Abstract
Objectives
Significant questions remain regarding both the incidence patterns of mood episodes in adolescents and young adults from the community and the conversion rate from unipolar to bipolar disorders. We addressed these issues by examining data from a prospective longitudinal community study to (i) determine the cumulative incidence of mood episodes and disorders in the first three decades of life; (ii) determine the risk for first onset of depression among individuals with a previous history of hypomanic/manic episodes and vice versa; and (iii) determine the clinical and treatment characteristics of these subjects.
Methods
Using the Munich-Composite International Diagnostic Interview, clinically trained interviewers assessed mood episodes and mental disorders in 3,021 community subjects (aged 14–24 at baseline and 21–34 at third follow-up).
Results
The estimated cumulative incidence at age 33 was 2.9% for manic, 4.0% for hypomanic, 29.4% for major depressive, and 19.0% for minor depressive episodes; overall, 26.0% had unipolar major depression, 4.0% bipolar depression, 1.5% unipolar mania, and 3.6% unipolar hypomania (no major depression). Overall, 0.6% and 1.8% had unipolar mania or hypomania, respectively, without indication for even minor depression. A total of 3.6% of the initial unipolar major depression cases subsequently developed (hypo)mania, with particularly high rates in adolescent onset depression (< 17 years: 9%). A total of 49.6% of the initial unipolar mania cases subsequently developed major depression and 75.6% major or minor depression. While bipolar cases had more adverse clinical and course depression characteristics and higher treatment rates than unipolar depressed cases, bipolar cases did not significantly differ in mania characteristics from unipolar mania cases.
Conclusions
Unipolar and bipolar mood disorders are more frequent than previously thought in adolescence and young adulthood, a time period when both the recognition and the intervention rates by the healthcare system are rather low. ‘Conversion’ to bipolar disorder is limited in initial unipolar depression, but common in initial unipolar mania. The remaining unipolar mania cases appear to be significant in terms of clinical and course characteristics and thus require more research attention to replicate these findings.
Keywords: bipolar disorder, community study, conversion, epidemiology, mood episode
In the traditional nosology of manic-depressive illness/bipolar disorder (BD), depression and mania are viewed as part of a unitary illness, reflecting dysregulation along a mood dimension (1). The frequency of (hypo)manic episodes without lifetime episodes of depression remains controversial; prevalence data among all bipolar patients range from 1.1 to 47.2% (2). Less controversial is the observation that individuals with unipolar depressive disorder might subsequently develop (hypo)manic episodes, thus converting to BD. The question remains what proportion will convert and whether it is feasible to predict conversion, e.g., by characteristics of the initial depressive episode. The answers to these questions would inform nosology and facilitate early recognition and intervention (3).
While there are a substantial number of large, community-based surveys, most are limited by their cross-sectional nature and inclusion of a broad age spectrum, spanning adolescence (age 16+) to late adulthood (4–9). Thus, these studies may be subject to notable recall bias and they typically do not provide an adequately powered sample to estimate the prevalence and incidence of mood episodes in restricted age ranges, such as adolescence and young adulthood. Yet these studies suggest that the highest incidence of mood episodes occurs between ages 15–25 (9–14). Ages of first onset may date back to childhood (15, 16), but childhood studies often differ from those in adolescents and adults in terms of diagnostic criteria and assessment instruments (e.g., self versus parental report). Thus, it is difficult to draw firm conclusions about the frequency of hypomania and mania in childhood and adolescence. Furthermore, little information is available about the probability of longitudinal transitions from depressive to (hypo)manic episodes, and also the reverse direction, in this time period. Beyond major depression, considering minor depression (potential ‘counterparts’ of hypomanic episodes) is important given significant functional impairment (17).
Using data from a prospective, longitudinal community sample of adolescents and young adults, we examined the following questions:
What is the cumulative incidence of manic episodes (ME), hypomanic episodes (HE), major depressive episodes (MDE), and minor depressive episodes (MinDE), as well as of unipolar and bipolar mood disorders, in the first three decades of life?
What is the risk for first onset of major or minor depression among individuals with a previous history of HE/ME? And what is the risk for first onset of HE/ME among individuals with a preceding MDE or MinDE?
What clinical and treatment features characterize subjects with unipolar and bipolar mood disorders?
Patients and methods
Sample
The Early Developmental Stages of Psychopathology (EDSP) study is a prospective, longitudinal study in a representative community sample of 3,021 subjects aged 14–24 years at baseline (T0) that was followed prospectively (T1/T2/T3) over up to 10 years (14, 18, 19). The baseline response rate was 70.8%. The conditional response rates were 88.0% at T1 (interval since baseline: 1.2–2.1 years), 84.3% at T2 (interval since baseline: 2.8–4.1 years), and 73.2% at T3 (interval since baseline: 7.3–10.6 years).
Diagnostic assessment
Individuals were assessed by trained clinical interviewers (mostly psychologists) with the computer-assisted Munich-Composite International Diagnostic Interview (DIA-X/M-CIDI) (20, 21). The lifetime DIA-X/M-CIDI was used at baseline and the interval version at follow-ups. Test-retest reliability and validity for the DIA-X/M-CIDI have been previously established (21–23).
Diagnoses were computed using the M-CIDI/DSM-IV algorithms. Consistent with DSM-IV and M-CIDI conventions, we studied the following mood episodes: MDE, HE, and ME. We also considered the research category of MinDE, defined as 2–4 depressive symptoms (one of them depressed mood or loss of interest) occurring over at least two weeks with distress/impairment.
In addition to these definitions of episode types, we used the DSM-IV diagnoses: major depressive disorder [(MDD) = unipolar depression; MDE but no ME/HE] and bipolar disorder [(BD) =ME/HE and MDE]. When DSM-IV ME or HE criteria were met without lifetime presence of MDE, we deviated from the DSM-IV convention by using the terms unipolar mania (instead of BD as in DSM-IV) and unipolar hypomania (instead of BD not otherwise specified as in DSM-IV). We also labeled cases with ME and MDE, or HE and MDE, as bipolar depression to differentiate these cases from DSM BD, which also includes cases with ME but no MDE. Furthermore, we also considered MinDE for broadly defined bipolar depression.
Age of onset information for mood episodes over assessment waves was based on the minimum age of onset reported by the respondent (24). This definition agreed well (> 90%) with other age-of-onset aggregation methods (e.g., using the first or the mean of reported ages of onset), i.e., the absolute value of differences were at most one year. The only exception was that agreement between the mean and minimum method in MDE onset was 72.5%. Duration of longest episode was based on the maximum reported number of consecutive weeks with depression or (hypo)mania, respectively, at any assessment. Number of episodes was based on the maximum number of reported depressive or (hypo)manic episodes at any assessment; a two-month period of euthymia was required to account for the presence of different episodes. Professional attention/treatment was hierarchically assessed (hospitalization, treatment by doctor, treatment by other specialist, medication use) separately for depression and/or (hypo)mania in the respective M-CIDI sections. Impairment due to depression or (hypo)mania, respectively, was dichotomized to severe (a fair amount or much) versus nonsevere (a little/none).
Statistical analysis
Data were weighted by age, sex, and geographic location at baseline to match the distribution of the sampling frame; frequencies are reported unweighted. Stata 10.0 (25) was used to compute robust variances, confidence intervals (CI), and p-values (by applying the Huber-White sandwich matrix) required when basing analyses on weighted data (26).
Age-specific cumulative incidence rates (in contrast to observed rates) were estimated with the Kaplan-Meier method (27). Separate Cox regressions with hazard ratios (HR) were used to assess overall differences in the risk of mood episodes between females and males. Cox regressions were also used to assess associations with the risk for MDE and MinDE between those without HE and ME and those with HE and ME, respectively. Conversely, associations with the risk for HE/ME were assessed between those without MDE or MinDE and those with MDE or MinDE.
Group differences in binary outcomes were assessed with odds ratios (ORs) from logistic regressions. Differences in moderately skewed outcomes (e.g., age of onset) were assessed with median differences from linear regressions. All associations were adjusted for sex and age at last assessment.
Of note, age-of-onset information was missing for two cases with MDE and three cases with HME; these subjects were excluded from all analyses considering temporal order of onset.
Results
Cumulative incidence
Mood episodes
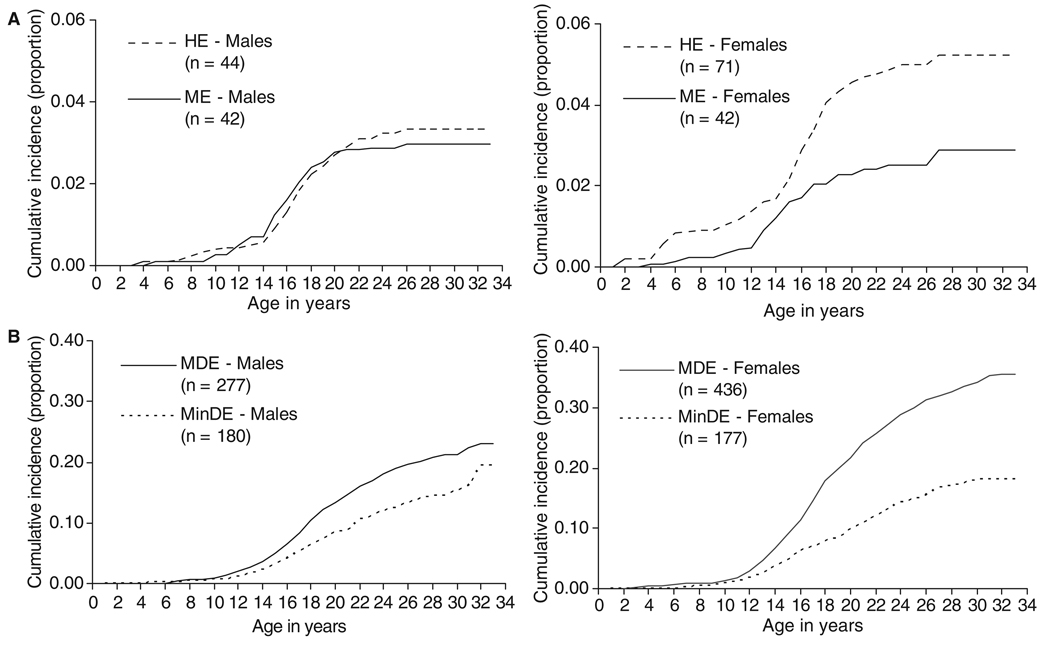
The estimated age-specific cumulative incidence at age 33 was 2.9% for ME (observed n = 84, 2.8%; note: numbers are unweighted, percentages are weighted), 4.0% for HE (observed n = 115, 3.8%), 29.4% for MDE (observed n = 822, 28.4%), and 19.0% for MinDE (observed n = 357, 12.4%).
The cumulative incidence for ME was almost the same for males (3.0%) and females (2.9%; HR = 0.92; 95% CI: 0.57–1.49, p = 0.733; Fig. 1A). For both genders, peak incidence period for ME was the mid-teens. With respect to HE, females had a higher estimated cumulative incidence at age 33 (5.2%) than males (3.3%; HR = 1.74; 95% CI: 1.15–2.64, p = 0.009). Some first ME/HE cases occurred in childhood, and a sharp incidence increase was found in adolescence; first onsets after the age of 20 were rare.
Fig. 1.
Overall age-specific cumulative incidence of mood episodes for males (n = 1,533) and females (n = 1,488). (A) hypomanic episode (HE) and manic episode (ME); (B) major depressive episode (MDE) and minor depressive episode (MinDE).
Females revealed a higher estimated cumulative incidence at age 33 than males for MDE (females: 35.6%, males: 23.1%; HR = 1.70, 95% CI: 1.44–2.01, p < 0.001), but not for MinDE (females: 18.0%, males: 19.4%) (Fig. 1B). In both genders, some few depression onsets occurred in childhood. Most cases emerged between ages 12 and 25 and, in contrast to the HE/ME curves, both males and females showed continued new onsets of MDE and MinDE up to the mid-30s.
Mood disorders
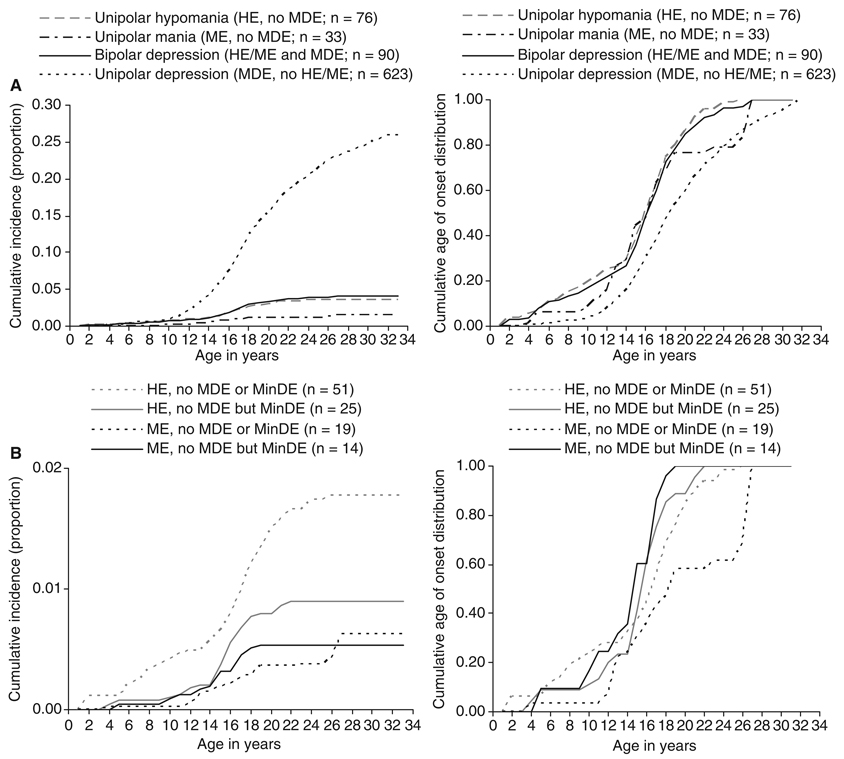
A total of 33 of the 84 observed ME cases (36.9%) and 76 of the 115 HE cases (67.8%) never had threshold DSM-IV MDE, and thus could be best labeled as unipolar mania or unipolar hypomania, respectively. Among the 713 MDE cases, 623 (88.0%) did not experience HE/ME (MDD; unipolar major depression), while 90 (12.0%) did [bipolar depression; i.e., MDE and ME (7.0%; n = 51) or MDE and HE (5.0%; n = 39)]. The estimated cumulative incidences of mutually exclusive mood disorder categories up to age 33 are 1.5% for unipolar mania (ME, no MDE), 3.6% for unipolar hypomania (HE; no MDE), 26.0% for unipolar major depression (MDD; MDE, no HE/ME); and 4.0% bipolar depression (MDE and HE or ME) (Fig. 2A). The age-of-onset patterns suggest that unipolar mania/hypomania occurs earlier than unipolar major depression and that bipolar cases reveal earlier onset of first mood episode compared to unipolar major depression cases.
Fig. 2.
Age-specific cumulative incidence and age-of-onset distribution of (A) unipolar hypomania/mania, unipolar depression, and bipolar depressiona and of (B) unipolar hypomania/mania with or without minor depressiona. HE = hypomanic episode; ME = manic episode; MDE = major depressive episode; MinDE = minor depressive episode.
aFor bipolar depression cases (A) and (hypo)mania with minor depression cases (B), age of onset is defined as the minimum age of onset of HE/ME and MDE (A) and MinDE (B).
Considering additionally MinDE (no MDE), the more strictly defined estimated cumulative incidence rates were 0.6% for unipolar mania (ME, no MDE/MinDE) and 1.8% for unipolar hypomania (HE, no MDE/MinDE); 0.5% had ME with MinDE but no MDE, and 0.9% had HE with MinDE but no MDE (Fig 2B). Earlier onsets of first mood episode occurred among (hypo)mania cases with MinDE compared to those without MinDE.
Importantly, an examination of ME and HE rates by age (Table 1) did not suggest that unipolar mania/hypomania as compared to bipolar depression cases were overrepresented in the younger age groups. Subjects with unipolar mania/hypomania appeared as likely as those with bipolar depression to have passed through the period of risk for depression.
Table 1.
Observed cases with hypomanic episode (HE) or manic episode (ME) in the total sample (n = 3,021) and by lifetime presence of major depressive episode (MDE) and minor depressive episode (MinDE)
| Gender |
Age at last assessment |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
≤ 20 years |
21–25 years |
26–30 years |
31–34 years |
|||||||||
| N | n | % w | n | % w | n | % w | n | % w | n | % w | n | % w | ||
| Total sample | ||||||||||||||
| Total | 3,021 | 1,533 | 49.4 | 1,488 | 50.6 | 424 | 9.9 | 1,259 | 31.9 | 956 | 36.5 | 382 | 21.8 | |
| HME or MNE | 199 | 86 | 42.6 | 113 | 57.4 | 28 | 14.1 | 80 | 40.2 | 67 | 33.7 | 24 | 12.1 | |
| HME | 115 | 44 | 36.2 | 71 | 63.8 | 15 | 9.9 | 46 | 30.4 | 44 | 45.2 | 10 | 14.6 | |
| MNE | 84 | 42 | 51.5 | 42 | 48.5 | 13 | 11.6 | 34 | 26.5 | 23 | 32.3 | 14 | 29.7 | |
| By MDE and MinDE | ||||||||||||||
| MDE | Total | 713 | 277 | 38.2 | 436 | 61.8 | 70 | 6.6 | 266 | 27.2 | 269 | 42.1 | 108 | 24.1 |
| HME or MNE | 90 | 34 | 38.6 | 56 | 61.4 | 12 | 9.4 | 38 | 30.5 | 23 | 28.1 | 17 | 31.9 | |
| HME | 39 | 13 | 26.7 | 26 | 73.3 | 4 | 9.4 | 18 | 35.5 | 11 | 29.6 | 6 | 25.5 | |
| MNE | 51 | 21 | 47.1 | 30 | 52.9 | 8 | 9.4 | 20 | 27.0 | 12 | 27.1 | 11 | 36.5 | |
| No MDE | Total | 2,308 | 1,256 | 53.1 | 1,052 | 46.9 | 354 | 10.9 | 993 | 33.5 | 687 | 34.6 | 274 | 21.0 |
| HME or MNE | 109 | 52 | 45.9 | 57 | 54.1 | 16 | 11.6 | 42 | 27.3 | 44 | 49.3 | 7 | 11.8 | |
| HME | 76 | 31 | 40.7 | 45 | 59.3 | 11 | 10.1 | 28 | 27.9 | 33 | 52.6 | 4 | 9.4 | |
| MNE | 33 | 21 | 59.1 | 12 | 40.9 | 5 | 15.3 | 14 | 25.6 | 11 | 41.1 | 3 | 18.0 | |
| MinDE | Total | 357 | 180 | 47.9 | 177 | 52.1 | 29 | 5.5 | 130 | 25.6 | 145 | 45.2 | 53 | 23.6 |
| HME or MNE | 39 | 18 | 43.2 | 21 | 56.8 | 6 | 12.1 | 12 | 22.6 | 18 | 52.2 | 3 | 13.1 | |
| HME | 25 | 10 | 36.0 | 15 | 64.0 | 3 | 7.8 | 10 | 31.9 | 11 | 53.8 | 1 | 6.6 | |
| MNE | 14 | 8 | 55.1 | 6 | 44.9 | 3 | 19.3 | 2 | 7.1 | 7 | 49.7 | 2 | 24.0 | |
| No MinDE | Total | 1,951 | 1,076 | 54.1 | 875 | 45.9 | 325 | 12.0 | 863 | 35.1 | 542 | 32.5 | 221 | 20.5 |
| HME or MNE | 70 | 34 | 47.6 | 36 | 52.4 | 10 | 11.3 | 30 | 30.2 | 26 | 47.5 | 4 | 11.1 | |
| HME | 51 | 21 | 43.1 | 30 | 56.9 | 8 | 11.3 | 18 | 25.9 | 22 | 52.0 | 3 | 10.9 | |
| MNE | 19 | 13 | 63.2 | 6 | 36.8 | 2 | 11.1 | 12 | 45.4 | 4 | 31.9 | 1 | 11.7 | |
N/n = unweighted number; % w = weighted row percentage.
Conditional probability and risk for onset of mood episodes
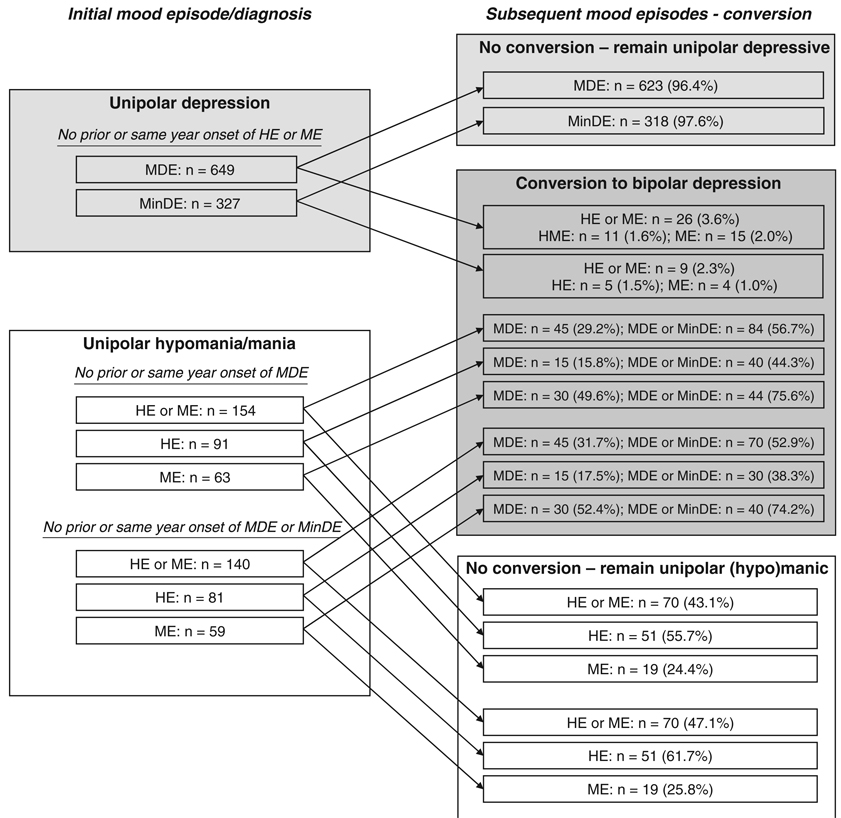
Two types of analyses were used to examine the probability and risk of developing bipolar depression given the presence of initial unipolar mania/hypomania and, conversely, initial unipolar depression. First, conversion numbers and rates were based on observed cases; and second, conversion risk up to age 33 was estimated by using survival analyses that take different ages at final assessment and dropouts into account. Cases with same-year onset of (hypo)mania and depression were not considered for these analyses because information on temporal priority was not available for these cases.
Risk for depressive episodes conditional on prior (hypo)manic episodes
Among the observed temporally primary unipolar (hypo)mania cases (HE/ME without a prior or same-year onset of MDE; n = 154), 45 (29.2%) subsequently developed MDE (Fig. 3), and thus bipolar depression. This rate did not differ by gender or by age of onset of HE/ME. Yet risk for bipolar depression was higher among primary ME cases (n = 30/63, 49.6%) than in primary HE cases (n = 15/91, 15.8%; OR = 5.2, 95% CI: 2.3–12.2, p < 0.001). Similar rates occurred when HE/ME cases with prior or same-year MinDE were excluded. Of note, however, rates were considerably higher when also considering subsequent MinDE in addition to MDE.
Fig. 3.
Conversion from unipolar to bipolar disorders. Shading: white = unipolar mania; light gray = unipolar depression; dark gray = bipolar depression. MDE = major depressive episode; MinDE = minor depressive episode; HE = hypomanic episode; ME = manic episode.
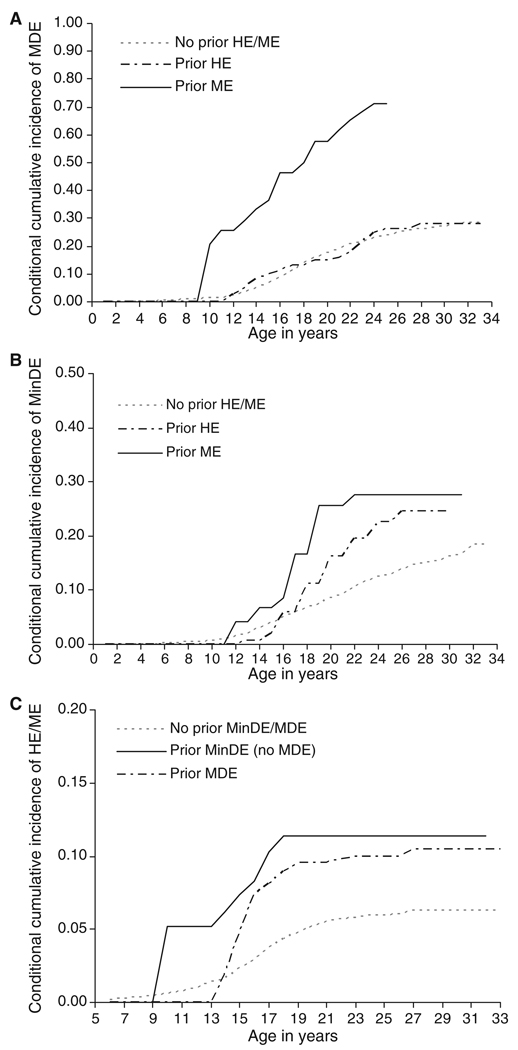
Survival analysis revealed that the estimated risk for a first onset of MDE (Fig. 4A) was greater among cases with prior ME [estimated percentage at age 25 (no stable estimates after that age): 71.2%; HR = 4.25; 95% CI: 2.83–6.40, p < 0.001] relative to cases without prior HE/ME (28.5%), both in males (HR = 3.94; 95% CI: 2.18–7.12, p < 0.001) and in females (HR = 4.61; 95% CI: 2.61–8.12, p < 0.001). Initial HE cases, however, did not reveal an increased estimated risk for temporally secondary MDE (estimated weighted percentage at age 33: 27.8%; HR = 0.89; 95% CI: 0.51–1.54, p = 0.580) compared to cases without prior HE/ME. Considering subsequent onset of MinDE (no MDE; Fig. 4B), similar findings occurred with ME (estimated percentage of MinDE at age 33: 27.6%; HR = 3.26; 95% CI: 1.64–6.46, p = 0.001) but not HE cases (estimated percentage of MinDE at age 33: 24.5%; HR = 1.46; 95% CI: 0.84–2.53, p = 0.177) showing a significantly increased risk compared to cases without prior HE/ME (estimated percentage of MinDE at age 33: 18.5%).
Fig. 4.
Conditional cumulative incidence of major depressive episode (MDE) (A) and minor depressive episode (MinDE) (B) by prior hypomanic episode (HE)/manic episode (ME), and conditional cumulative incidence of HE/ME by prior MDE and MinDE (C)a.
aIn (C) analyses are restricted to age range 5–33 due to unstable estimates because of low case numbers.
Risk for (hypo)manic episodes conditional on prior MDE
Among temporally primary MDE cases without prior or same-year onset of HE/ME (n = 649), 3.6% (n = 26) reported a subsequent onset of HE/ME (Fig. 3), with no significant gender difference. ‘Conversion’ rates to BD were highest among subjects with early MDE onset (age < 17: 9.0%) and lower among those with MDE onset at ages 17–20 (0.5%; OR = 0.05; 95% CI: 0.01–0.35, p = 0.003), 21–25 (0.7%; OR = 0.07; 95% CI: 0.01–0.56, p = 0.012), or 26 and above (0.0%). Compared to MDE, ‘conversion’ rates for MinDE were lower, particularly due to lower rates of ME onset (1.0%).
Survival analyses (age span 5–33; Fig. 4C) showed that the estimated risk for the onset of HE/ME tended to be higher among cases with prior MDE (estimated weighted percentage at age 33: 10.4%; HR = 1.54; 95% CI: 0.94–2.52, p = 0.089) compared to cases without prior MDE (6.3%). The risk for onset of HE/ME among cases with no prior MDE but MinDE was numerically similar (estimated weighted percentage at age 33: 11.4%) but not significantly increased compared to cases with neither MDE nor MinDE (6.3%; HR = 1.37; 95% CI: 0.65–2.89, p = 0.406).
Clinical and treatment characteristics of unipolar and bipolar cases
Course
Unipolar (hypo)mania cases (HE/ME, no MDE) did not differ from bipolar cases (HE/ME and MDE) in reported number of HE/MEs, duration of longest HE/ME, or age of onset of first HE/ME (Table 2; p-values > 0.1). Similar findings occurred when MinDE was considered in HE/ME cases, i.e., HE/ME cases with versus without MinDE did not differ in these characteristics. However, bipolar cases (MDE and HE or ME) were more likely to have a higher number of MDEs relative to unipolar depression cases (unweighted median difference: 2.0, p < 0.001; three or more episodes relative to only one episode: OR = 2.3, 95% CI: 1.3–3.8, p = 0.003; Table 3). They also had a longer episode duration of depression (unweighted median difference: 2.3, p = 0.051; 6–10 versus 2–5 weeks: OR = 3.5, 95% CI: 1.7–7.1, p = 0.001; 11 + versus 2–5 weeks: OR = 2.7, 95% CI: 1.4–4.9, p = 0.002), and an earlier age of onset of first MDE (unweighted median difference: –1.1, p = 0.030). This pattern was particularly pronounced for individuals with ME and MDE as opposed to those with HE and MDE.
Table 2.
Course characteristics of unipolar and bipolar (hypo)mania [n = 199 individuals with hypomanic episode (HE) or manic episode (ME) at any assessment]
| Unipolar (hypo)mania (no MDE) |
Bipolar (hypo)mania (with MDE) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HE/ME n = 109a |
HE n = 76a |
ME n = 33a |
HE/ME n = 90a |
HE n = 39a |
ME n =51a |
|||||||
| n | % w | n | % w | n | % w | n | % w | n | % w | n | % w | |
| Number of HE/MEs | ||||||||||||
| 1–7 | 29 | 32.8 | 18 | 29.4 | 11 | 40.1 | 27 | 38.2 | 12 | 40.9 | 15 | 36.5 |
| 8–15 | 30 | 37.2 | 18 | 34.8 | 12 | 42.7 | 21 | 28.7 | 10 | 27.7 | 11 | 29.4 |
| 16+ | 28 | 30.0 | 22 | 35.8 | 6 | 17.3 | 25 | 33.0 | 8 | 31.5 | 17 | 34.1 |
| Total | 87 | 100.0 | 58 | 100.0 | 29 | 100.0 | 73 | 100.0 | 30 | 100.0 | 43 | 100.0 |
| Median number of HE/MEs | 10 | 10 | 10 | 10 | 10 | 10 | ||||||
| Duration of HE/ME (length of longest HE/ME in days) | ||||||||||||
| 4–7 | 32 | 34.1 | 23 | 36.3 | 9 | 29.1 | 24 | 32.8 | 12 | 41.4 | 12 | 27.3 |
| 8–14 | 27 | 29.1 | 17 | 27.7 | 10 | 32.4 | 17 | 20.2 | 6 | 17.2 | 11 | 22.1 |
| 15+ | 29 | 36.8 | 19 | 36.0 | 10 | 38.4 | 32 | 47.0 | 12 | 41.4 | 20 | 50.6 |
| Total | 88 | 100.0 | 59 | 100.0 | 29 | 100.0 | 73 | 100.0 | 30 | 100.0 | 43 | 100.0 |
| Median length of longest HE/ME in days | 14 | 14 | 14 | 14 | 14 | 21 | ||||||
| Age of onset of HE/ME | ||||||||||||
| <16 | 53 | 44.2 | 34 | 40.0 | 19 | 54.9 | 45 | 44.6 | 14 | 32.2 | 31 | 53.3 |
| ≥16 | 53 | 55.8 | 39 | 60.0 | 14 | 45.1 | 45 | 55.4 | 25 | 67.8 | 20 | 46.7 |
| Total | 106 | 100.0 | 73 | 100.0 | 33 | 100.0 | 90 | 100.0 | 39 | 100.0 | 51 | 100.0 |
| Median age at onset of first HE/ME | 16 | 16 | 15 | 16 | 17 | 15 | ||||||
Slightly reduced n for some variables due to missing information.
n = unweighted number; % w = weighted row percentage; MDE = major depressive episode.
Table 3.
Course characteristics of unipolar and bipolar depression [n = 713 individuals with major depressive episode (MDE) at any assessment]
| Unipolar depression |
Bipolar depression |
|||||||
|---|---|---|---|---|---|---|---|---|
| No HE/ME n = 623a |
HE/ME n = 90a |
HE n = 39a |
ME n = 51a |
|||||
| n | % w | n | % w | n | % w | n | % w | |
| Number of MDEs | ||||||||
| 1 | 313 | 50.2 | 31 | 33.1 | 19 | 48.7 | 12 | 22.0 |
| 2 | 46 | 6.8 | 5 | 4.9 | 3 | 5.9 | 2 | 4.2 |
| 3 or more | 264 | 43.0 | 54 | 62.0 | 17 | 45.4 | 37 | 73.8 |
| Total | 623 | 100.0 | 90 | 100.0 | 39 | 100.0 | 51 | 100.0 |
| Median number of MDEs | 1 | 3 | 2 | 4 | ||||
| Duration of MDE (length of longest MDE in weeks) | ||||||||
| 2–5 weeks | 241 | 41.7 | 22 | 20.4 | 13 | 33.2 | 9 | 11.5 |
| 6–10 weeks | 98 | 17.2 | 23 | 28.4 | 9 | 19.0 | 14 | 34.9 |
| 11 or more weeks | 228 | 41.2 | 41 | 51.2 | 15 | 47.9 | 26 | 53.6 |
| Total | 567 | 100.0 | 86 | 100.0 | 37 | 100.0 | 49 | 100.0 |
| Median length of longest MDE in weeks | 8 | 12 | 8 | 12 | ||||
| Age of onset of MDE | ||||||||
| < 16 | 191 | 26.8 | 42 | 39.7 | 18 | 39.4 | 24 | 40.0 |
| ≥ 16 | 430 | 73.2 | 48 | 60.3 | 21 | 60.6 | 27 | 60.0 |
| Total | 621 | 100.0 | 90 | 100.0 | 39 | 100.0 | 51 | 100.0 |
| Median age at onset of first MDE | 18 | 16 | 17 | 16 | ||||
Slightly reduced n for some variables due to missing information.
HE = hypomanic episode; ME = manic episode; n = unweighted number; % w = weighted row percentage.
Among the total 90 bipolar cases with MDE and HE or ME, the first mood episode was hypomanic/manic in 45 cases (50.1%), with ME cases being more frequently temporally primary (n = 30/51, 57.6%) than HE cases (n = 15/39, 39.5%). A same-year MDE onset occurred equally as frequent in ME (n = 10/51, 21.8%) and HE (n = 9/39, 23.9%).
Impairment
There were no significant differences in severity of impairment due to ME between bipolar cases with ME and MDE and those with unipolar ME (severe impairment: 90.9% versus 78.0%). However, there were higher rates of impairment due to hypomania in bipolar HE/MDE as compared to unipolar HE (severe impairment: 60.3% versus 43.4%; OR = 3.01, 95% CI: 1.70–7.24, p = 0.001). Among unipolar HE/ME cases, impairment rates due to (hypo)mania did not significantly differ in subjects with versus without MinDE.
In terms of impairment due to depression, bipolar subjects with ME and MDE (but not HE and MDE) tended to be more severely impaired than unipolar depressed individuals (severe impairment: 96.1% versus 89.5%; OR = 2.90, 95% CI: 0.87–9.68, p = 0.084). Similar findings occurred when also considering MinDE.
Professional attention and treatment
Unipolar hypomania/mania cases were as likely to receive any treatment for HE/ME (hospitalization, treatment by doctor/other specialist, medication use) as bipolar cases (ME/MDE: 25% versus ME alone: 14.8%, p = 0.366; HE/MDE: 6.9% versus HE alone: 3.3%, p = 0.511). However, a trend for higher rates of hospitalizations for mania occurred in bipolar cases (ME and MDE) compared to unipolar ME cases (11.6% versus 1.8%; OR = 6.91, 95% CI: 0.78–61.03, p = 0.081).
Overall, depressive episodes received greater professional attention than did HE/ME. Bipolar cases with MDE and ME were more likely to receive any treatment for depression than unipolar depression cases (70.6% versus 45.6%; OR = 2.53, 95% CI: 1.24–5.16, p = 0.010). Among the treatments for depressive episodes, hospitalizations (16.4% versus 7.8%; OR = 2.26, 95% CI: 0.95–5.37, p = 0.065) and treatments by other healthcare professionals (psychologists, psychotherapists; 16.4% versus 14.5%; OR = 3.12, 95% CI: 1.19–8.19, p = 0.021) were overrepresented in bipolar cases with ME and MDE relative to unipolar depression cases. In contrast, bipolar cases with HE and MDE tended to have lower overall treatment rates for depression than unipolar depression cases (34.7% versus 45.6%; OR = 0.53, 95% CI: 0.26–1.10, p = 0.090). Considering MinDE as well, there were no differences in professional attention among HE/ME cases with MinDE in comparison to cases with MinDE alone.
Discussion
Using data from a large, representative community sample of subjects aged 14–24 that were followed over 10 years, the present investigation provides novel insights regarding the incidence patterns of mood episodes and mood disorders, the risk for conversion from unipolar disorder to BD, and the clinical and treatment characteristics of unipolar and bipolar mood disorders in the critical time period of adolescence and young adulthood.
Cumulative incidence of mood episodes and mood disorders in the first three decades of life
Unlike previous contributions, our study provides an incidence characterization of mood episodes and mood disorders from puberty into early adulthood. The cumulative incidence estimates of HE and ME, and of DSM-IV BD up to age 33, were higher than the lifetime prevalence estimates reported by previous cross-sectional community studies, which covered a considerably broader age range (e.g., 28, 29). Yet they resemble the findings reported by Angst et al. (30) in their longitudinal cohort study, providing support for the suggestion that cross-sectional lifetime studies may underestimate the prevalence of ME and HE. Consistent with earlier studies in adult samples (e.g., 12), peak onset for mania was in the mid-teen period. Our finding that manic cases revealed numerous indications of being clinically severe (impairment and course characteristics) underlines the credibility of these mania cases. For hypomania, the incidence pattern showed two peak onset periods: one as early as childhood, and then a second, sharper increase in adolescence. Here caution is warranted because of the challenges inherent in assessing hypomania in childhood and early adolescence, and in particular because the childhood assessments were done retrospectively.
The estimated cumulative incidence for (unipolar) major depression up to age 33 was higher than retrospective lifetime rates from adult community surveys (4, 28), but in the range of estimates from multiwave prospective studies (12, 31). A further considerable proportion meets criteria for MinDE. First onsets of depression occurred rarely in childhood. Quite different from HE/ME, depression was characterized by a fairly steady rate of new-onset cases from early adolescence up to the mid-30s. Our findings are consistent with previous clinical studies that report the mean age of onset of unipolar depression in the mid- to late-20s (5) and of BD within the age range of 15–19 years [median age of onset of 17.5 years (see 32)]. They are also in agreement with other epidemiological studies in comparable age groups (4, 33, 34) that typically reveal slightly lower mean onsets than do clinical samples.
Particularly noteworthy is our finding of relatively high rates of unipolar mania/hypomania without indication for threshold DSM-IV MDE in the first three decades of life. The occurrence of unipolar mania has been rarely examined and its existence remains controversial. Our findings, however, are in agreement with some other epidemiological longitudinal studies (35, 36) as well as recent long-term follow-up data (2), indicating considerable rates of unipolar (hypo)mania. Although these rates substantially decreased when additionally considering MinDE or dysthymia, further explorations of unipolar (hypo)mania are warranted. In particular, the unipolar mania cases without MDE did not significantly differ from bipolar cases in terms of clinical and course characteristics, impairment severity, professional help seeking, and treatment for the ME, suggesting that these cases are clinically relevant. This conclusion holds when minor depression is also considered, because these characteristics did not significantly differ in unipolar mania cases with and without minor depression. Because of the restricted follow-up period and the relatively young age of our sample, however, these cases might be best diagnosed as ‘provisional unipolar mania’, even though we ruled out the possibility that the cases were overrepresented in younger age groups that had not passed the first core incidence period for depression in a similar way as older individuals.
Conditional probability and risk for onset of mood episodes
Consistent with traditional thinking, we observed considerable rates of subsequent MDE onsets among primary hypomania (15.8%) and particularly mania cases (49.6%), with no indication that conversion to ‘true’ BD differed by age of (hypo)mania onset. These proportions increased when subsequent minor depression (44.3% of HE and 75.6% of ME cases developed MDE or MinDE) was also considered, or when projecting the lifetime risk (as opposed to the observed rates) by using survival analyses (27.8% of primary HE and 71.2% of primary ME cases were estimated to have developed MDE by age 33). Angst and Zimmermann (37) reported a conversion rate of 2.7 per year in patients whose disorder started with mania. Of note, compared to individuals without (hypo)mania, the depression onset risk was significantly increased only in mania but not hypomania cases.
In contrast, the conversion rate from unipolar depression to bipolar depression appears to be overall relatively low. A total of 3.6% of all initial MDD cases were observed to have a subsequent first ME or HE, with indications that the conversion risk is remarkably high (9%) in early-onset depression (< 17 years). In a recent analysis of a sample of unipolar depressive and bipolar patients, Benazzi (38) showed a close association between an early onset of the mood disorder and bipolarity (history of hypomania, family history of mania/hypomania). Of note, the overall projected estimated (as opposed to the observed rate) conversion risk up to age 33 is about 10% in both our patients with initial MDD and in subjects with MinDE but no MDE, and thus substantial for the age range considered. Although 90% did not convert in the observation period, and despite our finding that the risk rates were not significantly higher when compared to subjects with no depression, this finding confirms cautionary notes by some authors (11, 39) who consider the diagnosis of unipolar depression in adolescence as provisional. Angst and colleagues (40) reported a conversion rate of 39% in patients with unipolar depression followed prospectively for an average of 20 years from the onset of the disorder. As the age range and follow-up period in our study was restricted to the mid-30s, further conversions are conceivable, yet rates are expected to be very limited as the core risk period for first (hypo)mania onset appears to be adolescence. Unfortunately, due to the fairly low number of conversion cases, our study was not sufficiently powered to determine whether these cases reveal substantially different course characteristics that might help to identify early cases at risk. It is unlikely that epidemiological research will provide useful information in that way. A combination of retrospective assessment and prospective observation of children and adolescents at risk, as determined by prodromal syndromes or newly diagnosed depression, should provide more opportunities. Also, studies focussing on those with a familial risk for BD may be beneficial.
Clinical and treatment characteristics of unipolar and bipolar mood disorders
Consistent with results from Perlis et al. (41), our study showed evidence that unipolar and bipolar depression differ with respect to course, impairment, and treatment. Individuals with ME and MDE in particular reported a greater number and duration of depressive episodes and earlier depression onset than unipolar depression cases. Bipolar ME/MDE subjects, unlike bipolar HE/MDE cases, were also more frequently severely impaired due to depression than were unipolar depressed individuals and received inpatient and outpatient treatment for depression more frequently. This underscores the fact that bipolar I disorder is a particularly severe and clinically significant condition.
In contrast to our finding of more adverse clinical and treatment characteristics in bipolar versus unipolar depression, our characterization of (hypo)manic episodes suggests that bipolar cases do not significantly differ from unipolar mania cases in terms of critical mania course characteristics and impairment as well as treatment due to mania. This finding holds even when additionally considering minor depression, providing support for the validity of our unipolar mania group. Despite the fact that the size of this group was small compared to unipolar and bipolar depression, together with our finding that (hypo)mania receives, in general, little professional attention and treatment, these findings indicate the strong need to further explore this patient group in terms of special diagnostic and treatment needs.
Limitations
First, we examined the incidence patterns and conversion rates only up to the mid-30s; thus, no conclusions can be drawn for ‘true lifetime’ incidence and conversion rates. Second, our data did not allow for analyses regarding temporal order of onset of (hypo)manic and depressive episodes emerging within the same year; our conversion rates refer to cases with onsets in different years (minimum one year). Third, the symptom and diagnostic assessment was exclusively based on a standardized diagnostic interview (DIA-X/M-CIDI) administered by trained clinical interviewers (psychologists or MDs), with the limitation of imperfect reliability and validity. Fourth, despite the prospective longitudinal design of the EDSP study, data are based on retrospective recall of participants for the time before baseline assessment and variable time intervals between the respective follow-up interviews. Fifth, some of the subgroup comparisons were based on small numbers, and thus should be interpreted with caution. Finally, our analyses were conducted by strictly applying the DSM-IV criteria as operationalized in the DIA-X/M-CIDI. We deliberately did not manipulate the threshold definitions of mood episodes, with the exception that we included additional analyses on the research category of minor depression. We did not examine overlap with cyclothymia or various types of personality disorders because these data were not available in our study.
Conclusions
Mood episodes are frequent conditions among youth from the community, with adolescence being the core incidence phase for mania and hypomania, whereas depression incidence continues into the third decade of life. Risk of ‘conversion’ to BD in the course of initial unipolar depression is limited, but is particularly elevated among adolescent-onset depression cases. In contrast, initial mania cases frequently develop depression. However, there is also evidence for the significance of a (small) group of patients remaining unipolar (hypo)manic at least up to their mid-30s. In particular, unipolar mania cases were found to have similar clinical and course characteristics of mania as bipolar cases. Further research is needed to replicate these findings, especially as our study indicates particularly low treatment rates for this patient group that may require more specific diagnostic and professional attention. Overall, our study suggests that both unipolar and bipolar mood disorders seem to be more frequent than previously thought in adolescence and young adulthood, a time period when both the recognition and the intervention rates by the healthcare system have remained relatively low.
Acknowledgements
This work is part of the Early Developmental Stages of Psychopathology (EDSP) study which, is funded by the German Federal Ministry of Education and Research (BMBF; project no. 01EB9405/6, 01EB 9901/6, EB01016200, 01EB0140, and 01EB0440). Part of the field work and analyses were also additionally supported by grants of the Deutsche Forschungsgemeinschaft (DFG; project no. LA1148/1-1, WI2246/1-1, WI709/7-1, and WI709/8-1).
Principal investigators of the EDSP study are Hans-Ulrich Wittchen and Roselind Lieb. Both take responsibility for the integrity of the study data. All authors and coauthors had full access to all study data. Data analysis and manuscript preparation were completed by the authors and coauthors of this article, who take responsibility for its accuracy and content. Core staff members of the EDSP group are: Kirsten von Sydow, Gabriele Lachner, Axel Perkonigg, Peter Schuster, Michael Höfler, Holger Sonntag, Tanja Brückl, Elzbieta Garczynski, Barbara Isensee, Agnes Nocon, Chris Nelson, Hildegard Pfister, Victoria Reed, Barbara Spiegel, Andrea Schreier, Ursula Wunderlich, Petra Zimmermann, Katja Beesdo, and Antje Bittner. Scientific advisors are Jules Angst (Zurich), Jürgen Margraf (Basel), Günther Esser (Potsdam), Kathleen Merikangas (NIMH, Bethesda), Ron Kessler (Harvard, Boston), and Jim van Os (Maastricht).
We thank Hans-Ulrich Wittchen for his helpful comments on earlier versions of this manuscript.
Footnotes
The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manuscript.
References
- 1.Cuellar AK, Johnson SL, Winters R. Distinctions between bipolar and unipolar depression. Clin Psychol Rev. 2005;25:307–339. doi: 10.1016/j.cpr.2004.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harish T, Grover S, Basu D. Recurrent unipolar mania: does it warrant a separate nosological status? German J Psychiatry. 2005;8:8–15. [Google Scholar]
- 3.Goodwin GM, Anderson I, Arango C, et al. ECNP consensus meeting. Bipolar depression. Eur Neuropsychopharmacol. 2008;18:535–549. doi: 10.1016/j.euroneuro.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med. 1997;27:1079–1089. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7:3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 6.Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- 8.Bijl RV, Ravelli A, van ZG. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 9.Ten Have M, Vollebergh W, Bijl R, Nolen WA. Bipolar disorder in the general population in The Netherlands (prevalence, consequences and care utilisation): results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) J Affect Disord. 2002;68:203–213. doi: 10.1016/s0165-0327(00)00310-4. [DOI] [PubMed] [Google Scholar]
- 10.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 11.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- 12.Bijl RV, DE GR, Ravelli A, Smit F, Vollebergh WA. Gender and age-specific first incidence of DSM-III-R psychiatric disorders in the general population. Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 2002;37:372–379. doi: 10.1007/s00127-002-0566-3. [DOI] [PubMed] [Google Scholar]
- 13.Wittchen HU, Mhlig S, Pezawas L. Natural course and burden of bipolar disorders. Int J Neuropsychopharmacol. 2003;6:145–154. doi: 10.1017/S146114570300333X. [DOI] [PubMed] [Google Scholar]
- 14.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med. 1998;28:109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- 15.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 16.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60:991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 17.Howland RH, Schettler PJ, Rapaport MH, et al. Clinical features and functioning of patients with minor depression. Psychother Psychosom. 2008;77:384–389. doi: 10.1159/000151519. [DOI] [PubMed] [Google Scholar]
- 18.Wittchen HU, Perkonigg A, Lachner G, Nelson CB. Early developmental stages of psychopathology study (EDSP): objectives and design. Eur Addict Res. 1998;4:18–27. doi: 10.1159/000018921. [DOI] [PubMed] [Google Scholar]
- 19.Lieb R, Isensee B, von Sydow K, Wittchen HU. The Early Developmental Stages of Psychopathology Study (EDSP): a methodological update. Eur Addict Res. 2000;6:170–182. doi: 10.1159/000052043. [DOI] [PubMed] [Google Scholar]
- 20.Wittchen HU, Pfister H. DIA-X-Interviews: Manual für Screening-Verfahren und Interview Interviewheft Längs-schnittuntersuchung (DIA-X-Lifetime); Ergänzungsheft (DIA-X-Lifetime); Interviewheft Querschnittuntersuchung (DIA-X-12 Monate); Ergänzungsheft (DIA-X-12Monate); PC-Programm zur Durchführung des Interviews (Längsund Querschnittuntersuchung); Auswertungsprogramm. Frankfurt: Swets & Zeitlinger; 1997. [Google Scholar]
- 21.Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI) Soc Psychiatry Psychiatr Epidemiol. 1998;33:568–578. doi: 10.1007/s001270050095. [DOI] [PubMed] [Google Scholar]
- 22.Reed V, Gander F, Pfister H, et al. To what degree the Composite International Diagnostic Interview (CIDI) correctly identify DSM-IV disorders? Testing validity issues in a clinical sample. Int J Methods Psychiatr Res. 1998;7:142–155. [Google Scholar]
- 23.Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 24.Wittchen HU, Lieb R, Schuster P, Oldehinkel AJ. When is onset? Investigations into early developmental stages of anxiety and depressive disorders. In: Rapoport JL, editor. Childhood Onset of “Adult” Psychopathology, Clinical and Research Advances. Washington: American Psychiatric Press; 1999. pp. 259–302. [Google Scholar]
- 25.Stata Cooperation. Stata Statistical Software: Release 9.2. College Station TX: Stata Corporation; 2008. [Google Scholar]
- 26.Royall RM. Model robust confidence intervals using maximum likelihood estimators. Stat Rev. 1986;54:221–226. [Google Scholar]
- 27.Therneau TM, Grambsch PM. Modeling Survival Data – Extending the Cox Model. New York: Springer; 2000. [Google Scholar]
- 28.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 29.Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rossler W. Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J Affect Disord. 2003;73:133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 31.Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–151. doi: 10.1016/s0165-0327(98)00142-6. [DOI] [PubMed] [Google Scholar]
- 32.Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry. 2002;63:120–125. doi: 10.4088/jcp.v63n0206. [DOI] [PubMed] [Google Scholar]
- 33.Lewinsohn PM, Seeley JR, Buckley ME, Klein DN. Bipolar disorder in adolescence and young adulthood. Child Adolesc Psychiatr Clin N Am. 2002;11:461–475. doi: 10.1016/s1056-4993(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 34.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000;2:281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- 35.Abrams R, Taylor MA, Hayman MA, Krishna NR. Unipolar mania revisited. J Affect Disord. 1979;1:59–68. doi: 10.1016/0165-0327(79)90025-9. [DOI] [PubMed] [Google Scholar]
- 36.Solomon DA, Leon AC, Endicott J, et al. Unipolar mania over the course of a 20-year follow-up study. Am J Psychiatry. 2003;160:2049–2051. doi: 10.1176/appi.ajp.160.11.2049. [DOI] [PubMed] [Google Scholar]
- 37.Angst J, Zimmermann P. The manic wing of the bipolar spectrum. European Psychiatric Review. 2008;1:19–21. [Google Scholar]
- 38.Benazzi F. Classifying mood disorders by age-at-onset instead of polarity. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:86–93. doi: 10.1016/j.pnpbp.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 39.Akiskal HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J Am Acad Child Adolesc Psychiatry. 1995;34:754–763. doi: 10.1097/00004583-199506000-00016. [DOI] [PubMed] [Google Scholar]
- 40.Angst J, Sellaro R, Stassen HH, Gamma A. Diagnostic conversion from depression to bipolar disorders: results of a long-term prospective study of hospital admissions. J Affect Disord. 2005;84:149–157. doi: 10.1016/S0165-0327(03)00195-2. [DOI] [PubMed] [Google Scholar]
- 41.Perlis RH, Brown E, Baker RW, Nierenberg AA. Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. Am J Psychiatry. 2006;163:225–231. doi: 10.1176/appi.ajp.163.2.225. [DOI] [PubMed] [Google Scholar]