Abstract
Objective
To examine if a minimum efficient scale (MES) holds with respect to the population serviced by a local health department (LHD) given the congestability, externality, and scale/scope economy effects potentially associated with public health services.
Data Sources/Study Setting
A nationally representative sample of LHDs in 2005.
Study Design
Multiple regression analysis is used to isolate the relation between population and spending while controlling for other factors known to influence local public health costs.
Data Collection
Data were obtained from the 2005 National Profile of Local Public Health Agencies, a project supported through a cooperative agreement between the National Association of County and City Health Officials and the Centers for Disease Control and Prevention.
Principal Findings
The MES of a local public health department is approximately 100,000 people. After that size, additional population has little impact on public health spending per capita.
Conclusions
Seventy-seven percent of LHDs in the sample fall below the 100,000 MES. Higher levels of government may want to provide financial inducements so that smaller LHDs consolidate or enter into agreements with larger public health organizations to provide services.
Keywords: Public health services, costs of production, economies of scale
Public health services refer to the actions taken by society to advance the health of the general population. Spending on public health services in the United States amounted to roughly US$64 billion in 2007 (Hartman et al. 2009). While the precise mix of services differs across health departments, most local public health spending funds the surveillance and prevention of communicable diseases, testing and preservation of water quality, maintenance of sanitary conditions (e.g., approval of septic systems), ensuring of food protection (restaurant inspections), and the providing of health information (National Association of County and City Health Officers [NACCHO] 2006).
Relatively little is known about the determinants of public health expenditures probably because that spending only accounts for <3 percent of all health care costs (Hartman et al. 2009). However, many experts predict a more important role for public health in the future given the threat of bioterrorism attacks, concerns over emerging diseases such as avian flu and SARS, and the seemingly growing burden from natural disasters such as Katrina (Tilson and Berkowitz 2006).1 If so, a better understanding of public health spending variations may prove useful to public health policy makers.
This paper focuses directly on the relation between jurisdiction size, in terms of population, and local public health spending. Theoretically, a fairly complex relation exists between these two variables because of the congestability, externality, and scale and scope economy effects potentially associated with public health services as discussed in the next section. Consequently, this paper uses a nationally representative sample of local health departments (LHDs) during 2005 to investigate empirically the relation between population size and local public health spending. The results suggest that the minimum efficient scale (MES) for the representative LHD occurs at a population of approximately 100,000.
THEORETICAL RELATION BETWEEN POPULATION AND PUBLIC HEALTH SPENDING
The relation between population size and local public health spending depends on several conditions. First, public finance economists have long noted that collectively provided goods like public health may exhibit nonrivalry in consumption (e.g., Borcherding and Deacon 1972; Bergstrom and Goodman 1973;). Nonrivalry in consumption holds when one person's enjoyment of a good does not detract from another person receiving enjoyment from that same good. Nonrivalry can be conceptualized mathematically in the following way:
| (1) |
In equation (1), Q represents the total amount of the collectively provided good, N stands for the population in the jurisdiction, and α reflects the degree of congestability.
If α=0, then everyone benefits from the entire amount of the collectively provided good so that Q represents a pure public good. If, however, α=1, then each person receives only 1/Nth of the good so that Q represents a private good. Intermediate cases can also arise (0<α<1) so that Q reflects a quasi-public good. A more complex version of equation (1) allows for a variable congestability parameter with α increasing with population size, or
| (2) |
It follows that the effect of population on public health spending depends, in part, on the congestability of public health services. If local public health decision makers target a particular level of captured units, q, for each person in the jurisdiction and Q represents a private good in consumption, then more resources and spending on public health services are necessary, ceteris paribus. Conversely, lower levels of resources and public health spending are necessary for a targeted q if public health more closely resembles a pure public good.
Given local public health services such as disease surveillance, communicable disease immunizations, restaurant inspections, and water quality control, one would think that public health resembles a pure public good. To date, only Borcherding and Deacon (1972) and Santerre (1985) have estimated the congestability parameter for local public health services. Both studies find that local public health services are highly congestable with α equaling 0.983 on average. However, these two studies include acute care services produced in government-owned hospitals in their measure of public health activities, and so the estimated congestability parameters may be biased upward (Bates and Santerre 2008).
Second, the effect of population on spending depends on whether any externalities hold with respect to public health services. Externalities occur when actions taken by producers or consumers positively or negatively affect others not directly involved in the market transaction and these side effects remain unpriced (Carande-Kulis, Getzen, and Thacker 2007). In the context of public health, cigarette smoking offers a prime example of a negative externality in consumption because of secondary smoke hazards. Unsafe sexual practices provide another example particularly because diseases such as the HIV and AIDS can widely transmit to others. Public health officials often attempt to counteract these and other types of negative externalities through various services such as tobacco cessation counseling and free condom distribution. Moreover, some local public health services such as immunizations for infectious disease control and epidemiological investigations directly yield positive externalities. The magnitude of the externalities depends on whether the external effects rise, fall, or remain constant with respect to a larger population size.2
Finally, the relation between population size and public health spending may be influenced by whether scale and scope economies hold in production. Scale economies exist when per unit costs of production decline with increasing amounts of output and result from labor and capital specialization and the spreading of fixed costs. Rising per unit costs with respect to the quantity of output reflects scale diseconomies, which can result from an organization becoming physically too large such that communication flows break down, bureaucratic inertia sets in, and principal/agent problems develop (Santerre and Neun 2007). In addition to scale economies, costs may decline with population because of scope economies if larger LHDs consolidate a variety of services and thereby reap the benefits of lower costs from joint production. On the other hand, costs could rise if scope diseconomies prevail.
This discussion suggests that the theoretical relation between population size and public health spending is unclear and depends on the net influence of the congestability, externality, and scale and scope economy effects. Thus, empirical studies are needed to sort out the precise relationship, but unfortunately not too many studies exist on this issue.
Borcherding and Deacon (1972) and Santerre (1985) estimate the demand for public health services and find that population has no impact on per capita public health spending using cross-sectional national and Connecticut samples of local governments, respectively. These two studies are suspect, however, because they include the expenditures of government hospitals in their measures of public health spending and do not treat the public health department as the unit of analysis. Nevertheless, Shonick and Price (1978) corroborate their findings when they also observe that the level of population does not affect per capita public health spending when using a national sample of 694 LHDs in 1975.
Also using a demand approach but confining the sample to a set of district health departments in Connecticut, Bates and Santerre (2008) find that a 1 percent increase in population results in a 1.6 percent decline in public health spending per capita. Finally, Gordon, Gerzoff, and Richards (1997), using a nationwide sample of LHDs in 1993, estimate an inverted U-relation between population and per capita public health expenditures. However, these researchers include both population and the number of full-time employees as right-hand-side variables in their estimation equation. Because the delivery of public health services is labor intensive, it remains unclear why public health expenditures would adjust in response to a population change given that their estimation process, by construction, assumes a constant number of full-time employees.
Thus, previous empirical studies tend to be inconclusive about the precise nature of the relation between population and public health spending. Given the importance but limited resources associated with public health activities, finding least-cost methods of organizing services seems a worthwhile venture. Indeed, the Council on Linkages between Academia and Public Health Practice considers cost-effectiveness and questions regarding scale economies as two areas where research is needed (see http://www.phf.org/Link/phsr/agendas.pdf). The next section of this paper uses neoclassical microeconomic theory and a national sample of local public health departments in 2005 to reexamine the empirical relation between population size and public health spending.
DATA AND METHODS
The NACCHO provides the data used in the forthcoming empirical analysis. NACCHO collected the data with a national survey of 2,864 LHDs in 2005 of which 2,300 or 80 percent responded to the questionnaire. The response rate was lowest for LHDs with population under 25,000 (73 percent), around 83 percent for LHDs with population between 25,000 and 74,999, relatively constant at about 90 percent for LHDs with population between 75,000 and 999,999 people, and then 98 percent for LHDs with population over 1 million. Not all LHDs answered every question, however.
Based on fairly solid theory, population can be worked into the empirical analysis in the following manner. According to neoclassical microeconomic theory (e.g., Santerre and Neun 2007), the long-run total costs of an organization, C, can be expressed as a function of the quantity of output produced, Q, and the prices of any inputs employed, P, conditioned upon the state of technology, T, or
| (3) |
Given the service nature of the product, the quantity of public health delivered is not directly observable and measurable. However, the NACCHO survey provides a number of variables that can reasonably serve as proxies by capturing the scale and variety of services offered by the various LHDs.
First, population is specified to reflect the scale or amount of services. Population represents a worthwhile output measure, because as mentioned previously, public health services refer to the actions taken for the health of the community as a whole.3 Indeed, health economists often use patient indicators to reflect output measures of hospital services (e.g., Cowing and Holtmann 1983; Granneman, Brown, and Pauly 1986;). However, not all public health needs may be the same across the various LHDs because of population heterogeneity. Therefore, the racial and ethnic composition of the population served by each LHD is specified in the estimation equation. Second, the amount of public health services may also depend on the compactness of people. In fact, Santerre (1985) argues that many local public health services act as density off-setting goods. Thus, a set of dummy variables is included to control for the urban nature of the jurisdiction (urban, micropolitan, or rural) served by each LHD based on the RUCA taxonomy.
Third, the variety of public health services offered in each LHD is specified in the estimation equation. The NACCHO database lists up to 95 different public health services and identifies if the LHD provides or contracts out for each service and if that same service is provided by state, other local, or nongovernmental agencies. Given that each type of service may be partially offered by each of the five parties, the maximum number of services can range up to 475. The percentage of services contracted out and the percentage from parties other than the LHD are included as two additional variables in the estimation equations. One would expect that operating costs rise with a greater variety of services but decline with a greater proportion of services contracted out or produced outside the LHD, particularly if the latter comes at no expense to the LHD.
Experimentation showed that the percentage of services that are medical or clinical in nature (i.e., immunizations, screening for diseases, treatment for communicable diseases, maternal and child health, and other health services) has a direct effect on costs, and so this ratio also appears in the empirical model. Clinical services, other than immunizations for infectious diseases, may be costly because they more closely resemble pure private goods with little public spillover effects. Lastly, the percentages of revenues funded by various third parties (e.g., state, federal, Medicaid, Medicare, and private) are specified as additional explanatory variables. The mix of funding sources may mirror the extent to which particular services are offered by the various LHDs. For example, a greater mix of Medicaid and Medicare funding may reflect more services aimed at low-income and elderly individuals in a jurisdiction. In addition, the percentages of revenues from Medicare, Medicaid, and private insurance may provide another indicator of a health department's orientation toward clinical rather than population-based services, which are more costly to produce because of their highly congestible nature.4
Direct measures of input prices, the second determinant of costs in equation (3), are not available from the NACCHO survey.5 However, the absence of direct price information may be unimportant for the following reason. A cross-sectional study, like that conducted here, is considered a long-run analysis because sufficient time is assumed for all changes to completely adjust. In competitive input markets, perfect mobility of resources ensures that only one price exists for an input in the long run. Otherwise, the movement of inputs continues until price differentials are driven away. In this context, minimum wage laws, occupational licensing, and other state mandates and regulations, which act as mobility barriers, provide the only major reason why price differentials for the same input can exist in the long run. As a result, state-fixed effects are specified in the estimation equation to control for possible long-run input price differentials as well as any other cost differentials because of varying state public health laws and regulations.
As a reflection of technology, dummy variables are included to control for the type of jurisdiction served by each LHD (i.e., town/township, city, county, city/county, district/regional, or other). The degree of centralization may influence the efficiency at which public health services are delivered. For example, the Tiebout (1956) theory argues that decentralization promotes efficiency. Oppositely, centralization could favor coordination and thereby enhance the efficiency of public health delivery.
Equation (3) is assumed to take the following specific form for estimation purposes:
| (4) |
where C stands for total public health costs, N captures population, X represents the vector of control variables such as the variety of services offered, the βj's and λi's are the parameters to be estimated, and μ is the typical disturbance term. For several reasons, total costs and population are converted by taking the natural logarithms of their actual values. First, taking the log of a variable typically transforms an otherwise skewed variable into a more normally distributed one, which is a desirable property for estimation purposes. Both costs and population are skewed to the left because the sample contains a relatively large number of small jurisdictions with low expenditure levels.
Second, a log transformation of the two variables means that all of the variables in the final estimation equation are either in ratio or binary form (after also taking the log of total services). Lastly, because of the log transformation, the first derivative of ln C with respect to ln N equals β1. This coefficient represents the elasticity of total costs with respect to population or the percentage change in total costs resulting from a 1 percent change in population. For example, if β1=1, then both population and public health costs rise proportionately so that per capita costs remain constant.
EMPIRICAL RESULTS
Table 1 offers a glimpse at the characteristics of the LHDs in the sample. Population averages 131,000 and ranges from a low of 313 to nearly 10 million people. The mean value of per capita local public health spending equals US$45 but varies widely from 39 cents to US$4,249 (not shown). About 86 different services, on average, are provided either internally by the typical LHD, through contracting out, or by state, other local government, or nongovernmental agencies. Agencies other than the LHD offer a large percentage of the services. One-third of all public health services are clinical in nature. Most LHDs are organized on a county basis and are just about evenly split between urban and rural locations. Not surprisingly, most funding for the LHDs comes from government sources.
Table 1.
Descriptive Statistics
| Number of Observations | Mean | Standard Deviation | Minimum Value | Maximum Value | |
|---|---|---|---|---|---|
| Total costs (US$) | 2,021 | 6,864,566 | 45,065,008 | 1,200 | 1.54E+09 |
| Population | 2,296 | 130,999 | 426,430 | 313 | 9,998,371 |
| % LHDs with <25,000 people | 2,296 | 0.406 | 0.491 | 0 | 1 |
| % LHDs with 25,000–49,999 people | 2,296 | 0.214 | 0.410 | 0 | 1 |
| % LHDs with 50,000–99,999 people | 2,296 | 0.151 | 0.358 | 0 | 1 |
| % LHDs with 100,000–249,999 people | 2,296 | 0.122 | 0.328 | 0 | 1 |
| % LHDs with 250,000–499,999 people | 2,296 | 0.052 | 0.222 | 0 | 1 |
| % LHDs with 500,000–999,999 people | 2,296 | 0.034 | 0.182 | 0 | 1 |
| % LHDs with 1,000,000+people | 2,296 | 0.021 | 0.143 | 0 | 1 |
| Total service offerings | 2,003 | 86.37 | 26.00 | 0 | 233 |
| % Clinical services | 2,003 | 0.338 | 0.083 | 0 | 0.960 |
| % Services contracted out | 2,003 | 0.026 | 0.054 | 0 | 0.700 |
| % Services produced by others | 2,003 | 0.620 | 0.148 | 0 | 0.989 |
| % City/town funding | 2,079 | 15.09 | 31.61 | 0 | 100 |
| % County funding | 2,079 | 18.53 | 20.56 | 0 | 100 |
| % State funding | 2,079 | 20.86 | 20.14 | 0 | 100 |
| % Federal funding (e.g., grants) | 2,079 | 19.11 | 18.13 | 0 | 100 |
| % Medicaid funding | 2,079 | 8.16 | 12.43 | 0 | 83 |
| % Medicare funding | 2,079 | 4.12 | 9.83 | 0 | 65 |
| % Private foundation funding | 2,079 | 0.62 | 2.48 | 0 | 40 |
| % Private health insurance funding | 2,079 | 1.02 | 3.10 | 0 | 53 |
| % Patient personal fees | 2,079 | 4.02 | 6.95 | 0 | 85 |
| % Regulatory fees | 2,079 | 4.77 | 11.66 | 0 | 100 |
| % Tribal funding | 2,079 | 0.029 | 0.77 | 0 | 27 |
| % Other funding | 2,079 | 3.67 | 9.61 | 0 | 100 |
| % White | 2,274 | 84.08 | 16.58 | 0 | 100 |
| % Black | 2,274 | 8.12 | 13.44 | 0 | 86 |
| % Asian | 2,274 | 1.62 | 3.14 | 0 | 45 |
| % Hispanic | 2,259 | 6.25 | 10.60 | 0 | 95 |
| % LHDs with city jurisdiction | 2,300 | 0.072 | 0.258 | 0 | 1 |
| % LHDs with county jurisdiction | 2,300 | 0.589 | 0.492 | 0 | 1 |
| % LHDs with city/county jurisdiction | 2,300 | 0.139 | 0.346 | 0 | 1 |
| % LHDs with town/township jurisdiction | 2,300 | 0.088 | 0.283 | 0 | 1 |
| % LHDs with regional jurisdiction | 2,300 | 0.101 | 0.302 | 0 | 1 |
| % LHDs with other jurisdiction | 2,300 | 0.012 | 0.108 | 0 | 1 |
| % LHDs servicing urban areas | 2,298 | 0.403 | 0.491 | 0 | 1 |
| % LHDs servicing micropolitan areas | 2,298 | 0.199 | 0.400 | 0 | 1 |
| % LHDs servicing rural areas | 2,298 | 0.398 | 0.490 | 0 | 1 |
LHD, local health department.
The multiple regression results associated with the estimation of equation (4) are reported in Table 2. Standard errors have been adjusted to account for a heteroskedastic error term. The results for three models are shown. All three models contain state-fixed effects but include different sets of control variables that are added sequentially to determine if the effect of population on public health costs is sensitive to their inclusion. The estimated coefficient and corresponding t-statistic in absolute terms are shown opposite each explanatory variable. For each equation, over 80 percent of the variation in local public health spending around its mean value is collectively explained by the right-hand-side variables.
Table 2.
Basic Multiple Regression Results: Dependent Variable=Log of Total Costs
| Estimated Coefficient (t-Statistic) |
|||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Constant | 4.717 | 2.755 | 2.137 |
| (25.11) | (8.73) | (4.65) | |
| Log of population | 0.904 | 0.825 | 0.845 |
| (52.21) | (46.57) | (35.58) | |
| Log of total service offerings | 0.803 | 0.718 | |
| (11.26) | (9.65) | ||
| % Services contracted out* | −1.262 | −0.648 | |
| (2.71) | (1.30) | ||
| % Services produced by other agencies* | −1.952 | −1.662 | |
| (9.91) | (8.49) | ||
| % Clinical services† | 1.319 | 1.056 | |
| (5.42) | (4.46) | ||
| % County funding† | 0.004 | ||
| (2.60) | |||
| % State funding† | 0.005 | ||
| (2.22) | |||
| % Federal funding† | 0.004 | ||
| (1.99) | |||
| % Medicaid funding† | 0.016 | ||
| (7.16) | |||
| % Medicare funding† | 0.018 | ||
| (7.50) | |||
| % Private foundation funding† | 0.027 | ||
| (5.44) | |||
| % Private health insurance funding† | 0.006 | ||
| (1.08) | |||
| %Patient personal fees† | 0.004 | ||
| (1.60) | |||
| % Regulatory fees† | −0.001 | ||
| (0.22) | |||
| % Tribal funding† | −0.046 | ||
| (3.39) | |||
| % Other funding† | 0.008 | ||
| (3.30) | |||
| % White‡ | 0.002 | ||
| (0.79) | |||
| % Black‡ | 0.009 | ||
| (2.95) | |||
| % Asian‡ | 0.016 | ||
| (1.62) | |||
| % Hispanic‡ | 0.002 | ||
| (0.74) | |||
| LHD with county jurisdiction§ | −0.150 | ||
| (1.39) | |||
| LHD with city/county jurisdiction§ | 0.033 | ||
| (0.29) | |||
| LHD with town/township jurisdiction§ | −0.182 | ||
| (1.51) | |||
| LHD with regional jurisdiction§ | −0.203 | ||
| (1.78) | |||
| LHD with other jurisdiction§ | −0.418 | ||
| (2.68) | |||
| LHD serving micropolitan area¶ | −0.004 | ||
| (0.10) | |||
| LHD serving rural area¶ | 0.059 | ||
| (1.13) | |||
| Adjusted R2 | 0.830 | 0.853 | 0.875 |
| Number of observations | 2,018 | 1,751 | 1,654 |
Notes. All models are specified with a set of 47 state dummy variables for which the results are not shown to save space.
Heteroskedasticity-consistent standard errors are shown in parentheses.
Omitted category is percent of services produced internally.
Omitted category is percent town or city funding.
Omitted category is percent other (e.g., Pacific Islander or non-Hispanic).
Omitted category is city jurisdiction.
Omitted category is urban area.
LHD, local health department.
The empirical findings suggest that the elasticity of total costs with respect to population is <1 for all the three models. This means that local public health costs rise less than proportionately to an increase in population. According to the results, a 10 percent increase in population is associated with an 8–9 percent rise in total public health costs, on average. From a statistical perspective, these population elasticities are highly significant and fairly robust across the three specifications.
The analysis is taken a step further by analyzing whether the population elasticity varies across different population categories as established by NACCHO. The seven population categories are as follows: <25,000, 25,000–49,999, 50,000–99,999, 100,000–249,999, 250,000–499,999, 500,000–999,999, and 1,000,000 and above. Table 1 lists the percentage of LHDs in each of these population categories. To determine whether the population elasticity varies across different population ranges, the log of population is multiplied by a 0/1 dummy variable representing each population range except the default category of under 25,000 people. With this specification, the estimated coefficient on the log of population shows the cost elasticity with respect to population for LHDs with a population below 25,000. The coefficient on each population interaction term measures the incremental effect for that particular population range beyond that of the benchmark population elasticity estimate (i.e., LHDs with <25,000 people).
In addition, multiple regression results are obtained for two restricted samples because some outlier values for public health costs may be driving the empirical findings especially because relatively few LHDs are contained in some of the population categories. Recall that reported per capita costs range from a low of 39 cents to a high of US$4,249. Specifically, the sample is restricted to those LHDs with reported per capita costs between US$1 and US$500 and also to those LHDs with reported per capita spending between US$10 and US$100.
Table 3 reports the findings for the multiple regression equations including population range interaction terms. In all three cases, the results reveal a population elasticity that is <1 and statistically significant for the default population category of <25,000 people. The population elasticity of 0.746–0.789 remains fairly constant until a population of 100,000 is reached. After that point the population elasticity continually increases, rising to a high of 0.789–0.835 in the population category of 1 million or more.6
Table 3.
Multiple Results for Different Population Categories: Dependent Variable=Log of Total Costs
| Estimated Coefficient (t-Statistic) |
|||
|---|---|---|---|
| Full Sample | Reported Per Capita Costs >US$1 and <US$500 | Reported Per Capita Costs >US$10 but <US$100 | |
| Constant | 3.080 | 3.208 | 3.691 |
| (5.27) | (5.79) | (8.03) | |
| Log of population | 0.746 | 0.759 | 0.789 |
| (16.54) | (18.35) | (22.03) | |
| Log of population times population category 25,000–49,999 dummy variable | 0.001 | 0.001 | 0.006 |
| (0.20) | (0.22) | (1.35) | |
| Log of population times population category 50,000–99,999 dummy variable | 0.004 | 0.003 | 0.013 |
| (0.48) | (0.34) | (2.09) | |
| Log of population times population category 100,000–249,999 dummy variable | 0.027 | 0.025 | 0.031 |
| (2.58) | (2.60) | (3.79) | |
| Log of population times population category 250,000–499,999 dummy variable | 0.029 | 0.030 | 0.036 |
| (2.26) | (2.50) | (3.53) | |
| Log of population times population category 500,000–999,999 dummy variable | 0.041 | 0.041 | 0.042 |
| (2.75) | (2.83) | (3.61) | |
| Log of population times population category 1,000,000+ dummy variable | 0.043 | 0.043 | 0.046 |
| (2.27) | (2.35) | (3.42) | |
| Log of total service offerings | 0.727 | 0.654 | 0.464 |
| (9.73) | (9.71) | (8.50) | |
| % Services contracted out* | −0.921 | −0.850 | −0.683 |
| (1.91) | (1.91) | (1.84) | |
| % Services produced by other agencies* | −1.685 | −1.553 | −1.293 |
| (8.59) | (9.19) | (8.87) | |
| % Clinical services† | 1.047 | 0.955 | 0.876 |
| (4.50) | (4.41) | (5.07) | |
| % County funding† | 0.004 | 0.004 | 0.003 |
| (2.34) | (2.45) | (2.06) | |
| % State funding† | 0.004 | 0.005 | 0.004 |
| (2.05) | (2.43) | (2.69) | |
| % Federal funding† | 0.003 | 0.004 | 0.001 |
| (1.83) | (2.03) | (0.97) | |
| % Medicaid funding† | 0.015 | 0.016 | 0.010 |
| (7.17) | (7.56) | (5.08) | |
| % Medicare funding† | 0.018 | 0.018 | 0.013 |
| (7.62) | (8.47) | (6.99) | |
| % Private foundation funding† | 0.026 | 0.027 | 0.021 |
| (5.42) | (5.63) | (4.48) | |
| % Private health insurance funding† | 0.006 | 0.006 | 0.005 |
| (1.15) | (1.20) | (0.93) | |
| %Patient personal fees† | 0.004 | 0.004 | 0.0004 |
| (1.56) | (1.59) | (0.17) | |
| % Regulatory fees† | −0.001 | 0.00003 | −0.001 |
| (0.45) | (0.019) | (0.74) | |
| % Tribal funding† | −0.055 | −0.056 | 0.106 |
| (3.82) | (3.96) | (2.16) | |
| % Other funding† | 0.008 | 0.007 | 0.004 |
| (3.25) | (3.23) | (2.40) | |
| % White‡ | 0.002 | 0.002 | 0.003 |
| (0.67) | (0.061) | (1.04) | |
| % Black‡ | 0.008 | 0.008 | 0.009 |
| (2.61) | (2.43) | (3.21) | |
| % Asian‡ | 0.015 | 0.010 | −0.001 |
| (1.45) | (1.03) | (0.15) | |
| % Hispanic‡ | 0.004 | 0.004 | 0.003 |
| (1.44) | (1.33) | (1.25) | |
| LHD with county jurisdiction§ | −0.189 | −0.214 | −0.095 |
| (1.73) | (2.04) | (1.18) | |
| LHD with city/county jurisdiction§ | −0.080 | −0.026 | 0.060 |
| (0.07) | (0.25) | (0.73) | |
| LHD with town/township jurisdiction§ | −0.203 | −0.165 | −0.070 |
| (1.71) | (1.42) | (0.69) | |
| LHD with regional jurisdiction§ | −0.229 | −0.242 | −0.105 |
| (1.99) | (2.16) | (1.23) | |
| LHD with other jurisdiction§ | −0.447 | −0.453 | −0.296 |
| (2.95) | (3.01) | (1.79) | |
| LHD serving micropolitan area¶ | 0.087 | 0.062 | 0.057 |
| (1.72) | (1.33) | (1.51) | |
| LHD serving rural area¶ | 0.088 | 0.082 | 0.038 |
| (1.61) | (1.63) | (0.93) | |
| Adjusted R2 | 0.877 | 0.885 | 0.926 |
| Number of observations | 1,654 | 1,645 | 1,352 |
Notes. All models are estimated with a set of 47 state dummy variables for which the results are not shown to save space.
Heteroskedasticity-consistent standard errors are shown in parentheses.
Omitted category is percent of services produced internally.
Omitted category is percent town or city funding.
Omitted category is percent other (e.g., Pacific Islander or non-Hispanic).
Omitted category is city jurisdiction.
Omitted category is urban area.
LHD, local health department.
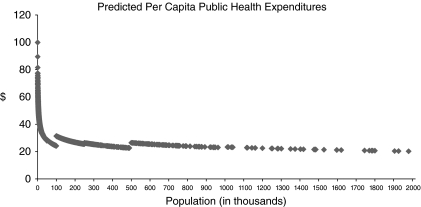
Figure 1 uses the estimated equation shown in column 2 of Table 3 to compute the predicted total costs associated with each level of population assuming all other independent variables are evaluated at their mean values. The predicted total costs are then divided by population to derive predicted per capita public health costs at each level of population. Predicted values for LHDs with populations above 2 million had to be suppressed so that the figure can be more easily viewed. Like the estimated equation, the figure shows some nonlinearity holds with respect to the relation between population and public health costs. More importantly, the figure reveals that the MES of an LHD is slightly below 100,000 people. The MES represents the smallest possible size at which an organization can minimize average costs, or per capita costs in this case. Figure 1 also shows that further increases in population have little effect on public health costs per capita after the MES.
Figure 1.
Predicted Per Capita Public Health Expenditures
DISCUSSION
The empirical results suggest that local public health costs rise less than proportionately to an increase in population. This characteristic holds in all population ranges but with some nonlinearity. In particular, the responsiveness of costs to a change in population is greater in more populous LHDs. This may mean that the congestability effects are stronger or the scale/scope and positive externality effects are weaker in LHDs with larger populations.
The results further show that the MES of an LHD is reached with a population of about 100,000 people. After that size, additional population is not associated with much reduction in public health spending per capita. In effect, an L-shaped relation exists between population and per capita public health costs with costs per capita falling rapidly at first but then leveling off after 100,000 people. Interestingly, studies have found L-shaped scale effects for various manufacturing firms and hospitals (Finkler 1979; Perloff 2007;). Finkler (1979) argues that an L-shaped scale effect may reflect that small organizations do not produce all of their services at efficient volumes. It follows from the empirical analysis that some cost savings might be realized if small public health departments are consolidated into larger districts. Thus, these results agree with Bates and Santerre (2008), who find that an independent LHD in Connecticut is unlikely to experience a sharp spike in taxes upon joining a unified public health district.
However, we cannot overlook that the results may be affected by omitted variable bias. Although the estimated relation between population and costs appears to be relatively insensitive to the inclusion of numerous factors, unmeasured variables such as quality, output heterogeneity, and the nature and severity of public health risks may have influenced the regression results. Such adjustments are especially important in a cost function analysis that relies on population size as the primary measure of quantity. Future research may want to improve upon this cross-sectional study by using a panel dataset of LHDs if that data become available. A panel dataset can control for unobservable heterogeneity to some degree and allow for a dynamic analysis of the effect of population on local public health costs.
CONCLUSION
Many experts suspect that LHDs will play an increasing role in the future. Because public health budgets are limited, public health officials will continually be interested in finding more cost-effective ways of expanding public health services. Thus, it stands to reason that research directed toward the most efficient way of structuring LHDs will provide useful information to public health officials both now and in the future.
This paper finds that the MES for an LHD occurs at approximately 100,000 people. That is, the typical LHD can fully exploit any cost savings associated with population at 100,000 people given the likely congestability, externality, and scale/scope effects associated with public health services. Unfortunately for public health policy makers and society, 77 percent of LHDs with about 18 percent of the U.S. population are below this efficient level of population. Even if it is assumed that the true efficient population is only one-half of the estimated efficient population, 62 percent of the surveyed LHDs, with about 10 percent of the population, fall below the MES. It should be noted that the unexploited cost savings are not trivial when LHDs remain small sized. According to the predicted per capita spending figures from this study, an LHD with 50,000 people will spend about 30.7 percent less on a per capita basis than an otherwise similar LHD with 10,000 people (US$28.74 versus US$41.46). Moreover, an LHD with 90,000 people will spend 13.6 percent less per capita than an otherwise similar LHD with 50,000 people (i.e., US$24.82). Clearly, small-sized LHDs face a serious cost disadvantage when it comes to producing local public health services.
Of course, costs represent only one side of the equation. The benefits associated with population size must also be considered. For example, one might argue that large population may compromise benefits by interfering with the provision of high-quality public health services. But Mays et al. (2006) show that any negative benefits of population size, in terms of diminishing the performance of 10 essential services, do not occur until a population of about 500,000 is reached for most services.
Some important policy implications follow from the empirical analysis. Given that many LHDs fall below the MES of 100,000 people, higher levels of government may want to employ financial incentives to encourage more LHDs to consolidate the provision of their public health services. Most of the focus should initially be directed at the smallest of the LHDs because a greater margin of benefits to costs should be gained from consolidation.7 For example, LHDs servicing <10,000 people may be awarded more dollars per capita upon joining a public health district than LHDs with 25,000 or more people. If research shows that the expected gains materialize for the smallest of the LHDs, then a higher level of government might incrementally extend financial inducements of lesser amounts to progressively more populated LHDs.
As an alternative to consolidation, it may be efficient for small agencies to buy scale-sensitive services from others (via contract) or to rely on the state agency or a larger neighboring agency to provide these services. Estimates from this analysis suggest that costs decrease significantly with increases in the proportion of services that are delivered by contract and the proportion of services that are delivered by other organizations. While these estimates are potentially vulnerable to endogeneity bias, they do suggest that small agencies may use these other production technologies for producing scale-sensitive services.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: I thank Carolyn Leep of the National Association of County and City Health Officers for helping me secure the necessary data. Data for this study were obtained from the 2005 National Profile of Local Public Health Agencies, a project supported through a cooperative agreement between the National Association of County and City Health Officials and the Centers for Disease Control and Prevention. I also thank the two anonymous referees of this journal for their many helpful suggestions for improving the paper.
Disclosures: None.
Disclaimers: None.
Prior Dissemination: This paper was very recently posted to our Program's webpage at the University of Connecticut. See ms# 2009-01 at http://www.business.uconn.edu/healthcare/working%20papers.html.
NOTES
Also many other articles in that same issue of Health Affairs.
For example, see Boulier, Datta, and Goldfarb (2007) to gain some insights into the complexities of the external effects associated with vaccinations.
Of course, how many services the typical consumer/voter receives and how much it costs depend on the congestability, externality, and scale and scope economies associated with local public health services.
The identity of the various LHDs remains confidential and direct measures of income and age distribution are not available from the NACCHO survey. The confidential nature of each LHD also prevents including other variables such as area, the number of hospitals and physicians in the area, and some type of wage index.
NACCHO does provide information on the number of full-time equivalent employees (FTEs). If total payroll data were collected by NACCHO, an average price of labor could be constructed (i.e., payroll/number of FTEs).
The results for the control variables are not discussed because many may be endogenous and because of space constraints.
Experimentation of this kind would also be a good practice because we cannot totally rule out that the empirical results obtained here have been influenced by omitted variable bias.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Bates LJ, Santerre RE. The Demand for Local Public Health Services: Do Unified and Independent Public Health Departments Spend Differently? Medical Care. 2008;46(6):590–6. doi: 10.1097/MLR.0b013e318164944c. [DOI] [PubMed] [Google Scholar]
- Bergstrom TC, Goodman RP. Private Demands for Public Goods. American Economic Review. 1973;63:280–96. [Google Scholar]
- Borcherding TE, Deacon RT. The Demands for the Services of Non-Federal Governments. American Economic Review. 1972;62:891–901. [Google Scholar]
- Boulier BL, Datta TS, Goldfarb RS. Vaccination Externalities. B.E. Journal of Economic Analysis & Policy. 2007;7(1) Available at http://www.bepress.com/bejeap/vol7/iss1/art23. [Google Scholar]
- Carande-Kulis VG, Getzen TE, Thacker SB. Public Goods and Externalities: A Research Agenda for Public Health Economists. Journal of Public Health Management and Practice. 2007;13(2):227–32. doi: 10.1097/00124784-200703000-00024. [DOI] [PubMed] [Google Scholar]
- Cowing TG, Holtmann AG. Multiproduct Short-Run Hospital Cost Functions: Empirical Evidence and Policy Implications from Cross-Section Data. Southern Economic Journal. 1983;49:637–53. [Google Scholar]
- Finkler SA. On the Shape of the Hospital Industry Long Run Average Cost Curve. Health Services Research. 1979;14(4):281–8. [PMC free article] [PubMed] [Google Scholar]
- Gordon RL, Gerzoff RB, Richards TB. Determinants of U.S. Local Health Department Expenditures, 1992 through 1993. American Journal of Public Health. 1997;87:91–5. doi: 10.2105/ajph.87.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granneman TW, Brown RS, Pauly MV. Estimating Hospital Costs: A Multiple-Output Analysis. Journal of Health Economics. 1986;5:107–27. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Hartman M, Martin A, McDonnell P, Catlin A and the National Health Expenditure Account Team. National Health Spending in 2007: Slower Drug Spending Contributes to Low Rates of Overall Growth Since 1998. Health Affairs. 2009;28:246–61. doi: 10.1377/hlthaff.28.1.246. [DOI] [PubMed] [Google Scholar]
- Mays GP, McHugh MC, Shim K, Perry N, Lenaway D, Halverson PK, Moonesinghe R. Institutional and Economic Determinants of Public Health System Performance. American Journal of Public Health. 2006;96(3):523–31. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of County and City Health Officers (NACCHO) 2005 National Profile of Local Health Departments. Washington, DC: NACCHO; 2006. [Google Scholar]
- Perloff JM. Microeconomics. New York: Pearson/Addison Wesley; 2007. [Google Scholar]
- Santerre RE. Spatial Differences in the Demands for Local Public Goods. Land Economics. 1985;61:119–28. [Google Scholar]
- Santerre RE, Neun SP. Health Economics: Theories, Insights, and Industry Studies. Mason, OH: Thomson/SouthWestern; 2007. [Google Scholar]
- Shonick W, Price W. Organizational Milieus of Local Public Health Units: Analysis of Response to Questionnaire. Public Health Reports. 1978;93(6):648–65. [PMC free article] [PubMed] [Google Scholar]
- Tiebout C. A Pure Theory of Local Public Expenditures. Journal of Political Economy. 1956;64(5):416–24. [Google Scholar]
- Tilson H, Berkowitz B. The Public Health Enterprise: Examining Our Twenty-First-Century Challenges. Health Affairs. 2006;25(4):900–10. doi: 10.1377/hlthaff.25.4.900. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.