Abstract
Background
To estimate the associations of weight dynamics with physical functioning and mortality in older adults.
Methods
Longitudinal cohort study using prospectively collected data on weight, physical function, and health status in four U.S. Communities in the Cardiovascular Health Study. Included were 3,278 participants (2,013 women and 541 African Americans), aged 65 or older at enrollment, who had at least five weight measurements. Weight was measured at annual clinic visits between 1992 and 1999, and summary measures of mean weight, coefficient of variation, average annual weight change, and episodes of loss and gain (cycling) were calculated. Participants were followed from 1999 to 2006 for activities of daily living (ADL) difficulty, incident mobility limitations, and mortality.
Results
Higher mean weight, weight variability, and weight cycling increased the risk of new onset of ADL difficulties and mobility limitations. After adjustment for risk factors, the hazard ratio (95% confidence interval) for weight cycling for incident ADL impairment was 1.28 (1.12, 1.47), similar to that for several comorbidities in our model, including cancer and diabetes. Lower weight, weight loss, higher variability, and weight cycling were all risk factors for mortality, after adjustment for demographic risk factors, height, self-report health status, and comorbidities.
Conclusions
Variations in weight are important indicators of future physical limitations and mortality in the elderly and may reflect difficulties in maintaining homeostasis throughout older ages. Monitoring the weight of an older person for fluctuations or episodes of both loss and gain is an important aspect of geriatric care.
Keywords: Weight change, ADL, Mortality
FLUCTUATIONS in weight in older persons may indicate difficulty maintaining homeostasis and therefore may be an early indication of declining health. Low body weight, weight loss, and weight instability have been associated with increased mortality in a number of studies (1–15). In older adults, there is some evidence that being overweight does not increase risk for mortality (3,7,16), but obesity at all ages remains a significant predictor of disability (16,17). Less well defined are the associations of weight changes with new onset of functional difficulty, where associations were seen in subgroups defined by sex or starting weight, but were not consistently observed for all participants, and where weight change was estimated from self-reported weight at an earlier age or during short-term follow-up of a cohort (18–21). For both mortality and functional impairment, questions remain about the significance of weight changes, in particular weight variability and weight cycling, when observed over time in older persons, a situation distinct from self-reported changes in weight from a much younger age.
Using measured weights over 7 years from participants in the Cardiovascular Health Study (CHS), we explored the associations of mean weight and variability about the mean, average weight change per year, and episodes of weight cycling, with new onset of functional difficulties and mortality among persons aged 65 and older. We hypothesized that higher weight and weight variability would predict incident functional impairment and that weight loss, variability, and cycling would predict mortality in this older cohort, even after adjustment for self-reported health and comorbidities.
METHODS
The CHS
The CHS is a population-based study of risk factors for cardiovascular disease (CVD) in older adults, sponsored by the National Heart, Lung, and Blood Institute (22). Participants aged 65 and older were recruited from random samples of Medicare eligibility lists in four communities: Sacramento County, California; Washington County, Maryland; Forsyth County, North Carolina; and Pittsburgh, Pennsylvania; and from age-eligible participants in the same household. Potential participants were excluded if they were institutionalized, wheelchair bound in the home, or under active treatment for cancer, including hospice care, radiation, or chemotherapy. An original cohort of 5,201 participants was enrolled in 1989–1990, and a second cohort of 687, predominately African Americans, was enrolled 3 years later in order to increase the diversity of the cohort. The combined cohort of 5,888 was 57.6% women and 15.7% Black. The average age at enrollment was 72.8 (±5.6) years. Participants provided written informed consent, and study methods were approved by the institutional review boards at each participating center. Details of the design and recruitment have been published (22,23).
Semiannual contacts alternated between clinic visits and phone calls through 1999, and phone calls continue through the present time. Components of the annual exams varied, but consistently included medical history, medication use, measurement of weight, and self-reported health status. In 2005–2006, participants were seen again in their home or the clinic to assess physical and cognitive function.
Study Participants and Time Line
The current analysis includes participants who were alive at the end of the annual clinic visits in 1999 and who had at least five measurements of weight between 1992 and 1999.
In order to define four summary measures from weight history, at least four weights must be observed. Because the opportunity to observe weight cycling depends on the number of weight measurements and length of time under observation, only weight measurements from the time of enrollment of the second cohort were considered, for a maximum of seven weight measurements per person, and only persons with five or more weights were included to minimize the likelihood of misclassifying weight cycling. Participants were followed for survival and functional status to the time of the 2005–2006 visits.
Definitions
Measurements defining each participant's weight history from 1992 to 1999 included mean weight, average rate of change, calculated as the slope of the regression line of weight on year, the coefficient of variation (CV) about the mean, defined as the standard deviation divided by the mean, and an indicator for weight cycling (Figure 1). Weight cycling was present if the participant both lost and gained greater than or equal to 5% of their body weight over time, when weight changes were evaluated yearly by comparing current weight against weight in the previous year and the initial year. For each year in turn, participants were classified as stable, if weight changed by less than 5% from the prior year and from baseline; weight loss (gain) if the participant lost (gained) 5% of body weight between consecutive visits or from baseline, without an intervening 5% gain (loss); and unstable or cycling after undergoing both a 5% loss and gain. Once a participant experienced a loss or gain, he/she remained in the loss or gain group unless and until weight changed sufficiently in the opposite direction to qualify as weight cycling. Weight pattern groups summarizing the cumulative observed pattern of loss, gain, stable, or cycling (unstable) were also defined. We use the phrase “weight summary measures” to refer to the four trajectory summaries of mean weight, slope, CV, and the indicator for weight cycling, and the term “weight pattern” to indicate the groups defined by loss, gain, stable, or unstable (cycling).
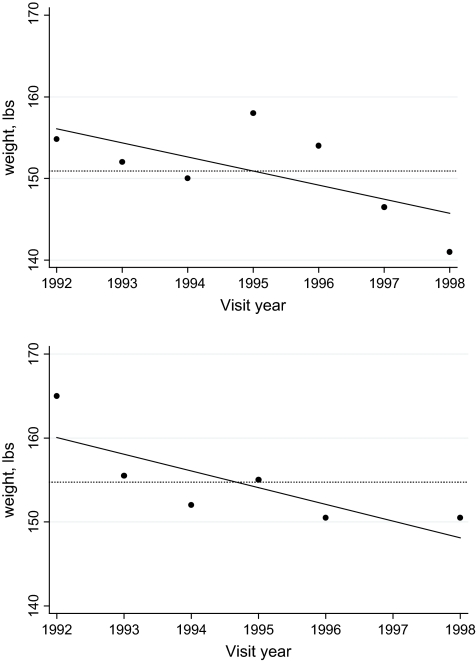
Figure 1.
Illustration of four weight measures. Points = observed weights; solid line = regression of weight on study year; dotted line = mean weight; squared distance from points to dotted line are components of the standard deviation, the numerator of the coefficient of variation. Top figure includes weight cycling; bottom figure does not.
Two measures of physical function were considered. Physical disability was defined as any difficulty with one or more of six activities of daily living (ADL): walking around the home, dressing, eating, bathing, toileting, or getting out of a bed or chair. Mobility impairment was defined as self-reported difficulty walking up 10 steps or walking half a mile. Questions on functioning were asked at 6-month intervals between 1999 and 2005–2006, except for the year 2003–2004, when these questions were not included in the telephone interview.
Health status was self-reported as excellent, very good, good, fair, or poor and recoded for analysis into good or better versus fair or poor. Diabetes was defined based on taking medications for diabetes. Hypertension was defined as a seated blood pressure greater than 140/90 mmHg or a reported history of hypertension along with use of antihypertensive medications. Lung ailments included self-report of doctor-confirmed chronic bronchitis, emphysema, or asthma. Cancer was defined as any hospitalization for cancer. Cardiovascular events, including angina, myocardial infarction, congestive heart failure, claudication, stroke, and transient ischemic attack, were self-reported and then medical records obtained and adjudicated by committee as previously described (24). Coronary heart disease included angina, myocardial infarction, bypass surgery, or angioplasty. Deaths were identified during regular 6-month contacts, by proxy informants, medical records, and obituaries, and are 100% complete.
Statistical Analysis
Participants alive in 1998–1999 but excluded from the analysis due to insufficient data were compared against those included using chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous measures. Pearson correlation coefficients (25) were computed to evaluate pairwise associations between the weight summary measures. Participant characteristics and comorbidities were compared across weight pattern groups using chi-square tests and ANOVA as appropriate. Pairwise comparisons were assessed, using a Bonferroni (25) correction for the overall p value. Cox proportional hazards regressions (26) were used to estimate the relative risks associated with the weight summary measures for incident ADL difficulty, incident mobility difficulty, and mortality. The four weight summary measures were included simultaneously in the multivariable models. Incident ADL impairment and mobility impairment were computed from phone follow-up data between 1999 and 2005–2006 among participants without the difficulty in 1998–1999. Dates of impairment were estimated as the median date between the time the impairment was first reported and the previous contact. Participants with incomplete follow-up were censored after their last follow-up contact or death. All analyses were adjusted for age, sex, race, height, and high school education, measured at baseline, and any of the following, determined in 1998–1999, that were significantly associated with the outcome: current smoking, diabetes, osteoporosis, self-reported health, hypertension, lung ailments, cancer, congestive heart failure, coronary heart disease, claudication, stroke, or transient ischemic attack. The significant covariate variables were entered first into the multivariable models, and associations of the continuous weight summary measures were assessed for nonlinearity by examining residual plots and testing the significance of quadratic effects in the models. Interactions of mean weight with slope and interactions of the weight summary measures with sex and race were evaluated for significance. Sensitivity analyses were performed that included only those participants who self-reported good to excellent health in 1998–1999, in order to reduce the likelihood that weight changes were due to poor health. Regression analyses were repeated using the weight pattern groups instead of the four weight summary measures for comparability with results reported in the literature.
RESULTS
A total of 4,199 participants were alive at the time of their 1998–1999 annual follow-up and 3,963 (94.4%) were contacted. Of those, 3,278 (82.7%) had at least five measurements of weight and were included in the analysis for mortality. Those included were healthier, younger, and had less cognitive and functional difficulty than those excluded, but did not differ by baseline weight or average weight change (among those with at least two weight measurements). After excluding participants with ADL or mobility difficulty, 2,492 were at risk for new onset of ADL difficulty and 2,136 for mobility difficulty. Characteristics of the cohort in 1998–1999 are shown in Table 1. The mean age was 80 years; 16.5% were African American and 61.4% (2,013) were women.
Table 1.
Description of Cohort in 1998–1999 and Associations With Weight Changes, 1992–1999
| All,N = 3,278 | Weight Loss, N = 1,057 a | Stable Weight, N = 862 b | Weight Gain, N = 632 c | Weight Cycling, N = 727 d | p Value* | |
| Male sex | 1,265 (38.6) | 369 (34.9) | 411 (47.7) | 241 (38.1) | 244 (33.6) | <.001; ab, bc, bd |
| Black race | 542 (16.5) | 190 (18.0) | 104 (12.1) | 105 (16.6) | 143 (19.7) | <.001; ab, bd |
| High school graduate | 2,473 (75.4) | 766 (72.5) | 688 (79.8) | 490 (77.5) | 529 (72.8) | <.001; ab, bd |
| Age, y | 80.0 (4.65) | 80.9 (4.9) | 79.3 (4.2) | 79.0 (4.3) | 80.2 (4.8) | <.001; ab, ac, ad, bd, cd |
| Weight, lbs | 157 (32.4) | 149 (31) | 162 (31) | 167 (32) | 155 (33) | <.001; ab, ac, ad, bd, cd |
| CV of weight | 0.035 (0.022) | 0.045 (0.024) | 0.016 (0.005) | 0.031 (0.013) | 0.049 (0.023) | <.001; all pairs |
| Current smoker | 216 (6.6) | 82 (7.8) | 36 (4.2) | 38 (6.0) | 60 (8.3) | .003; ab, bd |
| Diabetes | 367 (11.2) | 138 (13.1) | 69 (8.0) | 66 (10.4) | 94 (12.9) | .002; ab, bd |
| Hypertensive | 2,096 (64.0) | 668 (63.2) | 533 (61.8) | 413 (65.4) | 482 (66.4) | .23 |
| CHF | 401 (12.2) | 157 (14.8) | 66 (7.7) | 53 (8.4) | 125 (17.2) | <.001; ab, ac, bd, cd |
| CHD | 896 (27.3) | 314 (29.7) | 198 (23.0) | 154 (24.4) | 230 (31.6) | <.001; ab, bd, cd |
| Claudication | 109 (3.33) | 37 (3.5) | 16 (1.9) | 15 (2.4) | 41 (5.6) | <.001; bd, cd |
| Stroke | 262 (8.0) | 95 (9.0) | 49 (5.7) | 40 (6.3) | 78 (10.7) | .001; ab, bd, cd |
| TIA | 135 (4.1) | 48 (4.5) | 27 (3.1) | 25 (4.0) | 35 (4.8) | .32 |
| Osteoporosis | 440 (13.5) | 135 (12.8) | 105 (12.2) | 84 (13.4) | 116 (16.0) | .13 |
| Lung ailments | 468 (14.3) | 153 (14.5) | 112 (13.0) | 90 (14.3) | 113 (15.6) | .54 |
| Any cancer | 641 (19.6) | 205 (19.4) | 155 (18.0) | 119 (18.8) | 162 (22.3) | .17 |
| Fair or poor health | 947 (28.9) | 359 (34.0) | 173 (20.1) | 142 (22.5) | 273 (37.6) | <.001; ab, ac, bd, cd |
| ADL difficulty | 786 (25.1) | 272 (27.1) | 153 (18.6) | 144 (23.6) | 217 (31.2) | <.001; ab, ac, bd, cd |
| Mobility difficulty | 1,143 (37.0) | 425 (43.1) | 213 (26.1) | 201 (33.40) | 304 (44.3) | <.001; ab, ac, bc, bd, cd |
Notes: Entries are N (%) for categorical variables and mean (SD) for continuous variables. ADL = activities of daily living; CHD = coronary heart disease; CHF = congestive heart failure; CV = coefficient of variation; TIA = transient ischemic attack.
The lettered pairs identify significantly different weight pattern groups, after correcting for multiple comparisons (see Statistical Analysis).
Statistics describing the weight trajectory summary measures and the weight patterns appear in Table 2. Note that weight cycling is common to both our summary and pattern constructs, and the results for weight cycling appear only once in the table, under the heading of “weight patterns.” The average weight change was a loss of approximately three-fourth pounds per year, with women losing more on average than men. Nearly one fourth of the women and one fifth of the men experienced weight cycling, 20% of whom had more than one episode of cycling.
Table 2.
Summaries of Weight History, 1992–1999
| Women, N = 2,013 | Men, N = 1,265 | All, N = 3,278 | |
| Mean weight, lbs | 150 (30.0) | 176 (27.4) | 160 (31.6) |
| Weight change, lbs/y | −0.76 (2.22) | −0.68 (2.07) | −0.73 (2.16) |
| Weight variability, CV | 0.038 (0.024) | 0.031 (0.020) | 0.035 (0.022) |
| Weight patterns, N (%) | |||
| Loss | 688 (34.2) | 369 (29.2) | 1,057 (32.2) |
| Stable | 451 (22.4) | 411 (32.5) | 862 (26.3) |
| Gain | 391 (19.4) | 241 (19.0) | 632 (19.3) |
| Cycling (unstable) | 483 (24.0) | 244 (19.3) | 727 (22.2) |
Note: Entries are mean (SD) unless otherwise noted. lbs = pounds; CV = coefficient of variation.
Because our conceptual model required simultaneous entry of four weight trajectory summary measures, we first explored the linear correlations among them. The CV of weight was negatively correlated with both the mean weight (r = −.13) and the slope (r = −.51) and positively correlated with weight cycling (r = .32), all p < .0001. Although the linear correlation of the CV with slope was fairly strong, the relationship was v shaped indicating that the CV was higher in participants whose absolute weight change was greater in either direction. Despite its positive correlation with the CV, the weight cycling measure was needed to capture the aspect of both loss and gain, which is not necessarily captured by the CV as demonstrated in Figure 1. The figure shows two individuals with similar mean weights, slopes, and CVs, but one experienced weight cycling and the other did not. To further distinguish these two measures, note that weight cycling is absent in the presence of large unidirectional weight changes, when the CV is high, and is present with changes in both directions, which, if close to the 5% threshold, may not result in a large CV.
Changes in weight during the 7-year period were highly associated with participant characteristics and health status measures at the end of the period (Table 1). Men were more likely than women to remain at a stable weight, and African Americans were less likely to lose weight or experience weight fluctuations than Caucasians. Participants who experienced weight loss or weight fluctuations were generally older, in poorer overall health, more likely to be current smokers, and to have diabetes or CVD than those who remained stable or gained weight. ADL and mobility difficulties were greater in participants who experienced weight loss or fluctuations compared with those who remained stable or who gained weight.
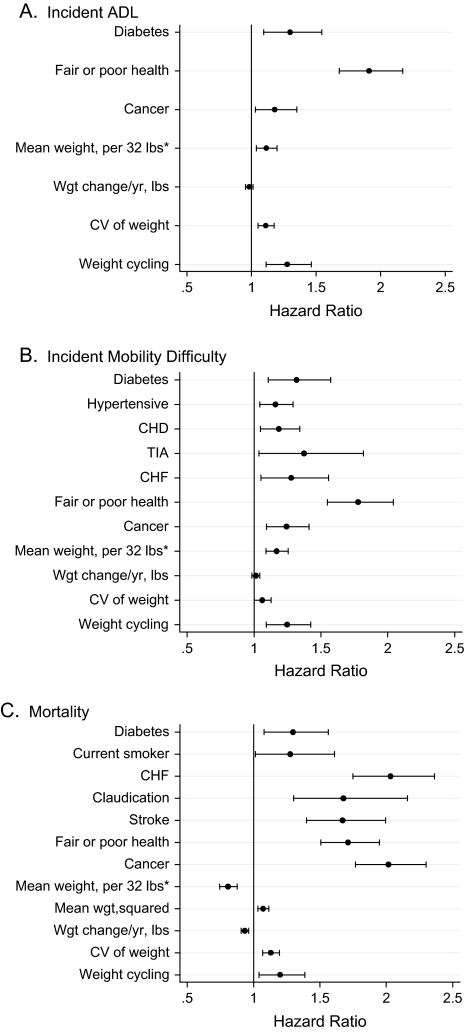
Among the participants without ADL difficulty in 1999, 1,350 (54%) reported new difficulty during follow-up, including 866 (58%) women and 484 (48%) men. After adjustment for age, sex, race, height, high school education, diabetes, cancer, and self-reported health, higher mean weight, weight variability, and weight cycling were associated with an increased risk of ADL impairment (Table 3 and Figure 2A). The table provides two columns of results for each weight dynamic: in the first column, models were adjusted for height and demographics, and in the second column, additionally adjusted for self-reported health and comorbidities. A history of weight cycling increased the risk of ADL difficulty by 28%, a risk estimate similar to those for diabetes and cancer (Figure 2A). In addition, each standard deviation increase in the CV increased risk by 11%. Results were similar for incident mobility difficulty (Table 3 and Figure 2B), which was very common in this cohort. A total of 1,537 participants (72%) of those at risk developed a mobility difficulty during follow-up, including 945 (76%) women and 592 (66%) men. Results were unchanged when limited to participants with self-reported good to excellent health in 1998–1999. There were no interactions of the weight summary measures with sex or race, and neither initial weight nor mean weight modified associations of the other weight summary measures with functional outcomes.
Table 3.
Adjusted* Hazard Ratios of Weight Summaries by Outcome
| Incident ADL† | Incident Mobility Difficulty‡ | Mortality§ | |
| No. of cases/no. at risk | 1,350/2,492 | 1,537/2,136 | 1,072/3,278 |
| Model 1. Trajectory summaries | |||
| Mean weight, per 32 lbs‖ | 1.14 (1.07, 1.22); 1.11 (1.04, 1.19) | 1.16 (1.05, 1.20); 1.12 (1.05, 1.20) | 0.87¶ (0.81, 0.94); 0.83¶ (0.77, 0.89) |
| Weight change, lbs/y | 0.98 (0.95, 1.01); 0.98 (0.95, 1.01) | 1.01 (0.98, 1.04); 1.01 (0.99, 1.04) | 0.93 (0.90, 0.96); 0.93 (0.91, 0.96) |
| Weight variability, per SD of CV | 1.14 (1.08, 1.21); 1.11 (1.05, 1.17) | 1.11 (1.05, 1.18); 1.07 (1.01, 1.13) | 1.21 (1.14, 1.28); 1.13 (1.07, 1.20) |
| Weight cycling | 1.30 (1.14, 1.50); 1.28 (1.12, 1.47) | 1.25 (1.09, 1.42); 1.25 (1.09, 1.42) | 1.39 (1.21, 1.61); 1.20 (1.04, 1.39) |
| Model 2. Weight patterns# | |||
| Loss | 1.32 (1.15, 1.53); 1.27 (1.10, 1.46) | 1.14 (1.00, 1.31); 1.08 (0.95, 1.24) | 1.82 (1.54, 2.17); 1.58 (1.33, 1.88) |
| Stable | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Gain | 1.04 (0.88, 1.23); 1.03 (0.87, 1.22) | 1.10 (0.95, 1.27); 1.06 (0.91, 1.22) | 1.14 (0.92, 1.40); 1.10 (0.89, 1.36) |
| Cycling (unstable) | 1.64 (1.40, 1.92); 1.54 (1.32, 1.80) | 1.44 (1.25, 1.67); 1.36 (1.18, 1.58) | 2.20 (1.83, 2.63); 1.66 (1.38, 2.00) |
Notes: ADL = activities of daily living; CHD = coronary heart disease; CHF = congestive heart failure; CV = coefficient of variance; lbs = pounds; TIA = transient ischemic attack.
Results in the first rows are adjusted for age, sex, height, race, and high school education. Results in the second rows are additionally adjusted for self-reported health and comorbidities, with specific adjustment variables given in the footnotes.
Additionally adjusted for diabetes, cancer, and self-reported poor or fair health.
Additionally adjusted for diabetes, hypertension, CHF, CHD, TIA, cancer, and self-reported poor or fair health.
Additionally adjusted for diabetes, CHF, claudication, stroke, current smoking, cancer, and self-reported poor or fair health.
Thirty-two pounds is 1 SD.
At the overall mean weight of 160 pounds; quadratic association found.
Additionally adjusted for starting weight.
Figure 2.
Hazard ratios (95% confidence intervals) for weight measures and comorbidities from multivariable models. (A) Incident activities of daily living (ADL) difficulty. (B) Incident mobility difficulty. (C) Mortality. CHF = congestive heart failure; CV = coefficient of variation; lbs = pounds. *32 lbs = 1 standard deviation. Also adjusted for age, sex, race, height and high school education.
Analyses using weight patterns, instead of the slope, CV, and cycling indicator yielded similar results (Table 3). Risk of ADL impairment was greatest in the unstable group and also elevated in the weight loss group, but not in the weight gain group compared with the stable group. Higher weight remained a risk factor. For new onset of mobility impairment, only the unstable group was significantly different from the stable group in the model adjusted for health status and comorbidities. Weight cycling was the only measure of variability in the weight pattern models, and its association was greater than in the models that also included the CV of weight.
A total of 1,072 (32.7%) of the participants died during follow-up, including 589 women (29.3%) and 483 (38.2%) men. After adjustment for age, sex, race, height, education, self-reported health, current smoking, diabetes, congestive heart failure, claudication, stroke, and cancer, weight loss, weight variability, and weight cycling were all associated with increased risk of mortality (Table 3 and Figure 2C). There was a significant (p = .001) quadratic effect for mean weight, with an inflection point at approximately 205 lbs (pounds) in the multivariable model. The range of mean weights in our study was 73–309 lbs, with only 8% of participants weighing more than 205 lbs. The unadjusted association of mean weight with mortality for men and women indicated a strong increase in risk at the lowest weights, especially for women, and a modest increase again for very high weights. Weight cycling increased risk by 20%, and the combined effect of a 1 SD higher CV plus an episode of weight cycling increased risk of mortality by 36% (95% confidence interval: 19%–56%). Results were unchanged when limited to participants with self-reported good to excellent health in 1998–1999. Results were consistent when weight patterns were modeled (Table 3), although, as before, the relative risk estimate for weight cycling was greater in the absence of the CV of weight. There were no interactions of the weight summary measures with sex or race, and neither initial weight nor mean weight modified associations of the other weight summary measures with mortality.
DISCUSSION
Using four summary measures from weights measured over 7 years in older adults, and patterns of weight change defined by 5% changes in weight, we have shown that higher variability in weight increased the relative risk for physical disability and mortality in the subsequent 7 years. Two measures of weight variability were considered: overall variability about a person's mean weight and weight cycling or weight instability. Both measures of variability were jointly predictive after adjustment for mean weight and average annual weight change. Once variability was considered, average annual weight change was not a risk factor for new onset of physical limitations, but higher mean weight was. Weight loss increased the risk for mortality, and the overall association of mean weight with mortality indicated increased risk with low and very high weights.
Our results support and extend the work of others. Several authors have reported associations of weight, weight loss, and weight variability with mortality (1–15) and of weight and weight change with physical difficulties (16–21), but to our knowledge, no one has evaluated simultaneously all the aspects of weight history captured by the four measures included here. Although intercorrelated, each of the four measures captures a unique aspect of the weight trajectory. In particular, commonly used measures of linear change, or classification into groups by amount and direction of change, fail to account for either variability or weight cycling. The addition of the CV to quantify variability still does not characterize weight cycling, as argued by Jeffrey (27) and illustrated in Figure 1. Further, we have utilized extensive health history data on individuals to evaluate the effect of weight history conditional on current health status. That is, for two individuals with similar risk factor and health status profiles, the one with greater variability in weight is at increased risk for physical impairments and mortality.
Although low weight is a known risk factor for mortality in older persons, a U-shaped association of mortality with body mass index (BMI) has also been reported (28). We found a similar, but flatter association for weight in multivariable models that adjusted for height, although few in the CHS cohort would be at increased risk due to high weight, and in the weight pattern models, neither weight gain nor initial weight were associated with increased risk of mortality. Others have reported a differential effect of weight change by initial weight (15). There was a modestly significant interaction of mean weight with weight change (p = .03) in the analysis for mortality, but it became nonsignificant (p = .09) once weight squared was included in the model. Initial weight was not as strong a predictor as mean weight, and we found no difference in association of overall weight pattern by initial weight or mean weight.
Weight changes, especially weight loss and weight cycling were associated with poorer self-reported health and comorbidities, which increase the risk of mortality and physical limitations. Risk estimates were adjusted for health status in 1999, the end of the period of weight observation, to ascertain the effect of weight changes above and beyond associated conditions. There was little attenuation of demographic-adjusted results after further adjustment for comorbidities, suggesting that health conditions do not explain the associations of weight dynamics with physical limitations or mortality. Sensitivity analyses restricted to participants in good to excellent health yielded identical results. Figure 2(A–C) allows for comparison of the effects of weight summary measures with other risk factors for functional limitations or mortality. The magnitude of the association between weight cycling and mobility limitations or ADL difficulty was similar to that for several comorbidities, such as cancer and diabetes, and the combined effects of variability (CV) and cycling on mortality were similar to those for smoking and diabetes. That weight variability, after adjusting for average weight and weight change per year, would still confer an amount of risk similar to diabetes or smoking is clear indication that weight fluctuations in older persons are not benign. These fluctuations include weight loss followed by recovery and support our hypothesis that the inability to maintain one's weight through periods of illness may be an indication of poorer homeostatic control, with the potential for subsequent health consequences.
To consider further the issue of weight loss followed by recovery, we evaluated consecutive years of weight changes during the time of annual weight measures from 1989–1999 and created indicators for the nine possible pairings of the three states from year to year: loss, stable, or gain to represent changes during every 2-year interval. We found that all patterns of change except for gain–stable and gain–gain were associated with increased odds of mortality compared with the stable–stable group, after adjustment for age, sex, race, current weight, and comorbidities. In particular, the pattern of weight loss followed by gain had an odds ratio (95% confidence interval) of 2.20 (1.46, 3.30), which was not significantly different from the odds of 2.57 (2.11, 3.13) for the stable–loss group or 2.59 (1.67, 4.01) for the gain–loss group. Only the loss–loss group had a significantly greater odds ratio of 4.17 (2.78, 6.21). Our power was limited because only 1.2% of the time was a gain directly followed by a loss; so, these results need confirmation in other studies with ample longitudinal measures of weight, but they lend support to our findings that weight changes are associated with adverse outcomes, even if weight loss is followed by a gain.
Current literature on weight and physical functioning documents the strong effect of obesity on disability (16,17). Associations of weight change with physical functioning were reported by Houston and Lee (19,20). Houston and colleagues found an association of weight change from age 25 to middle age with increased ADL limitations, but results were not consistent across race and sex groups and weight variability was not considered, nor would these results necessarily apply to an older population. Lee and colleagues explored weight change, weight change intention, and incidence of mobility limitation over 30 months in adults aged 70–79 years. They found that weight loss and weight fluctuation were associated with mobility limitation only in participants with lower BMI. We did not find any differences in associations by initial weight, mean weight, sex, or race. In our analyses of weight patterns, weight loss was associated with incident ADL difficulty; but when the four weight summary measures were used, weight change per year was not significant. This may be due to the higher weight variability seen in the weight loss group (Table 1), and once variability was separately accounted for, weight loss in itself was not a risk factor. This is further supported by an exploration of significance in the multivariable models, where, after controlling for covariates, slope was significantly associated with new ADL difficulties when other weight summary measures were not included in the model and lost significance once the CV was entered.
Strengths of our work include use of measured rather than self-reported weights, a focus on current weights in older persons rather than comparisons with recalled weights at an earlier age, enough repeated weight measurements to capture weight cycling, 7 years of follow-up beyond the weight trajectory measures, and adjustment for risk factors and health status at the end of the trajectory. A limitation of our work is that we have not considered intentionality of weight changes. It is unlikely that a single reason explained a participant's weight changes during the 7 years of the trajectory, making it difficult to classify; so, we have chosen instead to adjust for health conditions that would influence both the weight history and the outcomes of interest. Several studies have shown that episodes of unexplained weight loss are associated with poor health outcomes in geriatric outpatients, but these studies typically only consider weights over periods of a year or less. Episodes of severe illness may be associated with periods of weight loss, and weight regain may occur during the recovery period. So, despite the fact that we adjusted for many common comorbidities and overall health status, part of the association between weight dynamics and outcomes may reflect to some extent the underlying disease burden in our participants.
Our findings suggest that monitoring the weight of an older person for fluctuations or episodes of both loss and gain is an important aspect of geriatric care. Patients who are able to maintain a stable weight through periods of illness may represent those with better homeostatic control, and conversely, those who are unable to maintain a stable weight may be at increased risk for physical disability or mortality.
FUNDING
The research reported in this article was supported by the National Institute on Aging R01-AG-023629. The CHS was supported from contracts N01-HC-35129, N01-HC-45133, N01-HC-75150, N01-HC-85079 through N01-HC-85086, N01 HC-15103, N01 HC-55222, and U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. Additional support was provided through R01-AG-15928, R01-AG-20098, and R01-AG-027058 from the National Institute on Aging, HL-075366 from the National Heart, Lung, and Blood Institute, and the University of Pittsburgh Claude. D. Pepper Older Americans Independence Center P30-AG-024827.
Acknowledgments
Parts of the article were presented at the Gerontological Society of America meeting in November 2007. A full list of principal CHS investigators and institutions can be found at http://www.chs-nhlbi.org/pi.htm. The authors have no conflicts of interest, and the funding agency did not participate in preparation of the manuscript.
References
- 1.Lissner L, Odell PM, D'Agostino RB, et al. Variability of body weight and health outcomes in the Framingham population. N Engl J Med. 1991;324:1839–1844. doi: 10.1056/NEJM199106273242602. [DOI] [PubMed] [Google Scholar]
- 2.Corrada MM, Kawas CH, Mozaffar F, Paganini-Hill A. Association of body mass index and weight change with all-cause mortality in the elderly. Am J Epidemiol. 2006;163:938–949. doi: 10.1093/aje/kwj114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diehr P, O'Meara ES, Fitzpatrick A, Newman AB, Kuller L, Burke G. Weight, mortality, years of healthy life, and active life expectancy in older adults. J Am Geriatr Soc. 2008;56(1):76–83. doi: 10.1111/j.1532-5415.2007.01500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 5.Wannamethee SG, Shaper AG, Walker M. Weight change, weight fluctuation, and mortality. Arch Intern Med. 2002;162:2575–2580. doi: 10.1001/archinte.162.22.2575. [DOI] [PubMed] [Google Scholar]
- 6.Rzehak P, Meisinger C, Woelke G, Brasche S, Strube G, Heinrich J. Weight change, weight cycling and mortality in the ERFORT male cohort study. Eur J Epidemiol. 2007;22:665–673. doi: 10.1007/s10654-007-9167-5. [DOI] [PubMed] [Google Scholar]
- 7.Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP. Weight change in old age and its association with mortality. J Am Geriatr Soc. 2001;49(10):1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- 8.Folsom AR, French SA, Zheng W, Baxter JE, Jeffery RW. Weight variability and mortality: the Iowa Women's Health Study. Int J Obes Relat Metab Disord. 1996;20(8):704–709. [PubMed] [Google Scholar]
- 9.Diaz VA, Mainous AG, Everett CJ. The association between weight fluctuation and mortality: results from a population-based cohort study. J Comm Health. 2005;30(3):153–165. doi: 10.1007/s10900-004-1955-1. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen ND, Center JR, Eisman JA, Nguyen TV. Bone loss, weight loss, and weight fluctuation predict mortality risk in elderly men and women. J Bone Miner Res. 2007;22:1147–1154. doi: 10.1359/jbmr.070412. [DOI] [PubMed] [Google Scholar]
- 11.Yaar S, Goldbourt U. Voluntary and involuntary weight loss: associations with long term mortality in 9,228 middle-aged and elderly men. Am J Epidemiol. 1998;148:546–555. doi: 10.1093/oxfordjournals.aje.a009680. [DOI] [PubMed] [Google Scholar]
- 12.French SA, Folsom AR, Jeffery RW, Williamson DF. Prospective study of intentionality of weight loss and mortality in older women: the Iowa Women's Health Study. Am J Epidemiol. 1999;149:504–514. doi: 10.1093/oxfordjournals.aje.a009844. [DOI] [PubMed] [Google Scholar]
- 13.Mikkelsen KL, Heitmann BL, Keiding N, Sorensen TIA. Independent effects of stable and changing body weight on total mortality. Epidemiology. 1999;10:671–678. [PubMed] [Google Scholar]
- 14.Blair SN, Shaten J, Brownell K, Collins BS, Lissner L. Body weight change, all-cause mortality, and cause-specific mortality in the Mulitple Risk Factor Intervention Trial. Ann Intern Med. 1993;119:749–757. doi: 10.7326/0003-4819-119-7_part_2-199310011-00024. [DOI] [PubMed] [Google Scholar]
- 15.Somes GW, Kritchevsky SB, Shorr RI, Pahor M, Applegate WB. Body mass index, weight change, and death in older adults: the Systolic Hypertension in the Elderly Program. Am J Epidemiol. 2002;156:132–138. doi: 10.1093/aje/kwf019. [DOI] [PubMed] [Google Scholar]
- 16.Lang IA, Llewellyn DJ, Alexander K, Melzer D. Obesity, physical function, and mortality in older adults. J Am Geriatr Soc. 2008;56:1474–1478. doi: 10.1111/j.1532-5415.2008.01813.x. [DOI] [PubMed] [Google Scholar]
- 17.Stenholm S, Rantanen T, Alanen E, Reunanen A, Sainio P, Koskinen S. Obesity history as a predictor of walking limitation in old age. Obesity. 2007;15:929–938. doi: 10.1038/oby.2007.583. [DOI] [PubMed] [Google Scholar]
- 18.Chen H, Bermudez OI, Tucker KL. Waist circumference and weight change are associated with disability among elderly Hispanics. J Gerontol A Biol Sci Med Sci. 2002;57:M19–M25. doi: 10.1093/gerona/57.1.m19. [DOI] [PubMed] [Google Scholar]
- 19.Houston DK, Stevens J, Cai J, Morey MC. Role of weight history on functional limitations and disability in late adulthood: the ARIC study. Obes Res. 2005;13(10):1793–1802. doi: 10.1038/oby.2005.218. [DOI] [PubMed] [Google Scholar]
- 20.Lee JS, Kritchevsky SB, Tylavsky F, et al. Weight change, weight change intention, and the incidence of mobility limitation in well-functioning community dwelling older adults. J Gerontol A Biol Sci Med Sci. 2005;60A(8):1007–1012. doi: 10.1093/gerona/60.8.1007. [DOI] [PubMed] [Google Scholar]
- 21.Launer LJ, Harris T, Rumpel C, Madams J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994;271(14):1093–1098. [PubMed] [Google Scholar]
- 22.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1(3):263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 23.Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3(4):358–366. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- 24.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 25.Neter John, Kutner Michael H, Nachtsheim Christopher, Wasserman William. Applied Linear Statistical Models. Chicago, IL: McGraw-Hill; 1996. [Google Scholar]
- 26.Collett D. Modelling Survival Data in Medical Research. Boca Raton, FL: Chapman & Hall/CRC; 1999. [Google Scholar]
- 27.Jeffrey RW. Does weight cycling present a health risk? Am J Clinc Nutr. 1996;63(3):452S. doi: 10.1093/ajcn/63.3.452. [DOI] [PubMed] [Google Scholar]
- 28.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]