Abstract
Dual origin and fenestration of the vertebral artery (VA) are very rare anomalies. Understanding of these variations, however, is important because they can be misdiagnosed as a VA dissection. A 42-year-old woman presented with motor weakness and sensory disturbance of the right upper extremity. Radiologic evaluations showed ectatic change in the right VA and an arteriovenous fistula between the right VA and the vertebral vein. We decided on endovascular occlusion of the proximal right VA and its fistulous portion. During the endovascular procedure, we had misunderstood the dual origin and fenestration of the VA as a dissection. Thus, failure to recognize these anomalies might result in unnecessary anticoagulation or therapeutic intervention. Clinicians should be alert to such VA variations when making a diagnosis and when planning any intervention or surgery involving the proximal VA.
Keywords: Dissection, Dual origin, Fenestration, Vertebral artery
INTRODUCTION
Anomalous origins of the vertebral artery (VA) are present in approximately 5% of individuals and in the most instances, the left VA arises directly from the aortic arch4). Dual origin of the VA is very rare and the incidence of fenestration in the distal VA varies between 0.23 and 1.9%8). Acknowledging these variations is important for clinicians because they can be misdiagnosed as a VA dissection1,6). Here, we describe a case of dual origin of the left VA that was misdiagnosed as a dissection.
CASE REPORT
A 42-year-old woman presented with motor weakness and sensory disturbance of the right upper extremity. She had no history of trauma. Neurological findings included right C5 to C7 radiculopathy and weakness of the forearm. Cervical magnetic resonance imaging (MRI) demonstrated an abnormal dilated vessel on the right spinal canal and adjacent paravertebral area. Bilateral vertebral angiography showed ectatic change in the right VA and an arteriovenous fistula between the right VA and the vertebral vein (Fig. 1). We decided on endovascular occlusion of the proximal right VA and its fistulous portion. After successful endovascular occlusion of the proximal right VA using detachable coils and fibered pushable coils, we attempted to occlude the fistulous portion via the left VA. During navigation of the left VA with a guide wire, passing the VA with wire was impossible at the C5 level. At the time of diagnostic angiogram, passing the guide wire and diagnostic catheter were easy. Follow-up of left vertebral angiography demonstrated an irregular, filling defect in the lumen (Fig. 2). Ten mg of ReoPro® (Lilly, Indianapolis, IN, USA) was injected intra-arterially under the suspicion of dissection. After ReoPro® infusion, a vertebral angiogram revealed a reflux of contrast agent into another vascular structure (Fig. 3A). An aortogram was carried out and it showed another left VA, originating from the aorta between the left common carotid artery and the subclavian artery (Fig. 3B), implying the dual origin of the VA. After confirming that the lesion was not a dissection, we continued endovascular occlusion of the fistula. While further navigating the distal intracranial portion of the VA, we found what appeared to be a dissection, given the presence of a double lumen (Fig. 4A). This lesion was soon disclosed as a fenestration in oblique projection of left vertebral angiography (Fig. 4B). The patient successfully underwent endovascular occlusion of the fistula, recovered dramatically, and was subsequently discharged.
Fig. 1.

Left vertebral angiogram (antero-posterior view) shows the ectatic change in the right vertebral artery (VA) and an arteriovenous fistula between the right VA and the vertebral vein
Fig. 2.

Follow-up of a left vertebral angiogram suggests vertebral artery dissection with a finding of irregular, filling defect (arrow) of the lumen.
Fig. 3.
Left vertebral angiogram (A) after injection of ReoPro® (Lilly, Indianapolis, IN, USA) reveals the reflux of the contrast agent into another vascular structure (arrow). Aortogram (B) demonstrates that another left vertebral artery (VA) (white arrow head), originating from the aorta between the left common carotid artery and the subclavian artery, joins with the normal origin left VA (black arrow head).
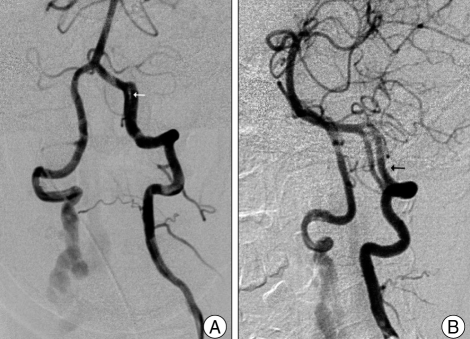
Fig. 4.
Intracranial left vertebral arteriogram (A) shows double lumen sign (white arrow). Oblique projection of the angiogram (B) demonstrates the aforementioned site as a fenestration (black arrow).
DISCUSSION
Various types of anomalous VA origins have been reported. Among these anomalies, the most common type is the left VA arising directly from the aortic arch, which is present in approximately 2.4-5.8% of healthy individuals10). The dual origin of the VA, directly from the aorta (medial leg) and the other from the left subclavian artery (lateral leg) to form a distal common trunk, is a rare condition11). The dual origin of the VA might be considered to result from the persistence of more than one embryological cervical intersegmental artery2). The condition was first described in 1844 and to date, 24 cases, including the current case, have been reported5).
The clinical significance of recognizing this anomaly is important in several situations. The anomaly can be confused with a VA dissection when a filling defect is created at the junction between the anomalous origin and the normal origin of the VA due to non-contrast filling blood from anomalous origin side during studies6). Especially as observed in the present case, if an operator has difficulty navigating the VA when passing the guide wire through the junction between the anomalous origin and the normal origin of the VA, the filling defect can be mistaken for dissection. In similar situations, one may encounter an abrupt change in the size of the VA at its junction, and this might be presumed to be hypoplasia or even pathologic narrowing of the vessel.
Acknowledging the dual origin of the VA is also important in the preoperative evaluation of patients with posterior circulation vascular disease who require an endovascular procedure or in patients with extracranial vascular disease requiring reconstruction of the VA. If the true anatomic configuration of the VA's dual origin is identified, the ideal route of endovascular procedure can be chosen preoperatively, and in such cases, reconstructive procedures (e.g., proximal VA endarterectomy, stenting, or transplantation) can be avoided.
Diagnosing the dual origin of a VA is difficult for several reasons. Aortography may fail to show it because of poor visualization of the small vessels5). When only either one leg of the dual origin of the VA is visualized, there is a possibility of misdiagnosis as hypoplasia. As illustrated by the current case, in order to detect the dual origin of the VA, pressure injection of a contrast agent in one leg may result in reflux into the other leg2). General ignorance of this congenital vascular anomaly also makes diagnosis difficult. Given the potential for technical opacifying difficulties or ignorance of this congenital vascular anomaly, many cases with double origin of the VA may be overlooked. Therefore, clinicians should always suspect the dual origin of the VA, when there is streaming of the contrast agent, filling defect in the vessel, irregularity of the lumen, or abrupt changes in the diameter of the VA or when dissection of the VA is suspected at the C4-6 level2,6).
The prevalence of fenestration or partial duplication of the VA is approximately 1%3,9). The most common site (approximately 70%) is in the cervical segment, mostly at the atlantoaxial level, while the remaining cases were found to occur intracranially3,7). Despite a double-lumen being regarded as a pathognomonic sign of arterial dissection, this anomaly may be confused with an arterial fenestration as occurred in the present case and in a previously reported case1).
CONCLUSION
Acknowledging vessel anatomy and their variations is important for clinicians in the current era of stents and with many new therapeutic options for interventions. Although VA dissection is best diagnosed with conventional angiography, dual origin and fenestration of the VA may mimic VA dissection in conventional angiography. Thus, failure to recognize these anomalies might result in unnecessary anticoagulation or therapeutic intervention. Clinicians should keep in mind that knowledge of the dual origin and fenestration of the VA is important when making a diagnosis and when planning for any intervention or surgery involving the proximal VA.
Acknowledgements
This paper was supported by Wonkwang University in 2008.
References
- 1.Drapkin AJ. The double lumen : a pathognomonic angiographic sign of arterial dissection? Neuroradiology. 2000;42:203–205. doi: 10.1007/s002340050046. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg RA, Vines FS, Taylor SB. Bifid origin of the left vertebral artery. Radiology. 1986;159:429–430. doi: 10.1148/radiology.159.2.3961176. [DOI] [PubMed] [Google Scholar]
- 3.Hasegawa T, Ito H, Hwang WZ, Yamamoto S. Single extracranial intracranial duplication of the vertebral artery. Surg Neurol. 1986;25:369–372. doi: 10.1016/0090-3019(86)90212-0. [DOI] [PubMed] [Google Scholar]
- 4.Haughton VM, Rosebaum AE. The normal and anomalous aortic arch and brachiocephalic arteries. In: Newton TH, Potts DG, editors. Radiology of the skull and brain. Vol. 2. St. Louis: Mosby; 1978. pp. 1145–1163. [Google Scholar]
- 5.Komiyama M, Nakajima H, Yamanaka K, Iwai Y. Dual origin of the vertebral artery : case report. Neurol Med Chir (Tokyo) 1999;39:932–937. doi: 10.2176/nmc.39.932. [DOI] [PubMed] [Google Scholar]
- 6.Nogueira TE, Chambers AA, Brueggemeyer MT, Miller TJ. Dual origin of the vertebral artery mimicking dissection. AJNR Am J Neuroradiol. 1997;18:382–384. [PMC free article] [PubMed] [Google Scholar]
- 7.Osborn RE, Kirk G. Cerebral arterial fenestration. Comput Radiol. 1987;11:141–145. doi: 10.1016/0730-4862(87)90039-4. [DOI] [PubMed] [Google Scholar]
- 8.Rieger P, Huber G. Fenestration and duplicate origin of the left vertebral artery in angiography. Report of three cases. Neuroradiology. 1983;25:45–50. doi: 10.1007/BF00327480. [DOI] [PubMed] [Google Scholar]
- 9.San-Galli F, Leman C, Kien P, Khazaal J, Phillips SD, Guérin J. Cerebral arterial fenestration associated with intracranial saccular aneurysms. Neurosurgery. 1992;30:279–283. doi: 10.1227/00006123-199202000-00026. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki S, Kuwabara Y, Hatano R, Iwai T. Duplicated origin of left vertebral artery. Neuroradiology. 1978;15:27–29. doi: 10.1007/BF00327442. [DOI] [PubMed] [Google Scholar]
- 11.Thomas AJ, Germanwala AV, Vora N, Prevedello DM, Jovin T, Kassam A, et al. Dual origin extracranial vertebral artery : case report and embryology. J Neuroimaging. 2008;18:173–176. doi: 10.1111/j.1552-6569.2007.00182.x. [DOI] [PubMed] [Google Scholar]