Abstract
Background
Few prospective studies have investigated the relationship between spousal cigarette smoking and the risk of incident stroke.
Methods
Stroke-free participants in the U.S.-based Health and Retirement Study (HRS) aged ≥50 years and married at baseline (n=16,225) were followed, on average, 9.1 years between 1992 and 2006) for proxy or self-report of first stroke (1130 events). Participants were stratified by gender and own smoking status (never-smokers, former smokers, or current smokers), and the relationship assessed between the spouse’s smoking status and the risk of incident stroke. Analyses were conducted in 2007 with Cox proportional hazards models. All models were adjusted for age; race; Hispanic ethnicity; Southern birthstate; parental education; paternal occupation class; years of education; baseline income; baseline wealth; obesity; overweight; alcohol use; and diagnosed hypertension, diabetes, or heart disease.
Results
Having a spouse who currently smoked was associated with an increased risk of first stroke among never-smokers (hazard ratio =1.42, 95% CI=1.05, 1.93) and former smokers (hazard ratio=1.72, 95% CI=1.33, 2.22). Former smokers married to current smokers had a stroke risk similar to respondents who themselves smoked.
Conclusions
Spousal smoking poses important stroke risks for never-smokers and former smokers. The health benefits of quitting smoking likely extend to both the individual smoker and his or her spouse.
Introduction
Secondhand tobacco smoke (SHS) exposure is now widely accepted as a risk factor for coronary heart disease incidence and mortality.1 However, few studies are available regarding the association between SHS and stroke risk, and the results are inconsistent.1–9 The 2006 Surgeon General’s report on SHS concluded that evidence was “suggestive but not sufficient to infer a causal relationship between exposure to secondhand smoke and an increased risk of stroke.”1 It was hypothesized that current or former spousal smoking would increase the risk of first-stroke onset among never, former, or current smokers.
Methods
The Health and Retirement Study (HRS) is a national, longitudinal survey of U.S. adults aged ≥50 years and their spouses.10–12 Enrollments occurred in 1992, 1993, 1998, and 2004, staggered by birth cohort. Biennial interviews (or proxy interviews for decedent participants) were conducted through 2006. Original survey response rates (70%–81%) and retention rates through the last interview (86%–90%) were good. HRS participants born between 1900 and 1953 were eligible for inclusion here if they were interviewed directly (not via proxy) and reported themselves to be both married and stroke-free at baseline. For participants enrolled before age 50, baseline was defined as the first interview after their 50th birthday. The HRS is approved by the University of Michigan Health Sciences Human Subjects Committee.
From 18,768 eligible participants, these were excluded: 73 (0.4%) with unknown baseline stroke status; 939 (5.0%) reporting prior stroke at enrollment; 529 (2.8%) with no available follow-up data; 859 (4.6%) with unknown own or spousal smoking status; and 143 (0.8%) missing adult risk-factor information. Final analyses included 16,225 respondents.
Incident events were defined as first nonfatal or fatal strokes, based on self-report of doctors’ diagnoses and month/year of event. Transient ischemic attacks were not coded as strokes. No information on stroke subtypes was obtained. For deceased participants unavailable for direct interviews, proxy informants—predominantly spouses—were interviewed. Stroke events for which the exact month in the 2-year interview interval was unknown (n=184 with no information and n=50 with stroke year only) were assigned a month based on the median month for events with known dates.
Smoking status referred to cigarettes and did not include pipe or cigar use. Spouses were cross-classified as never, former, or current smokers using baseline self-report.
Covariates (defined at baseline) include race (black/other); Hispanic ethnicity; age and age-squared; gender; Southern birthstate13,14; mother’s and father’s education (≥8/<8 years, plus indicators for unknown); father’s occupation (ranked 0–3, plus army/farming/unknown); own years of education; household income and wealth; overweight (BMI 25–<30) or obese (BMI ≥30); alcohol use (ever/never); and diagnoses of hypertension, diabetes, or heart disease. Standard RAND Corporation coding of health covariates, income, and wealth were used.15 Income and wealth were measured in 1992 dollars, adjusted for household size, and transformed by taking the natural log to reduce the substantial right skew to the distribution of these variables.
Cox proportional hazard models were used to estimate hazard ratios for stroke risk associated with spousal current and former smoking (relative to never smoking) among never-smokers, former smokers, and current smokers. Hazard ratios were calculated, associated with each combination of own/spousal smoking status relative to never-smokers married to never-smokers. Survival was defined as time from baseline interview to date of first stroke, proxy-reported death, or last interview.
The HRS employed a multistage, clustered sample design. To account for the complex sample design, all models were adjusted for major determinants of oversampling (race/ethnicity) and report 95% CIs obtained by clustered, bias-corrected bootstraps with 1000 resamples.16,17 Conventional CIs were nearly identical for all analyses examined.
Results
Over an average of 9.1 years of follow-up on 16,225 eligible respondents (mean baseline age 61), 1130 incident strokes were reported (crude stroke incidence=7.7 events/1000 person-years). Among never-smokers, current spousal smoking predicted a 42% increase in stroke hazard (95% CI=1.02, 1.92; Table 1). Among former smokers, current spousal smoking was associated with 1.72 (95% CI=1.31, 2.24) times the stroke risk compared to former smokers whose spouses had never smoked. Among current smokers, spousal smoking status did not increase stroke risk. Although the CIs are wider in gender-stratified analyses, the parameter estimates are very similar for men and women.
Table 1.
Spousal smoking status and hazard of incident stroke, stratified by own smoking status and gender
| Events | Person-years | Never-smokers HR (95% CI) | Former smokers HR (95% CI) | Current smokers HR (95% CI) | |
|---|---|---|---|---|---|
| Total | |||||
| Spouse never-smoker | 422 | 56,492 | ref | ref | ref |
| Spouse former smoker | 442 | 61,752 | 0.96 (0.75, 1.22) | 1.08 (0.88, 1.33) | 0.89 (0.63, 1.29) |
| Spouse current smoker | 266 | 29,059 | 1.42 (1.02, 1.92) | 1.72 (1.31, 2.24) | 1.03 (0.75, 1.49) |
| Men | |||||
| Spouse never-smoker | 234 | 36,419 | ref | ref | ref |
| Spouse former smoker | 164 | 20,948 | 0.81 (0.48, 1.33) | 0.98 (0.77, 1.25) | 0.91 (0.54, 1.51) |
| Spouse current smoker | 135 | 13,162 | 1.63 (0.83, 2.70) | 1.76 (1.31, 2.41) | 0.92 (0.61, 1.43) |
| Women | |||||
| Spouse never-smoker | 98 | 20,073 | ref | ref | ref |
| Spouse former smoker | 278 | 40,805 | 1.02 (0.77, 1.41) | 1.28 (0.77, 2.21) | 0.98 (0.54, 2.18) |
| Spouse current smoker | 131 | 15,897 | 1.46 (1.00, 2.18) | 1.56 (0.91, 3.12) | 1.31 (0.71, 2.97) |
Note: All models adjusted for self-reported race (black versus all other); Hispanic ethnicity; baseline age and age-squared; gender; Southern birthstate; mother’s and father’s education (≥8/<8 years); father’s occupation; own years of education; baseline household income and wealth; overweight; obese; ever drink alcohol; doctor’s diagnosis of hypertension, diabetes, or heart disease. See text for detailed description. Person-years do not sum precisely due to rounding. CIs are based on clustered bias-corrected bootstrap with 1000 resamples.
HR, hazard ratio
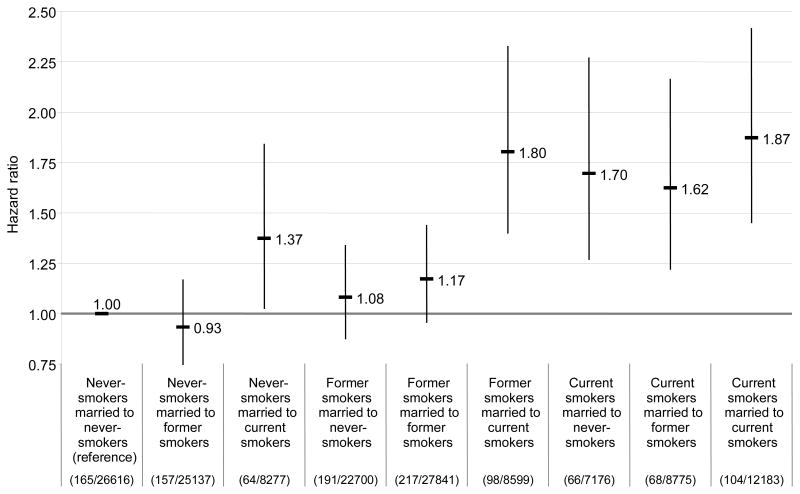
In couples in which either spouse currently smoked, both spouses had an elevated stroke risk compared to never-smokers married to never-smokers (Figure 1). Both former smokers married to current smokers (hazard ratio=1.80; 95% CI=1.40, 2.37) and current smokers married to current smokers (hazard ratio=1.87; 95% CI=1.50, 2.48) had nearly double the stroke risk as never-smokers married to never-smokers.
Figure 1.
Hazard ratios and 95% CIs for risk of first stroke by own and spousal smoking status among married HRS participants aged ≥50 years. Numbers in parentheses are the number of events/person-years of follow-up. Estimates are covariate-adjusted as described in the text. CIs are based on clustered bias-corrected bootstrap with 1000 resamples.
HRS, Health and Retirement Study
Discussion
This study found that prospectively assessed spousal smoking predicted an increased risk of first-incident stroke among never-smokers and former smokers. Spouses who formerly smoked did not confer any extra risk compared to spouses who never smoked. These findings are consistent with growing evidence that SHS increases the risk of stroke.1 The original hypothesis was partially supported, but no evidence was found that former spousal smoking increased stroke risk or that spousal smoking increased risk among current smokers.
These results differ from recent National Health and Nutrition Examination Survey (NHANES) findings, in which a husband’s smoking status conferred excess stroke risk among smoking women but not among nonsmoking women.2 The current study found that never-smoking women married to currently smoking husbands had an increased stroke risk, compared to never-smoking women married to never-smoking husbands. This apparent discrepancy may arise from inadequate statistical power: the CI for the HRS parameter estimate includes the null when restricted to women only. However, the discrepancy may also be attributable to differences in the samples. Although NHANES and HRS cover similar birth cohorts, NHANES participants are younger and stroke rates are lower than in HRS (3.5/1000 person-years vs 7.7/1000 person-years). Lower absolute stroke rates in NHANES result in larger relative effect estimates.18 The older HRS sample may also introduce a survival/selection phenomenon that obscures effects in current smokers. The effects of spousal smoking on high-risk current smokers may induce stroke at relatively young ages. Early strokes are largely excluded from the current study’s analyses, because HRS includes participants aged ≥50 years. Because nonsmokers have lower overall stroke risks, spousal smoking may emerge as a detectable risk factor for nonsmokers only at older ages. Among currently smoking women at baseline, spousal smoking was a significant risk factor for prevalent stroke at enrollment in HRS (results not shown).
The current analysis has some limitations. Self- and proxy-reported strokes correspond imperfectly with hospital-recorded strokes.19–22 Self-reported risk factors are vulnerable to misreporting or measurement error, and the study did not consider whether the effects of spousal smoking vary by the intensity or duration of exposure. Some of the adult characteristics included as model covariates may themselves be affected by spousal smoking. If so, these effect estimates likely underestimate the true risk due to statistical overadjustment. However, the primary results were not very sensitive to alternative covariate sets (results available from the authors).
Smoking status was classified at baseline, but approximately 15% of spouses quit smoking in each successive interview wave (some subsequently restarted). With the accumulation of quitting over follow-up, it is estimated that for ~40% of the exposure time classified as currently smoking spouse, the spouses were actually former smokers. Correcting for this misclassification inflates effect estimates substantially. For example, assuming that spousal former smokers do not increase stroke risk, the adjusted hazard-ratio estimate for never-smokers married to current smokers would increase from 1.4 to approximately 1.7 (relative to never-smokers married to never-smokers). The estimates presented here are probably underestimates, because the long-term effects of spouses’ smoking behavior on one another’s smoking have not been considered. Nonsmokers likely discourage smoking in their spouses; this may be the most important pathway through which smokers influence their spouses’ health.
These findings indicate that spousal smoking increases stroke risk among nonsmokers and former smokers. The health benefits of quitting smoking likely extend beyond individual smokers to affect their spouses, potentially multiplying the benefits of smoking cessation.
Acknowledgments
The authors gratefully acknowledge financial support from the U.S. National Institute of Aging (AG023399) and a seed grant from the Robert Wood Johnson Foundation Health and Society Program at Columbia University. Maria Glymour is a Robert Wood Johnson Foundation Health and Society Scholar at Columbia University. Mauricio Avendano was supported by a grant from The Netherlands Organisation for Scientific Research (NWO, grant no. 451-07-001) and a Fellowship from the Erasmus University.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.USDHHS. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta GA: CDC, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [PubMed] [Google Scholar]
- 2.Qureshi AI, Suri MFK, Kirmani JF, Divani AA. Cigarette smoking among spouses: another risk factor for stroke in women. Stroke. 2005;36:E74–6. doi: 10.1161/01.STR.0000177475.30281.7f. [DOI] [PubMed] [Google Scholar]
- 3.Bonita R, Duncan J, Truelsen T, Jackson RT, Beaglehole R. Passive smoking as well as active smoking increases the risk of acute stroke. Tob Control. 1999;8:156–160. doi: 10.1136/tc.8.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iribarren C, Darbinian J, Klatsky AL, Friedman GD. Cohort study of exposure to environmental tobacco smoke and risk of first ischemic stroke and transient ischemic attack. Neuroepidemiology. 2004;23:38–44. doi: 10.1159/000073973. [DOI] [PubMed] [Google Scholar]
- 5.Donnan GA, McNeil JJ, Adena MA, O’Malley HM, Doyle AE, Neill GC. Smoking as a risk factor for cerebral ischemia. Lancet. 1989;2:643–7. doi: 10.1016/s0140-6736(89)90894-5. [DOI] [PubMed] [Google Scholar]
- 6.Lee PN, Chamberlain J, Alderson MR. Relationship of passive smoking to risk of lung-cancer and other smoking-associated diseases. Br J Cancer. 1986;54:97–105. doi: 10.1038/bjc.1986.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howard G, Wagenknecht LE, Cai JW, Cooper L, Kraut MA, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29:913–7. doi: 10.1161/01.str.29.5.913. [DOI] [PubMed] [Google Scholar]
- 8.You RX, Thrift AG, McNeil JJ, Davis SM, Donnan GA. Ischemic stroke risk and passive exposure to spouses’ cigarette smoking. Am J Public Health. 1999;89:572–5. doi: 10.2105/ajph.89.4.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandler DP, Comstock GW, Helsing KJ, Shore DL. Deaths from all causes in non-smokers who lived with smokers. Am J Public Health. 1989;79:163–7. doi: 10.2105/ajph.79.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juster F, Suzman R. An overview of the health and retirement study. J Hum Resour. 1995;30 (S):S7–56. [Google Scholar]
- 11.Heeringa SG, Connor J. Technical description of the Health and Retirement Study sample design. Ann Arbor MI: Survey Research Center, University of Michigan; 1995. HRS/AHEAD Documentation Report. Report No.: DR-002. [Google Scholar]
- 12.Ofstedal MB, McAuley GF, Herzog AR. HRS/AHEAD Documentation Report. Ann Arbor MI: Survey Research Center, University of Michigan; 2002. Documentation of cognitive functioning measures in the health and retirement study. hrsonline.isr.umich.edu/docs/userg/HRSSAMP.pdf. [Google Scholar]
- 13.Lackland DT, Egan BM, Jones PJ. Impact of nativity and race on “stroke belt” mortality. Hypertension. 1999;34:57–62. doi: 10.1161/01.hyp.34.1.57. [DOI] [PubMed] [Google Scholar]
- 14.Glymour MM, Avendano MP, Berkman LF. Is the stroke belt worn from childhood? Risk of first stroke and state of residence in childhood and adulthood. Stroke. 2007;38:2415–21. doi: 10.1161/STROKEAHA.107.482059. [DOI] [PubMed] [Google Scholar]
- 15.StClair P, Blake D, Bugliari D, et al. RAND HRS data documentation, Version G. 2007 rand.org/labor/aging/dataprod/randhrsg.pdf.
- 16.Carpenter J, Bithell J. Bootstrap confidence intervals: When, which, what? A practical guide for medical statisticians. Stat Med. 2000;19:1141–64. doi: 10.1002/(sici)1097-0258(20000515)19:9<1141::aid-sim479>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 17.Rust K, Rao J. Variance estimation for complex surveys using replication techniques. Stat Methods Med Res. 1996;5:283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- 18.Howard G, Goff DC. A call for caution in the interpretation of the observed smaller relative importance of risk factors in the elderly. Ann Epidemiol. 1998;8:411–4. doi: 10.1016/s1047-2797(98)00041-6. [DOI] [PubMed] [Google Scholar]
- 19.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: the Tromso study. Stroke. 2000;31:1602–7. doi: 10.1161/01.str.31.7.1602. [DOI] [PubMed] [Google Scholar]
- 20.Beckett M, Weinstein M, Goldman N, Lin YH. Do health interview surveys yield reliable data on chronic illness among older respondents? Am J Epidemiol. 2000;151:315–23. doi: 10.1093/oxfordjournals.aje.a010208. [DOI] [PubMed] [Google Scholar]
- 21.Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147:969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 22.Magaziner J, Bassett SS, Hebel JR, Gruber-Baldini A. Use of proxies to measure health and functional status in epidemiologic studies of community-dwelling women aged 65 years and older. Am J Epidemiol. 1996;143(3):283–92. doi: 10.1093/oxfordjournals.aje.a008740. [DOI] [PubMed] [Google Scholar]