Abstract
Introduction
Although early post-surgical over-correction for exotropia is widely advised, post-operative drift has not been well quantified in concomitant exotropia, and has not been described specifically with A and V patterns. While such patterns have been proposed to result from abnormal locations of the rectus muscle pulleys, others have suggested that A and V patterns may result from the disruption of fusion arising from exotropia itself.
Methods
We prospectively performed Hess screen analysis in 20 exotropic patients (mean age 42 ± 16 yrs) before and two to six times after strabismus surgery, with a post-operative follow-up of 2–108 weeks. Primary surgery cases included medial rectus resection (2) and lateral rectus recession (10), combined resection/recession (6), and superior oblique tenectomy (2). Alignment trends in primary and secondary gazes were analyzed for concomitant, pattern, and re-operated subgroups. Results were also analyzed by type of surgery performed.
Results
Mean pre-operative central gaze exotropia was 8.6 ± 7.1°. Twelve cases were concomitant, while 8 exhibited A or V patterns. Twelve cases were re-operations. In initial surgery for concomitant exotropia, there was a well-defined exotropic drift approaching 5° by 30 weeks post-operatively (linear regression, r = 0.43, p = 0.01). There was similar exo drift in re-operations. However, in pattern exotropia, post-operative drift was more variable, with mean esotropic drift of approximately 5° (r = 0.18, p = 0.43). For all patients, final post-operative central gaze exotropia was 1.9 ± 5.8°, with significant pattern collapse (p < 0.01).
Discussion
Post-operative exo-shift of about 5° occurs in initial and re-operated concomitant exotropia. However, in A and V patterns, there is no definitive direction of post-operative drift, suggesting that pattern strabismus may be more likely due to mechanical factors in the orbit than to neural factors associated with fusion disruption.
Conclusions
Alignment following strabismus surgery differs in concomitant vs. pattern exotropia. Initial over-correction of about 5° is advisable for concomitant exotropia, but should be avoided in A and V patterns.
Keywords: Concomitant exotropia, pattern exotropia, strabismus surgery, postoperative drift, binocular alignment, over-correction
INTRODUCTION
It has long been recognized that exotropia (XT) tends to recur after strabismus surgery (Eino & Kraft, 1997; Lee & Lee, 2001; Raab & Parks, 1969), accounting for its relatively low surgical success rate. Several studies have addressed the divergent post-operative drift after XT surgery, and have found that long-term post-operative alignment is better when there is over-correction in the very early period following procedures including bilateral lateral rectus recession (Raab & Parks, 1969), unilateral lateral rectus recession combined with medial rectus resection (Lee & Lee, 2001), and various approaches using adjustable sutures (Eino & Kraft, 1997; Lee & Lee, 2001; Raab & Parks, 1969; Weston et al., 1991). Initial over-correction also appears favorable in surgery for consecutive XT (Langmann et al., 2005).
Many of the studies detailing XT post-operative drift have excluded patients with A or V pattern strabismus. Less attention has been given to post-operative drifts after surgical intervention for pattern XT. Thus, there is a paucity of data concerning immediate post-operative alignment goals or post-operative drift in pattern strabismus. In addition, the underlying mechanism of pattern strabismus is still under debate, and studies of surgical outcomes may further elucidate whether the underlying mechanism is a mechanical or a neural factor. Miller and Guyton (1994) suggest that abnormal ocular torsion is the primary problem in pattern strabismus, and that patients are predisposed to abnormal ocular torsion by a loss of fusion from strabismus over-correction. However, others have argued that the primary lesion is mechanical, either from dysfunctional rectus and oblique muscles (Dunlap, 1961), or from dynamic instability of rectus pulleys (Oh et al., 2002).
This study prospectively evaluated the results of surgery for XT using serial Hess screen tests as a measurement of alignment. The aim was to determine if long-term results are influenced by the presence of incomitance, re-operation, and surgical method.
METHODS
Patients
This study was prospectively approved by the local Institutional Review Board and was compliant with relevant privacy laws. All subjects gave written informed consent prior to participation in conformity with the Declaration of Helsinki. Subjects underwent Hess screen testing of binocular alignment in the same laboratory from 1989 through 2006. For Hess screen testing, subjects’ heads were placed on a forehead- and chin-rest 50 cm from a ruled tangent screen containing short line targets composed of three red light-emitting diodes (LEDs). The laboratory was otherwise dimly lit. Each set of LEDs could be illuminated individually under infra-red remote control of the operator. The fixating eye viewed the linear LED targets individually through a red lens, while the following eye, viewing through a green lens, was used to guide the location of a projected green target streak. Neither eye could see anything but the corresponding lighted target. With the two eyes thus dissociated, the subject was instructed to superimpose the projected green streak upon the red line or LEDs at each target location. Targets were central, and at ±15° and ±30° horizontal and vertical eccentricities. While a total of 25 targets could be illuminated individually, in practice the extreme corners of the array could not be fixated binocularly by the majority of subjects due to occlusions by the brow and nose, so binocular alignment was systematically tested at only 21 target locations. For each test, each eye was tested in the fixating and following roles by reversing the red-green spectacle lenses. For each fixation location by each eye, the operator marked on a pre-printed recording sheet the horizontal and vertical position of the light streak projected by the subject to record binocular misalignment. All Hess screen testing was done by a technician who was unaware of the purpose of the study.
Surgery was done by one of two surgeons, who chose the surgical technique based on his preference. At the time of surgery, the surgeons were unaware of the study. Subjects were included who had XT requiring surgical correction, and who completed a pre-operative Hess screen test, a post-operative Hess screen test within 5 days of surgery, and at least one Hess screen test after the first post-operative week. Subjects were excluded if they had vertical deviations >5PD, or cranial nerve palsies, strabismic suppression or anomalous retinal correspondence precluding reliable Hess screen testing, no potential for binocular vision or fusion (determined by various tests for stereopsis), or constant XT.
Alignment Analysis
Deviation from intended gaze was recorded in degrees for each eye in central position, as well as in 30° up, down, left, and right gaze using the Hess screen data. Hess screen results were translated to degrees of deviation using estimation to a single degree from the 5° screen markings. Exo-deviation was labeled as positive (+), while eso-deviation was labeled as negative (−). Deviations were then graphed as functions of time for individual subjects, as well as for the following cohorts: all patients with concomitant strabismus, all patients with pattern strabismus, all patients who were undergoing a re-operation, all patients who were undergoing primary surgery, and in cohorts according to surgical method. To facilitate comparison, follow-up was limited to 30 weeks as most patients did not have lengthier follow-up. Linear regressions were then fit to the data to delineate secular trends. Linear regression was deemed significant if p < 0.05 using ANOVA.
Statistical Analysis
Mean pre-operative and post-operative deviations, measured in degrees, were compared using Student’s paired t-test. Mean squared error (MSE) deviation was used to classify cases as concomitant or pattern. MSE was calculated as the mean of the square of the difference in deviation between up or down-gaze and primary gaze, i.e.:
Cases were considered concomitant if the MSE was less than 25 degrees2, (i.e. the average difference in deviation from central gaze was less than 5°). Post-operative pattern was determined by comparing the mean MSE of pattern XT cases pre- and post-operatively using Student’s paired t-test. Results were deemed statistically significant if p < 0.05.
Linear regression slope was used to represent the rate and direction of post-operative drift in each patient. A sign test was utilized to compare the probability of a positive or negative slope within each group.
RESULTS
Subjects
Twenty cases (18 patients) met the inclusion criteria (2 patients underwent 2 surgical interventions that met the study inclusion criteria). Subjects’ ages ranged from 13 to 72 years (mean 42 ± 16 years; mean within concomitant group: 48 ± 17 years and in pattern group: 32 ± 7 years). The mean pre-operative XT in primary gaze was 8.6 ± 7.1°. Among patients with concomitant XT, the mean deviation was 9.7 ± 6.5°; in the pattern group, the mean deviation was 8.2 ± 8° (p = 0.4). Smaller angle deviations were operated on if the patient was bothered by diplopia in any direction of gaze. The last post-operative follow-up Hess screen test ranged from 2 to 108 weeks (mean follow up 24.5 ± 28 weeks). The primary surgical techniques included medial rectus resection (2 cases), lateral rectus recession (10 cases), combined medial rectus resection and lateral rectus recession (6 cases), and superior oblique tenectomy (2 cases). All cases with pattern strabismus and rectus surgery underwent rectus transposition in an attempt to collapse their pattern. Eight cases exhibited clinical A (5) or V (3) patterns, while 12 cases were vertically concomitant. Twelve cases were re-operations for residual XT. Individual patient characteristics including surgical technique, degree of fusion, and presence of diplopia are summarized in Table 1.
TABLE 1.
Patient characteristics
| Patient Number | Pre-operative XT (degrees) | Intermittent XT Type | Surgical Technique | Degree of pre-operative binocularity, pre/post--operative diplopia | Slope of linear regression |
|---|---|---|---|---|---|
| 1 | 25 | V pattern | 5 mm BMR resection with inferior transposition | 400 arcsec + pre-operative diplopia; − post-operative diplopia | (0) |
| 2 | 17 | V pattern | 6 mm LLR recession with superior transposition | 400 arcsec − pre-operative diplopia; − post-operative diplopia | (0) |
| 3 | 2 | A pattern | BSO tenectomy | 60 arcsec − pre-operative diplopia; − post-operative diplopia | (+) |
| 4 | 2 | A pattern | 3.5 mm BLR recession with inferior transposition | 60 arcsec − pre-operative diplopia; − post-operative diplopia | (−) |
| 5 | 10 | V pattern | 4 mm BLR resection with superior transposition | 400 arcsec + pre-operative diplopia; + post-operative diplopia | (+) |
| 6 | 1 | A pattern | 4 mm BLR resection with superior transposition | 40 arcsec + pre-operative diplopia; +post-operative diplopia | (−) |
| 7 | 9 | A pattern | BSO tenectomy | 40 arcsec + pre-operative diplopia; +post-operative diplopia | (+) |
| 8 | 1 | A pattern | 5 mm BLR recession and superior transposition | 100 arcsec + pre-operative diplopia; − post-operative diplopia | (−) |
| 9 | 7 | Vertically Concomitant | 4 mm RLR recess, 6 mm RMR resect | 400 arcsec + pre-operative diplopia; − post-operative diplopia | (+) |
| 10 | 5 | Vertically Concomitant | 6 mm RLR recession, 4 mm RMR resection | 50 arcsec + pre-operative diplopia; − post-operative diplopia | (+) |
| 11 | 5 | Vertically Concomitant | 4 mm RLR recession, 3.5 mm RMR resection | 40 arcsec − pre-operative diplopia; − post-operative diplopia | (+) |
| 12 | 5 | Vertically Concomitant | 4 mm BLR recession | 40 arcsec − pre-operative diplopia; − post-operative diplopia | (+) |
| 13 | 10 | Vertically Concomitant | 4.5 mm BLR recession | 400 arcseconds + pre-operative diplopia; + post-operative diplopia | (+) |
| 14 | 10 | Vertically Concomitant | 6 mm LLR recession, 4 mm LMR resection | 40 arcsec − pre-operative diplopia; +post-operative diplopia | (0) |
| 15 | 9 | Vertically Concomitant | 3 mm RMR resection, 5 mm RLR recession | 40 arcsec − pre-operative diplopia; + post-operative diplopia | (+) |
| 16 | 5 | Vertically Concomitant | 3 mm BLR recession | 50 arcsec − pre-operative diplopia; − post-operative diplopia | (+) |
| 17 | 10 | Vertically Concomitant | 3.5 mm BMR resection | 100 arcsec − pre-operative diplopia; + post-operative diplopia | (+) |
| 18 | 25 | Vertically Concomitant | 4 mm BLR recession | 400 arcsec + pre-operative diplopia; − post-operative diplopia | (+) |
| 19 | 5 | Vertically Concomitant | 8.5 mm BLR recession | 40 arcsec − pre-operative diplopia; − post-operative diplopia | (+) |
| 20 | 8 | Vertically Concomitant | 6 mm RLR recession, 9 mm RMR resection | 400 arcsec + pre-operative diplopia; − post-operative diplopia | (+) |
Arcsec (arcseconds), BMR (bilateral medial rectus), BLR (bilateral lateral rectus), RMR (right medial rectus), LMR (left medial rectus), RLR (right lateral rectus), LLR (left lateral rectus), BSO (bilateral superior oblique).
Hess Screen Results
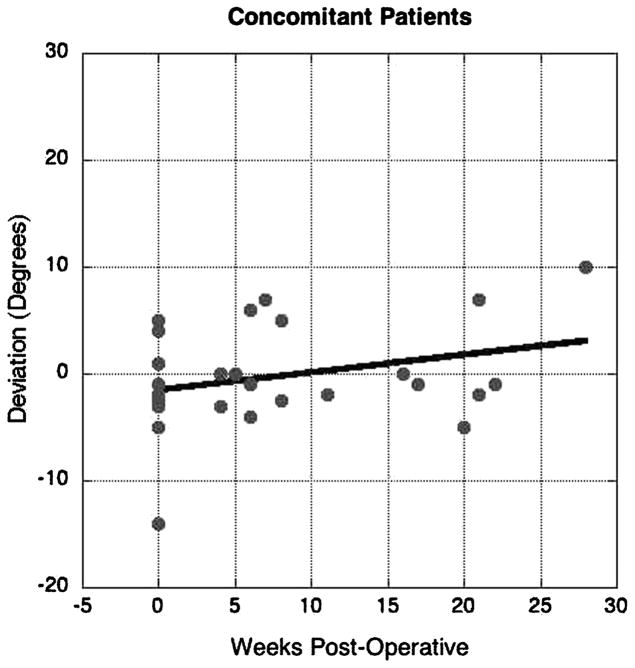
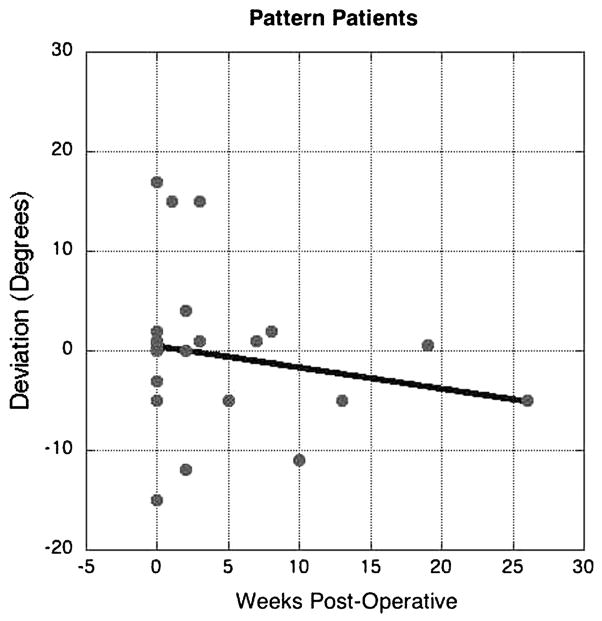
Hess screen test results were analyzed and graphed individually for each subject and cohort. Data were pooled for individual patients according to concomitance of strabismus (Figs. 1 and 2), and were also segregated as cohorts made up of concomitant (Fig. 3) vs pattern (Fig. 4) deviations. Figures 1 and 3 show that the majority of subjects with concomitant XT drifted in the XT direction (r = 0.43, p = 0.01). Figures 2 and 4 demonstrate that many of the pattern subjects did not drift in the XT direction, and the group overall exhibited a non-statistically significant trend toward a convergent drift (r = 0.18, p = 0.43) Cohorts were also analyzed for re-operations vs. primary surgery, and by individual surgical techniques (graphs not shown). There was no significant effect of surgical technique. In addition, we could not identify a significant difference between groups with small vs. large pre-operative deviations.
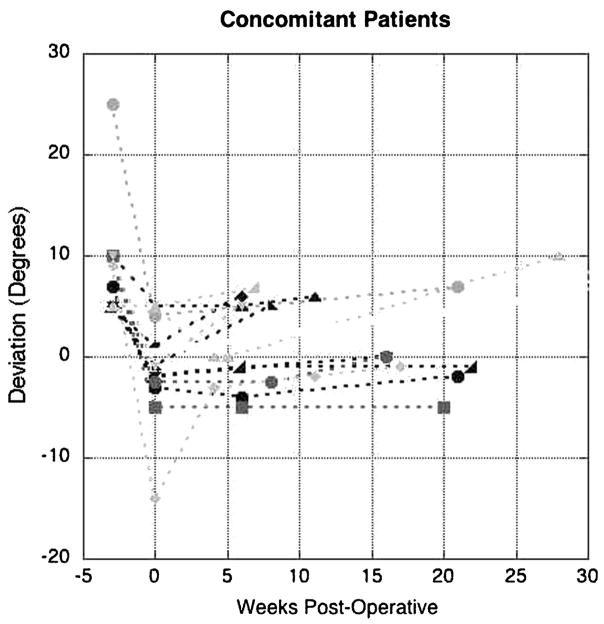
Figure 1.
Individual post-operative alignment for cases of concomitant exotropia. Binocular alignment in central gaze for individual patients showing post-operative drift from day 0 (first post-operative measurement) through the long-term follow-up period. The majority of the patients drifted in the XT direction over the first 30 weeks.
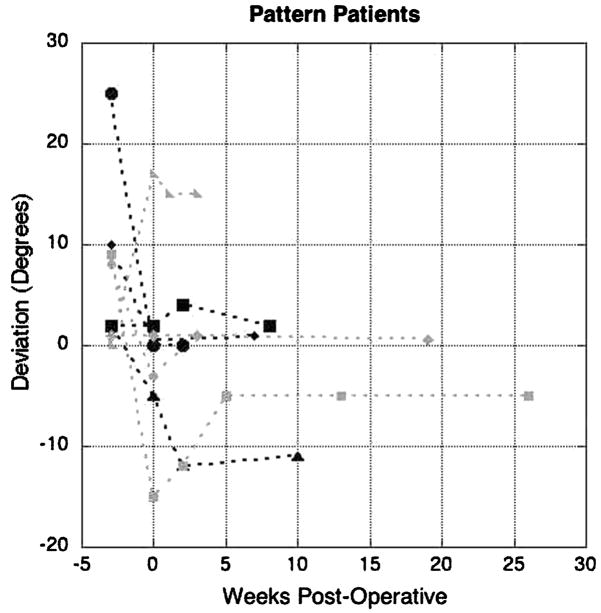
Figure 2.
Individual post-operative course for cases of pattern exotropia. Binocular alignment in central gaze for individual patients detailing the course of post-operative drift from day 0 (first post-operative measurement) through the long-term follow-up period. There was no clear trend associated with the post-operative drift over the first 30 weeks.
Figure 3.
Cohort of patients with concomitant exotropia. Scatter plot of all individual measurements of deviation for each case of concomitant XT. A polynomial regression demonstrates a general trend toward an XT drift (r = 0.43, p = 0.01).
Figure 4.
Cohort of patients with pattern exotropia. Scatter plot of all individual measurements of deviation for each case of pattern XT. A polynomial regression demonstrates a general trend toward no or an esotropic drift (r = 0.18, p = 0.43).
The data summarized in Table 2 indicate that there was a decrease in the mean final XT for all cohorts of subjects. There was also a significant decrease in the MSE indicating a collapse of the “A” or “V” pattern in the pattern cases (p < 0.01), whereas the MSE did not change significantly in concomitant cases. Using linear regression, a slope of post-operative drift was calculated for each patient (demonstrated in Table 1), and then averaged for each cohort (Table 3). For subjects with concomitant XT, the average regression slope was +0.4 degrees/week, signifying XT drift. For subjects with pattern XT, the regression slope was −0.1 degrees/week, signifying esotropic (ET) drift. The sign test indicated that XT drift was significantly more common that ET drift in subjects with concomitant XT (p < 0.01), but neither direction of drift was significantly more common for subjects with pattern XT (p = 0.727).
TABLE 2.
Exotropia and mean squared error (MSE) of alignment
| Cohort (Number of cases) | Pre-Operative Exotopia | Immediate Post-Operative Exotropia | Final Post-Operative Exotropia P-Value (Pre-Operative vs Final Deviation) | Pre-Operative MSE (degrees2) | Immediate Post-Operative (degrees2) | Final Post-Operative MSE (degrees2) P-Value (Pre-Operative vs Final MSE) |
|---|---|---|---|---|---|---|
| Comitant (12) | 9.7 ± 6.5° | −1.6 ± 5.1° | 2.4 ± 4.9° (p < 0.01) | 10 ± 10 | 15 ± 18 | 13 ± 18 (p = 0.66) |
| Pattern (8) | 8.2 ± 8° | 0.1 ± 8.8° | 0.3 ± 7.3° (p = 0.057) | 78 ± 42 | 25 ± 32 | 28 ± 16 (p < 0.01) |
| Re-Operations (12) | 8.1 ± 5.9° | −2.5 ± 5.8° | 0.8 ± 5.6° (p < 0.01) | 26 ± 37 | 17 ± 19 | 15 ± 18 (p = 0.36) |
| Primary Surgery (8) | 9.0 ± 9.5° | 2 ± 6.8° | 3.6 ± 6.2° (p = 0.1) | 54 + 48 | 23 ± 32 | 25 ± 20 (p = 0.06) |
TABLE 3.
in concomitant and pattern exotropia
| Comitance | Mean Rate of Exotropic Drift (degrees/week) | Cases Exhibiting Exotropic Drift | Cases Exhibiting Esotropic Drift | P-value (Sign Test) |
|---|---|---|---|---|
| Comitant | +0.4 ± 0.4 | 11 | 1 | <0.01 |
| Pattern | −0.1 ± 0.3 | 3 | 5 | 0.727 |
DISCUSSION
Multiple authors have asserted that over-correction is the desired immediate post-operative outcome in surgery for XT (Lee & Lee, 2001; Raab & Parks, 1969; Scott et al., 1981; Souza-Dias & Uesugui, 1993). Knapp suggested that over-correction may precipitate a nasal scotoma, which would thus reduce temporal suppression and impede the relapse of XT (Knapp & Hardesty, 1960). Initial overcorrection has also been proposed to stimulate fusional divergence (Lee & Lee, 2001).
Raab & Parks (1969) explored the post-operative XT drift in patients with intermittent XT who underwent lateral rectus recessions in both eyes. These authors reported that an initial over-correction of 11–20PD gave the most satisfactory long-term result, defined as a deviation of <10Δ in primary position in the fifth to eighth post-operative week. Later, other authors (Mc-Neer, 1987; Scott et al., 1981) reported a smaller postoperative drift, 4–14Δ and 0–10Δ, respectively. Other surgical methods have also been investigated, including combined medial rectus resection with lateral rectus recession, for which a somewhat smaller overcorrection of 5–10Δ was recommend (Souza-Dias & Uesugui, 1993).
Exotropic drift of 4–5Δ (Weston et al., 1991) or 3–7Δ (Eino & Kraft, 1997) has been reported using adjustable suture techniques. In patients operated for consecutive XT, post-operative XT drifts from 4Δ (Weston et al., 1991) to 7Δ (Donaldson et al., 2004; Langmann et al., 2005) have been reported. However, occasional studies have disputed the apparent XT drift when particular surgical methods were employed. For example, in a study of unilateral lateral rectus recession for intermittent XT, there was no significant post-operative drift in either direction (Olitsky, 1998). Notably, in most of the foregoing studies, patients with A or V pattern XT were excluded. In addition, many of these previous studies differ from our current study in that they quantified drift at a single time point, and did not utilize standardized methods such as the Hess screen test.
Using Hess screen testing, our study confirms prior reports of an XT drift regardless of surgical technique in patients with concomitant XT, and extends these reports to define the rate of change and behavior of the drift. Beyond this, we report the novel finding that “A” or “V” pattern XT does not appear to demonstrate similar post-operative drift. When the individual cases were analyzed using linear regression, XT drift was statistically significant for concomitant patients. Conversely, there was no significant drift in patients with pattern XT, with a general trend towards minimal esotropic drift. Pattern collapse was defined as statistically significant decrease in the MSE. Subjects with concomitant XT had no significant change in MSE following surgery, indicating that there was no change in the comitance of their strabismus. Subjects with pattern XT demonstrated a significant pattern collapse, with a decrease in the MSE from appr ximately 78 degrees2 to approximately 28 degrees2.
The results of this study, if corroborated by larger studies in the future, may suggest that the underlying mechanism of pattern strabismus is more likely mechanical than neurally based. Whereas concomitant XT, which is most likely neurally based, drifts outwards over time, our pattern patients did not behave the same way, thereby suggesting that perhaps there is less of a neural drive in this direction. Furthermore, unlike the concomitant patients, there was no over-arching trend of post-operative drift. No correlation between diplopia or degree of fusion could be garnered from this small group of patients.
There are several limitations to our study. Although carefully studied, the population size was small, as inclusion into the study required long-term follow-up with multiple post-operative measurements using Hess screen testing, which requires a level of cooperation and participation not encompassed by many patients. Multiple surgical techniques were used by two different surgeons. Many cases were re-operations referred to a tertiary care setting, and may not represent typical XT. Also, given the nature of the Hess screen test, young children were eliminated from the study as they were unable to perform the test. However, these data do represent a cohort of XT patients with quantitative follow-up, and suggest that the post-operative behavior of pattern XT may differ from that of initially operated or re-operated XT.
Acknowledgments
This work was supported by Grant USPHS NIH EY08313 to Dr. Demer, the Leonard Apt Professor of Ophthalmology.
Footnotes
Presented at the Association for Research in Vision and Ophthalmology Meeting, Fort Lauderdale, FL, 2007
Contributor Information
Stacy L. Pineles, Jules Stein Eye Institute and Department of Ophthalmology, UCLA, Los Angeles, CA
Arthur L. Rosenbaum, Jules Stein Eye Institute and Department of Ophthalmology, UCLA, Los Angeles, CA
Joseph L. Demer, Jules Stein Eye Institute and Department of Ophthalmology, UCLA, Los Angeles, CA.
Joseph L. Demer, Department of Neurology, Neuroscience, Interdepartmental Program, Bioengineering, Interdepartmental Program, UCLA, Los Angeles, CA.
References
- Donaldson M, Forrest MP, Gole GA. The surgical management of consecutive exotropia. J AAPOS. 2004;8:230–236. doi: 10.1016/j.jaapos.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Dunlap E. Present status of the A and V syndromes. Am J Ophthalmol. 1961;52:396–401. doi: 10.1016/0002-9394(61)90740-1. [DOI] [PubMed] [Google Scholar]
- Eino D, Kraft SP. Postoperative drifts after adjustable-suture strabismus surgery. Can J Ophthalmol. 1997;32(3):163–169. [PubMed] [Google Scholar]
- Knapp P, Hardesty HH. Treatment of recurrent exotropia. Am J Ophthalmol. 1960;60:2036–2040. [Google Scholar]
- Langmann A, Lindner S, Koch M, et al. Dosis-Wirkungs-Beziehung bei Revisionsoperation des konsekutiven Strabismus divergens im Erwach-senenalter [Dose-effect relation in revision surgery for consecutive strabismus divergens in adults] Ophthalmologe. 2005;102:869–872. doi: 10.1007/s00347-005-1210-x. [DOI] [PubMed] [Google Scholar]
- Lee S, Lee YC. Relationship between motor alignment and postoperative day 1 and at year 1 after symmetric and asymmetric surgery in intermittent exotropia. Jpn J Ophthalmol. 2001;45:167–171. doi: 10.1016/s0021-5155(00)00351-8. [DOI] [PubMed] [Google Scholar]
- McNeer K. Observations on the surgical overcorrection of childhood intermittent exotropia. Am Orthopt J. 1987;37:135–150. [Google Scholar]
- Miller M, Guyton DL. Loss of fusion and the development of A or V patterns. J Pediatr Ophthalmol Strabismus. 1994;31:220–224. doi: 10.3928/0191-3913-19940701-06. [DOI] [PubMed] [Google Scholar]
- Oh S, Clark RA, Velez F, et al. Incomitant strabismus associated with instability of rectus pulleys. Invest Ophthalmol Vis Sci. 2002;42:2169–2178. [PubMed] [Google Scholar]
- Olitsky S. Early and late postoperative alignment following unilateral lateral rectus recession for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 1998;35:146–148. doi: 10.3928/0191-3913-19980501-05. [DOI] [PubMed] [Google Scholar]
- Raab E, Parks MP. Recession of the lateral recti. Arch Ophthalmol. 1969;82:203–208. doi: 10.1001/archopht.1969.00990020205010. [DOI] [PubMed] [Google Scholar]
- Scott W, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981;99:1814–1818. doi: 10.1001/archopht.1981.03930020688013. [DOI] [PubMed] [Google Scholar]
- Souza-Dias C, Uesugui CF. Postoperative evolution of the planned initial overcorrection in intermittent exotropia. Binocular Vis Eye Muscle Surg Q. 1993;8:141–148. [Google Scholar]
- Weston B, Enzenauer RW, Kraft SP, Gayowsky GR. Stability of the postoperative alignment in adjustable-suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1991;28:206–211. doi: 10.3928/0191-3913-19910701-05. [DOI] [PubMed] [Google Scholar]