Abstract
Background
This study examines leisure time sedentary behavior (LTSB) and usual occupational/domestic activity (UODA) and their relationship with metabolic syndrome and individual cardiovascular disease (CVD) risk factors, independent of physical activity level.
Methods
National Health and Nutrition Examination Survey (NHANES) 2003–2006 data from men (n = 1868) and women (n = 1688) with fasting measures were classified as having metabolic syndrome by the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) definition. LTSB was determined from self-reported television viewing and computer usage. UODA was self-reported daily behavior (sitting, standing, walking, carrying loads).
Results
LTSB ≥4 hours/day was associated with odds of having metabolic syndrome of 1.94 (95% confidence interval [CI], 1.24, 3.03) in men compared to ≤1 hour/day. LTSB ≥4 hour/day was also associated with higher odds of elevated waist circumference (1.88, CI, 1.03, 3.41), low high-density lipoprotein cholesterol (HDL-C) (1.84, CI, 1.35, 2.51), and high blood pressure (1.55, CI, 1.07, 2.24) in men. LTSB 2–3 hours/day was associated with higher odds of elevated glucose (1.32, CI, 1.00, 1.75) in men. In women, odds of metabolic syndrome were 1.54 (CI, 1.00, 2.37) with ≥4 hours/day LTSB, but LTSB was not associated with risk of the individual CVD risk factors. Higher LTSB was associated with metabolic syndrome in inactive men (1.50, CI, 1.07, 2.09), active men (1.74, CI, 1.11, 2.71), inactive women (1.69, CI, 1.24, 2.33), but not active women (1.62, CI, 0.87,3.01). UODA was not strongly associated with metabolic syndrome or CVD risk factors in either men or women.
Conclusions
In men, high LTSB is associated with higher odds of metabolic syndrome and individual CVD risk factors regardless of meeting physical activity recommendations. In women, high LTSB is associated with higher odds of metabolic syndrome only in those not meeting the physical activity recommendations.
Introduction
Sedentary behaviors include activities at the lowest spectrum of energy expenditure such as lying down, sitting, watching TV, using the computer, and other media and screen-based pastimes (i.e., 1.0–1.5 METs).1 TV viewing is the measure of leisure time sedentary behavior (LTSB) most often used in recent research 2 and is perhaps a stronger marker for an overall sedentary lifestyle in women than in men.3 Analysis of accelerometer data revealed that approximately 55% of waking hours is spent in sedentary behavior in adults and children in the United States.4 Furthermore, as people age, a larger percent of the day is spent in sedentary pursuits.
There is a growing body of literature highlighting the health risks associated with acute exposure to a sedentary behavior, such as bouts of sitting.5 Furthermore, a habitual sedentary lifestyle has been associated with a plethora of risk factors; they include a higher risk for obesity6 and type 2 diabetes,7 in addition to an elevated cardiovascular disease (CVD) risk factor profile.8,9 Not only has sedentary behavior been associated with individual CVD risk factors,10 but it has also been associated with the clustering of risk factors and the metabolic syndrome.11−14
Metabolic syndrome is a constellation of several CVD and diabetes risk factors, including obesity, high triglycerides, low high-density lipoprotein cholesterol (HDL-C), high blood pressure, and high fasting glucose classified by the American Heart Association/ National Heart, Lung, and Blood Institute (AHA/NHLBI) criteria.15 According to the National Health and Nutrition Examination Survey (NHANES) 1999–2004, approximately 36% of the U.S. adult population have metabolic syndrome as classified by the AHA/NHLBI criteria.16 Recent studies have reported that physical activity level17−20 and physical fitness21,22 are associated with lower prevalence and incidence of metabolic syndrome and individual CVD risk factors (e.g., high blood pressure, insulin resistance, abdominal adiposity, and dislipoproteinemia). Sedentary time and lack of exercise have also been related to metabolic syndrome and individual CVD risk factors in populations across the globe.11−14 Furthermore, it appears that the influence of LTSB on a number of individual CVD risk factors is evident even in those individuals who accumulate recommended amounts of moderate-to-vigorous physical activity.10 Higher levels of occupational activity have also been associated with lower metabolic and CVD risk.23,24
Four or more hours of LTSB (in this case, computer and TV viewing time) have been associated with a higher risk of metabolic syndrome compared to those reporting less than 1 hour per day (odds ratio [OR] 2.10; 95% confidence interval [CI], 1.27, 3.47) in a nationally representative sample of Americans from 1999–2000.14 Increments less than 4 or more hours (i.e., 1, 2, 3 h/day) were not significantly different from the referent group, emphasizing a potential threshold effect. The purpose of this study is to examine LTSB and usual occupational/domestic physical activity (UODA) independent of meeting current physical activity recommendations and the relationship with metabolic syndrome and individual CVD risk factors in U.S. men and women.
Materials and Methods
Analyses were conducted using data from the NHANES25 cycles 2003–2004 and 2005–2006 combined to increase the sample size. NHANES uses a complex, multistage, probability sampling design to select participants who are representative of the civilian, noninstitutionalized U.S. population. Race or ethnicity was derived from questions about race and Hispanic origin [European American (EA), Mexican American (MA), African American (AA)]. For these analyses, “other Hispanic” and other were combined into the “other” category. For LTSB, participants were asked “Over the past 30 days, on average how many hours per day did you sit and watch TV or videos?” and “Over the past 30 days, on average about how many hours per day did you use a computer or play computer games [outside of work]?” Response categories included “none,” “<1 hour,” “1 hour,” “2 hours,” “3 hours,” “4 hours,” and “5 or more hours.” The questions regarding TV and computer did not specify that the behavior in question be the primary activity. These variables were combined to create a total “screen time” outcome variable, which serves as our primary measure of LTSB, which has been done in similar studies.11,14 Once total LTSB was created, it was collapsed into 2 (≤2 and ≥3 h/day) and 3 (≤1, 2–3, and ≥4 h/day) categories for analyses to maintain sufficient sample sizes. For UODA, participants were asked “Which of the 4 sentences best describe your usual daily activities?” Response categories included “sit during the day and do not walk about very much,” “stand or walk about quite a lot during the day but do not have to lift or carry things very often,” “lift or carry light loads or have to climb stairs or hills often,” and “heavy work or carries heavy loads.” For the analyses, stands or walks, lifts or carries, and heavy work were combined into 1 category to be compared against the mostly sitting category to examine the risk of a sedentary lifestyle. UODA was selected as a measure of domestic and occupational activity because the sample of participants includes students, homemakers, retirees, as well as employed individuals. Self-reported participation in moderate and vigorous physical activity were categorized as meeting or not meeting current physical activity recommendations defined as at least 150 minutes per week of leisure-time moderate-to-vigorous physical activity.
Weight, height, waist circumference, and blood pressure were measured in the mobile exam center.25 Blood was typically drawn from an antecubital vein of the left arm following an overnight fast. Diagnosis of metabolic syndrome was made using the AHA/NHLBI guidelines.15 The guidelines state that for a person to be diagnosed with metabolic syndrome they must have 3 or more of the following five risk factors: (1) high waist circumference (≥102 cm for men and ≥88 cm for women); (2) high triglycerides (≥150 mg/dL or on drug treatment); (3) low HDL-C (<40 mg/dL for men and <50 mg/dL in women or on drug treatment); (4) high blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic or on drug treatment); (5) high fasting glucose (≥100 mg/dL or on drug treatment).15 The collection procedures for NHANES were reviewed and approved by the Institutional Review Board of the National Center for Health Statistics (NCHS). Documentation on informed consent can be located on the NHANES website.25
Data analysis followed the guidelines of the NCHS for analysis of NHANES data due to complex sampling design and methods.26 Participants younger than 20 years of age, those that were pregnant or breast feeding, those physically unable to be active, or those that responded “don’t know” or refused, or those having a missing response for the questions on LTSB were excluded from the present analysis. Two participants were removed due to extreme values (body mass index [BMI] ≥100 kg/m2 and total cholesterol ≥600 mg/dL). For the primary outcome analyses, all continuous variables were standardized to a mean of zero and unit standard deviation to aid in the interpretation of the findings.
Descriptive statistics for the prevalence of spending ≥2 hours per day in LTSB were calculated using sampling weights so that estimates were representative of the adult U.S. population. Primary outcome analyses were performed with sex-specific, sequential binary logistic regression models. The primary outcomes included the AHA/NHLBI metabolic syndrome and each of its five component risk factors. Covariates in the fully adjusted model included age (years), BMI (kg/m2), smoking status (current or past vs. never), education (<high school (HS) or HS/or equivalent vs. >HS), ethnicity (AA or MA or other vs. EA), and dietary fat intake (percent of total calories consumed from dietary fat). The first model included LTSB or UODA and age (years) only. Model 2 included LTSB or UODA, age, and the other covariates. Model 3 included variables from model 2 and sufficient physical activity. SAS 9.1 software was used for these analyses.
Results
There were 1868 men (n = 645, 34.1% with metabolic syndrome) and 1688 women (n = 640, 32.7% with metabolic syndrome) included in the final analyses. The prevalence of U.S. adults spending ≥4 hours per day in LTSB was 32.5% for men and 31.1% for women. For men, 39.6% versus 28.7% and for women 42.0% versus 25.8% spend more than 4 hours daily in LTSB for those with and without metabolic syndrome, respectively. Descriptive characteristics by sex and by presence (or not) of metabolic syndrome are presented in Table 1.
Table 1.
Descriptive Characteristics (Mean ± SE) of Sample From National Health and Nutrition Examination Survey 2003–2004 and 2005–2006 for Males and Females With and Without Metabolic Syndrome As Classified by the AHA/NHLBI
| |
Males |
Females |
||||
|---|---|---|---|---|---|---|
| Variables | Total | With MetS | Without MetS | Total | With MetS | Without MetS |
| n | 1868 | 645 (34.1%) | 1223 (65.9%) | 1688 | 640 (32.7%) | 1048 (67.3%) |
| Age (years) | 45.1 ± 0.6 | 50.5 ± 0.6 | 42.3 ± 0.7 | 47.9 ± 0.6 | 54.8 ± 0.7 | 44.6 ± 0.6 |
| Ethnicity | ||||||
| Mexican American (%) | 8.9 ± 1.3 | 6.8 ± 1.4 | 10.0 ± 1.4 | 6.6 ± 1.1 | 7.3 ± 1.7 | 6.2 ± 0.9 |
| European American (%) | 72.4 ± 2.4 | 80.2 ± 2.9 | 68.4 ± 2.3 | 72.0 ± 2.3 | 72.1 ± 3.2 | 72.0 ± 2.2 |
| African American (%) | 10.2 ± 1.3 | 6.3 ± 0.9 | 12.3 ± 1.6 | 12.1 ± 1.4 | 12.5 ± 2.0 | 11.9 ± 1.2 |
| Other (%) | 8.4 ± 1.2 | 6.7 ± 1.7 | 9.3 ± 1.3 | 9.3 ± 1.2 | 8.1 ± 1.4 | 9.9 ± 1.5 |
| Body mass index (kg/m2) | 28.6 ± 0.1 | 32.4 ± 0.3 | 26.5 ± 0.1 | 28.6 ± 0.2 | 32.9 ± 0.4 | 26.6 ± 0.2 |
| Waist circumference (cm) | 101.2 ± 0.4 | 113.2 ± 0.7 | 94.9 ± 0.5 | 94.7 ± 0.5 | 106.2 ± 0.7 | 89.1 ± 0.5 |
| Systolic blood pressure (mmHg) | 123.1 ± 0.6 | 129.4 ± 0.9 | 119.7 ± 0.6 | 120.4 ± 0.6 | 129.9 ± 0.8 | 115.9 ± 0.6 |
| Diastolic blood pressure (mmHg) | 71.2 ± 0.4 | 75.5 ± 0.6 | 69.0 ± 0.5 | 69.1 ± 0.4 | 71.4 ± 0.7 | 68.0 ± 0.5 |
| HDL-C (mg/dL) | 49.2 ± 0.5 | 41.9 ± 0.7 | 52.9 ± 0.5 | 59.9 ± 0.5 | 50.8 ± 0.7 | 64.4 ± 0.6 |
| Triglycerides (mg/dL) | 156.9 ± 3.4 | 227.6 ± 9.6 | 120.0 ± 2.8 | 131.7 ± 3.7 | 199.8 ± 11.8 | 97.9 ± 1.6 |
| Glucose (mg/dL) | 103.9 ± 0.7 | 115.4 ± 1.2 | 97.9 ± 0.7 | 100.1 ± 0.9 | 115.5 ± 1.7 | 92.5 ± 0.5 |
| Education (% >HS) | 55.1 ± 1.7 | 52.0 ± 2.4 | 56.8 ± 2.0 | 57.4 ± 1.9 | 47.5 ± 3.1 | 62.2 ± 1.9 |
| Household income (% ≥$45K) | 48.1 ± 1.8 | 46.0 ± 2.7 | 49.2 ± 2.0 | 42.8 ± 1.9 | 33.5 ± 2.9 | 47.3 ± 1.9 |
| Dietary fat (%) | 33.7 ± 0.3 | 34.7 ± 0.6 | 33.1 ± 0.3 | 34.0 ± 0.3 | 34.2 ± 0.5 | 33.9 ± 0.4 |
| Sufficient physical activity (%) | 41.7 ± 1.4 | 38.6 ± 2.0 | 43.3 ± 1.5 | 35.0 ± 1.4 | 23.3 ± 2.0 | 40.6 ± 1.8 |
| Screen time | ||||||
| ≤1 h/day (%) | 25.3 ± 1.1 | 18.8 ± 2.2 | 28.6 ± 1.6 | 27.8 ± 1.3 | 20.2 ± 1.9 | 31.5 ± 1.7 |
| 2–3 h/day (%) | 42.3 ± 1.7 | 41.6 ± 2.3 | 42.6 ± 1.9 | 41.1 ± 1.2 | 37.7 ± 3.1 | 42.7 ± 1.5 |
| ≥4 h/day (%) | 32.5 ± 1.8 | 39.6 ± 3.3 | 28.7 ± 1.6 | 31.1 ± 1.4 | 42.0 ± 2.9 | 25.8 ± 1.6 |
| Usual daily physical activity | ||||||
| Sitting (%) | 19.8 ± 0.9 | 25.5 ± 1.8 | 16.8 ± 1.2 | 24.9 ± 1.4 | 27.3 ± 2.3 | 23.7 ± 1.4 |
| Standing (%) | 45.0 ± 1.6 | 45.1 ± 2.6 | 45.0 ± 2.1 | 57.3 ± 2.0 | 57.5 ± 2.6 | 57.2 ± 2.1 |
| Light loads and stairs (%) | 21.7 ± 1.3 | 19.7 ± 1.6 | 22.7 ± 1.6 | 15.0 ± 1.5 | 13.0 ± 2.5 | 15.9 ± 1.3 |
| Heavy work or loads (%) | 13.5 ± 1.3 | 9.6 ± 1.8 | 15.5 ± 1.4 | 2.8 ± 0.6 | 2.1 ± 0.8 | 3.2 ± 0.7 |
Abbreviations: SE, standard error; MetS, metabolic syndrome; AHA/NHLBI, American Heart Association/National Heart, Blood, and Lung Institute; HS, high schoool; HDL-C, high-density lipoprotein cholesterol.
The results of the analyses of LTSB and metabolic syndrome outcome are presented in Table 2 and each of the individual CVD risk factors is shown in Table 3. The highest category of LTSB (≥4 h/day) was associated with 1.95 greater odds (95% CI, 1.25, 3.04) of having metabolic syndrome in men compared to ≤1 hour/day (Model 2). The intermediate category (2–3 h/day) of LTSB was not associated with an increase in odds of metabolic syndrome. When sufficient physical activity (yes/no for engaging in >150 minutes or more per week of moderate-to-vigorous physical activity) was added to the regression analyses (Model 3), the relationship between LTSB and metabolic syndrome was unchanged (1.94 increased odds; 95% CI, 1.24, 3.03). Interpretation of the results of Model 3 is that the odds of having metabolic syndrome is approximately 94% higher in those men who spend 4 or more hours in LTSB daily compared to those spending 1 hour or less independent of their physical activity level. For the individual CVD risk factors in the fully adjusted models, LTSB was associated with significantly higher risk for high waist circumference, low HDL-C, high blood pressure, and high glucose (Table 3). UODA was not significantly associated with metabolic syndrome or any of the individual CVD risk factors in the fully adjusted model, although it was a significant predictor for metabolic syndrome and for high waist circumference in men in model 1 (adjusted only for age) (Table 4).
Table 2.
Odds Ratios for Leisure Time Sedentary Behavior as a Predictor of Metabolic Syndrome with All Continuous Variables Standardized to a Mean of Zero and Unit Standard Deviation for Men and Women in a Sample from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006
| |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| Variable | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) |
| Screen time | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.41 (0.99–2.02) | 1.39 (0.93–2.08) | 1.39 (0.93–2.07) | 1.20 (0.82–1.77) | 1.04 (0.67–1.61) | 1.05 (0.68–1.61) |
| ≥4 h/day | 2.09 (1.37–3.20)a | 1.95 (1.25–3.04)a | 1.94 (1.24–3.03)a | 2.15 (1.51–3.05)a | 1.56 (1.00–2.41)a | 1.54 (1.00–2.37)a |
| Age | 1.66 (1.49–1.84)a | 1.90 (1.61–2.243)a | 1.90 (1.61–2.24)a | 1.85 (1.66–2.05)a | 2.18 (1.86–2.56)a | 2.13 (1.81–2.51)a |
| BMI | 3.84 (3.21–4.59)a | 3.84 (3.21–4.59)a | 2.84 (2.41–3.35)a | 2.79 (2.36–3.30)a | ||
| Smoke | ||||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Current | 1.02 (0.75–1.40) | 1.01 (0.74–1.39) | 1.30 (0.96–1.75) | 1.24 (0.92–1.68) | ||
| Past | 1.06 (0.79–1.42) | 1.05 (0.78–1.42) | 1.15 (0.79–1.68) | 1.19 (0.80–1.77) | ||
| Education | ||||||
| >HS | 1.00 | 1.00 | 1.00 | 1.00 | ||
| HS/GED | 1.31 (0.93–1.83) | 1.29 (0.92–1.83) | 1.20 (0.88–1.62) | 1.17 (0.86–1.59) | ||
| <HS | 1.18 (0.79–1.76) | 1.16 (0.77–1.75) | 1.61 (1.02–2.53)a | 1.48 (0.92–2.36) | ||
| Ethnicity | ||||||
| EA | 1.00 | 1.00 | 1.00 | 1.00 | ||
| AA | 0.32 (0.21–0.46)a | 0.31 (0.21–0.46)a | 0.62 (0.46–0.86)a | 0.61 (0.44–0.84)a | ||
| MA | 0.80 (0.57–1.12) | 0.79 (0.56–1.11) | 1.33 (0.74–2.38) | 1.24 (0.68–2.26) | ||
| Other | 0.76 (0.41–1.40) | 0.76 (0.41–1.41) | 1.14 (0.66–1.95) | 1.14 (0.67–1.93) | ||
| Dietary fat | 0.94 (0.81–1.10) | 0.94 (0.81–1.09) | 0.98 (0.86–1.12) | 0.98 (0.86–1.12) | ||
| Sufficient activity (yes vs. no) | 0.92 (0.70–1.20) | 0.61 (0.45–0.83)a | ||||
Predictors included in Model 1: screen time and age (SD = men 24.6 years; women 24.2 years). Predictors included in Model 2: screen time, age, body mass index (SD = men 6.0 kg/m2; women 8.6 kg/m2), smoking (current vs. never and past vs. never), education (<high school degree vs. >high school degree and high school or GED vs. >high school degree), ethnicity (African American vs. European American, Mexican American vs. European American, and other vs. European American), and percent of fat in diet (SD = men 12.3%; women 13.7%). Predictors included in Model 3: all variables from Models 1 and 2 and sufficient physical activity (yes vs. no ≥150 min per week of moderate-to-vigorous physical activity).
aSignificant predictors (P < 0.05).
Abbreviations: OR, odds ratio; CI, confidence interval; BMI, body mass index; HS, high school; GED, General Educational Development; EA, European American; AA, African American; MA, Mexican American; SD, standard deviation.
Table 3.
Odds Ratios for Leisure Time Sedentary Behavior as a Predictor of Individual Risk Factors for Men and Women in a sample from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006
| |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| Variable | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) |
| High waist circumference | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.32 (0.97–1.81) | 1.60 (1.10–2.35)a | 1.56 (1.08–2.27)a | 1.23 (0.91–1.66) | 1.07 (0.66–1.74) | 1.07 (0.67–1.70) |
| ≥4 h/day | 1.73 (1.28–2.35)a | 1.90 (1.05–3.44)a | 1.88 (1.03–3.41)a | 1.93 (1.42–2.61) | 1.41 (0.70–2.84) | 1.39 (0.69–2.80) |
| Low HDL-C | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.52 (1.10–2.12)a | 1.49 (1.06–2.10)a | 1.48 (1.06–2.06)a | 1.14 (0.87–1.49) | 0.95 (0.74–1.22) | 0.96 (0.74–1.24) |
| ≥4 h/day | 2.00 (1.44–2.77)a | 1.90 (1.40–2.59)a | 1.84 (1.35–2.51)a | 1.67 (1.28–2.17)a | 1.10 (0.82–1.47) | 1.08 (0.81–1.44) |
| High triglycerides | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.07 (0.79–1.47) | 1.05 (0.77–1.44) | 1.05 (0.77–1.44) | 1.09 (0.77–1.54) | 0.96 (0.66–1.42) | 0.97 (0.66–1.42) |
| ≥4 h/day | 1.34 (0.95–1.89) | 1.31 (0.96–1.80) | 1.29 (0.94–1.78) | 1.48 (1.05–2.09)a | 1.18 (0.81–1.71) | 1.17 (0.81–1.68) |
| High blood pressure | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.05 (0.82–1.36) | 1.03 (0.77–1.37) | 1.02 (0.77–1.37) | 1.05 (0.72–1.53) | 0.96 (0.62–1.50) | 0.97 (0.62–1.51) |
| ≥4 h/day | 1.73 (1.24–2.43)a | 1.56 (1.08–2.26)a | 1.55 (1.07–2.24)a | 1.61 (1.13–2.29)a | 1.15 (0.73–1.80) | 1.14 (0.73–1.79) |
| High glucose | ||||||
| ≤1 h/day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 h/day | 1.32 (1.02–1.70)a | 1.32 (1.00–1.75)a | 1.32 (1.00–1.75)a | 1.36 (0.99–1.85) | 1.24 (0.85–1.79) | 1.25 (0.87–1.80) |
| ≥4 h/day | 1.33 (0.98–1.79) | 1.22 (0.89–1.68) | 1.22 (0.89–1.69) | 1.70 (1.21–2.39)a | 1.37 (0.92–2.02) | 1.36 (0.92–2.01) |
Predictors included in Model 1: screen time and age (SD = men 24.6 years; women 24.2 years). Predictors included in Model 2: screen time, age, body mass index (SD = men 6.0 kg/m2; women 8.6 kg/m2), smoking (current vs. never and past vs. never), education (<high school degree vs. >high school degree and high school or GED vs. >high school degree), ethnicity (African American vs. European American, Mexican American vs. European American, other vs. European American), and percent of fat in diet (SD = men 12.3%; women 13.7%). Predictors included in Model 3: all variables from Models 1 and 2 and sufficient physical activity (yes vs. no ≥150 min per week of moderate-to-vigorous physical activity).
aSignificant predictors (P < 0.05).
Abbreviations: OR, odds ratio; CI, confidence interval; HDL-C, high-density lipoprotein cholesterol; SD, standard deviation.
Table 4.
Odds Ratios for Usual Daily Physical Activity as a Predictor of Metabolic Syndrome and All Constituent Individual Risk Factors for Men and Women in a Sample from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006
| |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| Variable | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) |
| Metabolic syndrome | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 1.66 (1.23–2.23)a | 1.44 (1.00–2.09)a | 1.43 (0.99–2.06) | 1.17 (0.91–1.51) | 0.88 (0.65–1.20) | 0.82 (0.59–1.13) |
| High waist circumference | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 1.58 (1.20–2.09)a | 1.20 (0.62–2.32) | 1.15 (0.60–2.22) | 1.40 (1.16–1.69)a | 1.09 (0.71–1.67) | 1.03 (0.66–1.59) |
| Low HDL | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 1.31 (0.96–1.79) | 1.21 (0.84–1.74) | 1.14 (0.78–1.66) | 1.24 (0.96–1.60) | 1.08 (0.81–1.45) | 1.01 (0.75–1.37) |
| High triglycerides | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 1.25 (0.92–1.72) | 1.15 (0.84–1.58) | 1.20 (0.81–1.54) | 1.27 (0.99–1.64) | 1.25 (0.94–1.68) | 0.21 (0.91–1.61) |
| High blood pressure | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 1.30 (0.93–1.80) | 1.15 (0.80–1.64) | 1.13 (0.78–1.63) | 1.06 (0.74–1.51) | 0.89 (0.60–1.33) | 0.87 (0.59–1.28) |
| High glucose | ||||||
| Stand, walk, loads | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sitting | 0.89 (0.66–1.22) | 0.75 (0.54–1.03) | 0.75 (0.54–1.03) | 1.19 (0.91–1.56) | 0.95 (0.70–1.28) | 0.90 (0.65–1.24) |
Predictors included in Model 1: usual daily physical activity and age (SD = men 24.6 years; women 24.2 years). Predictors included in Model 2: usual daily physical activity, age, body mass index (SD = men 6.0 kg/m2; women 8.6 kg/m2), smoking (current vs. never and past vs. never), education (<high school degree vs. >high school degree and high school or GED vs. >high school degree), ethnicity (African American vs. European American, Mexican American vs. European American, and other vs. European American), and percent of fat in diet (SD = men 12.3%; women 13.7%). Predictors included in Model 3: all variables from Models 1 and 2 and sufficient physical activity (yes vs. no ≥150 min per week of moderate-to-vigorous physical activity).
aSignificant predictors (P < 0.05).
Abbreviations: OR, odds ratio; CI, confidence interval; HDL, high-density lipoprotein; SD, standard deviation.
In women, odds of having metabolic syndrome were 1.56 higher (95% CI, 1.00, 2.41) in those who spent 4 or more hours in LTSB daily compared to those spending 1 hour or less (Model 2). The intermediate category of LTSB (2–3 h/day) was not associated with higher odds of metabolic syndrome. Once sufficient physical activity level was included in the model (Model 3), the relationship of the highest category of LTSB with increased likelihood of metabolic syndrome remained unchanged (1.54 increased odds; 95% CI, 1.00, 2.37). Thus the odds of having metabolic syndrome were approximately 54% higher in those women who spent 4 or more hours in LTSB daily compared to those spending 1 hour or less. For the individual CVD risk factors in the fully adjusted models, LTSB was not associated with an increased risk for any of the outcome variables (Table 3). However, in the unadjusted models, LTSB was associated with increased odds of low HDL-C, high triglycerides, high blood pressure, and high glucose (Table 3). UODA was not significantly associated with metabolic syndrome or any of the individual CVD risk factors in the fully adjusted model (Model 3), although in model 1 it was a significant predictor of high waist circumference (Table 4).
When the sample was stratified by physical activity level (meeting or not current recommendation) (Fig. 1), the influence of LTSB on likelihood of metabolic syndrome remained significant, especially in the men. In men meeting the physical activity recommendations, the odds of having metabolic syndrome were 1.74 (95% CI, 1.11, 2.71) and in inactive men 1.50 (95% CI, 1.07, 2.09) for men spending ≥3 versus ≤2 h/day in LTSB when adjusted for other covariates. In women meeting the physical activity recommendations, the odds of having metabolic syndrome were not significant at 1.62 (95% CI, 0.87, 3.01) between those spending ≥3 versus ≤2 h/day in LTSB. However, for those women achieving insufficient levels of physical activity (i.e., inactive), the OR for having metabolic syndrome was significant 1.69 (95% CI, 1.24, 2.33) for those spending ≥3 versus ≤2 h/day in LTSB when adjusted for other covariates.
FIG. 1.
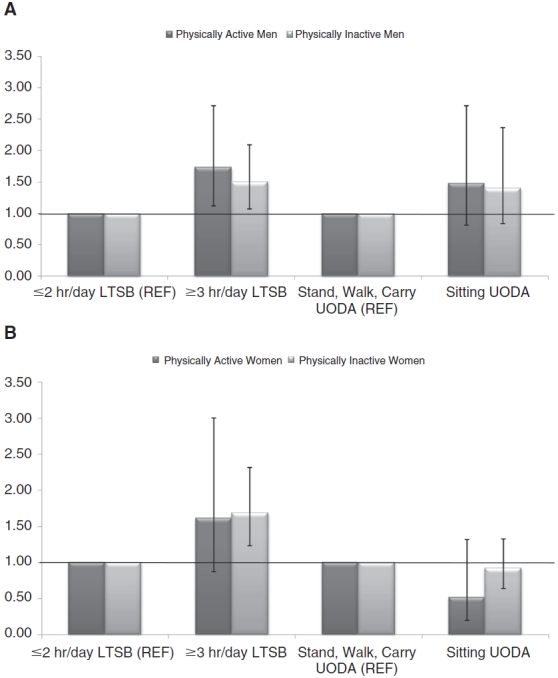
Odds ratios and 95% confidence intervals for leisure time sedentary behavior (LTSB) and usual occupational/domestic activity (UODA) and metabolic syndrome, stratified by meeting or not meeting physical activity recommendations (>150 min/week of moderate-to-vigorous physical activity) for men (A) and women (B) from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006. Referent was ≤2 hours/day versus ≥3 hours/day for LTSB, and referent was stand, walk, carry loads versus sitting for usual occupational/domestic activity categories. Covariates included: age, smoking (current vs. never and past vs. never), education (<high school degree vs. >high school degree and high school or General Educational Development [GED] vs. >high school degree), ethnicity (African American vs. European American, Mexican American, other vs. European American), and percent of fat in diet.
Discussion
Similar to previous findings,16 over one-third of the U.S. population met the criteria for diagnosis of metabolic syndrome according to the AHA/NHLBI definition. It is important to note that caution be used when comparing studies examining LTSB because different definitions and measures are used in different studies. The primary findings of the present study indicate that higher levels of LTSB (≥4 versus ≤1 hour/day) are associated with a higher prevalence of metabolic syndrome and with some of the individual CVD risk factors as shown in previous studies.11−14 The odds of having metabolic syndrome in men and women increased by 94% and 54%, respectively, in those spending more than 4 versus less than 1 hour per day in LTSB. Ford et al.14 also reported this relationship in the overall sample using 1999–2000 NHANES, however when stratified, only women showed the similar relationship (OR 2.76; 95% CI, 1.19, 6.41).14 Furthermore, our analyses of UODA did not appear to influence the odds of exhibiting metabolic syndrome or individual CVD risk factors in men or in women.
Previous reports note that LTSB in women has a stronger association with metabolic syndrome than men,11,13,14 inconsistent with our findings. One study, however, showed a relationship between LTSB and metabolic syndrome in both women and men,12 which is congruent with our findings. In our study, differences between men and women were apparent when stratified by physical activity level (sufficient vs. insufficient physical activity); the increased risk of higher levels of LTSB was independent of physical activity level in men, but not in women. In those women that met the current physical activity recommendation, higher levels of LTSB did not significantly impact metabolic syndrome. In an Australian study, the relationship between LTSB and metabolic syndrome was independent of meeting physical activity recommendations in both men and women.10 In relation to the individual CVD risk factors, our study shows that higher LTSB was associated with 32–88% higher odds of increased risk factors, similar to previous research10; our findings, however, were stronger in men than in women.
The reason for the discrepancies between genders pertaining to LTSB and metabolic syndrome stratified by physical activity level and LTSB and individual CVD risk factors is not clearly understood. We hypothesize that it could be due to subtle differences in daily patterns of behavior. A recent study highlighted the apparent benefits of breaks (i.e., standing up, walking down the hall, etc.), regardless of physical activity level or energy expenditure of breaks, during sedentary time as a way to reduce a number of individual CVD risk factors.27 The latter study, however, did not differentiate between patterns of behavior and breaks between men and women. The small effects of breaks during sedentary time cannot be captured by a gross measure of sedentary lifestyle behavior and are therefore missed in the present study and others. It is plausible that women may multitask and engage in alternate light or moderate activities while they are watching TV, such as attending to household chores. This would artificially inflate LTSB by reporting the period as time spent watching TV, but they were not actually fully sedentary for the entire duration or were perhaps taking breaks from sedentary behavior to engage in light or moderate activity. Another possible explanation for these findings is that men and women recall their LTSB differently; the questions asked pertained to their typical daily behavior over the past 30 days.
There are strengths and limitations in this study that warrant discussion. A clear strength of our study was the quality of the data; NHANES data were collected using rigorous standards allowing for extrapolation to the U.S. national population. Even though the NHANES data are collected and released in large samples of about 10,000 people every 2-year cycle, the adult sample that was available for analysis with all necessary variables was substantially smaller (approximately 1900 men and 1700 women) even when 2 waves were combined. The smaller sample size does not allow for multiple stratifications to examine differences in LTSB and metabolic syndrome in different subpopulations. The primary limitation is that it is cross-sectional rather than longitudinal or prospective in nature, and therefore causality cannot be determined. Another limitation to our study is that only LTSB that included self-reported TV viewing and nonwork computer usage were analyzed. Although TV time is the most often reported measure of LTSB2,5 used in current research, people may engage in a breadth of sedentary activities at work and during leisure time. Furthermore, the questions did not specify that the sedentary behavior in question be the primary activity potentially allowing for the misclassification of sedentary time via TV watching, for example, when the participant could have been simultaneously engaging in other household chores requiring bodily movement. Different sedentary behaviors may impact metabolic syndrome and individual risk factors differently; for example, reading has not been associated with increases in metabolic risk.11 However, we did include UODA patterns that would capture daily occupational activity and personal chores, but these findings were not significantly associated with any metabolic indicators. We could speculate that a more sensitive measure of occupational/domestic activity and sedentary patterns would improve the probability of finding associations if they exist.
Future research in this area is necessary to increase the robustness of the field and lead to greater clinical application and development of specific recommendations to decrease sedentary behavior. Several prospective studies have examined the effects of physical fitness and physical activity on risk of metabolic syndrome,21,22 but more sedentary behavior research is clearly warranted on the role of the time spent in sedentary behavior on the development of metabolic syndrome and individual CVD risk factors. A large prospective study on women reported that LTSB and sitting at work were both associated with increased risk of obesity and type 2 diabetes; each 2-hour/day increment in TV watching was associated with a 14% increase in diabetes risk.7 The Physical Activity Guidelines for Americans recommend that adults should avoid physical inactivity.28 However, before clear guidelines can be applied to support public health recommendations and clinical practice, randomized controlled trials (RCT) will be necessary to fully quantify the strengths of these epidemiologic findings and to define the dose–response profile. Television viewing has been associated with snacking and increased caloric intake in adults,29,30 although more research is necessary. Whereas the percent of dietary fat consumed was not a significant predictor of metabolic syndrome in our study, the influence of dietary intake, especially during LTSB, on cardiovascular disease risk factors is an important area for future investigations.
In summary, self-reported LTSB is associated with metabolic syndrome and some individual CVD risk factors in men and women. These associations are present regardless of meeting physical activity recommendations in men, whereas this relationship is less clear in women. UODA (as described in this study) does not appear to influence metabolic syndrome or individual CVD risk factors in our study. It would be prudent to consider recommending limiting LTSB in addition to being physically active at the recommended level for the primary prevention of metabolic syndrome and individual CVD risk factors. More research is necessary before definitive conclusions about the risk of leisure time and occupational/domestic sedentary behavior on metabolic disease can be determined.
Contributor Information
Susan B. Sisson, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Sarah M. Camhi, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Timothy S. Church, M.D., M.P.H., Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Corby K. Martin, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Catrine Tudor-Locke, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Claude Bouchard, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Conrad P. Earnest, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Steven R. Smith, M.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Robert L. Newton, Jr., M.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Tuomo Rankinen, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana.
Peter T. Katzmarzyk, Ph.D., Pennington Biomedical Research Center, Baton Rouge, Louisiana..
Acknowledgments
S.B.S., S.M.C., T.S.C., C.K.M., C.T.-L., C.B., C.P.E., S.R.S., R.L.N. Jr., T.R., and P.T.K. are all affiliated with Pennington Biomedical Research Center, Baton Rouge, LA. C.B. is partially supported by the George A. Bray Chair in Nutrition. P.T.K. is partially supported by the Louisiana Public Facilities Authority Endowed Chair in Nutrition, and T.S.C. is partially funded by the John S. McIlhenny Endowed Chair in Health Wisdom. C.K.M. is partially supported by National Institutes of Health grant K23 DK068052-01. R.L.N. is partially support by National Institutes of Health grant 5K01HL88723-2. We would also like to thank Emily F. Mire for her assistance in data management and analysis.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Pate RR, O’Neill JR, Lobelo F. The evolving definition of “sedentary.”. Exerc Sport Sci Rev. 2008;36:173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 2.Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev. 2000;28:153–158. [PubMed] [Google Scholar]
- 3.Sugiyama T, Healy GN, Dunstan DW, Salmon J, Owen N. Is television viewing time a marker of a broader pattern of sedentary behavior? Ann Behav Med. 2008;35:245–250. doi: 10.1007/s12160-008-9017-z. [DOI] [PubMed] [Google Scholar]
- 4.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 6.Shields M, Tremblay MS. Sedentary behaviour and obesity. Health Rep. 2008;19:19–30. [PubMed] [Google Scholar]
- 7.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289:1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 8.Kronenberg F, Pereira MA, Schmitz MK, et al. Influence of leisure time physical activity and television watching on atherosclerosis risk factors in the NHLBI Family Heart Study. Atherosclerosis. 2000;153:433–443. doi: 10.1016/s0021-9150(00)00426-3. [DOI] [PubMed] [Google Scholar]
- 9.Jakes RW, Day NE, Khaw KT, et al. Television viewing and low participation in vigorous recreation are independently associated with obesity and markers of cardiovascular disease risk: EPIC-Norfolk population-based study. Eur J Clin Nutr. 2003;57:1089–1096. doi: 10.1038/sj.ejcn.1601648. [DOI] [PubMed] [Google Scholar]
- 10.Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40:639–645. doi: 10.1249/MSS.0b013e3181607421. [DOI] [PubMed] [Google Scholar]
- 11.Bertrais S, Beyeme-Ondoua JP, Czernichow S, Galan P, Hercberg S, Oppert JM. Sedentary behaviors, physical activity, and metabolic syndrome in middle-aged French subjects. Obes Res. 2005;13:936–944. doi: 10.1038/oby.2005.108. [DOI] [PubMed] [Google Scholar]
- 12.Chang PC, Li TC, Wu MT, et al. Association between television viewing and the risk of metabolic syndrome in a community-based population. BMC Public Health. 2008;8:193. doi: 10.1186/1471-2458-8-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunstan DW, Salmon J, Owen N, et al. Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia. 2005;48:2254–2261. doi: 10.1007/s00125-005-1963-4. [DOI] [PubMed] [Google Scholar]
- 14.Ford ES, Kohl HW, 3rd, Mokdad AH, Ajani UA. Sedentary behavior, physical activity, and the metabolic syndrome among U.S. adults. Obes Res. 2005;13:608–614. doi: 10.1038/oby.2005.65. [DOI] [PubMed] [Google Scholar]
- 15.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 16.Churilla JR, Fitzhugh EC, Thompson DL. The metabolic syndrome: How definition impacts the prevalence and risk in U.S. adults: 1999–2004 NHANES. Metab Syndr Relat Disord. 2007;5:331–342. doi: 10.1089/met.2007.0010. [DOI] [PubMed] [Google Scholar]
- 17.Pitsavos C, Panagiotakos D, Weinem M, Stefanadis C. Diet, exercise and the metabolic syndrome. Rev Diabet Stud. 2006;3:118–126. doi: 10.1900/RDS.2006.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Churilla JR, Zoeller J, Robert F. Physical activity and the metabolic sundrome: A review of the evidence. Am J Lifestyle Med 2007. Mar–Apr, 2007:118–125. [Google Scholar]
- 19.Carroll S, Dudfield M. What is the relationship between exercise and metabolic abnormalities? A review of the metabolic syndrome. Sports Med. 2004;34:371–418. doi: 10.2165/00007256-200434060-00004. [DOI] [PubMed] [Google Scholar]
- 20.Katzmarzyk PT, Herman K. The role of physical activity and fitness in the prevention and treatment of metabolic syndrome. Curr Cardiovasc Risk Rep. 2007;1:228–236. [Google Scholar]
- 21.LaMonte MJ, Barlow CE, Jurca R, Kampert JB, Church TS, Blair SN. Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: a prospective study of men and women. Circulation. 2005;112:505–512. doi: 10.1161/CIRCULATIONAHA.104.503805. [DOI] [PubMed] [Google Scholar]
- 22.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 23.Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K. Risk factors for the metabolic syndrome: The Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2001. Diabetes Care. 2004;27:2707–2715. doi: 10.2337/diacare.27.11.2707. [DOI] [PubMed] [Google Scholar]
- 24.Hu G, Jousilahti P, Borodulin K, et al. Occupational, commuting and leisure-time physical activity in relation to coronary heart disease among middle-aged Finnish men and women. Atherosclerosis. 2007;194:490–497. doi: 10.1016/j.atherosclerosis.2006.08.051. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey
- 26.Centers for Disease Control and Prevention NHANES, Analytic Guidelines
- 27.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Department of Health and Human Services Physical Activity Guidelines for Americans 2008.
- 29.Gore SA, Foster JA, DiLillo VG, Kirk K, Smith West D. Television viewing and snacking. Eat Behav. 2003;4:399–405. doi: 10.1016/S1471-0153(03)00053-9. [DOI] [PubMed] [Google Scholar]
- 30.Thomson M, Spence JC, Raine K, Laing L. The association of television viewing with snacking behavior and body weight of young adults. Am J Health Promot. 2008;22:329–335. doi: 10.4278/ajhp.22.5.329. [DOI] [PubMed] [Google Scholar]


