Abstract
Objectives The Newcastle 85+ Study aims to systematically study the clinical, biological, and psychosocial attributes of an unselected cohort of 85 year olds and to examine subsequent health trajectories as the cohort ages; health at baseline is reported.
Design Cross sectional analysis of baseline data from a cohort study.
Setting Newcastle upon Tyne and North Tyneside primary care trusts, United Kingdom.
Participants 1042 people born in 1921 and registered with the participating general practices.
Main outcome measures Detailed health assessment and review of general practice records (disease, medication, and use of general practice services); participants could decline elements of the protocol.
Results Of the 1453 eligible people, 851 (58.6%) were recruited to health assessment plus record review, 188 (12.9%) to record review only, and 3 (0.2%) to health assessment only. Data from record review are reported on a maximum of 1030 and from health assessment on a maximum of 853; individual denominators differ owing to withdrawal and missing values. Of the health assessment sample (n=853), 62.1% (n=530) were women and 10.4% (n=89) were in institutional care. The most prevalent diseases were hypertension (57.5%, 592/1030) and osteoarthritis (51.8%, 534/1030). Moderate or severe cognitive impairment was present in 11.7% (96/824) of participants, severe or profound urinary incontinence in 21.3% (173/813), hearing impairment in 59.6% (505/848), and visual impairment in 37.2% (309/831). Health assessment identified participants with possible disease but without a previous diagnosis in their medical record for hypertension (25.1%, 206/821), ischaemic heart disease (12.6%, 99/788), depression (6.9%, 53/772), dementia (6.7%, 56/840), and atrial fibrillation (3.8%, 30/788). Undiagnosed diabetes mellitus and thyroid disease were rare (1%, 7/717 and 6/762, respectively). A median of 3 (interquartile range 1-8) activities of daily living were undertaken with difficulty. Overall, 77.6% (646/832) of participants rated their health compared with others of the same age as good, very good, or excellent. High contact rates in the previous year with general practitioners (93.8%, 960/1024) were recorded. Women had significantly higher disease counts (medians: women 5, men 4; P=0.033) and disability scores (medians: women 4, men 2; P=0.0006) than men, but were less likely to have attended outpatient clinics in the previous three months (women 29% (150/524), men 37% (118/320), odds ratio 0.7, 95% confidence interval 0.5 to 0.9).
Conclusions This large cohort of 85 year olds showed good levels of both self rated health and functional ability despite significant levels of disease and impairment. Hypertension, ischaemic heart disease, atrial fibrillation, depression, and dementia may be underdiagnosed. Notable differences were found between the sexes: women outnumbered men and had more disease and disability.
Introduction
The world’s population is ageing. In developed countries in 2000 almost one fifth of the population was aged 60 or more, and by 2050 this is expected to rise to one third. Although the proportion of older people is still low in less developed regions, the pace of population ageing is even more rapid.1 Whereas the notable increase in life expectancy over much of the last two centuries was driven chiefly by declines in mortality in early and middle life, since the 1950s increasing longevity has been dominated by falling age specific death rates among the oldest age groups.2 The oldest old, defined variously as those aged 80 or 85 years or more, are now the fastest growing sector of the population worldwide.1 Many of the oldest old experience disease, disability, and dependency, with high costs of health and social care,3 but detailed data on the spectrum of health in this age group and the individual health trajectories followed in the later years of a long life are lacking. It is unclear whether the decline in disability levels seen in the younger old in certain countries will translate to the oldest old4 and there is little information on factors that maintain health and independence in this age group. Effective service planning requires detailed population health needs assessment.
Although studies provide information on the health of the oldest old in several countries, few comprise single year birth cohorts5 6 7 despite these offering distinct advantages for studying the complexity of the ageing process with its inherent variability. In addition, a review of population based cohort studies of ageing in developed countries8 highlighted the need for new studies to recruit the oldest old at baseline and to include people living in institutions. The oldest old have evaded the risks of mortality associated with specific adverse factors and are therefore particularly likely to be informative about the effects of intrinsic ageing. Within the United Kingdom, previous cohort studies have provided valuable information but are limited by the exclusion of those living in institutions9 10; a lack of detailed coverage of physical, psychological, social, functional, and biological domains9 11; a reliance on self report for data on disease rather than on medical records9 10 11 12; outdated information9 11; and a lack of comprehensive follow-up data.12 Similarly, UK cross sectional studies that include this age group are limited by small numbers,13 exclusion of those living in institutions or who are unable to provide consent,13 and a lack of comprehensive information on health.13 14
The Newcastle 85+ Study aims to determine the full spectrum of health within an inception cohort of 85 year olds, selected without regard to health status, and to examine health trajectories and outcomes as the cohort ages and the association between these outcomes and a complex array of clinical, biological, and psychosocial factors. This paper reports the health status of the cohort at baseline, together with information about undiagnosed disease and use of health services.
Methods
The sampling frame comprised all people born in 1921 who were permanently registered with a participating general practice in Newcastle upon Tyne or North Tyneside primary care trusts in the UK. We approached all 64 general practices in these trusts to participate in the study. The general practitioners were asked to review patient lists before mail-out and to exclude only those with end stage terminal illness and those who might pose a safety risk to a nurse visiting alone. Excepting these exclusions, all those remaining in the sampling frame were sent a letter of invitation by the study team, whether living at home or in an institution and regardless of their state of health. Recruitment and assessment took place over a 17 month period during 2006-7.
Measures
Details of the study protocol have been reported.15 Participation at baseline entailed a detailed multidimensional health assessment, comprising questionnaires, measurements, function tests, a fasting blood sample, and a review of medical records held by the general practice; participants could decline elements of the protocol. Further details of the measures reported in this paper together with the study questionnaires and the proforma used for record review are available in the web extra and on the Newcastle 85+ Study website (www.ncl.ac.uk/iah/research/programmes/85plus.htm).
Procedures
Assessment was carried out in the participant’s usual residence (home or institution) by a research nurse. Participants who were temporarily admitted to hospital at the time of recruitment were assessed after discharge. Information was collected during three interviews, with one further visit to collect a fasting blood sample and to measure body weight. Data were entered directly onto a laptop computer.
A research nurse reviewed the general practice medical records to collect information on diseases, current medication, and use of general practice services. All computerised and paper records were reviewed, including hospital correspondence and the results of investigations. A predetermined list of key diseases was used and all diagnoses of listed diseases were recorded, together with the date of first diagnosis. Medication included any prescribed item—that is, drugs and items such as wound management products, elastic hosiery, catheter and stoma products, and food preparations.
The 11 research nurses underwent training for six weeks in the standardised protocols to be used, with regular updates. Inter-rater reliability for data extraction from general practice records was examined for 24 randomly selected participants across a core set of variables. Intraclass correlations16 for binary variables ranged from 0.45 to 0.79; mean 0.57 (angina 0.6, myocardial infarction 0.45, heart failure 0.45, hypertension 0.57, and stroke 0.79), indicating moderate or better agreement between the nurses. Analysis of inter-rater reliability for ordinal variables including the total number of prescribed medications; number of medications for cardiovascular, central nervous system, and gastrointestinal conditions; number of consultations with a general practitioner or practice nurse; and number of consultations at home and at the general practice, showed the only significant disagreement between the nurses to be in the total number of prescribed medications.
Written informed consent was obtained from participants. Where people lacked capacity to consent—for example, because of dementia—an opinion was sought from a relative or carer (a “consultee”) according to the requirements of the UK Mental Capacity Act.17
Disease prevalence and undiagnosed diseases
For most diseases we determined prevalence on the basis of a review of data from general practice records alone. Exceptions were atrial fibrillation or flutter, renal impairment, and anaemia, which we took from the relevant health assessment data.
We estimated the extent of possible undiagnosed hypertension, ischaemic heart disease, diabetes, hypothyroidism, and hyperthyroidism by taking account of health assessment measures in those without the particular diagnosis recorded in the general practice records. For depression, dementia, and atrial fibrillation we estimated the point prevalence of possible disease from health assessment data and then checked if that particular diagnosis was recorded in the general practice records. We defined the presence of disease from health assessment data by standard cut-off points (see web extra for details of measures and cut-off points used).
Disease count
We derived a simple disease count (maximum score 18) from selected chronic diseases (box 1). Only participants in whom all variables were scored as present (score 1) or absent (score 0) were included in the analysis of disease count.
Box 1: Diseases included in disease count
Hypertension
Ischaemic heart disease
Cerebrovascular disease
Peripheral vascular disease
Heart failure
Atrial flutter or fibrillation
Arthritis (osteoarthritis or cervical or lumbar spondylosis or rheumatoid arthritis or other arthritis or non-specified arthritis)
Osteoporosis
Chronic obstructive pulmonary disease or asthma
Other respiratory disease
Diabetes
Hypothyroidism or hyperthyroidism
Cancer diagnosed within past five years (excluding non-melanoma skin cancer)
Eye disease (cataract or age related macular degeneration or glaucoma or diabetic eye disease or registered blind or partially sighted)
Dementia
Parkinson’s disease
Renal impairment
For ischaemic heart disease, diabetes, and thyroid disease, presence was defined as diagnosis either in general practice records or from health assessment test; for atrial fibrillation or flutter from an electrocardiogram (health assessment test); for renal impairment from estimated glomerular filtration rate <30 ml/min/1.73 m2 (health assessment test); and for anaemia, a haemoglobin concentration <11.5 g/dl (<115 g/l) (health assessment test). For all other diseases the presence was taken from record review data alone.
Statistical analysis
We present normally distributed continuous data as means and standard deviations, and variables with a non-Gaussian distribution as medians and interquartile ranges. When appropriate we present categorical data as percentages and 95% confidence intervals. To compare men with women we used logistic or ordinal regression as appropriate, with odds ratios and 95% confidence intervals, Mann-Whitney U test for non-normally distributed continuous variables, and χ2 tests for categorical variables. P values were two sided. We used version 1.0 of the dataset.
In general we excluded missing values from the analysis and calculated percentages from the number of valid responses. Where individual items were missing within two measures reported as categorical data—the 15 item geriatric depression scale18 and the standardised mini-mental state examination19—we compared scoring the missing item as zero or the maximum possible for that item with data retained only if a participant was classified in the same category in either case.
We considered a sample size of 800 sufficient to give a confidence interval of 3.5% either way on a prevalence of 50% and to provide sufficient power for analyses of major subgroups.
Results
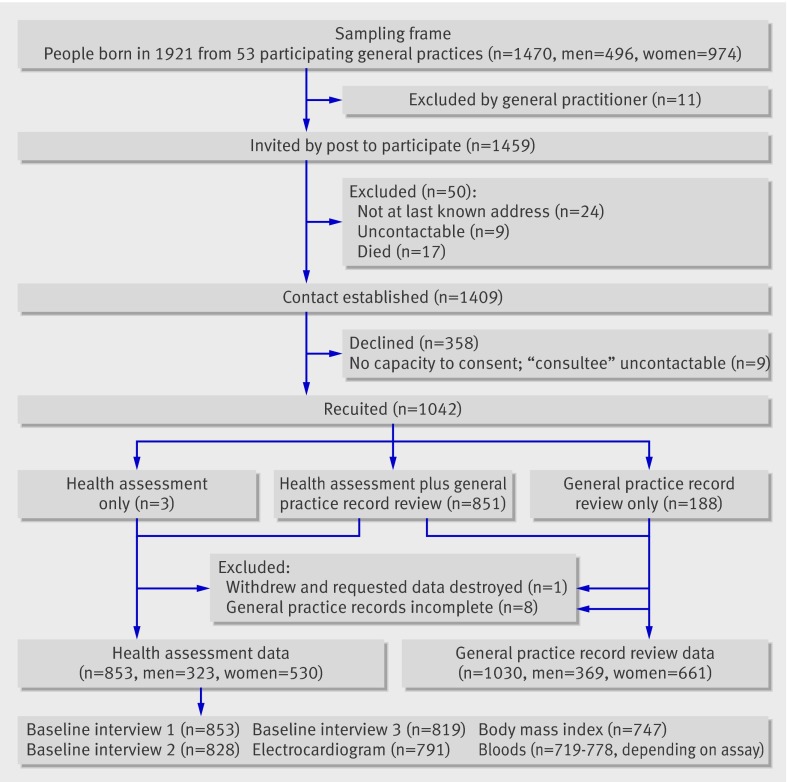
The figure summarises the recruitment profile. Of the 1453 people eligible to participate—that is, registered with a participating general practice and still alive—1042 (71.7%) participated. In total, 851 (58.6% of those eligible) people were recruited to health assessment plus review of general practice records, with an additional 188 (12.9%) to record review only, and 3 (0.2%) to health assessment only. Box 2 gives some technical details about the health assessment. One participant who agreed to a health assessment plus record review subsequently withdrew and requested the data to be destroyed; this participant was excluded from the health assessment and record review analysis. In eight cases (four each from the record review group and the health assessment plus record review group) the general practice paper records were unavailable and these participants were excluded from the record review analysis. To ensure maximum use of available data, variables from the general practice record review are reported on a maximum sample of 1030 people (representing 70.9% of those eligible) and from the health assessment on a maximum sample of 853 people (representing 58.7% of those eligible); sample sizes for individual variables may differ owing to missing values. Tables detailing the number of valid responses and missing values for each variable are given in the web extra.
Recruitment profile for cohort
Box 2: Health assessment technical details
The mean (standard deviation) total time taken for the health assessment (excluding the short visit for taking fasting blood samples and measuring body weight) was 206 (55) minutes over a median 25 days (interquartile range 16-36.5 days)
An informant supplied information in at least one of the interviews for 29% (247/853) of the participants in the health assessment group
96% of the 778 participants who had blood taken gave fasting samples
Representativeness of study sample
Overall, 53 of the 64 (83%) general practices in Newcastle upon Tyne and North Tyneside primary care trusts agreed to participate. Practices that participated were similar to those that did not for median practice size (6709 v 6000; Mann-Whitney U test P=0.78), proportion that were training practices (32% v 36%; χ²=0.1, P=0.78), median score from the UK National Health Service (NHS) quality and outcomes framework for 2006-720 (993.5 v 981.7; Mann-Whitney U test P=0.23), and median index of multiple deprivation score for 200421 using the practice postcode (22.1 v 20.7; Mann-Whitney U test P=0.37).
On comparing participants’ sociodemographic status with equivalent figures from the 2001 national census for Newcastle upon Tyne and North Tyneside and for England and Wales (table 1), the Newcastle 85+ cohort is broadly representative of the local population, although there was slight under-representation of women (62.1% (530/853) in health assessment sample, 64.2% (661/1030) in record review sample, 66.5% in local census data). Sociodemographically, Newcastle upon Tyne and North Tyneside are generally comparable to England and Wales except for ethnic diversity (census data for non-white population in Newcastle upon Tyne and North Tyneside 0.7% and in England and Wales 10.8%). To investigate whether differential response might affect results, a comparison was made between refusers (n=358), record review only participants (n=184), and those agreeing to health assessment plus record review (n=846) on sex and index of multiple deprivation score, excluding cases with incomplete general practice records. Deprivation did not differ significantly but significantly fewer females were in the health assessment plus record review group (62.3%, 527/846) than in the record review only group (73%, 134/184) and refusers (74%, 265/358) (χ2=21.3, df=2, P<0.001).
Table 1.
Sociodemographic data, smoking status, and body mass index of population aged 85, by sex. Values are percentages (numbers) unless stated otherwise
| Variables | All | Women | Men | Census (2001) | P value* | |
|---|---|---|---|---|---|---|
| Newcastle and North Tyneside (%) | England and Wales (%) | |||||
| Men | 37.9 (323) | — | — | 33.5 | 32.6 | — |
| Women | 62.1 (530) | — | — | 66.5 | 67.3 | — |
| Housing: | 0.007 | |||||
| Standard | 76.8 (655) | 73.0 (387) | 83.0 (268) | — | — | |
| Sheltered | 12.7 (108) | 14.2 (75) | 10.2 (33) | — | — | |
| Institution | 10.4 (89) | 12.6 (67) | 6.8 (22) | 12.0 | 11.2 | |
| Other | 0.1 (1) | 0.2 (1) | 0 (0) | — | — | |
| Living arrangements†: | <0.001 | |||||
| Alone | 61.0 (465) | 73.3 (338) | 42.2 (127) | 57.0 | 55.0 | |
| With spouse only | 28.1 (214) | 13.9 (64) | 49.8 (150) | — | — | |
| With others | 10.9 (83) | 12.8 (59) | 8.0 (24) | — | — | |
| Marital status: | <0.001 | |||||
| Widowed | 59.0 (500) | 70.4 (371) | 40.2 (129) | 62.3‡ | 61.2‡ | |
| Married | 30.0 (254) | 16.3 (86) | 52.3 (168) | 27.0‡ | 27.6‡ | |
| Never married | 8.3 (70) | 9.9 (52) | 5.6 (18) | 8.0‡ | 8.2‡ | |
| Divorced or separated | 2.8 (24) | 3.4 (18) | 1.9 (6) | 2.8‡ | 2.4‡ | |
| Ethnic origin: | 0.304 | |||||
| White | 99.6 (846) | 99.8 (526) | 99.4 (320) | 99.3‡ | 89.2‡ | |
| Non-white | 0.4 (3) | 0.2 (1) | 0.6 (2) | 0.7‡ | 10.8‡ | |
| Born in north east England | 77.0 (652) | 79.7 (419) | 72.6 (233) | — | — | 0.018 |
| Smoking status: | <0.001 | |||||
| Current smoker | 5.8 (49) | 6.5 (34) | 4.7 (15) | — | — | |
| Former regular smoker | 53.5 (453) | 45.7 (241) | 66.3 (212) | — | — | |
| Former occasional smoker | 5.0 (42) | 5.9 (31) | 3.4 (11) | — | — | |
| Never smoker | 35.8 (303) | 41.9 (221) | 25.6 (82) | — | — | |
| Body mass index (kg/m2)§: | ||||||
| Underweight (<18.50) | 6.4 (48) | 7.8 (35) | 4.4 (13) | — | — | |
| Normal range (18.50-24.99) | 51.3 (383) | 51.2 (230) | 51.3 (153) | — | — | |
| Pre-obese (25.00-29.99) | 32.5 (243) | 30.3 (136) | 35.9 (107) | — | — | |
| Obese (30.00-39.99) | 9.5 (71) | 10.2 (46) | 8.4 (25) | — | — | |
| Morbidly obese (≥40.00) | 0.3 (2) | 0.5 (2) | 0.0 (0) | — | — | |
Data from health assessment.
*Sex difference.
†Excludes people in institutional care.
‡Average of 80-84 and 85-89 age groups.
§Odds ratio (95% confidence interval) women to men 0.9 (0.7 to 1.2).
Sociodemographics
Three quarters (655/853) of the health assessment sample lived in standard housing, with only 12.7% (n=108) in sheltered accommodation and 10.4% (n=89) in institutional care (table 1); all those in institutional care were living in care homes. Of those not in institutional care, 61.0% (465/762) were living alone. Women outnumbered men by 1.6 to 1 and were more likely to be living in institutional care or sheltered accommodation, living alone, or widowed.
Disease prevalence and undiagnosed diseases
The most prevalent diseases were hypertension (57.5%, 592/1030) and osteoarthritis (51.8%, 534/1030); other common diseases were atherosclerosis (47.2% 486/1030) and cataract (47.0%, 483/1030; tables 2 and 3 ). Women were 10 times more likely than men to have rheumatoid arthritis, eight times more likely to have a diagnosis of hyperthyroidism, three times more likely to have a diagnosis of hypothyroidism, and six times more likely to have osteoporosis. Women also had a significantly higher prevalence of cataract, osteoarthritis, joint replacement, renal impairment (by the modification of diet in renal disease formula22 but not the Mayo Clinic quadratic equation),23 and anaemia (Joosten’s criterion).24 Men were significantly more likely to have a diagnosis of atherosclerotic disease and cancer.
Table 2.
Disease, by sex. Values are percentages (numbers) unless stated otherwise
| Diseases | All | Women | Men | Odds ratio (95% CI) women to men |
|---|---|---|---|---|
| Cardiovascular: | ||||
| Hypertension* | 57.5 (592) | 60.1 (397) | 52.9 (195) | 1.3 (1.0 to 1.8) |
| Any atherosclerotic disease* | 47.2 (486) | 42.8 (283) | 55.0 (203) | 0.6 (0.5 to 0.8) |
| Ischaemic heart disease* | 31.4 (323) | 28.3 (187) | 36.9 (136) | 0.7 (0.5 to 0.9) |
| Cerebrovascular disease* | 20.1 (207) | 17.6 (116) | 24.7 (91) | 0.7 (0.5 to 0.9) |
| Peripheral vascular disease* | 6.8 (70) | 5.3 (35) | 9.5 (35) | 0.5 (0.3 to 0.9) |
| Heart failure* | 11.1 (114) | 10.1 (67) | 12.7 (47) | 0.8 (0.5 to 1.2) |
| Atrial fibrillation† | 14.0 (111) | 12.3 (59) | 16.8 (52) | 0.7 (0.5 to 1.1) |
| Atrial flutter† | 0.5 (4) | 0.4 (2) | 0.7 (2) | 0.6 (0.1 to 8.9) |
| Musculoskeletal*: | ||||
| Osteoarthritis | 51.8 (534) | 57.0 (377) | 42.6 (157) | 1.8 (1.4 to 2.3) |
| Cervical or lumbar spondylosis | 29.6 (305) | 30.4 (201) | 28.2 (104) | 1.1 (0.8 to 1.5) |
| Rheumatoid arthritis | 3.5 (36) | 5.1 (34) | 0.5 (2) | 10.0 (2.5 to 85.9) |
| Other arthritis (specified) | 3.3 (34) | 3.0 (20) | 3.8 (14) | 0.8 (0.4 to 1.7) |
| Arthritis (type not specified) | 9.0 (93) | 10.0 (66) | 7.3 (27) | 1.4 (0.9 to 2.3) |
| Joint replacement | 13.5 (139) | 15.6 (103) | 9.8 (36) | 1.7 (1.1 to 2.6) |
| Osteoporosis | 14.2 (146) | 20.0 (132) | 3.8 (14) | 6.3 (3.6 to 12.1) |
| Eye*: | ||||
| Cataract | 46.9 (483) | 51.6 (341) | 38.5 (142) | 1.7 (1.3 to 2.2) |
| Cataract surgery | 36.2 (373) | 39.2 (259) | 30.9 (114) | 1.4 (1.1 to 1.9) |
| Age related macular degeneration | 13.8 (142) | 14.8 (98) | 11.9 (44) | 1.3 (0.9 to 1.9) |
| Glaucoma | 8.6 (89) | 8.9 (59) | 8.1 (30) | 1.1 (0.7 to 1.8) |
| Diabetic eye disease | 1.5 (15) | 1.4 (9) | 1.6 (6) | 0.8 (0.3 to 2.9) |
| Registered blind | 2.2 (23) | 1.8 (12) | 3.0 (11) | 0.6 (0.2 to 1.5) |
| Registered partially sighted | 3.2 (33) | 4.1 (27) | 1.6 (6) | 2.6 (1.0 to 7.7) |
| Cancer*: | ||||
| Any cancer | 23.9 (246) | 19.8 (131) | 31.2 (115) | 0.6 (0.4 to 0.7) |
| Any cancer, excluding non-melanoma skin cancer | 15.1 (155) | 12.3 (81) | 20.1 (74) | 0.6 (0.4 to 0.8) |
| Any cancer <5 years since diagnosis‡ | 6.5 (67) | 5.2 (34) | 9.0 (33) | 0.6 (0.3 to 0.9) |
*Data from general practice record review.
†Data from health assessment 12 lead electrocardiogram.
‡Excluding non-melanoma skin cancer.
Table 3.
Disease, by sex, continued from table 2. Values are percentages (numbers) unless stated otherwise
| Diseases | All | Women | Men | Odds ratio (95% CI) women to men |
|---|---|---|---|---|
| Respiratory*: | ||||
| Chronic obstructive pulmonary disease | 16.5 (170) | 14.5 (96) | 20.1 (74) | 0.7 (0.5 to 1.0) |
| Asthma† | 4.8 (49) | 5.8 (38) | 3.0 (11) | 2.0 (1.0 to 4.4) |
| Other respiratory disease | 2.7 (28) | 1.8 (12) | 4.3 (16) | 0.4 (0.2 to 0.9) |
| Endocrine*: | ||||
| Diabetes mellitus | 13.1 (135) | 12.1 (80) | 14.9 (55) | 0.8 (0.5 to 1.2) |
| Hypothyroidism | 12.0 (124) | 15.7 (104) | 5.4 (20) | 3.3 (2.0 to 5.7) |
| Hyperthyroidism | 2.8 (29) | 4.1 (27) | 0.5 (2) | 7.8 (1.9 to 68.1) |
| Neurological and psychiatric*: | ||||
| Dementia | 8.4 (86) | 9.1 (60) | 7.1 (26) | 1.3 (0.8 to 2.2) |
| Parkinson’s disease | 1.5 (15) | 1.2 (8) | 1.9 (7) | 0.6 (0.2 to 2.1) |
| Anaemia‡: | ||||
| WHO criteria for haemoglobin concentration§ | 29.8 (225) | 27.5 (126) | 33.3 (99) | 0.8 (0.6 to 1.1) |
| Joosten’s criterion for haemoglobin concentration: <11.5 g/dl (<115 g/l) | 14.2 (107) | 17.7 (81) | 8.8 (26) | 2.2 (1.4 to 3.7) |
| Renal function¶ using modification of diet in renal disease formula: | 1.7 (1.3 to 2.3) | |||
| Normal | 1.0 (8) | 0.9 (4) | 1.3 (4) | |
| Mildly reduced | 36.4 (283) | 31.5 (149) | 43.9 (134) | |
| Moderately reduced(stage 3††) | 59.5 (463) | 64.3 (304) | 52.1 (159) | |
| Severely reduced (stage 4††) | 2.4 (19) | 2.8 (13) | 2.0 (6) | |
| Very severely reduced (stage 5††) | 0.6 (5) | 0.6 (3) | 0.7 (2) | |
| Renal function¶ using Mayo Clinic quadratic equation: | 0.8 (0.6 to 1.1) | |||
| Normal | 3.6 (28) | 0.0 (0) | 9.2 (28) | |
| Mildly reduced | 61.4 (478) | 69.6 (329) | 48.9 (149) | |
| Moderately reduced (stage 3††) | 31.8 (247) | 27.7 (131) | 38.0 (116) | |
| Severely reduced (stage 4††) | 2.2 (17) | 2.1 (10) | 2.3 (7) | |
| Very severely reduced (stage 5††) | 1.0 (8) | 0.6 (3) | 1.6 (5) | |
| Median (interquartile range) disease count‡‡ | 5 (3-6) | 5 (4-6) | 4 (3-6) |
*Data from general practice record review.
†Excluded in combination with chronic obstructive pulmonary disease.
‡Data from health assessment measured haemoglobin concentration.
§Men <13 g/dl (<130 g/l), women <12 g/dl (<120 g/l).
¶Data from health assessment measured creatinine concentration. Estimated glomerular filtration rate ranges for renal function categories for both formulas: normal >89 ml/min/1.73 m2, mildly reduced 60-89 ml/min/1.73 m2, moderately reduced 30-59 ml/min/1.73 m2, severely reduced 15-29 ml/min/1.73 m2, and very severely reduced <15 ml/min/1.73 m2.
††Stage of chronic kidney disease; US National Kidney Foundation Kidney Disease Outcomes Quality Initiative classification (see www.kidney.org/PROFESSIONALS/kdoqi/guidelines_ckd/toc.htm).
‡‡18 diseases: hypertension, ischaemic heart disease, cerebrovascular disease, peripheral vascular disease, heart failure, atrial flutter or fibrillation, arthritis, osteoporosis, chronic obstructive pulmonary disease or asthma, other respiratory disease, diabetes, hypothyroidism or hyperthyroidism, cancer diagnosed within past five years (excluding non-melanoma skin cancer), eye disease, dementia, Parkinson’s disease, renal impairment, and anaemia.
Table 4 gives estimates of the prevalence of possible undiagnosed disease; data are reported for those participants with both the general practice record review and the relevant test from the health assessment available. For hypertension, ischaemic heart disease, diabetes, and thyroid disease the prevalence of diagnosed disease is reported from record review data followed by the prevalence of possible undiagnosed disease taken from the relevant health assessment data in those without a previous diagnosis. For depression, dementia, and atrial fibrillation, an estimate of the point prevalence of possible disease is reported from health assessment data followed by the prevalence of possible disease in the absence of a previous diagnosis in the general practice records. Although hypertension would not be diagnosed from a single time point, review of the measured blood pressure in those without a recorded diagnosis of hypertension suggested an additional 25.1% (206/821) with possible at least grade 1 hypertension, of whom half had grade 2. Of those with a diagnosis of hypertension recorded in the general practice records, only 35% (164/475) had both a systolic blood pressure below 140 mm Hg and a diastolic blood pressure below 90 mm Hg, although 87% (411/475) were using antihypertensive drugs. In addition to the 33.0% (260/788) of the sample who had a recorded diagnosis of ischaemic heart disease, electrocardiography in those with no diagnosis revealed a further 12.6% (99/788) with evidence of definite (2.4%, 19/788) or probable (10.2%, 80/788) myocardial ischaemia. There was little evidence of undiagnosed diabetes or thyroid disease. With respect to depression, 8.4% (65/772) had a geriatric depression scale score suggestive of severe depression, of whom 82% (53/65) had no diagnosis recorded in the general practice records in the previous year. A standardised mini-mental state examination score suggesting moderate or severe cognitive impairment was found in 12.5% (105/840) of participants, of whom 53% (56/105) had no diagnosis of dementia in the general practice records. Atrial fibrillation was evident on electrocardiography in 13.8% (109/788) of participants, of whom 28% (30/109) had no diagnosis apparent in the general practice records. Levels of undiagnosed disease did not differ significantly between men and women.
Table 4.
Potential undiagnosed disease, by sex. Values are percentages (numbers) unless stated otherwise
| Diseases | All | Women | Men | Odds ratio (95% CI) women to men |
|---|---|---|---|---|
| Hypertension | ||||
| Measured blood pressure and record review available: | 100 (821) | 100 (508) | 100 (313) | |
| Hypertension diagnosis in record review | 57.9 (475) | 60.8 (309) | 53.0 (166) | |
| No diagnosis; systolic ≥140 mm Hg or diastolic ≥90 mm Hg | 25.1 (206) | 24.0 (122) | 26.8 (84) | 0.9 (0.6 to 1.2) |
| No diagnosis; systolic ≥160 mm Hg or diastolic ≥100 mm Hg | 12.3 (101) | 12.0 (61) | 12.8 (40) | 0.9 (0.6 to 1.5) |
| No diagnosis; systolic ≥160 mm Hg and diastolic <90 mm Hg | 8.5 (70) | 7.9 (40) | 9.6 (30) | 0.8 (0.5 to 1.4) |
| Ischaemic heart disease | ||||
| ECG and record review available: | 100 (788) | 100 (480) | 100 (308) | |
| Ischaemic heart disease diagnosis in record review | 33.0 (260) | 30.6 (147) | 36.7 (113) | |
| No diagnosis; ECG evidence of definite ischaemic heart disease | 2.4 (19) | 2.3 (11) | 2.6 (8) | 0.9 (0.3 to 2.6) |
| No diagnosis; ECG evidence of probable ischaemic heart disease | 10.2 (80) | 10.8 (52) | 9.1 (28) | 1.2 (0.7 to 2.1) |
| Diabetes | ||||
| Fasting glucose and record review available: | 100 (717) | 100 (432) | 100 (285) | |
| Diabetes diagnosis in record review | 13.5 (97) | 13.9 (60) | 13.0 (37) | |
| No diagnosis; fasting glucose ≥7 mmol/l | 1.0 (7) | 0.9 (4) | 1.1 (3) | 0.9 (0.2 to 6.0) |
| Hypothyroidism | ||||
| Hypothyroid blood screen and record review available: | 100 (762) | 100 (465) | 100 (297) | |
| Hypothyroidism diagnosis in record review | 12.3 (94) | 16.6 (77) | 5.7 (17) | |
| No diagnosis; hypothyroid screen positive | 0.5 (4) | 0.4 (2) | 0.7 (2) | 0.6 (0.1 to 8.8) |
| Hyperthyroidism | ||||
| Hyperthyroid blood screen and record review available: | 100 (762) | 100 (465) | 100 (297) | |
| Hyperthyroidism diagnosis in record review | 2.9 (22) | 4.3 (20) | 0.7 (2) | |
| No diagnosis; hyperthyroid screen positive | 0.3 (2) | 0.2 (1) | 0.3 (1) | 0.6 (0.0 to 50.2) |
| Depression | ||||
| GDS-15 score* and record review available: | 100 (772) | 100 (474) | 100 (298) | |
| GDS-15 ≥8 (suggestive of severe depression) | 8.4 (65) | 9.3 (44) | 7.1 (21) | |
| GDS-15 ≥8 and no record review diagnosis of depression in past year | 6.9 (53) | 7.6 (36) | 5.7 (17) | 1.4 (0.7 to 2.6) |
| Dementia | ||||
| SMMSE score and record review available: | 100 (840) | 100 (523) | 100 (317) | |
| SMMSE ≤21 (moderate or severe cognitive impairment) | 12.5 (105) | 14.2 (74) | 9.8 (31) | |
| SMMSE ≤21 and no record review diagnosis of dementia | 6.7 (56) | 7.3 (38) | 5.7 (18) | 1.3 (0.7 to 2.6) |
| SMMSE ≤17 (severe cognitive impairment) | 6.9 (58) | 7.3 (38) | 6.3 (20) | |
| SMMSE ≤17 and no record review diagnosis of dementia | 3.0 (25) | 3.3 (17) | 2.5 (8) | 1.3 (0.5 to 3.5) |
| Atrial fibrillation | ||||
| ECG and record review available: | 100 (788) | 100 (480) | 100 (308) | |
| Atrial fibrillation on ECG (Minnesota code 8-3-1) | 13.8 (109) | 12.1 (58) | 16.6 (51) | |
| Atrial fibrillation on ECG and no record review diagnosis of atrial fibrillation | 3.8 (30) | 3.1 (15) | 4.9 (15) | 0.6 (0.3 to 1.4) |
ECG=electrocardiogram; GDS=geriatric depression scale; SMMSE=standardised mini-mental state examination.
*GDS-15 omitted if score <15 on SMMSE.
The disease count is reported on the 729 participants in whom all required variables were present. No participant was free of all 18 diseases and the maximum count was 11 (men 10, women 11). Women had a significantly higher number of diseases than men (P=0.033).
Geriatric syndromes, impairments, self rated health, and disability
Hearing impairment was reported by 59.6% (505/848) of the participants, visual impairment by 37.2% (309/831), pain in the past month (lasting a day or longer) by 50.0% (402/805), at least one fall in the previous year by 38.3% (312/815) (8.0% (65/815) reporting three or more falls), severe or profound urinary incontinence by 21.3% (173/813), and faecal incontinence by 8.6% (70/816) (table 5). Seventy eight per cent of participants (646/832) rated their health compared with others of the same age as good, very good, or excellent, with only 3.5% (29/832) rating it as poor. Almost one fifth (165/842) of the cohort had no difficulty with any of 17 activities of daily living; the median (interquartile range) for the number of items carried out with difficulty or requiring an aid, appliance, or personal help was 3 (1-8). Women had significantly higher disability scores than men (P=0.0006) and were also significantly more likely to have visual impairment or urinary incontinence and to be rated as depressed on the geriatric depression scale.
Table 5.
Geriatric syndromes, impairments, disability, and self rated health, by sex. Values are percentages (numbers) unless stated otherwise
| Variables | All | Women | Men | Odds ratio (95% CI) women to men |
|---|---|---|---|---|
| Hearing impairment | 59.6 (505) | 56.9 (300) | 63.9 (205) | 0.8 (0.6 to 1.0) |
| Visual impairment | 37.2 (309) | 40.7 (209) | 31.6 (100) | 1.5 (1.1 to 2.0) |
| Pain in past month (lasting ≥1 days) | 49.9 (402) | 53.0 (262) | 45.0 (140) | 1.4 (1.0 to 1.9) |
| Falls in past year: | 1.0 (0.7 to 1.3) | |||
| None | 61.7 (503) | 61.8 (312) | 61.6 (191) | |
| 1 | 20.5 (167) | 21.2 (107) | 19.4 (60) | |
| 2 | 9.8 (80) | 8.9 (45) | 11.3 (35) | |
| ≥3 | 8.0 (65) | 8.1 (41) | 7.7 (24) | |
| Urinary incontinence: | 2.1 (1.6 to 2.8) | |||
| None | 56.7 (461) | 49.9 (251) | 67.7 (210) | |
| Minimal | 10.7 (87) | 11.3 (57) | 9.7 (30) | |
| Moderate | 10.1 (82) | 10.9 (55) | 8.7 (27) | |
| Severe or profound | 21.3 (173) | 26.6 (134) | 12.6 (39) | |
| Catheterised for past year | 1.2 (10) | 1.2 (6) | 1.3 (4) | |
| Faecal incontinence | 8.6 (70) | 9.3 (47) | 7.4 (23) | 1.3 (0.8 to 2.3) |
| Depression (GDS-15 score*): | 1.6 (1.1 to 2.3) | |||
| None (0-5) | 79.1 (601) | 76.4 (356) | 83.3 (245) | |
| Mild or moderate (6-7) | 12.4 (94) | 14.2 (66) | 9.5 (28) | |
| Severe (8-15) | 8.6 (65) | 9.4 (44) | 7.1 (21) | |
| Cognitive impairment (SMMSE score): | 1.1 (0.8 to 1.5) | |||
| Normal (26-30) | 73.1 (602) | 73.1 (372) | 73.0 (230) | |
| Mild (22-25) | 15.3 (126) | 14.0 (71) | 17.5 (55) | |
| Moderate (18-21) | 5.1 (42) | 6.5 (33) | 2.9 (9) | |
| Severe (0-17) | 6.6 (54) | 6.5 (33) | 6.7 (21) | |
| Median (interquartile range) disability score† | 3 (1-8) | 4 (1-9) | 2 (0-6) | — |
| Self rated health (compared to others of same age): | 1.3 (1.0 to 1.7) | |||
| Excellent | 10.3 (86) | 9.5 (49) | 11.7 (37) | |
| Very good | 29.7 (247) | 28.1 (145) | 32.3 (102) | |
| Good | 37.6 (313) | 38.2 (197) | 36.7 (116) | |
| Fair | 18.9 (157) | 20.2 (104) | 16.8 (53) | |
| Poor | 3.5 (29) | 4.1 (21) | 2.5 (8) |
GDS=geriatric depression scale; SMMSE=standardised mini-mental state examination.
Data from health assessment.
*GDS-15 omitted if score <15 on SMMSE.
†No of activities of daily living carried out with difficulty or requiring an aid, appliance, or personal help.
Health service use
Almost one third (268/844) of the sample had attended outpatient clinics in the three months before the study (table 6). In the previous year, 22.1% (188/850) had had at least one overnight stay in hospital, spending, on average, seven days in total over the stays. Almost all (93.8%, 960/1024) of the sample had seen their general practitioner within the past year (median consultation rate over the year for those who consulted of 5); 61.7% (3752/6085) of consultations took place at the general practice surgery, 23.5% (1430/6085) were home visits, 13.5% (822/6085) were telephone consultations, and 1.0% (80/6085) were by letter. Only 6.0% (58/971) had contact with the general practice out of hours service. Just over three quarters (780/1008) had seen the practice nurse (median consultation rate over the year for those who consulted of 2) with 90.0% (2768/3074) of contacts in the general practice surgery. In the previous month, 95.0% (979/1030) were taking medication prescribed by their general practice team, with a mean (standard deviation) of 6.7 (3.7) items: men 6.3 (3.5), women 6.9 (3.7), P=0.07. Coding according to the British National Formulary,25 the top three categories of prescribed medication were for the cardiovascular system (40.3%, 2639/6547), central nervous system (13.4%, 879/6547, including analgesics but excluding non-steroidal anti-inflammatory drugs), and gastrointestinal system (10.6%, 692/6547). The only sex difference in health service use was a significantly lower proportion of women having outpatient attendances and consultations with a practice nurse.
Table 6.
Health service use, by sex. Values are percentages (numbers) unless stated otherwise
| Variables | All | Women | Men | Odds ratio (95% CI) women to men | P value* |
|---|---|---|---|---|---|
| Previous 3 months†: | |||||
| Any outpatient attendance | 31.8 (268) | 28.6 (150) | 36.9 (118) | 0.7 (0.5 to 0.9) | |
| Median (interquartile range) No of outpatient attendances | 1 (1-2) | 1 (1-2) | 1 (1-2) | — | 0.218 |
| Any accident and emergency attendance | 7.1 (60) | 7.2 (38) | 6.8 (22) | 1.1 (0.6 to 1.9) | |
| Median (interquartile range) No of accident and emergency attendances | 1 (1-1) | 1 (1-1) | 1 (1-1) | — | 0.858 |
| Any emergency ambulance use | 5.1 (43) | 5.1 (27) | 5.0 (16) | 1.0 (0.5 to 2.1) | |
| Previous year: | |||||
| Any overnight hospital admission† | 22.1 (188) | 21.4 (113) | 23.2 (75) | 0.9 (0.6 to 1.3) | |
| Median (interquartile range) total stay in hospital (days) † | 7 (3-20) | 8.5 (3-20) | 7 (2-16) | — | 0.458 |
| Any respite care†‡ | 2.9 (24) | 3.2 (16) | 2.5 (8) | 1.3 (0.5 to 3.5) | |
| Median (interquartile range) total stay in respite care (days)† ‡ | 14 (7-22.5) | 14 (12.5-22.5) | 11.5 (7-28) | — | 0.829 |
| Any day hospital attendance† | 7.5 (63) | 7.8 (41) | 6.8 (22) | 1.2 (0.7 to 2.1) | |
| Any other intermediate care contact† | 7.6 (64) | 8.5 (44) | 6.2 (20) | 1.4 (0.8 to 2.5) | |
| Any consultations with own general practitioner (including out of hours contacts)§ | 93.8 (960) | 93.8 (616) | 93.7 (344) | 1.0 (0.6 to 1.8) | |
| Median (interquartile range) No of own general practitioner consultations§ | 5 (2-8) | 5 (2-8) | 5 (2-8) | — | 0.661 |
| Any consultations with out of hours general practice service§ | 6.0 (58) | 6.6 (41) | 4.8 (17) | 1.4 (0.8 to 2.7) | |
| Any consultations with practice nurse§ | 77.4 (780) | 73.8 (477) | 83.7 (303) | 0.6 (0.4 to 0.8) | |
| Median (interquartile range) No of practice nurse consultations§ | 2 (1-4) | 2 (0-4) | 2 (1-5) | — | 0.008 |
*Sex difference.
†Data from health assessment.
‡Excludes those in institutional care for previous year.
§Data from general practice record review.
Discussion
The Newcastle 85+ Study secured a high level of participation from 85 year olds, including those living in institutions and those with cognitive impairment. Perhaps the most striking findings were the low levels of disability and people living in institutional care, and positive self rated health (compared with others of the same age) despite high levels of disease and impairment. The prevalence of diagnosed hypertension, atherosclerotic disease, osteoarthritis, and cataract were each close to 50%, and almost 90% of participants had at least three diseases. Two thirds reported hearing impairment, one third visual impairment, almost 40% had had falls, and 20% had notable urinary incontinence. A meta-analysis26 found higher levels of optimism for self rated health in people aged 75 or more compared with younger age groups, when comparative measures (compared with people of the same age) as opposed to absolute measures were used. Notable sex differences were apparent from our study in line with previous reports;27 although women were more likely to survive to age 85 (female to male ratio 1.6:1), they were more likely to be living in institutional care, to have a higher total disease count and higher prevalence of many diseases (excepting two important life threatening conditions, atherosclerosis and cancer, where the prevalence was higher in men, potentially contributing to differences in survival), to have more visual impairment, urinary incontinence, and depression, and higher levels of disability, despite the tight age criteria. Men born in 1921 would have been 18 in 1939 at the outbreak of the second world war, which could have contributed to differences in survival. Although women had higher levels of disease and disability, they were less likely to have had an outpatient attendance in the previous three months.
Possible underdiagnosis of important clinical conditions
Despite the high contact rates of the participants with primary care in the previous year, our data raise the possibility of underdiagnosis of important clinical conditions, although the interpretation of this should be appropriately cautious. In collecting data from general practice records, a diagnosis was noted as present if recorded anywhere in the records, irrespective of date. In some cases—for example, cataract and thyroid disease—a disease may have been successfully treated, so the diagnosis would no longer be current; this should be considered when reviewing the data on disease in tables 2 and 3. The data on diabetes and thyroid disease from our two sources were in close agreement. Given what is known more generally about underdiagnosis, our data for hypertension, atrial fibrillation, ischaemic heart disease, dementia, and depression are not surprising. While our assessment of hypertension should be treated with caution, as blood pressure was measured on one occasion, 25% of the sample had a measured blood pressure in the hypertensive range, without a diagnosis of hypertension in the general practice records; with proper clinical assessment a proportion of these would subsequently be within the normal range. Similarly, for around two thirds of those with a known diagnosis of hypertension, the blood pressure measured in the study was outside the target ranges recommended by guidelines.28 29 Given that the recent Hypertension in the Very Elderly Trial30 showed that treatment of hypertension was beneficial in those aged 80 and older, a more aggressive approach to case finding and control of blood pressure may be warranted in this age group. However, considering the strict exclusion criteria applied in clinical trials, the utility and feasibility of this approach in unselected populations of older people remains to be established. The prevalence of undiagnosed dementia was estimated at 7% and although the screen used for dementia is not diagnostic, the overall prevalence of moderate to severe cognitive impairment of 13% was close to the prevalence of dementia found in the MRC-CFAS study,11 which used instruments more sensitive to dementia case finding. We have shown previously31 that differences in consultation patterns can be observed up to four years before a formal diagnosis of dementia, indicating that general practitioners do attend to possible signs of early dementia. It is not, however, practicable to use the systematic review of primary care records to facilitate earlier diagnosis without identifying large numbers of false positive results requiring investigation. Undiagnosed depression is not just a feature of the oldest old, and in a population with other chronic illness its presence is perhaps not surprising. What is less clear is how this could be readily detected in a routine setting and what might be the uptake and effects of treatment. We found a high prevalence of moderate renal impairment, particularly in women, using the widely accepted modification of diet in renal disease formula, in common with recent findings.32 Using the Mayo Clinic quadratic equation resulted in almost half of those classified as moderately impaired by the modification of diet in renal disease formula moving to a less severe category, in line with the findings of another study,33 and we conclude that the Mayo Clinic quadratic equation may be more appropriate for use in older people.
Strengths and limitations of the study
A key strength of our study is the high response rate achieved from both general practices and participants. Eighty three per cent of general practices in the region agreed to participate and participating and non-participating practices were similar in terms of practice size, training practice status, NHS quality and outcomes framework score, and index of multiple deprivation on the basis of practice postcode. Fifty nine per cent of eligible people were recruited to both health assessment and review of general practice records, with an additional 13% recruited to review of records only; good participation rates, considering the age group of the sample and the extensive assessment involved. A major concern in any cohort study is whether the participants are representative of the population from which they are drawn. It is possible that the non-responders or refusers to our study were frailer than the participants, which could lead to an underestimate in the reported levels of disease (both diagnosed and undiagnosed), disability, and poor self rated health. The reason for non-response or refusal to participate were available in 57% of non-participants for the health assessment and 49% for the review of general practice records, and in only 30% and 28% of these was non-response or refusal related to poor health. We have shown that by comparison with local census data the sample we recruited to health assessment was sociodemographically broadly representative of the local population, although women were slightly under-represented. Importantly, our sample was representative in terms of the proportion of people living in institutions and also included people who were cognitively impaired; two groups excluded from many previous studies.
In terms of study design, a major strength of the Newcastle 85+ Study is its success in securing a high recruitment of participants with two things in common; year of birth and registration with a general practice in Newcastle upon Tyne or North Tyneside. The focus on a single year birth cohort and a closely circumscribed geographical area, with known population stability and little ethnic diversity, will be a major strength when carrying out comparisons within a cohort to explore factors that influence health status, as this will lessen extraneous variability. However, we acknowledge that this strength might also constitute a weakness by limiting the generalisabilty of the health survey findings to other populations. Comparison of the Newcastle 85+ cohort with sociodemographic data from the national census 2001 showed our sample to be broadly representative of England and Wales but with a notable difference in ethnic diversity, and it is known that people from ethnic minority groups have different health risk profiles from those of white populations. In addition, Newcastle and North Tyneside are urban areas, which might limit application of our findings to rural settings. Home based assessment was vital for this high recruitment; 50% of participants in our pilot study stated that they would have been less likely to participate if hospital attendance was required (unpublished data). Additional strengths are the comprehensive nature of the health data collected and the use of a combination of detailed assessment of participants with review of general practice records for data on diseases and medication, rather than reliance on self report. Previous studies34 35 have shown self report to be less reliable than a doctor diagnosis for certain diseases, particularly in older age groups and in those with multiple morbidities or cognitive impairment. Inter-rater reliability for data extraction from general practice records showed moderate or better agreement for the diseases assessed; false positive and false negative results are possible, which could lead to overestimates or underestimates in the disease prevalence (tables 2 and 3) and also affect the prevalence of undiagnosed disease (table 4). The discordance that was found between nurses on the recording of the total number of medications necessitates some caution; however, the number of medications in the three most common categories showed no significant disagreement. We recognise that, despite a high level of recruitment and retention of participants throughout an intensive series of assessments, the greatly varying capabilities of the participants has the potential to introduce some bias through incompleteness of assessment, although this was not large.
Conclusions and policy implications
It is difficult to estimate to what extent this cohort of 85 year olds represents a “healthy elite,” given that life expectancy at birth for the 1921 cohort was 61 years for men and 68 years for women, with only 18% of men and 33% of women surviving to age 85.36 Information from the study is none the less valuable. For planners of services, on the basis of present demographic trends, we can say that in the UK by 2020 the 85 year old population will increase by 33%,37 10% of whom currently require institutional care, 32% of whom have had an outpatient attendance, and 7% an attendance at an accident and emergency department in the past three months; it is likely that these figures will be closely paralleled in other high income countries. In addition, 61% of older people not in institutional care were living alone, which has implications for the availability of help with activities of daily living and hence to providers of social care. The survey findings highlight the potential unmet health and social care needs of this age group mirroring the findings of a study38 in the late 1950s. In times of scarce resources for health and social care these findings can be used by local and national policy makers to help target those in greatest need. In summary, these 85 year olds seemed optimistic, most rating their overall health as good, very good, or excellent compared with others of the same age. Our study shows the opportunities available to intervene to improve health further in this age group. If the data are extrapolated to the future, much larger, populations of 85 year olds in developed countries, implications for health and social care and the resources needed to provide these are profound.
Future work
The baseline phase of the Newcastle 85+ Study has resulted in a uniquely rich dataset. This paper provides a comprehensive picture of health and disease among 85 year olds in north east England at a particular time, which will serve as a baseline for the prospective monitoring of changes in health status of study participants and as a comparison with future cohorts of the oldest old to monitor changes in population health. The full potential of these data has yet to be exploited; further work is in progress tackling particular health domains in more detail, together with an exploration of factors underlying the variability in health. The identification of biomarkers of ageing is a major avenue of research. Future work will include the development of a frailty index to combine the vast array of health measures into one variable of greater complexity and utility than the simple disease count included in this paper. The full potential of the study will be realised through longitudinal study of the cohort, when health trajectories and outcomes and their associations with underlying biological, medical, and social factors will be examined to identify factors that maintain health and independence.
What is already known on this topic
Those aged 85 or older (the oldest old) are the fastest growing group in the UK and many other countries
The full spectrum of health of the oldest old, and the complex factors influencing their health trajectories, need better description to assist health care and service planning
What this study adds
Levels of self rated health and functional ability are good among 85 year olds, despite substantial levels of disease and impairment
Hypertension, ischaemic heart disease, atrial fibrillation, depression, and dementia may be underdiagnosed in 85 year olds whereas diabetes and thyroid disease are not
We thank the participants for their time and personal information; the research nurses (Brenda Balderson, Sally Barker, Julie Burrows, June Edwards, Julie Ferguson, Gill Hedley, Joan Hughes, Judith Hunt, Julie Kimber, and Victoria Raynor); the blood sample processing technicians (Sam Jameson, Claire Kolenda, Craig Parker, and Anna Tang); the data manager (Pauline Potts); the study secretary (Lucy Farfort); Newcastle and North Tyneside primary care trusts and local general practices; Newcastle and North Tyneside 1 research ethics committee; Rudi Westendorp and Jacobijn Gussekloo (Leiden University Medical Centre, the Netherlands) for sharing their experiences of the Leiden 85+ Study; and Wendy den Elzen (Leiden University Medical Centre PhD student) for assistance with preparation of the blood datasets.
Contributors: JC participated in the design and execution of the study; data collection; data preparation, analysis, and interpretation; and the development and writing of the paper. KD participated in the study design, data collection, and data preparation. CJ participated in the study design, the development and writing of the paper, and supervised the analysis. AK participated in the analysis and interpretation of data and writing of the paper. JB participated in the design and conduct of the study, analysis, and writing of the paper. MPE participated in the design and conduct of the study, analysis, and writing of the paper. LAR participated in recruitment, data collection, and writing the paper. CM-R participated in the study set-up and blood collection and blood tests. TvZ participated in the study design and data collection. OFWJ participated in the study design, data interpretation, and development and writing of the paper. TBLK conceived the study, secured funding, and oversaw all aspects as principal investigator. He participated in the design and execution of the study; data management and analysis; and the development and writing of the paper. JC and TBLK are the guarantors. All authors saw and approved the final manuscript, had full access to all of the data (including statistical reports and tables) in the study, and can take responsibility for the integrity of the data and the accuracy of the data analysis. In addition to the authors the following contributed to the Newcastle 85+ Study as members of the management team or Academic Stakeholders Group: Ashley Adamson, Fraser Birrell, John Burn, Patrick Chinnery, Mike Clarke, Daniel Collerton, Paul Corris, Chris Day, Andrew Fisher, Gary Ford, Roger Francis, Tim Goodship, John Isaacs, Bernard Keavney, Roseanne Kenny, John Mathers, Janet McComb, Ian McKeith, Simon Pearce, Robert Pickard, Brian Saxby, Therese Small, Jimmy Steele, Angus Walls, and Keith Wesnes.
Funding: The baseline phase of the Newcastle 85+ Study was supported by a combined grant from the Medical Research Council and Biotechnology and Biological Sciences Research Council (grant No G0500997) and a grant from the Newcastle Healthcare Charity. The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the paper; and in the decision to submit the paper for publication.
Competing interests: None declared.
Ethical approval: This study was approved by the Newcastle and North Tyneside 1 research ethics committee.
Data sharing: No additional data are available.
Cite this as: BMJ 2009;399:b4904
References
- 1.United Nations Department of Economic and Social Affairs Population Division. World population ageing: 1950-2050. UN, 2002. www.un.org/esa/population/publications/worldageing19502050/.
- 2.Oeppen J, Vaupel JW. Demography. Broken limits to life expectancy. Science 2002;296:1029-31. [DOI] [PubMed] [Google Scholar]
- 3.Wanless D. Securing our future health: taking a long term view. Interim report. London: HM Treasury, 2001. www.hm-treasury.gov.uk/consult_wanless_final_2001.htm.
- 4.Christensen K Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009;374:1196-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Von Faber M, Bootsma-van der Wiel A, van Exel E, Gussekloo J, Lagaay AM, van Dongen E, et al. Successful aging in the oldest old: who can be characterized as successfully aged? Arch Intern Med 2001;161:2694-700. [DOI] [PubMed] [Google Scholar]
- 6.Nybo H, Gaist D, Jeune B, McGue M, Vaupel JW, Christensen K. Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. J Am Geriatr Soc 2001;49:601-9. [DOI] [PubMed] [Google Scholar]
- 7.Pitkala KH, Valvanne J, Kulp S, Strandberg TE, Tilvis RS. Secular trends in self-reported functioning, need for assistance and attitudes towards life: 10-year differences of three older cohorts. J Am Geriatr Soc 2001;49:596-600. [DOI] [PubMed] [Google Scholar]
- 8.Seematter-Bagnoud L, Santos-Eggimann B. Population-based cohorts of the 50s and over: a summary of worldwide previous and ongoing studies for research on health in ageing. Eur J Ageing 2006;3:41-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bowling AP. Contact with general practitioners and differences in health status among people aged over 85 years. J R Coll Gen Pract 1989;39:52-5. [PMC free article] [PubMed] [Google Scholar]
- 10.Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, eds. Health, wealth and lifestyles of the older population in England. The 2002 English Longitudinal Study of Ageing. Institute for Fiscal Studies, 2003.
- 11.MRC CFAS. Cognitive function and dementia in six areas of England and Wales: the distribution of MMSE and prevalence of GMS organicity level in the MRC CFA Study. The Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Psychol Med 1998;28:319-35. [DOI] [PubMed] [Google Scholar]
- 12.Fletcher AE, Price GM, Ng ESW, Stirling SL, Bulpitt CJ, Breeze E, et al. Population-based multidimensional assessment of older people in UK general practice: a cluster-randomised factorial trial. Lancet 2004;364:1667-77. [DOI] [PubMed] [Google Scholar]
- 13.National Centre for Social Research, Department of Epidemiology and Public Health at the Royal Free and University College Medical School. Health survey for England 2005: health of older People 2005. www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england/health-survey-for-england-2005:-health-of-older-people-%5Bns%5D.
- 14.Tinker A, Askham J, Hancock R, Mueller G, Stuchbury R. 85 not out: a study of people aged 85 and over at home. Anchor Trust, 2001.
- 15.Collerton J, Barrass K, Bond J, Eccles M, Jagger C, James O, et al. The Newcastle 85+ study: biological, clinical and psychosocial factors associated with healthy ageing: study protocol. BMC Geriatrics 2007;7:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn G. Design and analysis of reliability studies: the statistical evaluation of measurement errors. Arnold, 1992:145. [DOI] [PubMed]
- 17.Parliament. Mental Capacity Act 2005: Stationery Office, 2005. www.opsi.gov.uk/ACTS/acts2005/ukpga_20050009_en_1.
- 18.Sheikh JA, Yesavage JA. Geriatric depression scale (GDS): recent findings and development of a shorter version. In: Brink TL, ed. Clinical gerontology: a guide to assessment and intervention. Haworth Press, 1986.
- 19.Molloy DW, Standish TI. A guide to the standardised mini-mental state examination. Int Psychogeriatr 1997;9(suppl 1):87-94. [DOI] [PubMed] [Google Scholar]
- 20.NHS: Information Centre for Health and Social Care. The quality and outcomes framework. QOF 2006/07 data tables, 2007. www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-2006/07/qof-2006-07-data-tables.
- 21.Office of the Deputy Prime Minister. The English indices of deprivation 2004: summary (revised). Office for the Deputy Prime Minister, 2004. www.communities.gov.uk/archived/publications/communities/indicesdeprivation.
- 22.Manjunath G, Sarnak MJ, Levey AS. Prediction equations to estimate glomerular filtration rate: an update. Curr Opin Nephrol Hypertens 2001;10:785-92. [DOI] [PubMed] [Google Scholar]
- 23.Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med 2004;141:929-37. [DOI] [PubMed] [Google Scholar]
- 24.Joosten E, Pelemans W, Hiele M, Noyen J, Verhaeghe R, Boogaerts MA. Prevalence and causes of anaemia in a geriatric hospitalized population. Gerontology 1992;38:111-7. [DOI] [PubMed] [Google Scholar]
- 25.British Medical Association, Royal Pharmaceutical Society of Great Britain. British national formulary. BMA, RPS, 2009. (No58.) www.bnf.org/bnf/.
- 26.Roberts G. Age effects and health appraisal: a meta-analysis. J Gerontol B Psychol Sci Soc Sci 1999;54:S24-30. [DOI] [PubMed] [Google Scholar]
- 27.Gold CH, Malmberg B, McClearn GE, Pedersen NL, Berg S. Gender and health: a study of older unlike-sex twins. J Gerontol B Psychol Sci Soc Sci 2002;57:S168-76. [DOI] [PubMed] [Google Scholar]
- 28.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. JNC 7 express. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: US Department of Health and Human Services, 2003. www.nhlbi.nih.gov/guidelines/hypertension/express.pdf. [DOI] [PubMed]
- 29.National Institute for Health and Clinical Excellence. Management of hypertension in adults in primary care, 2006. www.nice.org.uk/nicemedia/pdf/CG034NICEguideline.pdf.
- 30.Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887-98. [DOI] [PubMed] [Google Scholar]
- 31.Bamford C, Eccles M, Steen N, Robinson L. Can primary care record review facilitate earlier diagnosis of dementia? Fam Pract 2007;24:108-16. [DOI] [PubMed] [Google Scholar]
- 32.Roderick PJ, Atkins RJ, Smeeth L, Nitsch DM, Hubbard RB, Flectcher AE, et al. Detecting chronic kidney disease in older people; what are the implications? Age Ageing 2008;37:179-86. [DOI] [PubMed] [Google Scholar]
- 33.Lippi G, Targher G, Salvagno GL, Montagnana M, Guidi GC. Detecting of chronic kidney disease in older people by the MDRD and MCQ formulas. Age Ageing 2008;37:722. [DOI] [PubMed] [Google Scholar]
- 34.Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc 2004;52:123-7. [DOI] [PubMed] [Google Scholar]
- 35.Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol 1996;49:1407-17. [DOI] [PubMed] [Google Scholar]
- 36.Government Actuary’s Department. Interim life tables 2005-2007, 2007. www.gad.gov.uk/Demography%20Data/Life%20Tables/Interim_life_tables.html.
- 37.Government Actuary’s Department. Government Actuary’s Department population projection database, 2006. www.gad.gov.uk/Demography%20Data/Population/index.aspx.
- 38.Williamson J, Stokoe IH, Gray S, Fisher M, Smith A, McGhee A, et al. Old people at home. Their unreported needs. Lancet 1964;1:1117-20. [DOI] [PubMed] [Google Scholar]