Abstract
Innate immune signals foster adaptive immunity through activation of antigen presenting cells. Recent in vitro evidence suggests that innate signaling may also contribute to immunity by countering the effects of regulatory T cells (T-regs), counter-regulation. We present in vivo evidence using a transgenic skin allograft model that the function of T-regs is lost in the setting of acute skin transplantation but remains intact when grafts were transplanted one month prior to allow surgery-induced inflammation to abate. Our findings identify T-reg counter-regulation as a naturally occurring process that accompanies transplantation and an important barrier to T-reg mediated tolerance. Our finding further highlights the central role of regulatory cell deactivation in the initiation of the immune response.
Keywords: T-reg, inflammation, transplant, tolerance, allograft
Introduction
Naturally occurring regulatory T cells (T-regs) are essential for the maintenance of tolerance to self-antigens, and in their absence, a syndrome of tissue-specific autoimmunity develops (1). Their ability to inhibit effector T cell proliferation in the draining lymph nodes and to promote indefinite allograft survival in multiple experimental systems (1, 2) makes them attractive for application in transplantation tolerance. In order to translate this potential benefit to the clinical arena, it is critical to understand the in vivo behavior of T-regs and the mechanisms by which T-regs themselves are controlled.
In support of theories linking the adaptive and innate immune responses are recent studies demonstrating that signaling through Toll-like receptors (TLR) interferes with T-reg activity in vitro and the induction of transplantation tolerance in vivo (3, 4). These observations identify a novel mechanism by which innate immune signals could effectively activate the adaptive response by deactivating T-regs (counter-regulation). Likewise, the suppressor function of T-regs can be inactivated indirectly if their target effector T cell is rendered resistant to suppression (5). The presence of counter-regulatory pathways may pose a formidable obstacle to T-reg mediated allograft tolerance.
In this study, we describe counter-regulation in vivo by contrasting the capacity of T-regs to prolong survival of skin allografts in two distinct settings— one in which there is a recent, unhealed transplant (acute) and a second in which the graft has completely healed (established). In the acute setting, T-reg activity in vivo is diminished, and this impairment of T-reg function is dependent on inflammatory activation of innate immune cells. Based on these findings, we propose that the inflammation accompanying transplantation activates innate immune processes which upregulate molecules that impair T-reg activity and prevent T-reg-mediated tolerance.
Materials and methods
Animals
TS1 transgenic mice possesses a high frequency of CD4+ T cells specific for the immunodominant (site 1) epitope (amino acid sequence, SFERFEIFPK) of the influenza hemagglutinin (HA) protein in the context of MHC Class II I-Ed (6). HA104 mice provide a source of HA-expressing grafts as they carry the HA transgene controlled by the SV40 early region promoter/enhancer which results in ubiquitous transgene expression(7). HACII animals express HA under control of the MHC class II promoter and have expression restricted to MHCII-expressing cells. HA28 mice also have HA expression driven by the SV40 promoter and hence have ubiquitous tissue expression. (TS1 x HA28)F1 mice were created and described by Jordan et al(8); these mice develop a roughly 1:1 mixture of regulatory foxp3+ and non-regulatory foxp3- HA-reactive CD4+ T cells. TS1, HACII, HA28, and HA104 transgenic lines are maintained as hemizygotes back-crossed with BALB/c mice (Taconic, Germantown, NY). All animals are maintained in a pathogen-free environment under IACUC approved protocols. Table 1 is provided as a reference for the various strains used in this manuscript.
Table 1. Transgenic strains used in transplantation studies.
The characteristics of the transgenic strains used in this study are outlined.
| Mouse Designation | Transgene Product | Expression Details |
|---|---|---|
| TS1 | HA-reactive TCR | |
| HA104 | Full-Length HA | SV40-driven ubiquitous expression |
| HA28 | Truncated HA (aa 1-237) | SV40 driven ubiquitous expression |
| HACII | HA | Expression on APCs driven by class II promoter |
| (TS1xHA28)F1 | HA and HA-reactive TCR | Normal numbers of lymphocytes. HA- reactive CD4 T cells are produced as a 1:1 ratio of foxp3+ regulatory T cells and foxp3− T cells |
CFSE Labeling
Lymph nodes were harvested, and cells were labeled and prepared as previously described (9). Briefly, lymph nodes were harvested and single-cell suspensions were prepared by passage of tissue through a cell strainer (70um; Falcon, NJ). Cells were resuspended at a density of 107 cells/mL in MEM. An equal volume of 5mM CFSE (Invitrogen) in MEM was added and cells were cultured at 37C for 5min. The reaction was quenched through the addition of an equal volume of FCS. Labeled cells were washed two times with cold MEM containing 10% FCS.
Flow Cytometric Analysis and FACS Purification
Cells were either harvested directly from in vitro culture plates or were obtained from in vivo experiments by sacrificing animals and harvesting lymph nodes followed by preparation of single cell suspensions. Cells were washed in biotin-free RPMI (Irvine Scientific, Santa Ana, CA), and 1×106 cells were stained per sample. The following antibodies were used for analysis: anti-CD4 PE and APC (antibody clone L3T4), anti-CD25 FITC and PE (antibody clone PC61), anti-CD45RB PE (antibody clone 16A) (BD Biosciences, San Diego, CA), and anti vβ8 FITC (CalTag, Burlingame, CA). In addition, 6.5 biotin (6.5 antibody recognizes TS1 TCR) followed by Strepavidin-Red670 (Gibco BRL) secondary were used to detect the transgenic TCR (6). Flow cytometric analysis was performed on a Becton Dickinson Immunocytometry System (San Jose, CA) FACSCalibur cytometer and on a BD LSR II cytometer. FACSCalibur Data acquisition and analysis were accomplished with Becton Dickinson CellQuest™ software, while LSRII utilized Diva and FlowJo Software (Tree Star, Stanford, CA). For sorting experiments, cells were separated on a BD FACSVantage SE (Becton Dickinson, San Jose, CA) high-speed cell sorter, or they were sorted using Miltenyi MACS Beads (Germany). Purity of the sorted populations ranged from 95–99%.
Skin Grafting
Skin grafts were transplanted to mice according to the technique of Billingham and Medawar (10). Grafts were scored as rejected when more than 75% of the grafted tissue area had been lost.
Activation of antigen presenting cells
Spleen cells were prepared by standard methods. For stimulation, 1×106 splenocytes were cultured in 1 ml of media containing 10% HI-FCS and 10 μg/mL LPS (Sigma).
Statistical Analysis
Survival data was compared with the Kaplan-Meier method and analyzed by the log-rank test. For normally distributed data, student’s t-test was applied. P-values less than 0.05 were considered significant.
Results
HA-specific CD4+CD25+ T cells prevent rejection of established HA+ skin allografts
We have previously described a transgenic system for the study of the interaction of antigen-specific naive effectors and regulatory T cells in a transplantation setting (2, 9, 11, 12). In this model hemagglutinin (HA)-expressing tissues for transplantation are derived from HA104 mice in which ubiquitous HA expression is controlled by the SV40 promoter (Table 1). HA-reactive transgenic effector T cells are provided by TS1 animals which express an HA-reactive T cell receptor (TCR) restricted to I-Ed on the BALB/c background. This model is unique due to the prior characterization of an intercross between the TS1 strain and a strain denoted HA28 in which HA is also expressed ubiquitously (2, 8, 13). In the (TS1 × HA28)F1 intercross, normal numbers of lymphocytes are produced and about 50% of the TCR-transgenic CD4 lymphocytes are thymically-derived CD4+CD25+Foxp3+ regulatory cells (14). The regulatory cells derived from the (TS1 × HA28)F1 mouse demonstrate all the features of normally generated T-regs (9) and inhibit the reactivity of the remaining non-regulatory TCR-transgenic T cells.
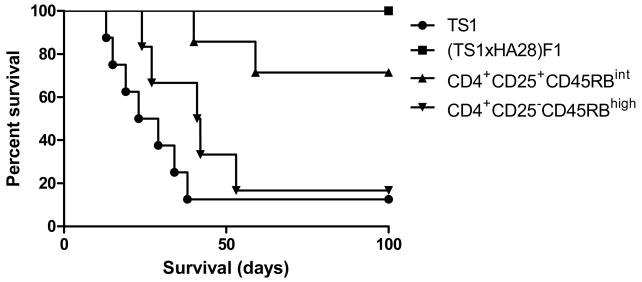
Consistent and prompt rejection of HA-bearing grafts can be induced in BALB/c hosts by adoptive transfer of a small number (5×105) of unfractionated TS1 lymphocytes (11). In this non-immunodeficient adoptive transfer model, rejection is accompanied by vigorous proliferation of HA-reactive T cells in the draining LN basin of the allograft (11, 12, 15). This adoptive transfer model permits assessment of T-reg-mediated graft tolerance without the confounding influences of immunodeficiency-induced homeostatic proliferation. In contrast to rejection resulting from transfer of TS1 LN cells, adoptive transfer of 5×105 (TS1 × HA28)F1 LN cells did not reject established HA104 allografts (Figure 1 and (15)); equalizing the total number of CD25− cells by transfer of 106 (TS1 × HA28) F1 cells failed to result in rejection (data not shown). In the absence of CD25+ regulatory cells, purified CD4+CD25− cells from (TS1 x HA28)F1 mice reject established HA+ grafts (Figure 1); this suggests that the graft protection in this model is due to the regulatory activity of the Foxp3+ fraction. In contrast, sorted CD4+CD25+ T cells from (TS1 × HA28)F1 mice rejected established grafts only in two of seven instances. Thus, the F1 population serves as a source of a mixed population of Tregs and regulated effector cells, each having specificity for the S1 epitope of HA. In the present work, we utilized this model to assess the ability of these regulatory T cells to protect acutely transplanted skin grafts from rejection. We hypothesized that acute inflammation could present a barrier to Treg-mediated tolerance as acute inflammation may locally attenuate regulatory T cell function.
Figure 1. HA-specific CD4+CD25+ T cells prolong the survival of established HA104 skin grafts.
TS1 cells (n=8), (TS1 × HA28)F1 cells (n=13), CD4+CD25+CD45RBint cells sorted from (TS1 × HA28)F1 mice (n=7), or CD4+CD25−CD45RBhigh cells sorted from (TS1 × HA28)F1 mice (n=6) were transferred to BALB/c mice bearing established HA104 skin transplants. MST among rejectors of CD4+CD25+CD45RBint cells versus CD4+CD25−CD45RBhigh cells, 49.5 versus 37.4 days, respectively, p=.036. Established grafts are placed at least 30 days prior to adoptive transfer of cells.
Injury and inflammation from transplant procedure counter-regulate T-reg suppressor function
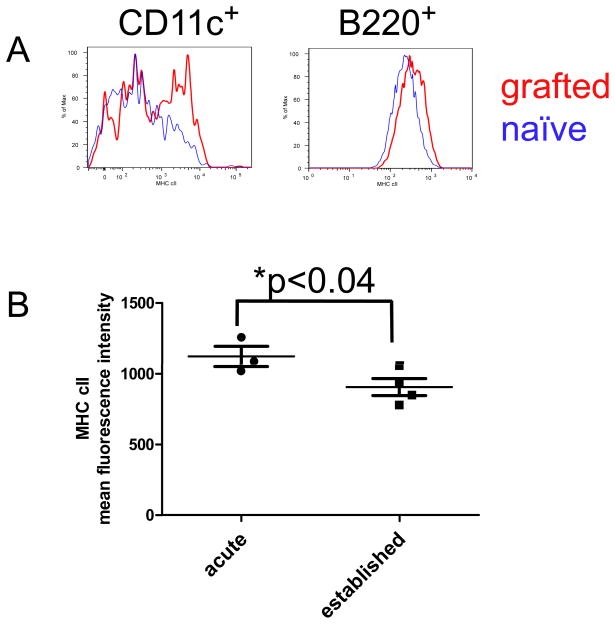
To test the hypothesis that injury and inflammation from the transplant procedure activate the immune system, we performed skin isograft transplants, and levels of MHC class II were assessed following the transplant procedure. Injury and inflammation have previously been demonstrated to upregulate MHC class II as well as recruit class II+ cells to the transplant site (16, 17). Antigen presenting cell types from the draining lymph nodes of BALB/c mice receiving BALB/c skin grafts were examined at multiple time points. Elevated MHC class II levels are detectable at 4 days after transplantation (data not shown) and are highest approximately six to eight days after the transplant procedure (Figure 2A). As this was an isograft one cannot distinguish between infiltration by class II+ cells versus upregulation of MHC class II. These data demonstrate that the inflammation alone resulting from the transplant procedure is sufficient to activate the immune system.
Figure 2. Injury and inflammation from transplant procedure upregulates MHC class II expression in recipient.
BALB/c recipients received BALB/c isograft, and draining lymph node cells (DLN) or spleen cells were analyzed for upregulation of MHC class II. A, Left, at day 8 post-transplant dendritic cells demonstrate increase in MHC class II expression (mean fluorescence intensity (MFI) of MHC class II of grafted mice increases 37%, p=0.014, n=16). Right, at day 3 post-transplant, B cells also demonstrate increase in MHC class II expression (MFI of grafted mice increases 20%, p=.043, n=5). Figures are representative of four separate experiments. B, at day 4 post-transplant, draining and non-draining lymph nodes were isolated from acute grafted and established grafted mice. MHC class II levels of CD11c+ DCs of established grafted mice in both draining and non-draining lymph nodes had returned to normal, while levels of both DLN and NDLN of acute grafted mice were elevated (MFI=906 for established n=4 versus 1122 for acute n=3).
To determine whether the elevation in MHC class II levels was localized to the draining lymph nodes (DLN), we compared levels in CD11c+ dendritic cells (DC) from acute draining lymph nodes versus acute contralateral non-draining lymph nodes (NDLN) versus lymph nodes of established grafted mice. The expression of MHC class II of DLN and NDLN of established grafted mice was at baseline levels. In contrast, both the DLN and NDLN MHC class II levels of acute grafted mice were elevated when compared to established grafted mice (Figure 2B).
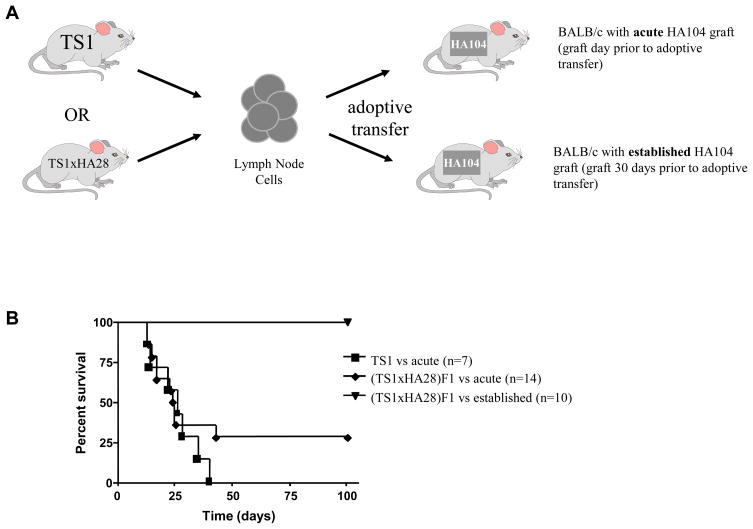
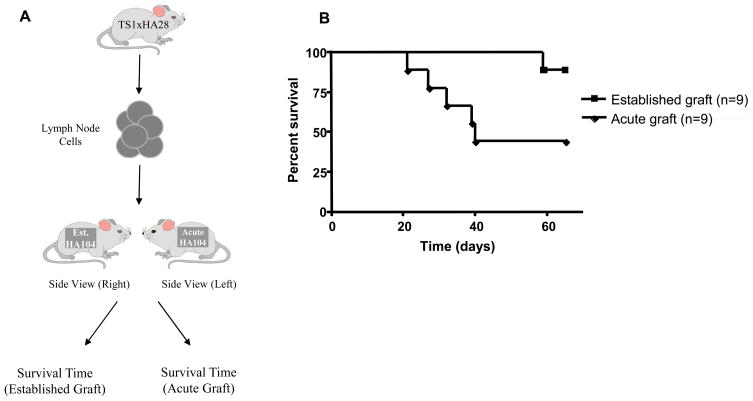
To assess the impact of an inflammatory environment on T-reg function, we first compared rejection of HA+ grafts transplanted to BALB/c hosts one day prior to adoptive cell transfer (acute grafts) versus grafting thirty days prior (established). Transfer of 5×105 TS1 LNC as a source of naive HA-specific effector cells to BALB/c mice bearing HA+ skin induced prompt rejection of both acute and established skin grafts, suggesting that the immunogenicity of the acute and chronic grafts were similar (MST (mean survival time) =20 days for established grafts vs MST=23 days for acute; Figure 3). Established grafts are not rejected by (TS1 × HA28)F1 LNC (Figure 1), however, when (TS1 × HA28)F1 LNC were transferred 24 hours after skin graft, unexpectedly, grafts were rejected with kinetics similar to TS1 LNC (MST=44 days for F1, p>0.05 vs TS1). These results suggest that CD4+CD25+ T cells from (TS1 × HA28)F1 are less able to suppress effector cell activity in the acute graft setting.
Figure 3. Tregs from (TS1 x HA28)F1 lymphocytes are less able to suppress graft rejection in the acute graft setting.
a) The experimental design is illustrated graphically. Skin grafts from HA104 donors were transplanted to wild-type BALB/c recipients either 1day (acute) or 30 days (established) prior to adoptive transfer of TS1 or (TS1 × HA28)F1 LNC. b) Transgene-negative BALB/c mice were transplanted with skin grafts harvested from HA104 mice. 5×105 unfractionated TS1 or (TS1 × HA28)F1 lymph node cells were transferred by tail vein injection either one (acute) or thirty (established) days after transplantation. No difference was detected in the rejection response between F1 and TS1 lymphocytes (p=0.33, log-rank). Data shown were compiled from at least two separate experiments in each instance. The response of (TS1 × HA28)F1 LNC to established HA104 skin grafts (grafted >30d prior) is shown for comparison.
Acute inflammatory state results in decreased levels of Foxp3 expression in T-regs
To determine whether differential migration of T-regs could explain the survival difference between acute and established grafts (18), we compared the ratio of injected 6.5+CD4+CD25− to injected 6.5+CD4+CD25+ in lymph nodes of ungrafted mice, draining lymph nodes of acute grafted mice, and draining lymph nodes of established mice. Purified CD4+CD25− and purified CD4+CD25+ T cells were combined at a 1:1 ratio and injected into ungrafted, acute HA104 grafted, and established HA104 grafted mice. If a migration difference is the mechanism by which the T-regs are unable to suppress in the acute setting, then we would expect to see a lower ratio of T-regs:CD4+CD25− T cells in the DLN of acute grafted mice compared to ungrafted or established grafted mice. At one day and three days post-adoptive transfer, we recovered roughly 1:1 ratio of cells from all three groups (data not shown), suggesting that differential migration does not explain the inability of T-regs to suppress in the acute graft setting.
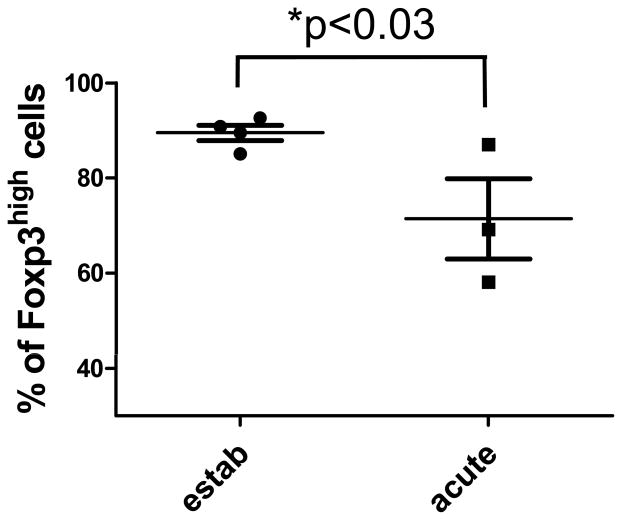
We next examined whether in the acute inflammatory state regulatory T cells had decreased Foxp3 levels, a marker previously demonstrated to reflect functional status (19). Acute grafted and established grafted BALB/c mice received CFSE-labeled, sorted (TS1 × HA28) regulatory T cells. Within seven days after adoptive transfer, draining lymph nodes were removed, and Foxp3 levels were examined in labeled regulatory T cells. In contrast to established grafted mice receiving adoptive transfer, the percentage of T-regs that maintain high levels is significantly decreased in acute grafted mice (Figure 4). These data together with the inability of T-regs to suppress graft rejection in an acute setting suggest that the effects of T-regs are inactivated by inflammation and injury.
Figure 4. Acute inflammatory state decreases percentage of Foxp3high cells.
Acute grafted and established grafted BALB/c mice received CFSE-labeled T-regs. Two to seven days post-adoptive transfer DLN were removed and CFSE-labeled T-regs were examined for levels of Foxp3 expression. Live, CFSE-labeled, divided CD4+ T-regs were gated.
Local factors inhibit T-reg function in the acute graft setting
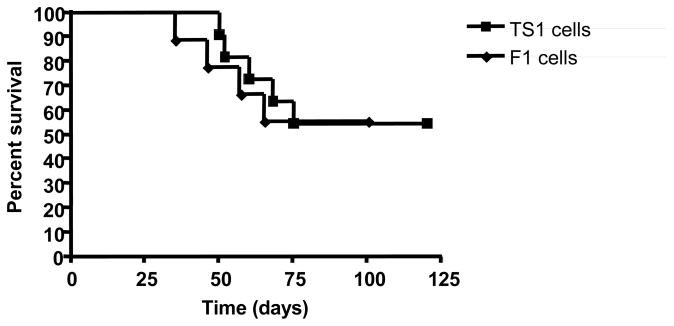
We previously demonstrated that prolonged graft survival in this system correlated with decreased effector T cell proliferation in the draining lymph node (12, 15). We have also previously demonstrated that proliferation of adoptively transferred cells is very robust in the DLN while minimal in the contralateral non-draining lymph nodes (11). We questioned whether inhibition of T-reg function in the acute graft setting also localized to the DLN or was a systemic phenomenon. To differentiate these possibilities, BALB/c mice bearing established HA+ skin grafts were subsequently given a second HA+ graft (acute) on the contralateral thorax and 5×105 (TS1 × HA28)F1 LNC. We reasoned that if T-reg function remains intact both locally and systemically, both transplants should remain viable. If the acute graft setting breaks suppression only locally, the acute graft should be rejected while the established graft remains intact. If the break in suppression is systemic, both grafts should be rejected by the transfer inoculum.
As hypothesized, the majority of acute HA104 skin grafts were rejected after cell transfer, while all but one of the established skin grafts remained intact indefinitely (p<0.05, Figure 5). This finding suggests that counter-regulation of T-reg function occurred only on the side of the acute graft while T-reg activity remained intact on the contralateral side bearing the established graft. We have previously shown that TS1 LNC reject established grafts more rapidly than acute grafts (2), indicating that established grafts are not generally less immunogenic than acute grafts.
Figure 5. Factors local to the graft inhibit T-reg function in the acute graft setting.
a) The experimental approach is represented graphically. BALB/c mice with established HA104 grafts received a second HA104 graft (acute) on the opposite thorax the day prior to transfer of 5×105 (TS1xHA28)F1 LNC. b) The majority of acute HA104 skin grafts were rejected while nearly all established skin grafts remained intact indefinitely. Survival times for the established (n=9) and acute (n=9) transplants were significantly different (p<0.05, log-rank).
To evaluate the possibility that some alteration of established HA+ grafts renders them invulnerable to rejection by F1 LNC specifically, we excised chronic grafts and re-transplanted them to naive BALB/c that then received F1 or TS1 LNC. Chronic grafts re-transplanted to naive BALB/c hosts were accepted. Although only half of the BALB/c hosts given F1 LNC rejected the re-transplanted grafts, the frequency and kinetics of rejection were similar to that in hosts receiving unfractionated TS1 LNC (Figure 6). Dendritic cells from the chronic graft have migrated from the graft to the DLN of the first recipient, and this could explain in part the lower antigenicity when re-grafted. Collectively, these data suggest that inhibition of T-reg function in the acute graft setting is a local rather than systemic phenomenon and that the response within the lymph node is controlled by the inflammatory state of the transplant.
Figure 6. Established HA104 grafts reacquire an acute graft phenotype on re-transplantation.
Established (>30 days) HA104 skin grafts were excised from BALB/c hosts and re-transplanted to naive BALB/c mice. These mice then received 5×105 TS1 LNC (n=11) or (TS1×HA28)F1 LNC (n=8) 1 day following re-transplantation. There is no significant difference between the two groups (p=0.99, log-rank).
Introduction of activated antigen presenting cells into established grafts inhibits T-reg-mediated prolongation
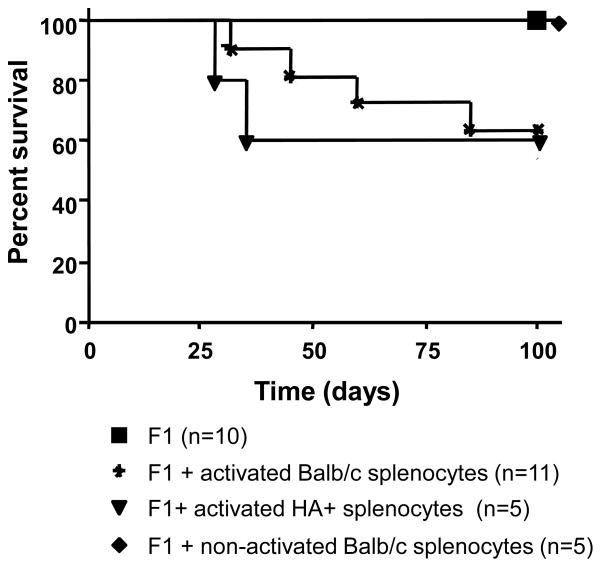
Since T-reg-mediated protection in established grafts (15) and loss of protection in acute grafts were local events (Figure 5), and prior studies suggested that inhibition of T-reg function can occur at the level of antigen presenting cells (APC) (4), we hypothesized that the activation of local APCs immediately following surgery and their migration to the DLN might account for the local loss of T-reg function. Specifically, activated APCs migrating from acute grafts to the DLN could block T-reg activity and allow effector proliferation to promote graft rejection. To test this postulate, we introduced APCs activated by stimulation with LPS into the established graft setting by intradermally injecting 5×106 LPS-activated BALB/c or HA-MHC class II (HACII) splenocytes into the graft at the time of F1 LNC transfer. HACII mice express HA under the control of the class II promoter and are maintained on the BALB/c background. LPS-activation of APCs was confirmed by documenting upregulation of MHC class II, B7, and GITRL by flow cytometry (data not shown).
Introduction of LPS-activated HA class II splenocytes resulted in rejection of established HA+ skin by F1 LNC in a significant fraction (approximately 40%) of host mice (Figure 7). Non-activated BALB/c splenocytes failed to induce rejection, indicating that rejection does not result simply from increased APC numbers. Activated BALB/c splenocytes also promoted rejection, likely by presenting graft-derived antigens in the DLN and efficiently activating effector T cells. These data suggest that activated APCs contribute to the inhibition of T-reg activity seen in the acute graft setting.
Figure 7. Intradermal injection of LPS-activated splenocytes promotes rejection of established HA104 skin grafts by (TS1xHA28)F1 LNC.
5×105 unfractionated (TS1×HA28)F1 lymph node cells were transferred by tail vein injection into BALB/c mice bearing established HA104 skin grafts. Mice receiving no intradermal APCs (square, n=10) or 5×106 non-activated BALB/c (diamond) did not reject. Intradermal injection of LPS-activated BALB/c (asterisk, n=11, p=0.03 vs. unactivated) or LPS-activated HA+ splenocytes (triangle, n=5, p=0.03 vs. unactivated) provoked graft rejection. Survival times for each group are shown.
T-reg activity in the acute graft setting depends on the T-reg:effector cell ratio
In both in vivo and in vitro models of T-reg activity, regulation is dependent on the ratio of T-regs to effector T cells. To assess whether the loss of suppressor activity induced by acute inflammation was relative or absolute, we examined the efficiency of T-regs at a range of T-reg:TS1 LNC ratios (Table 2). CD4+ CD25+ T-regs were cell sorted and combined with unsorted TS1 T-eff at various ratios and injected into mice bearing either acute or established grafts. As demonstrated in figure 1, in the established non-inflammatory setting, T-regs are able to suppress graft rejection. While a T-reg:T-effector ratio of 1.25:1 is sufficient to prevent rejection of an established graft (similar to the 1:1 ratio seen in unfractionated F1 cells), a 5:1 T-reg:T-effector ratio is required to prevent loss of an acute graft. These data demonstrate that the break in suppression in the acute graft setting can be overwhelmed by supra-physiologic numbers of regulatory T cells and indicate why the counter-regulating effect of acute grafting may not have been observed in earlier models of T-reg transfer where very high ratios of T-reg:T-effectors have been used.
Table 2. T-reg function in the acute graft setting is dependent on the T-reg:effector cell ratio.
5×105 unfractionated, TS1 lymph node cells were combined with 5×105 (5:1), 2.5×105 (2.5:1), or 1.25×105 (1.25:1) CD4+CD25+CD45RBint T cells sorted from (TS1 × HA28) F1 mice. It is important to note that only 20% of unfractionated TS1 LNC are CD4+ T cells specific for the HA antigen (6.5+), so a T-reg:TS1 LNC ratio of 1:1 is effectively a T-reg:T-effector ratio of 5:1. The mixed population was then transferred by tail vein injection into BALB/c mice bearing acute or established HA104 skin grafts. Rejection kinetics for each group are shown. There was a tendency toward significance at the 1:2 ratio (p=0.07, long-rank) and a significant difference was found in the 1:1 grouping (p=0.01).
| T-reg:TS1 ratio | Acute graft survival time (days) | Established graft survival time (days) | P-value (acute vs established) |
|---|---|---|---|
| 5:1 | >150 × 7 | >100 ×8 | NS |
| 2.5:1 | 20,28, >150 × 6 | >150 × 12 | 0.07 |
| 1.25:1 | 22,23,27,27,30,34, >150 | >100 ×4 | 0.01 |
DISCUSSION
T-regs offer an attractive avenue for the development of transplantation tolerance by either pharmacological induction in transplant recipients or by direct recovery, expansion in vitro, and return to the recipient. Factors governing T-reg activity in vivo are poorly described but will be critical determinants in the success or failure of these strategies. In this study, we report that the allogeneic response to recently transplanted skin is less amenable to suppression by T-regs than is the response to a graft for which procedure-related inflammation has abated. These findings are consistent with studies suggesting that innate immune signals may interfere with induction of transplant tolerance by costimulatory blockade (3). In concert with our findings, these studies implicate counter-regulatory pathways as critical impediments to T-reg-based transplantation tolerance. Our data also provide additional mechanistic insight by implicating the antigen presenting cell in the process of counter-regulation.
Critical to framing the findings of our investigations are other proposals for the interaction of innate and adaptive immunity. Janeway et al previously suggested that the major decision to respond or not to respond to a particular ligand is decided by innate immune receptors (20). In our model, innate immune signals not only activate T-effectors but also facilitate deactivation of T-reg suppressor activity to allow development of an adaptive immune response. Activation of innate immune receptors therefore plays a central role in development of the immune response in both proposals. Related is Matzinger’s “Danger” model which suggests that the immune system responds to substances that cause damage rather than simply to those that are foreign (21). Our data would suggest that a key role for “danger” signals is the deactivation of T-reg suppressor function. However, our finding that well-healed grafts can be rejected by transferred antigen-specific cells in the absence of “danger” signals affirms a need to refine this model.
Our findings are most readily unified with these earlier models by ascribing to T-regs a principle role in self/non-self discrimination. Since T-regs are required to prevent rejection of established grafts, activation of naive cells is a default pathway and the point of control resides in regulatory cells rather than solely in activation of the naive cell--the latter being the principle decision point of immune activation in more traditional models. In this regard, the immune system appears to possess control mechanisms that are governed by disinhibition. This organization of the immune system is buttressed by the limiting of counter-regulation to those lymph node sites that are reached by activated APCs. Thus, T-regs can continue to prevent autoreactivity from becoming systemic while permitting relaxation of this protection in local regions where there may be injury or infection. These data also indicate how dysregulation of APC activation, migration, and antigen presentation (to T-regs and naive T cells) can lead to autoimmune disease by counter-regulating T-regs in inappropriate locations (22, 23). Additionally, this interpretation may provide insight into other models of autoimmunity in which infection is thought to trigger disease. In most cases, destructive autoimmunity is most readily achieved when the infectious trigger infects the tissue targeted by the autoimmune response (24). In this way, infection can induce APCs to counter-regulate local T-regs. Infection at distant sites may be ineffective as T-regs would continue to protect these areas not reached by activated APC. If normal clearance of activated cells proceeds at these distant sites, this model would explain how stimulation of the immune system may in some cases prevent autoimmune disease.
Our observations in this transplantation system can be generalized to a more global postulate for activation of adaptive immunity. As has been detailed elsewhere, pathogen encounter results in initiation of innate immune processes, a function that includes Toll-like receptor-based APC activation. We hypothesize that like transplantation or LPS in this study, pathogen encounter upregulates signals on antigen presenting cells that inhibit T-reg function. Therefore, rather than a passive mechanism in which naive cells “out-proliferate” regulatory cells to overwhelm T-reg function, we posit that T-reg function is transiently inhibited in the setting of pathogen encounter due to innate signaling. In support of this hypothesis, table 2 demonstrates that a high T-effector:T-reg ratio can still be suppressed in the established setting, but when the effects of T-regs are inactivated in the acute setting suppression cannot take place and rejection ensues. As this signaling dissipates with pathogen elimination, T-regs then act in concert with other processes, such as activation-induced cell death and passive cell death, to ensure that effector T cells are restrained in order to prevent autoimmunity after pathogen eradication. Another interpretation is that LPS-activated APCs act on the T-eff and alter the ability of effector T cells to be regulated by T-regs.
Chen et al. hypothesize that certain organs, organs that are chronically exposed to the environment, are less susceptible to tolerance induction likely as a result of TLR engagement. In one model, TLR engagement prevented transplant tolerance possibly by blocking recruitment of T-regs, and by blocking TLR signaling transplant tolerance was restored (25). We hypothesize that allowing a graft to heal is a means to eliminate innate immunity activation and promote T-reg function.
In summary, these data indicate that the capacity of transferred antigen specific T-regs to promote allograft survival is determined in part by the inflammatory state of the graft. We suggest that innate activation of antigen presenting cells leads to counter-regulatory signals that transiently silence T-reg function thereby promoting immunity and precluding tolerance development. These findings highlight the importance of counter-regulatory pathways in the allogeneic response in vivo and identify the antigen presenting cell as critical in the generation of the adaptive immune response and as a potential target in therapeutic approaches designed to overcome rejection and induce tolerance to transplanted tissues through preserving regulation. Preliminary experiments in which we examine the suppressor activity of regulatory T cells from non-transgenic TCR mice in the context of transplantation demonstrate that these data are not specific to the transgenic TCR model.
Acknowledgments
Supported by NIH R01 AI-048820 and K01 DK079207-02
References
- 1.Lee MKt, Moore DJ, Markmann JF. Regulatory CD4+CD25+T cells in prevention of allograft rejection. Front Biosci. 2003;8:s968–981. doi: 10.2741/1164. [DOI] [PubMed] [Google Scholar]
- 2.Lee MKt, Moore DJ, Jarrett BP, Lian MM, Deng S, Huang X, et al. Promotion of allograft survival by CD4+CD25+ regulatory T cells: evidence for in vivo inhibition of effector cell proliferation. J Immunol. 2004;172(11):6539–6544. doi: 10.4049/jimmunol.172.11.6539. [DOI] [PubMed] [Google Scholar]
- 3.Thornley TB, Brehm MA, Markees TG, Shultz LD, Mordes JP, Welsh RM, et al. TLR agonists abrogate costimulation blockade-induced prolongation of skin allografts. J Immunol. 2006;176(3):1561–1570. doi: 10.4049/jimmunol.176.3.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pasare C, Medzhitov R. Toll pathway-dependent blockade of CD4+CD25+ T cell-mediated suppression by dendritic cells. Science. 2003;299(5609):1033–1036. doi: 10.1126/science.1078231. Epub 2003 Jan 1016. [DOI] [PubMed] [Google Scholar]
- 5.Stephens GL, McHugh RS, Whitters MJ, Young DA, Luxenberg D, Carreno BM, et al. Engagement of glucocorticoid-induced TNFR family-related receptor on effector T cells by its ligand mediates resistance to suppression by CD4+CD25+ T cells. J Immunol. 2004;173(8):5008–5020. doi: 10.4049/jimmunol.173.8.5008. [DOI] [PubMed] [Google Scholar]
- 6.Kirberg J, Baron A, Jakob S, Rolink A, Karjalainen K, von Boehmer H. Thymic selection of CD8+ single positive cells with a class II major histocompatibility complex-restricted receptor. J Exp Med. 1994;180(1):25–34. doi: 10.1084/jem.180.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih FF, Cerasoli DM, Caton AJ. A major T cell determinant from the influenza virus hemagglutinin (HA) can be a cryptic self peptide in HA transgenic mice. Int Immunol. 1997;9(2):249–261. doi: 10.1093/intimm/9.2.249. [DOI] [PubMed] [Google Scholar]
- 8.Jordan MS, Riley MP, von Boehmer H, Caton AJ. Anergy and suppression regulate CD4(+) T cell responses to a self peptide. Eur J Immunol. 2000;30(1):136–144. doi: 10.1002/1521-4141(200001)30:1<136::AID-IMMU136>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 9.Trani J, Moore DJ, Jarrett BP, Markmann JW, Lee MK, Singer A, et al. CD25+ immunoregulatory CD4 T cells mediate acquired central transplantation tolerance. J Immunol. 2003;170(1):279–286. doi: 10.4049/jimmunol.170.1.279. [DOI] [PubMed] [Google Scholar]
- 10.Billingham RE, Brent L, Medawar PB. Activity acquired tolerance of foreign cells. Nature. 1953;172(4379):603–606. doi: 10.1038/172603a0. [DOI] [PubMed] [Google Scholar]
- 11.Lee MKt, Huang X, Jarrett BP, Moore DJ, Desai NM, Moh Lian M, et al. Vulnerability of allografts to rejection by MHC class II-restricted T-cell receptor transgenic mice. Transplantation. 2003;75(8):1415–1422. doi: 10.1097/01.TP.0000064296.65628.6C. [DOI] [PubMed] [Google Scholar]
- 12.Lee MKt, Moore DJ, Chiaccio M, Lian MM, Deng S, Mohiuddin M, et al. T-reg mediated suppression of the allograft response in the draining lymph node. Transplantation. 2006;81(7):1063–1066. doi: 10.1097/01.tp.0000168365.80771.5a. [DOI] [PubMed] [Google Scholar]
- 13.Jordan MS, Boesteanu A, Reed AJ, Petrone AL, Holenbeck AE, Lerman MA, et al. Thymic selection of CD4+CD25+ regulatory T cells induced by an agonist self-peptide. Nat Immunol. 2001;2(4):301–306. doi: 10.1038/86302. [DOI] [PubMed] [Google Scholar]
- 14.Larkin J, 3rd, Picca CC, Caton AJ. Activation of CD4+ CD25+ regulatory T cell suppressor function by analogs of the selecting peptide. Eur J Immunol. 2007;37(1):139–146. doi: 10.1002/eji.200636577. [DOI] [PubMed] [Google Scholar]
- 15.Lee MK, Moore DJ, Jarrett BP, Lian MM, Deng S, Huang X, et al. Promotion of allograft survival by CD4+CD25+ regulatory T cells: evidence for in vivo inhibition of effector cell proliferation. J Immunol. 2004;172(11):6539–6544. doi: 10.4049/jimmunol.172.11.6539. [DOI] [PubMed] [Google Scholar]
- 16.Penfield JG, Wang Y, Li S, Kielar MA, Sicher SC, Jeyarajah DR, et al. Transplant surgery injury recruits recipient MHC class II-positive leukocytes into the kidney. Kidney Int. 1999;56(5):1759–1769. doi: 10.1046/j.1523-1755.1999.00741.x. [DOI] [PubMed] [Google Scholar]
- 17.Takeuchi O, Sims TN, Takei Y, Ramassar V, Famulski KS, Halloran PF. Differential usage of class II transactivator promoters PI and PIV during inflammation and injury in kidney. J Am Soc Nephrol. 2003;14(11):2823–2832. doi: 10.1097/01.asn.0000094084.18567.cc. [DOI] [PubMed] [Google Scholar]
- 18.Zhang N, Schroppel B, Lal G, Jakubzick C, Mao X, Chen D, et al. Regulatory T cells sequentially migrate from inflamed tissues to draining lymph nodes to suppress the alloimmune response. Immunity. 2009;30(3):458–469. doi: 10.1016/j.immuni.2008.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chauhan SK, Saban DR, Lee HK, Dana R. Levels of Foxp3 in regulatory T cells reflect their functional status in transplantation. J Immunol. 2009;182(1):148–153. doi: 10.4049/jimmunol.182.1.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medzhitov R, Janeway CA., Jr Innate immune recognition and control of adaptive immune responses. Semin Immunol. 1998;10(5):351–353. doi: 10.1006/smim.1998.0136. [DOI] [PubMed] [Google Scholar]
- 21.Matzinger P. The danger model: a renewed sense of self. Science. 2002;296(5566):301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 22.Wheat W, Kupfer R, Gutches DG, Rayat GR, Beilke J, Scheinman RI, et al. Increased NF-kappa B activity in B cells and bone marrow-derived dendritic cells from NOD mice. Eur J Immunol. 2004;34(5):1395–1404. doi: 10.1002/eji.200324490. [DOI] [PubMed] [Google Scholar]
- 23.Piganelli JD, Martin T, Haskins K. Splenic macrophages from the NOD mouse are defective in the ability to present antigen. Diabetes. 1998;47(8):1212–1218. doi: 10.2337/diab.47.8.1212. [DOI] [PubMed] [Google Scholar]
- 24.Horwitz MS, Bradley LM, Harbertson J, Krahl T, Lee J, Sarvetnick N. Diabetes induced by Coxsackie virus: initiation by bystander damage and not molecular mimicry. Nat Med. 1998;4(7):781–785. doi: 10.1038/nm0798-781. [DOI] [PubMed] [Google Scholar]
- 25.Chen L, Wang T, Zhou P, Ma L, Yin D, Shen J, et al. TLR engagement prevents transplantation tolerance. Am J Transplant. 2006;6(10):2282–2291. doi: 10.1111/j.1600-6143.2006.01489.x. [DOI] [PubMed] [Google Scholar]