Abstract
Objective:
The objective of this study was to review the physical examination tests available to a practitioner in order to arrive at a clinical diagnosis or suspicion of a meniscal lesion.
Background:
The menisci transmit weight bearing forces and increase stability of the knee. The menisci also facilitate nutrition, provide lubrication and shock absorption for the articular cartilage and promote knee proprioception. The combinations of torsional and axial loading appear to be the cause of most meniscal injuries. Diagnosis of acute knee injuries has long been a topic for discussion throughout the orthopedic literature. Many clinical tests and diagnostic studies have been developed to increase the clinician’s ability to accurately diagnose these types of disorders of the knee.
Conclusion:
The accuracy of all diagnostic tests is thought to be dependant upon the skill of the examiner, and the severity and location of the injury. The multitude of tests described to assess meniscal lesions suggests that none are consistently reliable. However, recent research has focused on a composite score to accurately predict meniscus lesions. The combination of a comprehensive history, multiple physical tests and diagnostic imaging for confirmation is typical for a clinical meniscal lesion diagnosis while the gold standard remains the arthroscopic procedure itself.
Keywords: knee, meniscus, tests, orthopedic
Abstract
Objectif :
L’objectif de cette étude était de passer en revue les examens physiques que peut faire passer un praticien pour en arriver à un diagnostic clinique ou un soupçon de lésion méniscale.
Contexte :
Le ménisque transmet les forces de charge et accroît la stabilité du genou. Le ménisque facilite également la nutrition et fournit de la lubrification et une absorption des chocs pour le cartilage articulaire, en plus de promouvoir la proprioception du genou. Les combinaisons de charge de torsion et axiale semblent être la cause de la plupart des blessures méniscales. Le diagnostic d’une blessure aiguë au genou est depuis longtemps un sujet de discussion dans la littérature orthopédique. Bon nombre de tests cliniques et d’études diagnostiques ont été créés pour accroître la capacité d’un clinicien à diagnostiquer avec exactitude ces types de troubles du genou.
Conclusion :
On croit que l’exactitude des tests diagnostiques dépend de l’aptitude de l’examinateur, ainsi que de la gravité et l’endroit de la blessure. La multitude de tests décrits pour évaluer les lésions méniscales suggère qu’il n’en existe pas qui soit fiable de façon constante. Cependant, la recherche récente a mis l’accent sur un résultat combiné pour prédire avec exactitude les lésions méniscales. La combinaison d’antécédents détaillés, de nombreux tests physiques et d’imagerie diagnostique aux fins de confirmation est typique pour le diagnostic clinique d’une lésion méniscale, bien que la norme d’excellence reste la technique arthroscopique.
Anatomy
The tibio-femoral, or knee joint is the largest articulation in the body. It is a double condyloid joint with 20° of freedom of motion.1 The condyles of the femur rest in an incongruent manner on the shallow convex surface of the tibia, thus the knee joint relies on other structures to provide both static and dynamic stability.1 This stability is accomplished by the various soft tissue structures: the anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, the menisci, the capsule and the muscles crossing the joint.1–4
Historically, the medial and lateral cartilages (menisci) of the knee were thought to be vestigial structures that had no real significance with regard to dynamic knee function.5 However, orthopedic literature clearly shows that the medial and lateral menisci serve very important roles in knee stability, function and dynamic loading and are thus important in maintaining proper joint health.1–9
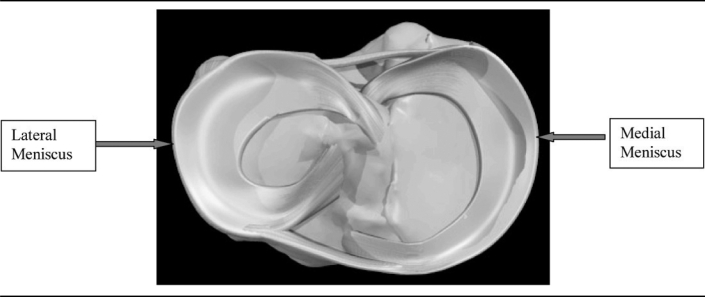
The medial and lateral menisci although similar in function have subtle differences in their shape and thus their biomechanical role in the knee. The knee joint menisci are a pair of wedge shaped (in cross-section), semilunar fibro-cartilage structures that are attached to the tibial plateau along the periphery via the coronary ligaments and to the femur via the ligaments of Humphrey and Wrisberg.10 In addition, the menisci are attached to the patella via the patellomeniscal ligaments which are thickenings of the anterior joint capsule.3,11 When viewed from above the medial meniscus appears ‘C’ shaped while the lateral meniscus appears more ‘O’ shaped3 (see the shape in Figure 1) The surface of each meniscus is concave superiorly, providing a congruous surface to the femoral condyles and is flat inferiorly to accompany the relatively flat tibial plateau.3,10 (see the contact depicted in Figure 2)
Figure 1.
The superior tibial plateau with the menisci (courtesy Primal Pictures Ltd. www.primalpictures.com)
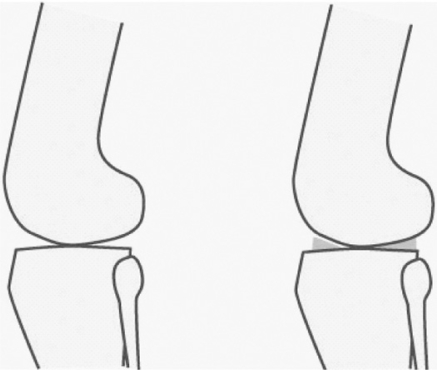
Figure 2.
Contact area between the convex articulating surface of the femur and the flat tibial plateau is increased by the menisci
The medial meniscus is much less mobile during joint motion than the lateral meniscus owing in large part to its firm attachment to the knee joint capsule and medial collateral ligament (MCL).3 On the lateral side the meniscus is less firmly attached to the joint capsule and has no attachment to the lateral collateral ligament. In fact, the posterior horn of the lateral meniscus is separated entirely from the posterolateral aspect of the joint capsule by the tendon of the popliteus muscle as it descends from the lateral epicondyle of the femur.3
The menisci are made of type 1 collagen.5 Gray (1999) has shown that the menisci are collagenous structures, however the different regions of each meniscus have different cell types. The predominant cell in the inner third are chondrocytic in nature and termed fibrochondrocytes.7,12 In the middle third the primary cell is fibrocytic and in the outer third of the meniscus the cells are fibroblastic (active fibrocytes).7 The different cell type in the outer periphery of the meniscus as compared to the central portion of the meniscus helps explain some of the healing properties of the different regions.13 Bullough et al (1970) demonstrated that the majority of the collagen was arranged in a circumferential orientation which provides “hoop stress” and allows the menisci to elongate as the femur places axial and torsional loads upon the knee joint. Interspersed among the longitudinal fibers are radially oriented fibers that act as “tie rods” to provide additional structural rigidity.14
The menisci are supplied mainly by the superior and inferior medial and lateral geniculate arteries which form a peripheral plexus within the synovial and capsular tissues of the knee.6,13 Nourishment to the outer third of the menisci is provided by small branching capillaries from this genicular plexus that penetrate the knee capsule.6 Anorczky and Warren (1983) have shown that only the peripheral 10–30% of the meniscus or what has been termed the “red zone” receives this blood supply. In the middle third or the “red/white zone” the blood supply is very limited and in the “white zone” or inner third of the meniscus there is no active blood supply with a reliance on diffusion and circulation of the synovial fluid for nourishment.13 (see the zones of the meniscus in Figure 3) The tenuous blood supply of the inner regions of the menisci is one of, if not the main detrimental factor in the poor healing properties of the meniscus.2–7,9,13–16
Figure 3.
Showing the red zone (dark grey box), red/white zone (light grey box) and white zone (white box), which represents the blood supply to the meniscus (courtesy Primal Pictures Ltd. www.primalpictures.com)
Biomechanical studies demonstrate that in extension at least fifty percent of the axial forces are transmitted through the meniscus.1–3,7,12 Conversely in flexion the meniscus transmits eighty-five to ninety percent of axial forces.1,3,7 In addition to transmitting weight bearing forces and increasing stability, the menisci facilitate nutrition, provide lubrication and shock absorption for the articular cartilage and promote knee proprioception.1–9
The combination of torsional and axial loading appear to be the cause of most meniscal injuries.2,3,7,17 The anatomical arrangement of the knee’s soft tissue structures ensures that during flexion with the tibia internally rotated, the posterior horn of medial meniscus is pulled in towards the center of the joint.7 This movement can produce a traction injury of the medial meniscus tearing it from its peripheral attachment along the medial joint capsule of the knee.7,18
Meniscal tears are classified by their complexity, plane of rupture, direction, location and overall shape.3 Specifically they may be classified as vertical longitudinal, oblique, horizontal cleavage, radial, and complex.3 The “bucket handle” tear is the most common type of vertical longitudinal tear and generally amenable to repair.3 Anatomy and body mechanics dictate that in isolated injuries to the menisci, the medial meniscus is injured more often than the lateral, and more specifically, the posterior horn more-so than the anterior horn.2,17–19 Seventy-five to ninety percent of all tears sustained during sports such as football, baseball, basketball, and soccer involve the medial meniscus.3
Diagnosis of acute knee injuries has long been a topic for discussion throughout the orthopedic literature. Many clinical tests and diagnostic studies have been developed to increase the clinician’s ability to accurately diagnose disorders of the knee. Torn menisci or ligamentous structures within the knee cause significant pain and disability and thus, require expeditious management.9,17–21 Prompt accurate diagnosis of a meniscus injury is necessary considering the diverse and potentially degenerative consequences of this injury for patients, especially those athletically inclined.17,19
In athletes, isolated meniscus tears typically result from a single traumatic event.17,19 Effusion is usually minimal and develops over a twenty-four to forty-eight hour period after the inciting injury.2,3,6–9,17–21 The occurrence of subsequent swelling secondary to haemarthrosis is approximately twenty percent in a peripheral (vascular) meniscus tear.8,17,19 The acute meniscus tear is often associated with an immediate limited range of motion especially in flexion.20,22,24
The presence of chronic recurrent pain and swelling after exercise is also indicative of a meniscal tear irritating the joint.3,8,21 Other common symptoms of a meniscus tear include locking, catching, buckling and joint line pain along either the medial or lateral joint line corresponding to the site of injury.3,6,8,9,17–21 A history of degenerative joint disease or anterior cruciate ligament injury both in the acute setting or with a chronic ACL deficiency, also predisposes one to a meniscus tear.3
Important historical questions should include the location of pain, duration of pain, a change in activities, trauma, an acute noise or an audible “pop,” swelling surrounding the knee joint, a feeling of give way weakness or buckling, locking or catching of the tibiofemoral articulation, and possibly associated hip, back or thigh pain.3,8,9,19,21 Concomitant or differential diagnosis’ to be considered include degenerative joint disease of the knee, osteochondral defect, cruciate/collateral ligament injury, patellar dislocation, plica, capsular lesion, muscle strain. Of course the practitioner must also rule out the possibility of a vascular injury which carries the risk of more serious sequelae.
A specific history and physical examination should give the clinician clues toward the diagnosis of a lesion of either meniscus. Although the location of pain will be similar it should also be noted that degenerative meniscal tears may present spontaneously without trauma or apparent mechanism. Clinically, the orthopedic literature abounds with several descriptions of physical examination procedures and diagnostic tests to specifically assess the integrity of the menisci, such as joint line tenderness (JLT),24 Apley compression test,23 Anderson medial-lateral grind test,25 McMurray’s test,26 Bounce home maneuver24 and newer tests such as the Axially loaded pivot shift test,10 KKU knee compression rotation test27, Ege’s test22 and Thessaly test.28 Therefore, we reviewed the medical literature to summarize the available evidence about the diagnostic accuracy of the diagnostic procedures for assessing meniscal lesions of the knee. We conducted a literature search of MEDLINE (1966–2007) to identify articles written in English. The Medical Subject Headings (MeSH) terms “knee,” “knee injury” and “meniscus” were combined with the terms “physical examination,” “diagnosis,” “clinical examination,” “sensitivity,” “specificity,” “accuracy,” and “screening.” In addition the cited references of relevant publications were examined to indentify articles not found on the initial searches. Articles comparing physical examination procedures to the findings of magnetic resonance imaging (MRI) were excluded.
The Tests
Palpation of the medial and lateral joint lines is the most basic procedure of the meniscal assessment.24 Flexing the knee and adding tibial rotation either internally or externally allows for easier palpation of the periphery of the medial and lateral meniscus respectively.24 Muellner et al (1997) have stated that the most important finding in patients with a meniscal tear is localized tenderness along the joint line. It is estimated that sixty to eight percent of patients with meniscal lesions will have a joint line that is painful upon palpation.24 Palpation of the joint line is induced through digital pressure by the practitioner into the “red zone” of the meniscus. (refer to the “red zone” depicted in Figure 3)
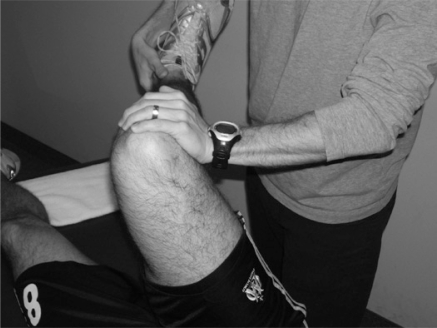
The Apley compression test was originally described by Apley in 1947. Since then the test has been known as “Apley’s test.” In his article he described the procedure of the test as follows: For this examination the patient lies on his face. To start the examination, the surgeon grasps one foot in each hand, externally rotates as far as possible, and then flexes both knees together to their limit. When this limit is reached, he changes his grasp, rotates the feet inward and extends the knees together again. The surgeon then applies his left knee to the back of the patient’s thigh. It is important to observe that in this position his weight fixes 1 of the levers absolutely. The foot is grasped in both hands, the knee is bent to a right angle and the powerful external rotation is applied. This test determines whether simple rotation produces pain. Next, without changing the position of the hands, the patient’s leg is strongly pulled upward, while the surgeon’s weight prevents the femur from rising off the table. In this position of distraction the external rotation is repeated. Two things can be determined 1) whether or not the maneuver produces pain and 2) still more important, whether the pain is greater than in rotation alone without the distraction. If the pain is greater, the distraction test is positive and a rotation sprain may be diagnosed. Then the surgeon leans well over the patient and with his whole body weight compresses the tibia downward onto the table. Again he rotates powerfully, and if addition of compression had produced an increase in pain, this grinding test is positive and meniscal damage is diagnosed.23 (refer to the compression and rotation as shown in Figure 4)
Figure 4.
Apley’s Test
The Anderson medial-lateral grind test was originally described by Anderson and published by Anderson and Lipscomb in 1986.25 The test is performed with the patient supine. The examiner cradles the test leg between the trunk and the arm while the index finger and thumb of the opposite hand are placed over the anterior joint line. A valgus stress is applied to the knee as it is passively flexed to 45°; then a varus stress is applied to the knee as it is passively extended, producing a circular motion to the knee. The motion is repeated, increasing the varus and valgus stresses with each rotation of the knee.25 (refer to the flexion and valgus stress shown in Figure 5)
Figure 5.
Anderson Grind Test
The McMurray or “McMurray’s” test is arguably the most commonly used test to diagnose tears of the meniscus.24 The test was first described in 1940 by McMurray.26 He described the test as follows: In carrying out the manipulation with the patient lying flat, the knee is first fully flexed until the heel approaches the buttock; the foot is then held by grasping the heel and using the forearm as a lever. The knee being now steadied by the surgeon’s other hand, the leg is rotated on the thigh with the knee still in full flexion. During this movement the posterior section of the cartilage is rotated with the head of the tibia, and if the whole cartilage, or any fragment of the posterior section is loose, this movement produces an appreciable snap in the joint. By external rotation of the leg the internal cartilage is tested, and by internal rotation any abnormality of the posterior part of the external cartilage can be appreciated. By altering the position of flexion of the joint the whole of the posterior segment of the cartilages can be examined from the middle to their posterior attachment. Probably the simplest routine is to bring the leg from its position of acute flexion to a right angle, whilst the foot is retained first in full internal, and then in full external rotation. When the click occurs with a normal but lax cartilage, the patient experiences no pain or discomfort, but when produced by a torn cartilage which has already given trouble, the patient is able to state that the sensation is the same as he experienced when the knee gave way previously.26 (refer to the valgus stress and rotation shown in Figure 6)
Figure 6.
McMurray’s Test
The Bounce home test evaluates for a possible limitation in the ability of the knee to fully extend.24 A lack of full knee extension may signify a torn meniscus fragment, an other intra-articular pathology such as a loose body or joint effusion, or a displaced bucket handle tear that requires immediate orthopedic consultation.24 The test is performed with the patient lying supine and the examiner holding the heel of the foot in his hand. After passively flexing the knee, the knee is then allowed to passively extend. The knee should fully extend and “bounce home” with a sharp endfeel.29 If full extension of the joint is not complete or has a rubbery end feel, there is probably a torn meniscus or some other blockage present.29 There have been two modifications of the bounce home test described in the literature. Oni described a modification in which the knee is forcibly extended in a quick jerk.30 He so named this modification the knee jerk test.30 With this test pain will occur in the area of tissue injury. In addition, Shybut and McGinty described a modification of simply forced hyperextension of the knee. A blocking of forced extension indicates a positive test and could be the result of a tear of the meniscus.31 (refer to the hyperextension shown in Figure 7)
Figure 7.
Bounce Home Test
Recently four newer diagnostic tests have been published in the sports medicine literature.10,22,27,28 The Axially loaded pivot shift test as described by Kurosaka et al (1999), is a modification of the pivot shift maneuver as described by MacIntosh, which is used for the diagnosis of ACL ruptures.10 For this test the patient lies supine with the knee in full extension. The examiner applies a valgus force to the proximal tibia in full internal rotation. Next, an axial load is transmitted through the tibia and the knee is brought into 30–45° of flexion. The maneuver is repeated whilst returning the knee to full extension again with axial compression.10 The test is regarded as positive when the patient feels specific pain along the joint line or a click is appreciated by the examiner.10 (refer to the valgus stress with an internally rotating leg shown in Figure 8)
Figure 8.
Axially Loaded Pivot Shift Test
The knee compression rotation test was developed by Sarachai et al (2007). To carry out this test the patient lies supine on the examining table. The knee is passively flexed by grasping the patient’s ankle, with the other hand positioned over the joint line. Knee compression is created by pushing the tibia onto the femur, then the tibia is rotated on the femur both internally and externally. This maneuver is repeated at 120°, 90°, 60°, 30°, and 0°.26 A positive test is indicated when the patient experiences joint line pain, or the examiner appreciates a click or grinding along either the medial or lateral joint line.27 (refer to the compression and rotation shown in Figure 9)
Figure 9.
Knee Compression Rotation Test
Ege’s test as described by Akseki et al (2005), is performed with the patient standing with the knees in extension and the feet held 40 cm apart. To detect a medial meniscus tear, the patient squats with both lower legs in maximal external rotation and stands up slowly.22 For lateral meniscal tears both lower extremities are held in maximum internal rotation while the patient squats and returns to standing.22 The test is positive when pain and/or a click is felt by the patient or is audible to the examiner.22 (refer to the squat with rotation as shown in Figures 10 a,b)
Figure 10a.
Ege’s Test (Internal Rotation)
Figure 10b.
Ege’s Test (External Rotation)
The Thessaly test is also a weight bearing test. It was originally described by Karachalios et al (2005). It attempts to reproduce dynamic load transmission in the knee joint. The examiner supports the patient by holding his outstretched hands. The patient then rotates his knee and body both internally and externally three times keeping the knee in slight flexion at 5°.28 The same testing procedure is then repeated with the patient maintaining the knee in more flexion at 20°.28 A positive test results in joint line discomfort or locking or catching.28 (refer to the slightly flexed knee with rotation as shown in Figures 11 a,b)
Figure 11a.
Thessaly Test (Internal Rotation)
Figure 11b.
Thessaly Test (External Rotation)
The diagnostic accuracy of these tests has often been questioned, and a review of the available sports medicine and orthopedic literature reveals conflicting results in regards to their purported usefulness.24,32,33
With newer surgical advancements, arthroscopy has become the gold standard for the accurate diagnosis of internal derangements of the knee including cruciate ligament tears, tears of the menisci, cartilage defects and other less common causes of significant intra-articular knee pain.33 It is commonplace in the literature investigating diagnostic methods in the physical examination of the knee to compare the findings of the physical examination to the findings at arthroscopy. Thus, in the proceeding discussion all of the reported sensitivities, specificities, and predictive values are in comparison to the findings of arthroscopy which as the gold standard is deemed to have a 100% sensitivity and specificity.
The Value of the Tests
McMurray’s Test
Originally described in 1940, McMurray’s test has been the subject of much debate and is still considered the primary test for the examination of the knee menisci.9 Anderson and Lipscomb investigated 100 meniscus tears and found that McMurray’s test was positive in 58% thus establishing its diagnostic accuracy. Fowler and Lubliner (1989) conducted a prospective study of 161 consecutive patients to evaluate the predictive value of five common clinical tests for meniscus tear. All patients were suspected of having a meniscal tear with or without concomitant ligament pathology.34 A positive McMurray had a high correlation with meniscal tear with a specificity of 95%.34 Evans et al.(1993) evaluated 104 consecutive patients for the accuracy of the McMurray test for the diagnosis of meniscal tear and also looked at the inter-examiner reliability in performing the test. Patients with suspected anterior or posterior cruciate ligament tears were excluded.35 The authors found that for inter-examiner reliability only a “thud” on the medial joint line with associated tibial external rotation was significantly associated with a medial meniscus tear.35 The sensitivity of the medial thud was 16% and the specificity was 98% with a positive predictive value of 83%.35 The sensation of pain on the medial joint line was not correlated with a tear of the medial meniscus.35 Interestingly, Evans et al (1993) found that for the diagnosis of lateral meniscus tears McMurray’s test was less than accurate. They found that lateral joint line pain with internal rotation as originally described by McMurray26 had a poor correlation with lateral meniscus tears, with a positive predictive value of only 29%.35 Sensitivity and specificity calculations for McMurray’s test in diagnosing lateral meniscus tears were not performed. Corea et al. (1994) also compared the McMurray test to surgical findings, using 93 patients with a suspected meniscus injury. He found a sensitivity of 59%, a specificity of 93%, and a positive prediction value of 83%.36 On the basis of low sensitivity they considered the McMurray test to be of limited value in clinical diagnosis.36 Kurosaka et al (1999) evaluated a battery of tests in their cohort of 160 knees, including McMurray’s test. They found that none of the tests used had a diagnostic accuracy over 75%, and that for all the tests used the sensitivity was lower than the specificity indicating that only a small percentage of patients with meniscus lesions exhibited a positive sign on physical examination.10 For McMurray’s test the authors found an overall sensitivity of 37%, a specificity of 77% and a diagnostic accuracy of 45%.10 Akseki et al (2005) compared the results of their new diagnostic test, Ege’s test to the results of McMurray’s test and JLT. They found that all three tests were well correlated to the arthroscopic findings.22 Specifically, McMurray’s test had a kappa score of 0.321 indicating a fair agreement between a positive test and surgical findings.22 The authors stratified their results into medial and lateral tears as diagnosed by each specific test.22 For McMurray’s test they established a sensitivity of 67%, a specificity of 69%, a diagnostic accuracy of 69%, a positive predictive value of 80% and a negative predictive value of 53% for lesions of the medial meniscus.22 They also ascertained a sensitivity of 53%, a specificity of 88%, a diagnostic accuracy of 82%, a positive predictive value of 59% and a negative predictive value of 88% for tears of the lateral meniscus.22 Karachalios et al (2005) also stratified their calculations into tears of either the medial or lateral meniscus. For McMurray’s test they found a sensitivity of 48%, a specificity of 94% and a diagnostic accuracy of 78% for injuries of the medial meniscus.28 For lesions of the lateral meniscus the authors found a sensitivity of 65%, a specificity of 86% and a diagnostic accuracy of 84%.28 The authors also examined McMurray’s test in patients with a combined ACL injury and a meniscus injury. With combined injuries McMurray’s test had a sensitivity of 45%, a specificity of 76% and a diagnostic accuracy of 74%.28 Recently, Surachai et al (2007) examined McMurray’s test and found an overall sensitivity of 70%, a specificity of 82%, a diagnostic accuracy of 73%, a positive predictive value of 92% and a negative predictive value of 48%.27 In their investigation Surachai et al (2007) found higher percentages for McMurray’s test when used in the diagnosis of medial meniscus tears as compared to lateral lesions.27 In their study of the composite knee examination, which included a battery of tests, Lowery et al (2006) found a sensitivity of 20%, a specificity of 96% and a positive predictive value of 84% for McMurray’s test. In a meta-analysis Scholten et al (2001) reviewed the available medical literature concerning various tests of the knee examination including the presence of effusion, joint line tenderness, McMurray’s test and Apley’s compression test. They identified eleven studies of substantial quality that investigated McMurray’s test.37 Scholten et al pooled the results of the individual studies deemed high quality and found an overall sensitivity of 48% and a specificity of 86%.37 The authors did find that McMurray’s test was the only physical examination procedure that had a favorable estimated positive predictive value.37 The negative predictive value of all the tests reviewed was poor.37 In another published review, Solomen et al (2001) found that the overall sensitivity of McMurray’s test was 53% and the specificity was 59%. More recently in a rigorous systematic review, Ryzewicz et al (2007) identified five research studies evaluating McMurray’s test. The authors noted that of the articles reviewed there was a large difference in the reported overall diagnostic accuracy of the test. They speculate that this is due to the varying criteria for clinically diagnosing a meniscus tear using McMurray’s test.38 For example, some articles used a palpable or audible thud as a positive test, whereas others used solely the recreation of pain to constitute a positive result. As such, this detection bias plays a role in the differing results between studies. A lower threshold for a positive test will obviously detect more tears, thus improving the sensitivity however this comes at the expense of specificity.38
Joint Line Tenderness
In the most recent investigation evaluating joint line tenderness (JLT), Wadley et al (2007) attempted to determine the positive predictive value of posterior joint line tenderness in diagnosing posterior horn meniscus tears. Seventy-one patients scheduled for arthroscopy of their knees took part in the study. Each one of three examiners blinded to the history or previous examination of the patients assessed each knee for joint line tenderness. Their results indicate a positive predictive value of 60% with 33 of 55 patients with JLT having a posterior meniscus tear.39 The overall sensitivity was 84.6% but the specificity was only 31.2%.39 In 75.8% of the patients, all three examiners found the same point of maximal tenderness. This corresponded to a kappa score of 0.48 suggesting good inter-examiner reliability.39 Rose et al (2006) examined 129 knees with a definite history of knee trauma and associated knee pain. They found that tenderness of the joint line had a higher diagnostic accuracy (93%), sensitivity (95%) and specificity (93%) for lateral meniscus tears as compared to tears of the medial meniscus.32 Similarly, Eren (2003) examined 104 knees with a history of trauma and found that tenderness of the joint line had a higher diagnostic accuracy (96%), sensitivity (89%) and specificity (97%) for the diagnosis of lateral meniscus lesions. In accordance with the results of Rose et al (2006), the rates obtained for tears of the medial meniscus were much lower.40 In both studies, patients with positive findings for cruciate ligament or collateral ligament injuries were excluded from the study. These three investigations are unique in that they are the only studies performed to date evaluating joint line tenderness as the sole physical examination procedure for diagnosing tears of the meniscus. Five other studies10,22,25,28,34 evaluated joint line tenderness in combination with other commonly used physical examination procedures. Anderson and Lipscomb (1986) examined the medial-lateral grind test, McMurray’s test and joint line tenderness in a series of 100 patients with suspected meniscus tears. The authors found that joint line tenderness was 77% accurate for the diagnosis.25 The authors did not report the sensitivity, specificity or positive predictive value. Fowler and Lubliner (1989) examined joint line tenderness tests in a cohort of 165 knees. Of those, 125 had joint line tenderness producing a sensitivity of 85% and a specificity of 29%.34 Akseki et al (2005) compared joint line tenderness to Ege’s test, one of the newer diagnostic procedures. In examining 150 knees they found a higher sensitivity for the diagnosis of medial tears (88% vs. 67%), a higher specificity for the diagnosis of lateral tears (80% vs. 44%) and a higher diagnostic accuracy for lateral tears (77% vs. 71%).22 In examining patients with suspected meniscal pathology with or without an associated ACL rupture and a history of precipitating trauma, Kurosaka et al (1999), calculated a sensitivity of 55% a specificity of 67% and a diagnostic accuracy of 57% for joint line tenderness. Of their cohort 68% had chronic ACL deficiency and acute injuries were excluded in this study.10 Shelbourne et al (1995) evaluated the correlation of joint line tenderness with meniscus tear in patients with acute ACL injuries. One hundred and seventy three patients were evaluated for joint line tenderness, and then the meniscus was inspected during subsequent ACL reconstruction.33 They found that in a knee with an ACL tear, joint line tenderness was neither sensitive nor specific for the presence of an associated meniscal tear.33 Karachalios et al (2005) investigated five physical examination tests and compared the results to magnetic resonance imaging (MRI). For joint line tenderness, they found a sensitivity of 71% and specificity of 87% and an overall diagnostic accuracy of 81% for the medial meniscus.28 For the lateral meniscus they found a sensitivity of 78%, a specificity of 90% and a diagnostic accuracy of 89%.28 With a combined ACL and meniscus lesion they found JLT to be 65% sensitive, 80% specific and had a diagnostic accuracy of 80%.28 The authors found significant heterogeneity of the sensitivity and specificity of all tests except for Apley’s test.28 Lowery et al (2006) documented a sensitivity of 65% and a specificity of 65% for diagnosing meniscus tears using JLT. They also found a positive predictive value of 55%.15 Scholten et al (2001) reviewed nine studies that examined the results of joint line tenderness. The overall sensitivity and specificity for joint line tenderness generated from the pooled analysis of all the available literature was 77% and 41% respectively.37 In addition, the pooled positive predictive value for using joint line tenderness in diagnosing a meniscus lesion was not substantially increased indicating poor additional diagnostic value.37 Solomon et al (2001) in their review found an overall mean sensitivity of 79% and a specificity of 15%. They calculated that the logical regression (LR) for a positive test was 0.9 (95% CI, 0.8–1.0) and for a negative test 1.1 (95% CI, 1.0–1.3).18 Essentially the regression means the probability of an anticipated outcome, with a negative test being more probable. More recently, Ryzewicz et al (2007) performed a systematic review on the diagnosis of meniscus tears. In it they identified four studies of acceptable methodological quality investigating joint line tenderness. Their conclusions are very similar to those of Scholten et al (2001), in that joint line tenderness alone is not sufficient for the diagnosis of tears of the meniscus.38
Bounce Home Test (Forced Hyperextension)
There are currently no research studies investigating the sensitivity, specificity or diagnostic accuracy of the bounce home test as originally described. Fowler and Lubliner (1989) found that pain with forced hyperextension generated a sensitivity of 44% and a specificity of 86% in their cohort of patients. Kurosaka et al (1999) also included the forced hyperextension test as described by Shybut and McGinty31 into their investigation. They found a sensitivity of 47%, a specificity of 67% and a diagnostic accuracy of 51% for the maneuver.10 Lowery et al (2006) found that forced knee hyperextensions generated a sensitivity of 36%, a specificity of 86% and a positive predictive value of 73%. The knee jerk test as described by Oni27 has not been investigated in the literature.
Apley’s Test
Fowler and Lubliner (1989) in their thorough investigation of the clinical examination of the knee meniscus examined the utility of Apley’s test. They reported a sensitivity of 16% and a specificity of 80%.34 More recently Kurosaka et al (1999) reported a sensitivity of 13% and a specificity of 90%. In addition, they reported a diagnostic accuracy of 28%.10 Karachalios et al (2005) also reported on the clinical examination results of Apley’s test with lesions of the medial meniscus determined to have a sensitivity of 41%, a specificity of 93% and a diagnostic accuracy of 75%. Furthermore, for lesions of the lateral meniscus they found a sensitivity of 41%, a specificity of 86% and a diagnostic accuracy of 82%.28 For combined lesions of the ACL and either the medial or lateral meniscus Karachalios et al (2005) attained a sensitivity of 20%, a specificity of 84% and a overall diagnostic accuracy of 59% for Apley’s test. It should be noted that the authors used MRI as the gold standard.
(Anderson’s) Media-Lateral Grind Test
Anderson and Lipscomb (1986) reported on and investigated a manipulative test for the diagnosis of meniscus tears. They compared the results of the medial-lateral grind test to those of McMurray’s test in one hundred patients with a suspected meniscus tear. All patients with a suspected ligament tear of the cruciates or collaterals were excluded.25 There were a total of 100 tears of the meniscus occurring in 93 patients.25 The authors report that the medial-lateral grind test was positive in 68% of the knees examined, thus reporting a diagnostic accuracy of 68%.25 The authors did not report sensitivity and specificity.
Thessaly Test
Karachalios et al (2005) examined the sensitivity, specificity and diagnostic accuracy of this new dynamic weight bearing test. In this investigation subjects were examined clinically with tests of JLT, McMurray’s, Apley’s and the newly described Thessaly test at 5° and 20° of knee flexion.28 Two hundred and thirteen patients with a suspected meniscus injury on the basis of the clinical history and mechanism of injury (Group A) were investigated and compared to a group of 197 volunteers with no injury to the meniscus (Group B).28 All patients underwent an MRI of the knee and those in Group A had further therapeutic arthroscopy.28 The results indicate that for injury to the medial meniscus the Thessaly test at 5° knee flexion is 66% sensitive, 96% specific, and 86% accurate.28 For the lateral meniscus it is 81% sensitive, 91% specific, and 90% accurate.28 The Thessaly test at 20° of knee flexion is 89% sensitive, 97% specific, and 94% accurate for medial lesions and 92% sensitive, 96% specific and 96% accurate for lateral lesions.28 For combined lesions of the ACL and either of the menisci the Thessaly test at 5° of knee flexion was 65% sensitive, 80% specific and had a diagnostic accuracy of 80%.28 The test performed at 20° of knee flexion performed at 80% sensitivity, 91% specificity and had a diagnostic accuracy of 90% for these combined ligament and meniscus injuries.28 It is evident that with an associated ACL tear the test becomes less accurate. Overall this new dynamic test performed better than all other tests evaluated in this study. As a result, the authors recommend the Thessaly test as the preferred first line test for the diagnosis of meniscus tears.28
Ege’s Test
Akseki et al (2005) compared the value of this new weight bearing diagnostic test with the two other most commonly used tests: JLT and McMurray’s test. Of 150 knees in 150 patients, 89 reported a specific history of trauma.22 All patients had a radiographic examination and underwent arthroscopic surgery.22 There were no statistically significant differences between the three tests in detecting a meniscus tear, however there were evident differences in terms of the sensitivity, specificity, and diagnostic accuracy. Ege’s test had a sensitivity of 67%, a specificity of 81% and a diagnostic accuracy of 71% for tears of the medial meniscus.22 For the lateral meniscus Ege’s test had a sensitivity of 64%, a specificity of 90% and a diagnostic accuracy of 84%.22 Also, Ege’s test had the highest overall positive predictive value for medial meniscus tears (86%).22 Overall, the accuracy of Ege’s test was equal to that of JLT and was superior to McMurray’s test. It was also the most specific test for both medial and lateral meniscus tears. The authors concluded that by using Ege’s test they were able to diagnose meniscal lesions as accurately as JLT but with an increased specificity and thus, Ege’s test should be incorporated into routine knee examination.22
KKU Knee Compression Rotation Test
Surachai et al (2007) compared the sensitivity, specificity, and diagnostic accuracy of this new test with McMurray’s test. Sixty-eight patients with suspected meniscus injury and who were scheduled for arthroscopy were examined using the KKU knee compression rotation test and McMurray’s test.27 KKU knee compression rotation test was positive in 46 of 51 torn menisci, while McMurray’s was positive in 39 of 51 torn menisci.27 This generated an 86% sensitivity, 88% specificity and 87% diagnostic accuracy for the KKU knee compression rotation test, which was far superior to the results of McMurray’s test.27 In 35 cases of meniscus lesions both tests were positive. This had a bearing on the sensitivity, increasing it to 90% when both tests were positive, however the specificity and diagnostic accuracy were not significantly affected by the addition of a positive McMurray test.27
Axially Loaded Pivot Shift Test
Kurosaka et al (1999) assessed the significance of the Axially loaded pivot shift test in the diagnosis of chronic meniscus lesions. One hundred and sixty knees were examined using this test as well as McMurray’s test, Apley’s test, JLT and pain on forced extension.10 All patients had knee symptoms for at least 8 weeks and were examined for isolated tears of the meniscus or with an associated ACL rupture.10 The results indicate that 68% percent of the knees examined had a chronic ACL deficiency and that there were 144 meniscus tears evident at arthroscopy.10 On the clinical examination the Axially loaded pivot shift test had the highest sensitivity (71%) compared to all other tests.10 The test also showed high specificity (83%) and had a significantly higher diagnostic accuracy than the other tests used.10 Incidentally only 13 knees exhibited a click with this test, with the majority of patients examined experiencing pain with a positive result. This was more apparent in those with chronic ACL deficiency.10
Composite Score
Often the diagnosis of a meniscus tear is a difficult one to make even for the experienced clinician. This is because a variety of signs and symptoms of lesions of the meniscus have been proposed in the literature. Much like the examination of specific diagnoses in other joints of the body no one test has been shown to be pathognomonic for the diagnosis of a meniscus tear.15 The clinician relies upon an accurate history/mechanism and a variety of physical examination procedures to arrive at a diagnosis of a lesion of the meniscus. It is from the results of these tests that the clinician then formulates a treatment plan. Recently, the literature has begun to explore the accuracy of a set of tests performed at the same time in the generation of a specific diagnosis of a meniscus tear. Referred to as a composite score, it attempts to assess the efficacy of a variety of procedures in detecting pathology. Scholten et al (2001) in their review conclude that the physical examination procedures they analysed (effusion, JLT, McMurray’s test) in isolation do not seem to be very helpful in guiding clinical decision making. They state that combining the results of the various tests might improve the diagnostic accuracy of detecting a meniscus lesion.37 Oberlander et al (1993) investigated the accuracy of the clinical examination for intra-articular knee disorders, including tears of the meniscus. Of 296 knees included in the study the correct diagnosis was made 56% of the time.41 Included, were other intra-capsular knee pathology besides solely meniscus lesions. When only one knee pathology was present the diagnostic accuracy was 72%.41 As the number of pathologies increased the diagnostic accuracy of the knee examination decreased. Specifically, the authors documented a sensitivity of 87%, a specificity of 93% and a diagnostic accuracy of 90% for tears of the medial meniscus.41 For the lateral meniscus the sensitivity was 81%, the specificity was 93% and the diagnostic accuracy was 95%.41 O’ Shea et al (1996) examined 156 knees for various pathology. Using a standardized composite knee exam the authors recognized the correct primary diagnosis in 83% of the knees.29 Of those given a secondary diagnosis (57 knees) the diagnosis was correct at a rate of 54%.29 Sixty-eight knees were diagnosed with medial meniscus tears, 60 of which were correctly diagnosed on physical examination.29 This generated a sensitivity of 88%, a specificity of 77% and a diagnostic accuracy of 82%.29 Of 49 lateral meniscus tears, only 25 were correctly diagnosed preoperatively.29 This produced a sensitivity of 51%, a specificity of 90% and a diagnostic accuracy of 78%.29 Muellner et al (1997) examined a cohort of 93 competitive athletes. Group 1 included 57 patients who also underwent arthroscopic surgery. Group 2 consisted of 36 patients who underwent further MRI. Of those patients in Group 1 the diagnosis of a meniscal lesion was confirmed in 51 of 57 patients.19 Of the 44 medial meniscus lesions all were diagnosed preoperatively.19 Seventeen medial menisci were normal at arthroscopy of which 13 were correctly diagnosed.19 The sensitivity was 100%, the specificity was 76%, the diagnostic accuracy was 93%, the positive predictive value was 91% and the negative predictive value was 100%.19 Of the 13 torn lateral menisci, 12 were correctly identified on examination.19 Forty four lateral menisci were normal, 43 of which were determined on physical examination.19 The sensitivity calculated was 92%, the specificity was 98%, the diagnostic accuracy was 96%, the positive predictive value was 92% and the negative predictive value was 98%.19 Solomon et al (2001) reviewed nine meniscal studies of which five reported the accuracy of the composite examination (averaged the results of several meniscal tests). The mean sensitivity of the composite examination was 77% and the specificity was 91%.37 Recently, Lowery et al (2006) investigated the composite examination for meniscus pathology in a cohort of 635 knees with either acute or chronic injury.15 The examination consisted of McMurray’s test, forced hyperextension, JLT and pain with forced flexion, in addition to a history of mechanical symptoms.15 Two hundred and nine knees then underwent arthroscopic evaluation, while the remainder did not.15 The results indicate that with a history of mechanical symptoms and a positive result on four tests examining the meniscus the sensitivity is 11%, the specificity is 99% and the positive predictive value is 92%.15 Overall, as the number of findings indicative of meniscus pathology increased so did the PPV of finding a lesion of the meniscus. Interestingly the authors found that when concurrent ACL pathology was present, the positive predictive value of the composite examination decreased to 67%.15 Ryzewicz et al (2007) indicated that a composite examination for meniscal injuries performs much better than any individual test used in isolation. This suggests that a synthesis of examination findings used in conjunction with an historical account of the knee injury (mechanism) must be refined for an accurate diagnosis of a meniscus lesion.38
Discussion
The sports medicine and orthopedic literature is full of various articles describing various signs and symptoms as well as diagnostic procedures in an attempt to ensure an accurate diagnosis of a meniscus lesion. Historically, from a physical examination perspective, this has included joint line tenderness, McMurray’s test and Apley’s compression test. Recently, there have been several newly developed physical examination procedures to further address this diagnostic challenge. Our goal was to collect and summarize the available evidence concerning the diagnostic accuracy of both the older and newer diagnostic tests for assessing injuries of the knee meniscus. On the basis of the current review, it is evident that there is a lack of consistency amongst the tests and that the more recent tests have not yet undergone rigorous scientific investigation. The accuracy of these tests seems to be relatively poor suggesting, if used in isolation, there is little evidence to support the notion that an accurate diagnosis of a meniscus lesion can be made through a physical examination, with the current orthopedic tests. Arthroscopy is truly the only gold standard. The recent research has focused on a composite score to accurately predict meniscus lesions and the research in this area is promising as the results more accurately predict the clinical situation of not relying solely on one test. Further, the composite examination can improve the clinician’s ability to diagnose meniscus tears more accurately. This improved diagnostic ability allows the physician to better counsel the patient regarding the possible management options. Unfortunately at this time it has not been well established as to which tests should be included in the composite examination. From our review it seems logical that any meniscus evaluation should include both McMurray’s test as well as joint line tenderness. The Thessaly test, has shown some promise as a good screening procedure, however future research should attempt to further define its diagnostic accuracy.
Conclusion
Future research in the area of diagnosing meniscus tears is warranted. Currently the need for utilizing more advanced diagnostic methods or specialty referral can really only be based on the severity of the patient’s complaints and a high index of suspicion by the practitioner. A composite score in which a practitioner uses a battery of tests to suggest the diagnosis is recommended. Further investigations into the statistical value of all the commonly used tests, which combinations of tests should be used and the importance of combining the physical examination with aspects of history taking is needed before any further evidence based recommendations can be made.
Table 1.
Summary of Ranges for Sensitivity and Specificity of the Tests
| Test | Sensitivity Range | Specificity Range |
|---|---|---|
| McMurray’s | 16–70% | 59–98% |
| Joint Line Tenderness | 55–95% | 15–97% |
| Bounce Home (forced hyperextension) | 36–47% | 67–86% |
| Apley’s | 13–41% | 80–93% |
| Thessaly | 65–92% | 80–97% |
| Ege’s | 64–67% | 81–90% |
| KKU (compression rotation) (1 study) | 86% | 88% |
| Axial Loaded Pivot Shift | 71% | 83% |
| Composite Score | 11–100% | 77–99% |
References
- 1.Levangie P, Norkin C. Joint Structure and Function. FA Davis Company; 2001. [Google Scholar]
- 2.Lee J, Fu F. The meniscus: basic science and clinical applications. Operative Techniques in Orthopaedics. 2000;10:162–168. [Google Scholar]
- 3.Lento P, Akuthota V. Meniscal injuries: a critical review. J Back Musculoskel Rehabil. 2000;15:55–62. doi: 10.3233/bmr-2000-152-302. [DOI] [PubMed] [Google Scholar]
- 4.Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34(4):252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics and rationale for clinical treatment. J Anat. 1998;193:161–178. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gray J. Neural and vascular anatomy of the menisci of the knee. J Ortho Sports Phys Ther. 1999;29:23–30. doi: 10.2519/jospt.1999.29.1.23. [DOI] [PubMed] [Google Scholar]
- 7.Kawamura S, Lotito K, Rodeo S. Biomechanics and healing response of the meniscus. Operative Techniques in Sports Medicine. 2003;11:68–76. [Google Scholar]
- 8.McDermott I. Meniscal tears. Current Orthopaedics. 2006;20:85–94. [Google Scholar]
- 9.Seneviratne A, Rodeo SA. Identifying and managing meniscal injuries. J Musculoskel Med. 2000;17:690–697. [Google Scholar]
- 10.Kurosaka M, Yagi M, Yoshiya S, Muratsu H, Mizuno K. Efficacy of the axially loaded pivot shift test for the diagnosis of a meniscal tear. Intl Orthopaedics. 1999;23:271–274. doi: 10.1007/s002640050369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huffman GB. Reliability of Clinical Examination of a Painful Knee. American Family Physician. 2002 Mar;:1–3. [Google Scholar]
- 12.Verdonk P, Forsyth R, Wang J, Almqvist K, Verdonk R, Veys E, Verbruggen G. Characterisation of human knee meniscus cell phenotype. Osteoarthritis and Cartilage. 2005;13:548–560. doi: 10.1016/j.joca.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Arnorczky S, Warren R. The microvasculature of the meniscus and its response to injury. Am J Sports Med. 1983;11:131–141. doi: 10.1177/036354658301100305. [DOI] [PubMed] [Google Scholar]
- 14.Bullough P, Murphy J, Weinstein A. The strength of the menisci of the knee joint as it relates to their fine structure. J Bone Jt Surg. 1970;52:564–570. [PubMed] [Google Scholar]
- 15.Lowery D, Farley T, Wing D, Sterett W, Steadman R. A clinical composite score accurately detects meniscal pathology. Arthroscopy. 2006;22:1174–1179. doi: 10.1016/j.arthro.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Stratford P, Binkley J. A review of the McMurray test: definition, interpretation and clinical usefulness. J Ortho Sports Phys Ther. 1995;22:116–120. doi: 10.2519/jospt.1995.22.3.116. [DOI] [PubMed] [Google Scholar]
- 17.Muellner T, Weinstable R, Schabus R, Vescei V, Kainberger F. The diagnosis of meniscal tears in athletes. Am J Sports Med. 1997;25(1):7–12. doi: 10.1177/036354659702500103. [DOI] [PubMed] [Google Scholar]
- 18.Solomon H, et al. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001;286(13):1610–1620. doi: 10.1001/jama.286.13.1610. [DOI] [PubMed] [Google Scholar]
- 19.Muellner T, Weinstable R, Schabus R, Vescei V, Kainberger F. Recommendations for the diagnosis of traumatic meniscal injuries in athletes. Sports Medicine. 1999;27(5):337–345. doi: 10.2165/00007256-199927050-00005. [DOI] [PubMed] [Google Scholar]
- 20.Bernstein J. Meniscal tears of the knee. Physician Sports Med. 2000;28(3):1–10. doi: 10.3810/psm.2000.03.778. 28. [DOI] [PubMed] [Google Scholar]
- 21.Swenson EJ. Diagnosing and managing meniscal injuries in athletes. J Musculoskel Med. 1995;12(5):35–45. [Google Scholar]
- 22.Akseki D, Ozcan O, Boya H, Pinar H. A new weight bearing test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy. 2005;20:951–958. doi: 10.1016/j.arthro.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 23.Apley A. The diagnosis of meniscus injuries: some new clinical methods. J Bone Jt Surg (Br) 1947;2:78–84. [PubMed] [Google Scholar]
- 24.Malanga G, Andrus S, Nadler S, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84:592–603. doi: 10.1053/apmr.2003.50026. [DOI] [PubMed] [Google Scholar]
- 25.Anderson A, Lipscomb B. Clinical diagnosis of meniscal tears. Am J Sports Med. 1986;14:291–293. doi: 10.1177/036354658601400408. [DOI] [PubMed] [Google Scholar]
- 26.McMurray T. The semilunar cartilages. Br J Surg. 1942;29:407–414. [Google Scholar]
- 27.Sarachai S, Kitti J, Thanathep B. KKU knee compression rotation test for detection of meniscal tears: a comparative study of its diagnostic accuracy with McMurray test. J Med Assoc Thailand. 2007;40:718–723. [PubMed] [Google Scholar]
- 28.Karachalios T, Hantes M, Zibis A, Zachos V, Karantanas A, Malizos K. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Jt Surg (Am) 2005;87:955–962. doi: 10.2106/JBJS.D.02338. [DOI] [PubMed] [Google Scholar]
- 29.O’Shea KJ, et al. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med. 1996;24(2):164–167. doi: 10.1177/036354659602400208. [DOI] [PubMed] [Google Scholar]
- 30.Oni A. The knee jerk test for diagnosis of torn meniscus (letter) Clinical Orthopedics. 1985;193:309. doi: 10.1097/00003086-198503000-00042. [DOI] [PubMed] [Google Scholar]
- 31.Shybut G, McGinty J. The office evaluation of the knee. Orthopaedic Clinics of North America. 1982;13(3):497–509. [PubMed] [Google Scholar]
- 32.Rose R. The accuracy of joint line tenderness in the diagnosis of meniscal tears. West Indian Med Jl. 2006;55:323–326. doi: 10.1590/s0043-31442006000500006. [DOI] [PubMed] [Google Scholar]
- 33.Shelbourne K, Martini D, McCarroll J, VanMeter C. Correlation of joint line tenderness and meniscal lesions in patients with acute anterior cruciate ligament tears. Am J Sports Med. 1995;23:166–169. doi: 10.1177/036354659502300207. [DOI] [PubMed] [Google Scholar]
- 34.Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Am J Sports Med. 1989;5(3):184–186. doi: 10.1016/0749-8063(89)90168-0. [DOI] [PubMed] [Google Scholar]
- 35.Evans P, Bell D, Frank C. Prospective evaluation of the McMurray test. Am J Sports Med. 1993;21(4):604–608. doi: 10.1177/036354659302100420. [DOI] [PubMed] [Google Scholar]
- 36.Corea J, Moussa M, Othman A. McMurray’s test tested. Knee Surgery Sports Traumatology and Arthroscopy. 1994;2:70–72. doi: 10.1007/BF01476474. [DOI] [PubMed] [Google Scholar]
- 37.Scholten R, Walter L. The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee. a meta-analysis. J Family Practice. 2001;50(11):938–944. [PubMed] [Google Scholar]
- 38.Ryzewicz M, Peterson B, Siparsky P, Bartz R. The diagnosis of meniscal tears. Clinical Ortho Rel Res. 2007;455:123–133. doi: 10.1097/BLO.0b013e31802fb9f3. [DOI] [PubMed] [Google Scholar]
- 39.Wadley V, Mohtadi N, Bray R, Frank C. Positive predictive value of maximal posterior joint-line tenderness in diagnosing meniscal pathology: a pilot study. Canadian J Surg. 2007;50:96–100. [PMC free article] [PubMed] [Google Scholar]
- 40.Eren O. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy. 2003;19:850–854. doi: 10.1016/s0749-8063(03)00736-9. [DOI] [PubMed] [Google Scholar]
- 41.Oberlander M, Shalvoy R, Hughston J. The accuracy of the clinical knee examination documented by arthroscopy: a prospective study. Am J Sports Med. 1993;21:773–778. doi: 10.1177/036354659302100603. [DOI] [PubMed] [Google Scholar]