUD | −11* | −0.121 | −1 | −0.014† | ||
| With SUD | +18** | +0.168 | −1 | −0.014† | ||
| Latinos | ||||||
| Without SUD | −18** | −0.195† | +1 | +0.013† | ||
| With SUD | −18** | −0.195† | +1 | +0.013† | ||
p value .000.
p value <.01.
SUD comorbidity does not moderate race effect (Race*SUD interaction term is not significant).
A less straightforward picture emerged from the two-part model for psychiatric inpatient services (Table 2B). Relative to whites, likelihood of use of these services was 11 percent lower for blacks without SUD comorbidity and 18 percent lower for Latinos with or without SUD comorbidity. However, likelihood of use was 18 percent higher for blacks with SUD comorbidity than for their white peers. Further, among psychiatric inpatient users (n=45,183 or 31 percent of our sample), spending did not differ by race/ethnicity.
Trend Analyses: Disparities Over Time
Table 3A shows that after adjusting for demographic and need variables, some but not all minority-white differences (Δ) in rates of change in psychotropic drug, total mental health, and total health spending were positive and statistically significant. In other words, growth in spending was either comparable across racial/ethnic groups or it was slightly larger for blacks or Latinos relative to whites. Growth in psychotropic drug spending was larger for blacks and Latinos than for whites: relative to whites, annual growth in spending was 3.4 percent higher for blacks and 2.5 percent higher for Latinos. Annual growth in total mental health spending was comparable for blacks and whites yet Latinos outpaced whites at a rate of 1.5 percent per year. Annual growth in total health spending was comparable for Latinos and whites yet blacks outpaced whites at a rate of 0.8 percent per year. Where they existed, the small differences in annual growth of spending favoring blacks or Latinos were not sufficient to eradicate the 12-year spending disparities described above.
Table 3.
Trends in Disparities: Percent Difference (Δ) in Rates of Change in Spending or Likelihood of Use over the Study Period (FY 1995–2006), Blacks or Latinos versus Whites
| Psychotropic Drugs |
Total Mental Health |
Total Health |
||||
|---|---|---|---|---|---|---|
| Group | Δ | β | Δ | β | Δ | β |
| A. Psychotropic drugs, total mental health, and total health: levels of spending | ||||||
| Blacks | +3.4** | +0.034 | +0.1 | +0.001 | +0.8* | +0.008 |
| Latinos | +2.5** | +0.025 | +1.5** | +0.015 | +0.3 | +0.003 |
| Likelihood of Use |
Levels of Spending |
|||||
| Group | Δ | β | Δ | β | ||
| B. Psychiatric inpatient services: likelihood of use and levels of spending among users | ||||||
| Blacks | +1.9** | +0.019 | +1.8** | +0.018 | ||
| Latinos | −0.4 | −0.004 | +0.2 | +0.002 | ||
p value <.01.
p value .000.
Minority-white differences (Δ) in rates of change in use/spending of psychiatric inpatient services were observed only for blacks and whites, with blacks outpacing whites in both outcomes (Table 3B). Annual growth in the likelihood of use of psychiatric inpatient services was 1.9 percent higher for blacks. Among users of these services, annual growth in spending was 1.8 percent higher for blacks.
DISCUSSION
Black and Latino Medicaid recipients diagnosed with schizophrenia experienced health care disparities during the 12-year study period. Our findings confirm the hypothesis that spending on psychotropic drugs is lower for minorities than for whites, a problematic result given that high-quality schizophrenia care rests on the appropriate and sustained use of one or more classes of psychotropic drugs (Lehman et al. 2004a,b;). Drug spending disparities were substantial, particularly for blacks. Although our findings indicate that relative to whites, blacks with SUD comorbidity had a higher likelihood of using psychiatric inpatient services, likelihood of psychiatric inpatient use was lower for blacks without SUD comorbidity and for all Latinos. Further, conditional on use, minority and white recipients had similar psychiatric inpatient spending, another result that runs counter to the inpatient-related study hypothesis. Given these findings, we were not surprised to find disparities in total mental health and total health spending. With the sole exception of spending on psychotropic drugs by blacks and whites, disparities were larger for people without SUD comorbidity.
Our drug spending disparity findings are consistent with studies of populations with other health and mental health conditions (Han and Liu 2005; Gaskin et al. 2006; Wang et al. 2006; Alegria et al. 2008;). These findings are also consistent with evidence of racial/ethnic disparities in the use of psychotropic drugs employed in the care of schizophrenia, including clozapine, other atypical antipsychotics, and adjunctive medications such as antidepressants and lithium (Lehman, Steinwachs, and Project 1998; Kuno and Rothbard 2002; West et al. 2005;). Because atypical agents account for a large fraction of Medicaid pharmacy spending, disparities in the use of these medications —prescribed at least once to two-thirds of our sample, are likely to be a major contributor to our psychotropic drug results (Huskamp 2006). It may be argued that psychotropic drug spending disparities that are largely driven by a lower use of atypical antipychotics among minorities should not cause concern because many observers no longer consider use of atypical agents necessary for high-quality schizophrenia care (Carpenter and Buchanan 2008). Although the lower use of atypicals in the care of minorities may have had far less negative consequences than initially thought, our disparities findings should be interpreted in light of what was considered high-quality care during the study period (McEvoy, Scheifler, and Frances 1999). Because the federal warning on atypical antipsychotics' health risks as well as compelling evidence of comparable effectiveness for conventional and non-clozapine atypical antipsychotics were made public in 2003 and later, it is safe to assume that atypical agents were considered the antipsychotics of choice during most if not all our study period. Our finding of a black–white psychotropic drug spending disparity is not at odds with previous evidence that use of conventional long-acting injectable antipsychotics is higher for blacks than whites because these particular agents are inexpensive and infrequently used in the United States (Kreyenbuhl et al. 2003).
We note that although psychotropic drugs are a critical component of high-quality schizophrenia care, higher psychotropic drug spending may not necessarily indicate higher quality of care. For example, use of high doses of antipsychotic drugs and use of more than one antipsychotic agent (antipsychotic polypharmacy) are empirically unsupported practices that drive up costs yet undermine quality (Taylor 2002; Rupnow et al. 2005). While high antipsychotic dosing is more frequent among blacks than whites, limited evidence suggests that antipsychotic polypharmacy may be slightly less frequent among blacks than whites (Leslie and Rosenheck 2004; Kreyenbuhl et al. 2007;). Although the evidence base is far smaller for Latinos, it appears that both practices are less frequent among them (Covell et al. 2002). Hence, we cannot rule out that our psychotropic drug spending disparity findings may have been driven by a lower frequency of 1 or more low-value practices among minorities.
Our finding that the likelihood of use of psychiatric inpatient services is higher only for blacks with SUD comorbidity than for their white peers, and that it is lower for blacks without SUD comorbidity and all Latinos regardless of SUD comorbidity status, is new to the literature. Although several studies have investigated racial/ethnic differences in the use of psychiatric inpatient services, only one study employed a sample entirely comprised of black and white Medicaid recipients with a schizophrenia diagnosis and no study has evaluated the effect-modifying role of SUD comorbidity (Padgett et al. 1994; Kuno and Rothbard 2002;).
Are Disparities Narrowing over Time?
Out trend results indicate that psychotropic drug spending disparities narrowed for blacks and Latinos, total mental health spending disparities narrowed for Latinos, and total health spending disparities narrowed for blacks. Thus, we found partial support for the trend-related study hypothesis. Differential growth in spending favoring minorities was not large enough to bring minority spending levels at par with white spending levels for the 12-year period observed by our study. We note that with the exception of psychotropic drugs, our adjusted longitudinal disparity findings are generally consistent with the unadjusted spending curves for minorities and whites presented in Figure 1 (A–D).
Although we do not have a cogent explanation for these trend results, policy changes instituted toward the end of the study period could bear some responsibility. For example, the Florida Medicaid program instituted a prior authorization requirement for olanzapine, a frequently used atypical antipsychotic, in the summer of 2005 (Becker et al. 2008). However, the timing of this policy change makes it an implausible explanation for our trend results (see Figure 1A).
Unlike most ambulatory services, a racial/ethnic disparity with regard to psychiatric inpatient services is defined by minorities using more of these services than whites. It is therefore puzzling that in the context of unchanging or narrowing disparities for the other study outcomes, blacks had a larger rate of change than whites in the likelihood of use of psychiatric inpatient services and in spending levels among users. We do not know what caused these trends but we speculate that poorer quality of care and other factors associated with use of psychiatric inpatient services may have had a growing differential impact on blacks relative to whites over the course of the study period.
LIMITATIONS
Our study has a number of limitations. First, because our study was based on administrative data, the method used to build a cohort with schizophrenia may not have had 100 percent sensitivity and specificity for the diagnosis. Second, because of the nonexperimental nature of our study design, our study may not have compared racial/ethnic groups that were entirely balanced with regard to need. Third, the generalizability of our study is limited by our data being administrative claims data from Florida, a state that differs from many others in the United States because of its racial/ethnic diversity and its restrictive requirements for Medicaid eligibility. Fourth, because we compared groups based on their actual use and spending, it is possible that some of our findings may have been unduly influenced by differential adherence behavior across the groups. Although some evidence suggests that minorities with schizophrenia are less adherent to medications than whites, we are unable to assess the extent to which this factor may have contributed to our findings (Gilmer et al. 2004). Lastly, we were unable to meaningfully assess whether our disparity findings could be attributed to geographic variations in quality of care (Baicker, Chandra, and Skinner 2005).
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Alegria M, Chatterji P, Wells K, Cao Z, Chen C-n, Takeuchi D, Jackson J, Meng X-L. Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States. Psychiatric Services. 2008;59(11):1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner JS. Geographic Variation in Health Care and the Problem of Measuring Racial Disparities. Perspectives in Biology and Medicine. 2005;48(1 suppl.):S42–53. [PubMed] [Google Scholar]
- Barrio C, Yamada AM, Hough RL, Hawthorne W, Garcia P, Jeste DV. Ethnic Disparities in Use of Public Mental Health Case Management Services among Patients with Schizophrenia. Psychiatric Services. 2003;54(9):1264–70. doi: 10.1176/appi.ps.54.9.1264. [DOI] [PubMed] [Google Scholar]
- Becker M, Constantine R, Robst J, Boaz T, Andel R. “The Relationship between Patient Characteristics and Discontinuance of Olanzapine Following a New Prior Authorization Requirement in Florida's Medicaid Program.”American Public Health Association, Annual Meeting, San Diego, CA.
- Brady J, Ho K, Kelley E, Clancy CM. AHRQs National Healthcare Quality and Disparities Reports: An Ever-Expanding Road Map for Improvement. Health Services Research. 2007;42(3p1):xi–xxi. doi: 10.1111/j.1475-6773.2007.00736.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresnahan M, Begg MD, Brown A, Schaefer C, Sohler N, Insel B, Vella L, Susser E. Race and Risk of Schizophrenia in a US Birth Cohort: Another Example of Health Disparity? International Journal of Epidemiology. 2007;36(4):751–8. doi: 10.1093/ije/dym041. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Buchanan RW. Lessons to Take Home from CATIE. Psychiatric Services. 2008;59(5):523–5. doi: 10.1176/ps.2008.59.5.523. [DOI] [PubMed] [Google Scholar]
- Cook BL, McGuire T, Miranda J. Measuring Trends in Mental Health Care Disparities, 2000–2004. Psychiatric Services. 2007;58(12):1533–40. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Covell NH, Jackson CT, Evans AC, Essock SM. Antipsychotic Prescribing Practices in Connecticut's Public Mental Health System: Rates of Changing Medications and Prescribing Styles. Schizophrenia Bulletin. 2002;28:17–29. doi: 10.1093/oxfordjournals.schbul.a006920. [DOI] [PubMed] [Google Scholar]
- Dassori AM, Miller AL, Saldana D. Schizophrenia among Hispanics: Epidemiology, Phenomenology, Course, and Outcome. Schizophrenia Bulletin. 1995;21(2):303–12. doi: 10.1093/schbul/21.2.303. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Crum RM, Guallar E, Powe NR, Primm AB, Steinwachs DM, Ford DE. Outpatient Prescriptions for Atypical Antipsychotics for African Americans, Hispanics, and Whites in the United States. Archives of General Psychiatry. 2003;60(2):121–8. doi: 10.1001/archpsyc.60.2.121. [DOI] [PubMed] [Google Scholar]
- dosReis S, Johnson E, Steinwachs D, Rohde C, Skinner EA, Fahey M, Lehman AF. Antipsychotic Treatment Patterns and Hospitalizations among Adults with Schizophrenia. Schizophrenia Research. 2008;101(1–3):304–11. doi: 10.1016/j.schres.2007.12.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan N, Manning WG, Morris CN, Newhouse JP. A Comparison of Alternative Models for the Demand for Medical Care. Journal of Business and Economic Statistics. 1983;1(2):115–26. [Google Scholar]
- Frank RG, Glied SA. Better but Not Well: Mental Health Policy in the U.S. since 1950. Baltimore: Johns Hopkins University Press; 2006. [Google Scholar]
- Gaskin DJ, Briesacher BA, Limcangco R, Brigantti BL. Exploring Racial and Ethnic Disparities in Prescription Drug Spending and Use among Medicare Beneficiaries. American Journal of Geriatric Pharmacotherapy. 2006;4(2):96–111. doi: 10.1016/j.amjopharm.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, Jeste DV. Adherence to Treatment with Antipsychotic Medication and Health Care Costs among Medicaid Beneficiaries with Schizophrenia. American Journal of Psychiatry. 2004;161(4):692–99. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- Han E, Liu GG. Racial Disparities in Prescription Drug Use for Mental Illness among Population in US. Journal of Mental Health Policy and Economics. 2005;8(3):131–43. [PubMed] [Google Scholar]
- Huskamp HA. Prices, Profits, and Innovation: Examining Criticisms of New Psychotropic Drugs' Value. Health Affairs. 2006;25(3):635–46. doi: 10.1377/hlthaff.25.3.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karno M, Hough RL, Burnam MA, Escobar JI, Timbers DM, Santana F, Boyd JH. Lifetime Prevalence of Specific Psychiatric Disorders among Mexican Americans and Non-Hispanic Whites in Los Angeles. Archives of General Psychiatry. 1987;44(8):695–701. doi: 10.1001/archpsyc.1987.01800200021004. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime Prevalence, Demographic Risk Factors, and Diagnostic Validity of Nonaffective Psychosis as Assessed in a US Community Sample. The National Comorbidity Survey. Archives of General Psychiatry. 1996;53(11):1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Zito JM, Buchanan RW, Soeken KL, Lehman AF. Racial Disparity in the Pharmacological Management of Schizophrenia. Schizophrenia Bulletin. 2003;29(2):183–94. doi: 10.1093/oxfordjournals.schbul.a006996. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl JA, Valenstein M, McCarthy JF, Ganoczy D, Blow FC. Long-Term Antipsychotic Polypharmacy in the VA Health System: Patient Characteristics and Treatment Patterns. Psychiatric Services. 2007;58(4):489–95. doi: 10.1176/appi.ps.58.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuno E, Rothbard AB. Racial Disparities in Antipsychotic Prescription Patterns for Patients with Schizophrenia. American Journal of Psychiatry. 2002;159(4):567–72. doi: 10.1176/appi.ajp.159.4.567. [DOI] [PubMed] [Google Scholar]
- Lehman AF. Quality of Care in Mental Health: The Case of Schizophrenia. Health Affairs. 1999;18(5):52–65. doi: 10.1377/hlthaff.18.5.52. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB, Goldberg R, Green-Paden LD, Tenhula WN, Boerescu D, Tek C, Sandson N, Steinwachs DM. The Schizophrenia Patient Outcomes Research Team (PORT): Updated Treatment Recommendations 2003. Schizophrenia Bulletin. 2004a;30(2):193–217. doi: 10.1093/oxfordjournals.schbul.a007071. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, Kreyenbuhl J American Psychiatric Association, and Steering Committee on Practice Group. Practice Guideline for the Treatment of Patients with Schizophrenia, Second Edition. American Journal of Psychiatry. 2004b;161(2 Suppl):1–56. [PubMed] [Google Scholar]
- Lehman AF, Steinwachs DM Survey Co-Investigators of the Port Project. Patterns of Usual Care for Schizophrenia: Initial Results from the Schizophrenia Patient Outcomes Research Team (PORT) Client Survey. Schizophrenia Bulletin. 1998;24(1):11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- Leslie DL, Rosenheck RA. Adherence of Schizophrenia Pharmacotherapy to Published Treatment Recommendations: Patient, Facility, and Provider Predictors. Schizophrenia Bulletin. 2004;30(3):649–58. doi: 10.1093/oxfordjournals.schbul.a007112. [DOI] [PubMed] [Google Scholar]
- McEvoy JP, Scheifler PL, Frances A. The Expert Consensus Guidelines Series: Treatment of Schizophrenia. Journal of Clinical Psychiatry. 1999;60(Suppl 11):1–80. [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. The Global Burden of Disease. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, Schlesinger HJ. Ethnic Differences in Use of Inpatient Mental Health Services by Blacks, Whites, and Hispanics in a National Insured Population. Health Services Research. 1994;29(2):135–53. [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Regier DA. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York: Free Press; 1991. [Google Scholar]
- Rupnow MF, Greenspan A, Gharabawi GM, Kosik-Gonzalez C, Zhu Y, Stahl SM. Incidence and Costs of Polypharmacy: Data from a Randomized Double-Blind, Placebo-Controlled Study of Risperidone and Quetiapine in Patients with Schizophrenia or Schizoaffective Disorder. Current Medical Research and Opinion. 2007;23(11):2815–22. doi: 10.1185/030079907x233359. [DOI] [PubMed] [Google Scholar]
- Saha S, Chant D, Welham J, McGrath J. A Systematic Review of the Prevalence of Schizophrenia. PLoS Medicine. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- Snowden LR, Holschuh J. Ethnic Differences in Emergency Psychiatric Care and Hospitalization in a Program for the Severely Mentally Ill. Community Mental Health Journal. 1992;28(4):281–91. doi: 10.1007/BF00755795. [DOI] [PubMed] [Google Scholar]
- Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and Ethnic Disparities in Detection and Treatment of Depression and Anxiety among Psychiatric and Primary Health Care Visits, 1995–2005. Medical Care. 2008;46(7):668–77. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor D. Antipsychotic Prescribing—Time to Review Practice. Psychiatric Bulletin. 2002;26(11):401–2. [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the Quality of Care and Racial Disparities in Medicare Managed Care. New England Journal of Medicine. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- USBLS. “Consumer Price Indexes, Databases” [accessed on September 1, 2008]. Available at http://www.bls.gov/CPI/
- Vega WA, Karno M, Alegria M, Alvidrez J, Bernal G, Escamilla M, Escobar J, Guarnaccia P, Jenkins J, Kopelowicz A, Lagomasino IT, Lewis-Fernandez R, Marin H, Lopez S, Loue S. Research Issues for Improving Treatment of U.S. Hispanics with Persistent Mental Disorders. Psychiatric Services. 2007;58(3):385–94. doi: 10.1176/ps.2007.58.3.385. [DOI] [PubMed] [Google Scholar]
- Wang J, Noel JM, Zuckerman IH, Miller NA, Shaya FT, Mullins CD. Disparities in Access to Essential New Prescription Drugs between Non-Hispanic Whites, Non-Hispanic Blacks, and Hispanic Whites. Medical Care Research and Review. 2006;63(6):742–63. doi: 10.1177/1077558706293638. [DOI] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of Treatment for Serious Mental Illness in the United States. American Journal of Public Health. 2002;92(1):92–8. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiden PJ, Kozma C, Grogg A, Locklear J. Partial Compliance and Risk of Rehospitalization among California Medicaid Patients with Schizophrenia. Psychiatric Services. 2004;55(8):886–91. doi: 10.1176/appi.ps.55.8.886. [DOI] [PubMed] [Google Scholar]
- West JC, Wilk JE, Olfson M, Rae DS, Marcus S, Narrow WE, Pincus HA, Regier DA. Patterns and Quality of Treatment for Patients with Schizophrenia in Routine Psychiatric Practice. Psychiatric Services. 2005;56(3):283–91. doi: 10.1176/appi.ps.56.3.283. [DOI] [PubMed] [Google Scholar]
- Williams DR, Earl TR. Commentary: Race and Mental Health–More Questions Than Answers. International Journal of Epidemiology. 2007;36(4):758–60. doi: 10.1093/ije/dym114. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal Data Analysis for Discrete and Continuous Outcomes. Biometrics. 1986;42(1):121–30. [PubMed] [Google Scholar]
- Zuvekas SH. Prescription Drugs and the Changing Patterns of Treatment for Mental Disorders, 1996–2001. Health Affairs. 2005;24(1):195–205. doi: 10.1377/hlthaff.24.1.195. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.