Abstract
Objective:
The objective of this study was to assess the ability of hockey parents/guardians to recognize concussion symptoms in their 13–14 year old (Bantam-aged) children.
Outcome Measures:
The outcome measures were the ability to recognize different signs and symptoms listed on the Sport Concussion Assessment Tool (SCAT) as well as 8 detractors consisting of signs and symptoms not associated with post concussive syndrome. Additional questions assessing the parents’ knowledge of concussion management and recognition abilities were also posed.
Participants:
Parents of Bantam-aged minor hockey league athletes volunteered for the study.
Methods:
The study investigators distributed questionnaires during the warm up period or following their children’s games to the study participants. Following questionnaire completion, participants were provided with an information package outlining the correct signs and symptoms of concussion.
Results:
The mean number of correct responses to signs and symptoms of concussion was 21.25/25 for the mothers and 20.41/25 for the fathers. The mean number of detractors identified as not associated with concussion was 5.93/8 for the mothers and 4.85/8 for the fathers, indicating that mothers were more capable of recognizing the signs and symptoms than fathers. An analysis of variance including sporting experience in the model did not strengthen the relationship between parent gender and test outcome.
Conclusion:
This investigation revealed that there is still a disconnect in regards to key components of recognizing a concussion, such as difficulty with sleep, disorientation symptoms, and emotional irritability. Mothers have displayed an ability to better differentiate between true and false signs and symptoms of concussion as compared to fathers. Continued education and awareness of mild traumatic brain injury in athletes should address the misconceptions amongst parents in regards to the true signs and symptoms of a concussion.
Keywords: hockey, bantam, concussion, chiropractic
Abstract
Objectif :
L’objectif de cette étude était d’analyser la capacité des parents/tuteurs de hockey à reconnaître les symptômes de commotion chez leurs enfants de 13 et 14 ans (âges bantam).
Critères d’évaluation :
Les critères d’évaluation étaient la capacité à reconnaître les divers signes et symptômes énumérés par l’outil d’évaluation des commotions dans le sport (SCAT), ainsi que huit facteurs défavorables composés de signes et symptômes qui ne sont pas associés au syndrome post-commotion. D’autres questions qui évaluent les capacités des parents par rapport à la connaissance du contrôle et de la reconnaissance des commotions ont également été posées.
Participants :
Des parents d’athlètes de hockey mineur d’âge bantam qui se sont proposés pour participer à l’étude.
Méthodes :
Les chercheurs de l’étude ont distribué des questionnaires aux participants à l’étude au cours de la période d’échauffement ou après les parties des enfants. Une fois les questionnaires remplis, on a fourni aux participants une trousse d’information indiquant les signes et symptômes exacts de commotion.
Résultats :
Le nombre moyen de réponses correctes vis-à-vis des signes et symptômes de commotion était 21,25/25 pour les mères et 20,41/25 pour les pères. Le nombre moyen de facteurs défavorables déterminés comme n’étant pas associés à la commotion était 5,93/8 pour les mères et 4,85/8 pour les pères, ce qui indique que les mères étaient plus en mesure de reconnaître les signes et symptômes que les pères. Une analyse de la variance comprenant l’expérience dans les sports au sein du modèle n’a pas renforcé la relation entre le sexe du parent et les résultats au test.
Conclusion :
Cette enquête a révélé qu’il existe toujours une coupure en ce qui a trait aux éléments clés permettant de reconnaître une commotion, comme la difficulté à dormir, des symptômes de désorientation et l’irritabilité émotionnelle. Les mères ont affiché une meilleure capacité à faire la différence entre les vrais et faux signes et symptômes de commotion que les pères. La sensibilisation continue des traumatismes cérébraux légers chez les athlètes doit aborder les idées fausses des parents en ce qui concerne les véritables signes et symptômes d’une commotion.
Introduction
Concussion is a common type of head injury that can occur in most contact sports. In the “Summary and Agreement Statement of the First International Symposium on Concussion in Sport, Vienna 2001,” concussion is defined as a “complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces.”1
It is thought that some coaches, trainers, and more importantly, parents or guardians don’t realize exactly how a concussion occurs. There are several different constructs in which a concussion occurs and can include the following:
Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an ‘impulsive’ force transmitted to the head.
Concussion typically results in the rapid onset of short-lived impairment of neurological function that resolves spontaneously.
Concussion may result in neuropathological changes but the acute clinical symptoms largely reflect a functional disturbance rather than structural injury.
Concussion results in a graded set of clinical syndromes that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course.
Concussion is typically associated with grossly normal structural neuroimaging studies.2
Perhaps the most common misconception when it comes to recognizing a concussion is the issue surrounding loss of consciousness. Most concussions occur without a loss of consciousness.1,2 In fact, loss of consciousness is just one of many possible signs and symptoms of a concussion.1,2 Loss of consciousness may be suggested if the victim cannot recall events before or after the incident, however this is more consistent of a person experiencing signs of amnesia. Another misconception surrounding concussion is the idea that you must be hit in the head for a concussion to occur. A significant blow to either the neck, face, jaw, or elsewhere in the body can result in a concussion as long as the force is transmitted to the head.1,2 Thus, a concussion can occur from what is normally viewed as a legal body check in the sport of hockey. An analogous model used to understand this phenomenon is that of a sponge in a bucket of water (brain within the skull). Under normal movements the sponge will move within the water freely, but with a jarring force to the bucket the sponge will make contact with the sides of the bucket.
There are many physical, cognitive, and emotional signs and symptoms associated with having sustained a concussion as listed below in Table 1.1,2
Table 1.
The Signs and Symptoms of Concussion
| Physical Symptoms | Cognitive Symptoms | Emotional Symptoms | Physical Signs |
|---|---|---|---|
| Headache | Confusion | Depression | Loss of consciousness |
| Dizziness | Amnesia | Irritability | Poor coordination |
| Nausea | Disorientation | Moodiness | Easily distracted |
| Feeling ‘Unsteady’ | Poor concentration | Poor concentration | |
| Feeling ‘Dinged’ | Memory disturbance | Slow responses | |
| Feeling ‘Stunned’ | Vomiting | ||
| Feeling ‘Dazed” | ‘Glassy eyed’ | ||
| Describe ‘Bell rung’ | Photophobia | ||
| ‘Seeing stars’ | Aphasia | ||
| Visual Disturbances | Personality change | ||
| Tinnitus | Inappropriate behavior | ||
| Diplopia | Decreased physical ability |
Not all of these indicators would be present in a concussion, but if one is present, a concussion should be considered as a possible diagnosis and appropriate referral needs to be advised.2
Early detection and documentation is critical in the management of the concussed athlete. The Vienna & Prague concussion conferences of 2001 and 2004 respectively confirm that the grading of concussions has been abandoned and the management of a concussion is to occur on a case by case basis.1,2 These proceedings also led to the development of a Sport Concussion Assessment Tool (SCAT card), see Appendix A. The SCAT was developed to create a standardized tool to be used for patient education and physician assessment of a concussion. It was developed by combining a variety of existing tools, including: Sideline Evaluation for Concussion-Colorado Head Injury Foundation, Inc [Society, 1990 (revised May 1991)], Management of Concussion Sports Palm Card-American Academy of Neurology & Brain Injury Association,3 Standardized Assessment of Concussions-SAC,4 Sideline Concussion Check-UPMC/Thinksafe/Sports Medicine New Zealand Inc and the Brain Injury Association, McGill Abbreviated Concussion Evaluation (ACE) (unpublished), National Hockey League Physician Evaluation Form (unpublished), UK Jockey Club Assessment of Concussion5 and Maddocks questions.6
The memory questions utilized in the SCAT were modified from the validated Maddocks questions in order to make them less football specific.6 The Maddocks questions included: Which ground are we at? Which team are we playing today? Who is your opponent at present? Which half is it? How far into the quarter is it? Which side scored the last goal? Which team did we play last week? Did we win last week?6
The importance of recognizing even a minor concussion is reinforced through the literature which reports that once an athlete experiences a concussion, the likelihood that they experience a subsequent concussion is increased; and the symptoms experienced in the second concussion may be more severe and take an extended period of time to resolve.7–9 The key to this concept is that once an initial concussion has been recognized, the involved athlete should not return to play until all symptoms have resolved or the risk of subsequent concussion is increased.1,10–21
A main issue in regards to the occurrence of concussions in minor hockey involves body checking. With the rising incidence of traumatic brain injury in hockey22–24 some authors fear that many Canadian youth are exposed to the lasting effects of concussions, some of which are not fully realized until the brain completes its maturation. Marchie et al. acknowledge that while many injuries can be caused by the body checking that occurs in hockey, concussion is a major concern due to the severity of the possible sequelae.24 Of these sequelae, some of the more notable include headache, cognitive/memory and executive-function disturbances, and/or visual abnormalities.25–30
The widespread knowledge of the signs and symptoms of a concussion in contact sports such as hockey would further enhance the accuracy of recognizing this condition. This could be facilitated by knowledge transfer amongst coaching staffs, parents/guardians, and even the players themselves. The National Hockey League (NHL) and Ontario Hockey League (OHL) have surveillance systems in place for the epidemiological analysis and control of concussions during the game, but the incidence of concussion in youth hockey is poorly established. Reporting of concussions in minor hockey is largely based on the players themselves reporting an injury to the bench staff who in turn must recognize the injury and its severity.31 This relies on the assumption that the bench staff, or even the hockey player, is knowledgeable in the important signs and symptoms of concussion. Unfortunately in many cases, this is where the line of communication may stop. When parents/guardians are unaware of what their child has experienced during the game, what is assumed to be a mild headache, or a moody child, could be considered normal.
Although in recent years there have been increases in the knowledge surrounding concussions through educational seminars hosted by associations such as the Greater Toronto Hockey League and Think First Canada, significant knowledge gaps still exist. Currently, studies are being done in diagnostic modalities, imaging, and concussion evaluation. Neuropsychological testing has been found to be an impressive way to assess severity and resolution, while shorter, computer based tests (such as Cog-Sport or ImPACT) are becoming popular adjuncts.2,28,32–46 Although there has been substantial research completed on concussions, this information is not consistently delivered to players’ parents or guardians as it is filtered down through physicians, coaches, and hockey organizations. In a recent study by Valovich-McLeod et al., coaches were surveyed as to their understanding of sport-related concussion.47 This study found that previous coaching experience was predictive of better symptom recognition, and that between 49.4% and 61.5% of coaches were able to answer correctly to four true/false questions on concussion. With this in mind, our study further aims to determine if parents/guardians are capable of identifying the signs and symptoms of a concussion in order to ensure the child receives the proper medical attention.
Methods
A questionnaire was developed in order to gather information from parents of Bantam aged (13–14 year old) athletes participating in the 7th Annual Penguins International Winter Classic hockey tournament (Appendix B). The tournament was hosted on January 19–21st, 2007, at the Chesswood and Westwood arenas in Toronto, Ontario, Canada.
Bantam-aged athletes were chosen because it has been found by Willer et al. that that there is a trend for an increasing occurrence of concussion as age increases.48 Additionally the study by Emery49 analyzed the risk of injury in different age groups of hockey players and found that 45% of all injuries occurred due to body checking. The relative risk of injury in Bantam aged hockey players was 3.72.49 Thus, for the current study, Bantam athletes were chosen because players have been in a body contact age group for at least two seasons and thus would have an increased risk of having sustained a concussion compared to younger players. Additionally, more parents or guardians are typically in attendance for Bantam-aged players compared to the older midget aged players.
This questionnaire was screened for content/wording and approved for inclusion in this study by the Canadian Memorial Chiropractic College Institutional Review Board for Research prior to collecting any data. The bulk of the questions used in this study’s questionnaire were taken from the Sport Concussion Assessment Tool (SCAT) (Appendix A).2 The SCAT was evaluated for face and content validity on the basis of scientific literature50 and clinical experience of the authors.
Our questionnaire (Appendix B) consisted of four demographic questions (a-d), and six additional questions specifically targeting the parent’s knowledge of concussions, signs, and symptoms (numbered 1–6). The questionnaires were distributed to the parents or guardians by hand during the warm up prior to each game or directly following the game. After filling out the questionnaire the parents were given the answer key to the questions posed (Appendix C).
The demographic questions were designed to indicate the level of bantam hockey the child was currently participating in, the child’s current age, the parents’ sporting experience, and their relationship to the child. Information regarding the level of Bantam hockey was collected in order to determine if higher levels of competition would have an effect on the parents’ knowledge. Study investigators were also interested in the parents’ sporting experience to determine if the level of experience of a parent would have a bearing on their knowledge of the signs and symptoms. The next six questions under the heading of ‘Questionnaire’ were designed to determine the parents’ ability to recognize the signs/symptoms and guideline information that is currently being used to determine whether a child has received a blow to the head or body that may be diagnosed as a concussion. Questions 1–4 and 6 were of the Yes/No type while question 5 was unique. Question 5 consisted of twenty-five true or false questions asking the parents to identify signs and symptoms of concussion (see Appendix B, #5). The questionnaire instructed the parents to check true or false depending on whether they believed the items were correct signs or symptoms of a concussion. Of the twenty-five questions there were seventeen true answers and eight false answers.
Specifically the 8 false detractors, which were considered “red herrings” included: difficulty with urination, lowered pulse rate, difficulty with defecation, hearing voices, sinus congestion, feelings of euphoria, inability to swallow, and chest pain. These incorrect signs or symptoms were included in order to avoid the possibility of people guessing all the correct answers, and to make the questionnaire a more thought provoking process.
After the guardian of the child had completed the questionnaire, the questionnaire was collected and placed into an envelope in which it was stored until data analysis could begin.
Data Analysis
For each completed survey the number of correct responses was tabulated for the 25 items (true signs recognized and false signs denied) for a score out of 25 allowing for a normal distribution.
Data analysis used a two sample T-Test to analyze the correct responses to the signs and symptoms both associated and not associated with concussion (the 8 ‘red herrings’). An analysis of variance was utilized to compare the differences in responses to identifying the correct and incorrect signs and symptoms of concussion between the two groups of mothers or fathers with the additional factor of their own participation in sport.
Results
One hundred and seventeen questionnaires were completed and collected from the 120 handed out for a 97.5% response rate. Inclusion criteria for the acceptance of the questionnaire into this study were that all questions were answered and that the questionnaire was fully completed.
Three questionnaires were discarded from the study. Two questionnaires were discarded because they were not completely finished, and one was discarded because no demographic information was listed. Our final number of collected questionnaires used for analysis was 114 (N = 114).
The demographic information revealed that 57% of the athletes were competing at the single ‘A’ level, 42% were competing at the ‘AA’ level, and 1% were competing at the ‘AAA’ level (All star levels progressing from A to AAA). 44% of the athletes were 13-years of age and 56% were 14-years of age. Just under 10% (9.65%) of the guardians participated at a self-rated “high level” of sport, 43.86% of guardians participated at a self rated “medium” level of sport, 29.82% played at a self rated “low level” of sport and 16.67% did not participate in any sport. Of the guardians questioned, 52.63% were mothers of the bantam aged participants and 47.37% were the fathers of the participants. The questionnaire’s demographic information revealed that no male or female legal guardians other than parents were questioned. The demographic information did not show any difference in the answers of the parents of varying sporting experience or with different levels of play for their children.
Questions 1–4 were generally answered correctly by the 114 respondents see table 2 below.
Table 2.
Percentage of Correct Responses Questions 1–4
| Question | Number of correct answers (N=114) |
|---|---|
| 1. Does a loss of consciousness determine whether a concussion has occurred? | 87 (76.32%) |
| 2. Can a player who has suffered a concussion return to play in the same day? | 109 (95.61% |
| 3. A concussion may be caused by a blow to the neck, jaw, or elsewhere in the body? | 99 (86.84%) |
| 4. Is it necessary for a player to be medically evaluated after having their bell rung? | 101 (88.6%) |
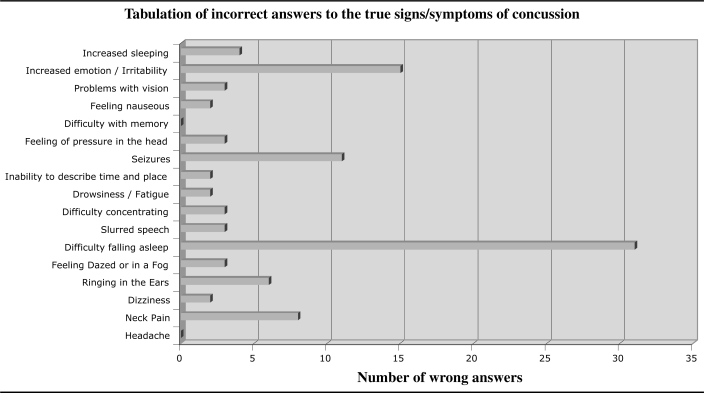
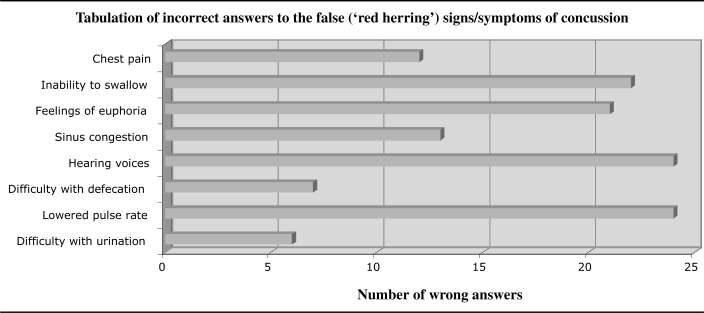
Question 5 tested the ability of the respondent to identify the signs and symptoms that are truly associated with a concussion and deny those that are not. Figure 1 reveals the number of incorrect responses in the attempt to identify the true signs and symptoms of concussion. The number of wrong answers in identifying the false signs and symptoms or ‘red herring’ detractors are displayed in the figure 2 below.
Figure 1.
The number of incorrect answers for the signs and symptoms not identified as being associated with concussion that are indeed related to concussion
Figure 2.
The number of incorrect answers for sign and symptoms identified as being associated with concussion that are not related to concussion
Considering the correct responses to questions 1–5, the 93 respondents or (81.58%) who answered “no” to question 6 (Has your child ever suffered a concussion?) has to be viewed with some degree of skepticism.
Statistical Analysis
A two-sample t test was done to compare the scores mothers and fathers received for the 25 questions. Of the 60 mothers the mean score was 21.25 (standard deviation 2.07, 95% confidence interval 20.71–21.79) while the 54 fathers mean score was 20.41 (standard deviation 2.54, 95% confidence interval 19.71–21.10). The two-sample t test for the 8 false detractors revealed that the mothers mean score was 5.93/8 (standard deviation 2.15, 95% confidence interval 5.38–6.49) while fathers mean score was 4.85/8 (standard deviation 2.65, 95% confidence interval 4.13–5.57). Thus a difference does exist, with the mothers having a better ability to discriminate mild traumatic brain injuries, recognizing the signs or symptoms associated with concussion. An additional analysis of variance that included sporting experience in the model did not strengthen the relationship between parent gender and the test outcome (25 detractors: F = 3.02, p = 0.0848, 8 false detractors: F = 5.04, p = 0.0268)
Discussion
The results of this study indicate that in general the parents surveyed were successful in correctly identifying the signs and symptoms of a concussion in their child. Our analysis of data revealed that mothers were more knowledgeable than fathers in identifying the correct signs and symptoms of concussion. Interestingly, mothers were significantly more capable of recognizing the false signs and symptoms added as detractors. Unfortunately, there have been no other studies analyzing the ability of parents to recognize signs and symptoms, so it is difficult to comment on any contrasting or supporting results.
The 2001 Vienna and the 2004 Prague Statements1,2 were instrumental in aiding the overall awareness of common signs and symptoms of a concussion and resulted in the creation of the Sport Concussion Assessment Tool (SCAT) (Appendix A). The SCAT makes it simpler and more convenient for coaching staffs and parents to become aware of the signs and symptoms of a concussion. Although this study shows that parents are generally aware of the signs and symptoms put forth in the guidelines, it sheds light on areas of confusion that may be overlooked in educational seminars or materials.
In comparison to the correct signs and symptoms, the incorrect signs and symptoms (‘red herring’ detractors) were not answered as well (review Figure 1 and 2). Both hearing voices and lowered pulse rate were incorrectly indicated as true signs/symptoms by 47.4% of the participants. Feelings of euphoria and inability to swallow were answered incorrectly by 43.9% of participants. We suggest that parents indicating these detractors as correct signs and symptoms could be overcautious in analyzing changes in their children’s health or demeanor, or simply that they had the perception that all of the detractors were indeed correct. In the current study, only one subject was found to have chosen all true responses. Although this could potentially lead to an increased reporting and subsequent demand to health care providers, we suggest that this is not likely to occur in reality and that more attention be paid to the commonly overlooked true signs and symptoms.
Of particular importance to recognizing a concussion, it should be noted that all participants answered both the headaches and difficulty with memory correctly as indeed signs/symptoms of a concussion.
The three signs and symptoms that were most commonly not recognized as being part of a concussion were: difficulty falling asleep (54.4% answered incorrectly), inability to describe time and place (28.9% answered incorrectly), and increased emotion/irritability (23.7% answered incorrectly).
The parents of Bantam-aged minor hockey league athletes in this study are reasonably knowledgeable in the common signs and symptoms of concussion. This is a similar result to the recent Valovich-McLeod study47 that found that although coaches are knowledgeable, there are certain signs and symptoms that continue to be overlooked.
Difficulty falling asleep is reported thoroughly throughout the literature as being one of the most common sequelae of a mild traumatic brain injury, along with poor memory and fatigue.51–53 However, the study by Chan et al.,54 analyzed a group of participants who had experienced no head injury and found that sleep disturbance was indicated by 50.6% of their sample. They argued that many of the symptoms indicated on a typical post concussion checklist are commonly endorsed by a normal uninjured population. This was further supported by a similar study by Iverson et al.,55 who argued that the typical symptoms noted in post concussive syndrome (PCS) are not unique to this syndrome. Yet in the Kaufman et al. study,56 the researchers found that participants who had suffered a minor head injury showed lower sleep efficiency with more awake time and with more awakenings lasting more than 3 minutes. There has been recent research into the specificity of the commonly indicated signs and symptoms of PCS,57–59 but this debate is beyond the scope of this paper.
Inability to describe place and time is a typical cognitive feature of a concussion. Often referred to in the literature as being disoriented, the inability to describe place and time can be considered highly indicative of a brain injury. The fact that the current study indicated this feature as being answered incorrectly 28.9% of the time may be concerning to health care providers. Several authors1,2,11,50,59,60 note disorientation as being one of the best prospectively validated indicators that a concussion has occurred. The importance of asking the injured athlete questions regarding their orientation is further emphasized in several papers.11,50,53,60–64
Maddocks53 further addresses the sensitivity of the typical orientation questions such as, “What year is it?” and “How old are you?” noting that these questions are typically sensitive in traumatic motor vehicle accidents, but may be less sensitive when examining a more subtle head injury such as those incurred during sport. In his study, Maddocks compared the correct answers by concussed and non concussed athletes. These questions ranged from recently acquired items (date, time, ground, quarter, last goal, etc) to more long term memory items (name, date of birth, age, year, etc). For those that were found to have sustained a concussion, the number of subjects answering the more recently acquired memory items correctly was significantly lower. In Young’s study,63 it was noted that many of these memory and orientation questions could be affected by the athletes’ level of intelligence. Because of this, they studied the answers to common orientation and memory questions in non-injured athletes. The results of this study showed that some tests (serial sevens) were only answered correctly half the time, whereas a test such as the ‘months of the year in reverse’ (MOYR) was answered correctly by over 90% of participants. Thus, these researchers postulate that it may be wiser to use a test such as MOYR as a sideline evaluation tool.
Irritability is also described by Johnston et al.50 as part of a wide variety of subjective findings that one may discover in a concussed athlete. These researchers also note that the time to resolution from these symptoms is quite variable and difficult to predict. As with many of the studies listed previously, irritability is commonly experienced by those suffering a concussion.1,2,50,54,58–60,65–66 These mood disturbances typically become noticeable at later stages of post concussion, approximately 4–8 weeks later.60 Often it is debated in the literature as to whether irritability is caused by neural damage incurred along with the concussion, or whether it is due to the effects of concussion on slowing cognitive functioning and subsequently causing increased emotional distress in the patient.67 Regardless of the true cause, the fact remains that irritability should be recognized as a symptom of sustaining a mild traumatic brain injury.
In interpreting the data presented in this study, it is important to be aware of the methodological limitations present. Despite adding detractors to the option list for question #5, there is still the possibility that parents simply chose ‘true’ for the entire section. The study investigators found that many parents were either unwilling to accept a questionnaire or rushed when it came to completing the questionnaire. In order to complete the questionnaire in less time, it is possible some parents may have simply chosen ‘true’ for all or most of the statements, without thoroughly reading them. This ‘all true’ scenario was documented only once within our sample, which implies that the questions were taken seriously and answered to the best of the respondents’ abilities. Analyzing the way the selections were actually made in this one questionnaire (deliberate penmanship), further suggests that the subject considered all signs and symptoms to indeed be correct.
The SCAT card had been previously evaluated for face and content validity by Johnston, McCrory, et al.,50 and thus for the present study, the SCAT signs and symptoms were incorporated into the questionnaire with additional false detractors to increase difficulty. Still, it must be considered that the questionnaire may not be measuring what it purports to, as the wording of the questions may not have been equally understood by all participants.
As this study was only directed to parents of children participating in the Bantam age group, the results can only be applied to this particular 13–14 years age group. It could be argued that parents of children in higher or more competitive age groups, or those with multiple children, may have more exposure to the topic of concussions and thus may have a more complete knowledge set. Conversely, one could also suggest that parents of players in a younger, pre-body checking age group may not yet be concerned with concussions in their children, and thus may be unaware of common signs and symptoms. Regardless of this, the study investigators would suggest an early start to the education process of parents with respect to concussion awareness in their children.
Conclusion
According to this study, it appears that the efforts of organizations such as ThinkFirst Canada, the Greater Toronto Hockey League, and individual primary health care providers within the community have largely been successful in increasing the awareness of parents to the signs and symptoms of concussions. However, a complete dissemination of concussion knowledge from researchers and health professionals to parents, still shows a disconnect. Key components of recognizing a concussion, such as difficulty with sleep, disorientation symptoms, and emotional irritability should be better known. The signs and symptoms of concussion require further knowledge transfer to all concerned parties. Continuing attempts to raise awareness for the proper and swift recognition of mild traumatic brain injury in young athletes is recommended. Further investigations towards the identification of concussion and the most effective ways to publicize this information would be prudent to enhance knowledge transfer of this condition.
Appendix A—SCAT card (Sport Concussion Assessment Tool)
| Name:____________________________ | Date:_________ | ||
| Sport/Team:_____________________ | Mouth Guard? | Y | N |
| 1) SIGNS | |||
| Was there loss of consciousness or unresponsiveness? | Y | N | |
| Was there seizure or convulsive activity? | Y | N | |
| Was there a balance problem/unsteadiness? | Y | N | |
| 2) MEMORY | |||
| Modified Maddocks questions (check those correct) | |||
| At what venue are we? _____ | Which half is it? ____ | Who scored last? ____ | What team did we play last? ____ |
| Did we win last game? ____ | |||
| 3) SYMPTOM SCORE | |||
| Total number of positive symptoms (from “ SYMPTOMS” box on other side of the card) =________ | |||
| 4) COGNITIVE ASSESSMENT(Check those correct) | |||
| 5 word recall (Examples) | Immediate | Delayed (after concentration tasks) | |
| Word 1_______ | cat | ____ | ____ |
| Word 2_______ | pen | ____ | ____ |
| Word 3_______ | shoe | ____ | ____ |
| Word 4_______ | book | ____ | ____ |
| Word 5_______ | car | ____ | ____ |
| Months in reverse order (circle those incorrect) Jun-May-Apr-Mar-Feb-Jan-Dec-Nov-Oct-Sep-Aug-Jul | |||
| OR | |||
| Digits backwards (check those correct) | |||
| 5–2–8 | 3–9–1 | ____ | |
| 6–2–9–4 | 4–3–7–1 | ____ | |
| 8–3–2–7–9 | 1–4–9–3–6 | ____ | |
| 7–3–9–1–4–2 | 5–1–8–4–6–8 | ____ | |
| Ask delayed 5-word recall now | |||
| 5) NEUROLOGICAL SCREENING | |||
| Pass | Fail | ||
| Speech | ____ | ____ | |
| Eye Motion and Pupils | ____ | ____ | |
| Pronator Drift | ____ | ____ | |
| Gait Assessment | ____ | ____ | |
| Any neurologic screening abnormality necessitates formal neurologic or hospital assessment. | |||
6) RETURN TO PLAY
ATHLETES SHOULD NOT BE RETURNED TO PLAY THE SAME DAY OF INJURY
When returning athletes to play, they should follow a stepwise symptom-limited program, with stages of progression. For example:
rest until asymptomatic (physical and mental rest)
light aerobic exercise (e.g. stationary cycle)
sport-specific training
non-contact training drills (start light resistance training)
full contact training after medical clearance
return to competition (game play)
There should be approximately 24 hours (or longer) for each stage and the athlete should return to stage 1 if symptoms recur. Resistance training should only be added in the later stages.
Medical clearance should be given before return to play.
INSTRUCTIONS:
This card is for the use of medical doctors, physiotherapists or athletic therapists. In order to maximize the information gathered from the card, it is strongly suggested that all athletes participating in contact sports complete a baseline evaluation prior to the beginning of their competitive season. This card is a suggested guide only for sports concussion and is not meant to assess more severe forms of brain injury.
Signs:
Assess for each of these items and circle – Y (yes) or N (no)
Memory:
Select any 5 words (an example is given). Avoid choosing related words such as “dark” and “moon” which can be recalled by means of word association. Reach each word at a rate of one word per second. The athlete should not be informed of the delayed testing of memory (to be done after the reverse months and/or digits). Choose a different set of words each time you perform a follow-up exam with the same candidate.
SYMPTOMS:
Headache, “pressure in the head,” neck pain, balance problems or dizziness, nausea or vomiting, vision problems, hearing problems or ringing in the ears, “don’t feel right,” feeling “dinged” or “dazed,” confusion, feeling slowed down, feeling like in a “fog,” drowsiness, fatigue or low energy, emotional, irritable, difficulty concentrating or remembering
Concentration/Attention:
Ask the athlete to recite the months of the year in reverse order, starting with a random month. Do not start with December or January. Circle any months not recited in the correct sequence.
For digits backwards, if correct, go to the next string length. If incorrect, read trail 2. Stop after incorrect on both trials.
Neurologic Screening:
Trained medical personnel must administer this examination. These individuals might include medical doctors, physiotherapists or athletic therapists. Speech should be assessed for fluency and lack of slurring. Eye motion should reveal no diplopia in any of the 4 planes of movement (vertical, horizontal and both diagonal planes). The pronator drift is performed by asking the patient to hold both arms in front of them, palms up, with eyes closed. A positive test is pronating the forearm, dropping the arm, or drift away from midline. For gait assessment, ask the patient to walk away from you, turn and walk back.
Return to Play:
A structured, graded exertion protocol should be developed; individualized on the basis of sport, age and the concussion history of the athlete. Exercise or training should be commenced only after the athlete is clearly asymptomatic with physical and cognitive rest. A doctor should ideally make final decision for clearance to return to competition.
This tool represents a standardized method of evaluating people after concussion in sport. This tool has been produced as part of the Summary and Agreement Statement of the Second International Symposium on Concussion in Sport, Prague, 2004. For more information see the “Summary and Agreement Statement of the Second International Symposium on Concussion in Sport” in the:
Clinical Journal of Sports Medicine 2005; in press
British Journal of Sports Medicine 2005; 39: 196–204
Neurosurgery 2005; in press
Physician and Sportsmedicine 2005; in press
Appendix B. – Questionnaire
| Demographic Information: | |||||
| a) Please indicate the level of Bantam Hockey your child participates in: | |||||
| 1 A | □ | ||||
| 2 AA | □ | ||||
| 3 AAA | □ | ||||
| b) Please indicate your child’s current age: | |||||
| 1 12 years | □ | ||||
| 2 13 years | □ | ||||
| 3 14 years | □ | ||||
| c) Have you/do you participate in high level (ex. Pro or semi pro), medium level (ex. Competitive leagues), or low level (ex. Recreational) sports: | |||||
| 1 High level | □ | ||||
| 2 Medium level | □ | ||||
| 3 Low/Rec. level | □ | ||||
| 4 No sport participation | □ | ||||
| d) What is your status of guardianship to the participating child? | |||||
| 1 Mother | □ | ||||
| 2 Father | □ | ||||
| 3 Male Legal Guardian | □ | ||||
| 4 Female Legal Guardian | □ | ||||
| Questionnaire: | |||||
| 1) Does a loss of consciousness determine whether a concussion has occurred? (Please check one) | |||||
| □ Yes 1 | □ No 2 | ||||
| 2) Can a player who has suffered a concussion return to play in the same day? (Please check one) | |||||
| □ Yes 1 | □ No 2 | ||||
| 3) A concussion may be caused by a blow to the neck, jaw, or elsewhere in the body? (Please check one) | |||||
| □ Yes 1 | □ No 2 | ||||
| 4) Is it necessary for a player to be medically evaluated after having their bell rung? (Please check one) | |||||
| □ Yes 1 | □ No 2 | ||||
| 5) The following are signs and symptoms of concussion. (Please circle True or False) | |||||
| T | F | Headache | |||
| T | F | Neck pain | |||
| T | F | Difficulty with urination | |||
| T | F | Dizziness | |||
| T | F | Lowered pulse rate | |||
| T | F | Ringing in the ears | |||
| T | F | Feeling dazed or in a “fog” | |||
| T | F | Difficulty with defecation | |||
| T | F | Difficulty falling asleep | |||
| T | F | Slurred speech | |||
| T | F | Difficulty concentrating | |||
| T | F | Drowsiness/fatigue | |||
| T | F | Hearing voices | |||
| T | F | Sinus congestion | |||
| T | F | Inability to describe time and place | |||
| T | F | Seizures | |||
| T | F | Feelings of euphoria | |||
| T | F | Inability to swallow | |||
| T | F | Chest pain | |||
| T | F | Feeling of “pressure” in the head | |||
| T | F | Difficulty with memory | |||
| T | F | Feeling nauseous | |||
| T | F | Problems with vision | |||
| T | F | Increased emotion/irritability | |||
| T | F | Increased sleeping | |||
| 6) Has your child ever suffered a concussion? (Please check one) | |||||
| □ Yes 1 | □ No 2 | ||||
Appendix C. —Information handed out to parents after survey
Thank you for participating in our study! The purpose of this study was to assess the ability of a parent/guardian to recognize the proper signs and symptoms of a concussion in their child. You were asked to answer “yes/no” or “True/False” to a series of statements. Here is a list of the CORRECT answers:
Q#1 Does a loss of consciousness determine whether a concussion has occurred? (Please check one) ANSWER: no, a concussion can occur without a loss of consciousness!!
Q#2 Can a player who has suffered a concussion return to play in the same day? (Please check one) ANSWER: absolutely not
Q#3 A concussion may be caused by a blow to the neck, jaw, or elsewhere in the body? ANSWER: yes, a concussion can occur from a blow to anywhere in the body if the force is subsequently transferred to the head
Q#4 Is it necessary for a player to be medically evaluated after having their bell rung? ANSWER: YES
Q#5 This question asked you to circle “true/false” for a variety of signs and symptoms. These are the CORRECT signs and symptoms of a concussion:
| Headache | Neck pain |
| Dizziness | Ringing in the ears |
| Feeling dazed or in a “fog” | Difficulty falling asleep |
| Slurred speech | Difficulty concentrating |
| Drowsiness/fatigue | Inability to describe time and place |
| Seizures | Feeling of “pressure” in the head |
| Difficulty with memory | Feeling nauseous |
| Problems with vision | Increased emotion/irritability |
| Increased sleeping |
The following signs and symptoms were INCORRECT:
| Difficulty with urination | Lowered pulse rate |
| Difficulty with defecation | Hearing voices |
| Sinus congestion | Feelings of euphoria |
| Inability to swallow | Chest pain |
Additional Information on Concussions
A concussion is defined as a traumatically induced physiological disruption of brain function with a short period of altered or loss of consciousness. This cannot be seen on CT or X rays. It affects the way your child thinks and remembers things and may cause a variety of symptoms.
What do I do if my child suffers a concussion??
Your child should STOP playing immediately! They should not be left alone and should be taken for evaluation at soon as possible. If the child has lost consciousness, they should be taken to the hospital by ambulance. Do not move the child until paramedics arrive.
How long will it take for my child to recover?
Signs and symptoms often last for 7–10 days, but my last longer. In some cases, the child may take weeks or months to recover. If your child has had a previous concussion, it may take longer for them to recover.
How is a concussion treated?
The best treatment for concussion is rest. They should not exercise, go to school or do any activities that may make them worse. If your child goes back to activity too soon, their symptoms may get worse, or be present longer.
When can my child return to school?
Sometimes a child that suffers a concussion can find it difficult to concentrate and could potentially feel ill or get a headache if they are in school. Children should stay at home if their symptoms get worse while attending school. Once they feel better, they can try going back to school at first for half days and if they are okay with that, then they can go back full time.
When can my child return to sport?
It is very important that your child not go back to sports if he/she has any concussion symptoms or signs. Return to sport and activity must follow a step-wise approach:
No activity, complete rest. Once back to normal and cleared by a doctor, go to step 2.
Light exercise such as walking or stationary cycling, for 10–15 minutes.
Sport specific activity (ie. skating in hockey, running in soccer), for 20–30 minutes.
“On field” practice with body contact, once cleared by a doctor.
Game play.
Note: Each step must take a minimum of one day. If your child has any symptoms of a concussion (e.g. headache, feeling sick to his/her stomach) that come back either during activity, or later that day, your child should stop the activity immediately and rest for 24 hours. Your child should be seen by a doctor and cleared again before starting the step wise protocol again.
When should I take my child to the doctor?
Every child who gets a head injury should be seen by a doctor as soon as possible. You should take him/her back to the doctor IMMEDIATELY if, after being told your child has a concussion, he/she has worsening of symptoms such as:
being more confused
has a headache that is getting worse
vomits more than once
doesn’t wake up
has any trouble walking
has a seizure
has strange behaviour
No child should go back to sport until they have been cleared to do so by a doctor.
Please take note of the true signs and symptoms of a concussion and seek proper evaluation if you suspect your child has potentially sustained a concussion. If you would like more information about the purposes or results of this study, please feel free to contact us:
Dr. Scott Howitt, Craig Coghlin, Bryan Myles
Canadian Memorial Chiropractic College
6100 Leslie Street
North York, ON
M2H 3J1
416-482-2340 ext. 395
showitt@cmcc.ca
Adapted from: Dr. L. Purcell and Dr. J. Kissick on behalf of the ThinkFirst-SportSmart Concussion Education and Awareness Program. July 2005 Version.
References
- 1.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the first international conference on concussion in sport, Vienna 2001: Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. British Journal of Sports Medicine. 2002;36:6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrory P, Johnston K, Meeuwisse W, Aubry M, Cantu R, Dvorak J, Graf-Baumann T, Kelly J, Lovell M, Schamasch P. Summary and agreement statement of the 2nd International conference on concussion in sport, Prague 2004. Clinical Journal of Sports Medicine. 2005;15:2. doi: 10.1097/01.jsm.0000159931.77191.29. [DOI] [PubMed] [Google Scholar]
- 3.Kelly J, Rosenberg J. Diagnosis and management of concussion in sports. Neurology. 1997;48:575–580. doi: 10.1212/wnl.48.3.575. [DOI] [PubMed] [Google Scholar]
- 4.McCrea M, Randolph C, Kelly J. The Standardized Assessment of Concussion (SAC): Manual for Administration, Scoring and Interpretation. 2nd Edition. Waukesha, WI: 2000. [Google Scholar]
- 5.Turner M. Concussion and head injuries in horse racing. In: Turner M, editor. The Jockey Club Conference on Head Injury in Sport. London: The Jockey Club of England; 1998. 1998. [Google Scholar]
- 6.Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clin J Sports Med. 1995;5:32–35. doi: 10.1097/00042752-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects of recurrent concussion in collegiate football players: the NCAA Concussion Study. Journal of the American Medical Association. 2003;290:2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 8.Guskiewicz KM, Weaver NL, Padua DA, et al. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 9.Iverson GL, Gaetz M, Lovell MR, et al. Cumulative effects of concussion in amateur athletes. Brain Injury. 2004;18:433–443. doi: 10.1080/02699050310001617352. [DOI] [PubMed] [Google Scholar]
- 10.Bailes JE, Hudson V. Classification of sport related head trauma: a spectrum of mild to severe injury. J Athl Train. 2001;36:236–423. [PMC free article] [PubMed] [Google Scholar]
- 11.Cantu RC. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36:244–248. [PMC free article] [PubMed] [Google Scholar]
- 12.Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36:228–235. [PMC free article] [PubMed] [Google Scholar]
- 13.Guskiewicz KM, Cantu RC. The concussion puzzle: evaluation of sport-related concussion. American Journal of Sports Medicine. 2004;6:13–21. [Google Scholar]
- 14.Kelly JP. Loss of consciousness: Pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36:249–252. [PMC free article] [PubMed] [Google Scholar]
- 15.Lovell MR, Iverson GL, Collins MW, et al. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9:193–198. doi: 10.1097/00042752-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school athletes. J Neurosurg. 2003;98:296–301. doi: 10.3171/jns.2003.98.2.0296. [DOI] [PubMed] [Google Scholar]
- 17.Lovell MR, Collins MW, Iverson GL, et al. Grade 1 or “ding” concussions in high school athletes. Am J Sports Med. 2004;32:47–54. doi: 10.1177/0363546503260723. [DOI] [PubMed] [Google Scholar]
- 18.McCrory P. What advice should we give to athletes postconcussion? Br J Sports Med. 2002;36:316–318. doi: 10.1136/bjsm.36.5.316. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.McCrory P, Ariens T, Berkovic SF. The nature and duration of acute concussive symptoms in Australian football. Clin J Sport Med. 2000;10:235–238. doi: 10.1097/00042752-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Oliaro S, Anderson S, Hooker D. Management of cerebral concussion in sports: the athletic trainer’s perspective. J Athl Train. 2001;36:257–262. [PMC free article] [PubMed] [Google Scholar]
- 21.Practice parameter: the management of concussion in sports (summary statement) Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 22.Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Med. 2000;19:693–715. doi: 10.1016/s0278-5919(05)70233-7. [DOI] [PubMed] [Google Scholar]
- 23.Kelly KD, Lissel HL, Rowe BH, Vincenten JA, Voaklander DC. Sport and recreation-related head injuries treated in the emergency department. Clin J Sport Med. 2001;11(2):77–81. doi: 10.1097/00042752-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Marchie A, Cusimano MD. Bodychecking and concussions in ice hockey: Should our youth pay the price? Canadian Medical Association Journal. 2003;169:3. [PMC free article] [PubMed] [Google Scholar]
- 25.Honey CR. Brain injury in ice hockey. Clin J Sport Med. 1998;8(1):43–6. doi: 10.1097/00042752-199801000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Goodman D, Gaetz M, Meichenbaum D. Concussions in hockey: There is cause for concern. Med Sci Sports Exer. 2001;33:2004–2009. doi: 10.1097/00005768-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Tegner Y, Lorentzon R. Concussion among Swedish elite ice hockey players. Br J Sports Med. 1996;30:251–255. doi: 10.1136/bjsm.30.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCrea M, Kelly JP, Randolph C, Cisler R, Berger L. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50:1032–1040. doi: 10.1097/00006123-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 29.Fick DS. Management of concussion in collision sports. Guidelines for the sidelines. Postgrad Med. 1995;97(2):53–56. [PubMed] [Google Scholar]
- 30.Annegers JF, Hauser WA, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20–24. doi: 10.1056/NEJM199801013380104. [DOI] [PubMed] [Google Scholar]
- 31.Williamson IJS, Goodman D. Converging evidence for the under-reporting of concussions in youth ice hockey. British Journal of Sports Medicine. 2006;40:128–132. doi: 10.1136/bjsm.2005.021832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erlanger D, Saliba E, Barth JT, et al. Monitoring resolution of postconcussion symptoms in athletes: preliminary results of a web-based neuropsychological test protocol. J Athl Train. 2001;36:280–287. [PMC free article] [PubMed] [Google Scholar]
- 33.McCrea M, Guskiewicz KM, Barr W, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 34.Barr WB, McCrea M. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J Int Neuropsychol Soc. 2001;7:693–702. doi: 10.1017/s1355617701766052. [DOI] [PubMed] [Google Scholar]
- 35.Bleiberg J, Cernich AN, Cameron K, et al. Duration of cognitive impairment after sports concussion. Neurosurgery. 2004;54:1073–1080. doi: 10.1227/01.neu.0000118820.33396.6a. [DOI] [PubMed] [Google Scholar]
- 36.Collie A, Darby D, Maruff P. Computerized cognitive assessment of athletes with sports related head injury. Br J Sports Med. 2001;35:297–302. doi: 10.1136/bjsm.35.5.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Collie A, Maruff P, Makdissi M, et al. CogSport: reliability and correlation with conventional cognitive tests used in postconcussion medical evaluations. Clin J Sport Med. 2003;13:28–32. doi: 10.1097/00042752-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Collins MW, Field M, Lovell MR, et al. Relationship between postconcussion headache and neuropsychological test performance in high school athletes. Am J Sports Med. 2003;31:168–173. doi: 10.1177/03635465030310020301. [DOI] [PubMed] [Google Scholar]
- 39.Collins MW, Grinder SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282:964–970. doi: 10.1001/jama.282.10.964. [DOI] [PubMed] [Google Scholar]
- 40.Collins MW, Lovell MR, Iverson GL, et al. Cumulative effects of concussion in high school athletes. Neurosurgery. 2002;51:1175–1181. doi: 10.1097/00006123-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 41.Daniel JC, Olesniewicz MH, Reeves DL, et al. Repeated measures of cognitive processing efficiency in adolescent athletes: implications for monitoring recovery from concussion. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12:167–169. [PubMed] [Google Scholar]
- 42.Echemendia R, Putukian M, Mackin RS, et al. Neuropsychological test performance prior to and following sports-related mild traumatic brain injury. Clin J Sport Med. 2001;11:23–31. doi: 10.1097/00042752-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Makdissi M, Collie A, Maruff P, et al. Computerized cognitive assessment of concussed Australian Rules footballers. Br J Sports Med. 2001;35:354–360. doi: 10.1136/bjsm.35.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCrea M. Standardized mental status assessment of sports concussion. Clin J Sport Med. 2001;11:176–181. doi: 10.1097/00042752-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 45.McCrea M. Standardized mental status testing on the sideline after sport-related concussion. J Athl Train. 2001;36:274–279. [PMC free article] [PubMed] [Google Scholar]
- 46.Pottinger L, Cullum M, Stallings RL. Cognitive recovery following concussion in high school athletes. Arch Clin Neuropsychol. 1999;14:39–40. [Google Scholar]
- 47.Valovich-McLeod TC, Schwartz C, Bay RC. Sport-related concussion misunderstandings among youth coaches. Clin J Sport Med. 2007 Mar;17(2):140–142. doi: 10.1097/JSM.0b013e31803212ae. [DOI] [PubMed] [Google Scholar]
- 48.Willer B, Kroetsch B, Darling S, Hutson A, Leddy J. Injury Rates in House League, Select, and Representative Youth Ice Hockey. Medicine & Science in Sports & Exercise. 2005 Oct;37(10):1658–1663. doi: 10.1249/01.mss.0000181839.86170.06. [DOI] [PubMed] [Google Scholar]
- 49.Emery CA, Meeuwisse WH. Injury rates, risk factors, and mechanisms of injury in minor hockey. American Journal of Sports Medicine. 2006 Dec;34(12):1960–1969. doi: 10.1177/0363546506290061. [DOI] [PubMed] [Google Scholar]
- 50.Johnston K, McCrory P, Mohtadi N, et al. Evidence-based review of sports-related concussion: clinical science. Clin J Sports Med. 2001;11:150–159. doi: 10.1097/00042752-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Lundin A, de Boussard C, Edman G, Borg J. Symptoms and disability until 3 months after mild TBI. Brain Injury. 2006 Jul;20(8):799–806. doi: 10.1080/02699050600744327. [DOI] [PubMed] [Google Scholar]
- 52.Wang Y, Chan RC, Deng Y. Examination of postconcussion-like symptoms in healthy university students: relationships to subjective and objective neuropsychological function performance. Archives of Clinical Neuropsychology. 2006 May;21(4):339–347. doi: 10.1016/j.acn.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Korinthenberg R, Schreck J, Weser J, Lehmkuhl G. Post-traumatic syndrome after minor head injury cannot be predicted by neurological investigations. Brain & Development. 2004 Mar;26(2):113–117. doi: 10.1016/S0387-7604(03)00110-4. [DOI] [PubMed] [Google Scholar]
- 54.Chan RC. Base rate of post-concussion symptoms among normal people and its neuropsychological correlates. Clinical Rehabilitation. 2001 Jun;15(3):266–273. doi: 10.1191/026921501675253420. [DOI] [PubMed] [Google Scholar]
- 55.Iverson GL, McCracken LM. ‘Postconcussive’ symptoms in persons with chronic pain. Brain Injury. 1997 Nov;11(11):783–790. doi: 10.1080/026990597122990. [DOI] [PubMed] [Google Scholar]
- 56.Kaufman Y, Tzischinsky O, Epstein R, Etzioni A, Lavie P, Pillar G. Long term sleep disturbances after minor head injury. Pediatric Neurology. 2001 Feb;24(2):129–134. doi: 10.1016/s0887-8994(00)00254-x. [DOI] [PubMed] [Google Scholar]
- 57.Potter S, Leigh E, Wade D, Fleminger S. The Rivermead Post Concussion Symptoms Questionnaire: a confirmatory factor analysis. Journal of Neurology. 2006 Dec;253(12):1603–1614. doi: 10.1007/s00415-006-0275-z. [DOI] [PubMed] [Google Scholar]
- 58.Yang CC, Tu YK, Hua MS, Huang SJ. The association between the postconcussion symptoms and clinical outcomes for patients with mild traumatic brain injury. Journal of Trauma. 2007 Mar;62(3):657–663. doi: 10.1097/01.ta.0000203577.68764.b8. [DOI] [PubMed] [Google Scholar]
- 59.Chen JK, Johnston KM, Collie A, McCrory P, Ptito A.A validation of the post concussion symptom scale in the assessment of complex concussion using cognitive testing and functional MRI J Neurol Neurosurg Psychiatry 2007March19; Epub ahead of print:1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goldberg LD, Dimeff RJ. Sideline management of sport-related concussions. Sports Medicine and Arthroscopy Review. 2006 Dec;14(4):199–205. doi: 10.1097/01.jsa.0000212326.23560.09. [DOI] [PubMed] [Google Scholar]
- 61.Whiteside JW. Management of head and neck injuries by the sideline physician. American Family Physician. 2006 Oct;74(8):1357–1362. [PubMed] [Google Scholar]
- 62.Peterson CL, Ferrara MS, Mrazik M, Piland S, Elliot R. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clinical Journal Sports Medicine. 2003 Jul;13(4):230–237. doi: 10.1097/00042752-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 63.Young CG, Jacobs BA, Clavette K, et al. Serial sevens: not the most effective test of mental status in high school athletes. Clin J Sports Medicine. 1997;7:196–198. [PubMed] [Google Scholar]
- 64.Grindel SH, Lovell MR, Collins MW. The assessment of sport-related concussion: The evidence behind neuropsychological testing and management. Clinical Journal of Sports Medicine. 2001;11(3):134–143. doi: 10.1097/00042752-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 65.Ryan LM, Warden DL. Post concussion syndrome. International Review of Psychiatry. 2003 Nov;15(4):310–316. doi: 10.1080/09540260310001606692. [DOI] [PubMed] [Google Scholar]
- 66.McAllister TW, Arciniegas D. Evaluation and treatment of postconcussive symptoms. Neurorehabilitation. 2002;17(4):265–283. [PubMed] [Google Scholar]
- 67.Bohnen N, Twijnstra A, Jolles J. Post-traumatic and emotional symptoms in different subgroups of patients with mild head injury. Brain Injury. 1992 Nov–Dec;6(6):481–487. doi: 10.3109/02699059209008145. [DOI] [PubMed] [Google Scholar]