Abstract
This article reviews progress in adapting addiction treatment to respond more fully to the chronic nature of most patients’ problems. After reviewing evidence that the natural history of addiction involves recurrent cycles of relapse and recovery, we discuss emerging approaches to recovery management, including techniques for improving the continuity of care, monitoring during periods of abstinence, and early reintervention; recent developments in the field related to self-management, mutual aid, and other recovery supports; and system-level interventions. We also address the importance of adjusting treatment funding and organizational structures to better meet the needs of individuals with a chronic disease.
Historically, addiction treatment systems and research have been organized to provide and improve the outcomes of acute episodes of care. The conceptual model has been that an addicted person seeks treatment, completes an assessment, receives treatment, and is discharged, all in a period of weeks or months. This orientation stands at variance with clinical experience and studies conducted over several decades, which confirm that, although some individuals can be successfully treated within an acute care framework, more than half the patients entering publicly funded addiction programs require multiple episodes of treatment over several years to achieve and sustain recovery (Dennis et al., 2005; Dennis, Foss, and Scott, 2007). The progress of many patients is marked by cycles of recovery, relapse, and repeated treatments, often spanning many years before eventuating in stable recovery, permanent disability, or death (Anglin et al., 2001; Anglin, Hser, and Grella, 1997; Dennis, Scott, and Funk, 2003; Hser et al., 1997, 2001; McLellan et al., 2000; Scott, Dennis, and Foss, 2005; Scott, Foss, and Dennis, 2005; Simpson, Joe, and Broome, 2002; Weisner et al., 2004; Weisner, Matzger, and Kaskutas, 2003; White, 1996).
The traditional acute care approach to drug abuse has encouraged people to suppose that patients entering addiction treatment should be cured and able to maintain lifelong abstinence following a single episode of specialized treatment. Accordingly, policymakers allocate limited public health dollars for addiction treatment; insurers restrict the number of patient days and visits covered; treatment centers make no infrastructure allowance for ongoing monitoring; and families and the public become impatient when patients relapse (McLellan et al., 2000).
The mismatch between the typical natural history of substance use disorders (SUDs) and treatment models and expectations reduces our ability to help addicted individuals. In this overview, we define SUDs, highlight their chronic features, discuss several recently developed techniques to manage SUDs over time, and present information that can help guide systems and programs in adapting to a chronic care approach to SUDs.
CHRONICITY OF SUDS
The American Psychiatric Association (APA; 2000) and World Health Organization (WHO; 1999) define addiction as a chronic, tenacious pattern of substance use and related problems; they distinguish two types of SUDs: dependence and abuse (the latter called “hazardous use” by the WHO). The definition of substance dependence implies chronicity: Symptoms—including increased tolerance for the substance, inability to abstain, replacement of healthy activities with substance use, and continued use despite medical or psychological problems—have been present for longer than 12 months and are likely to persist if left untreated. Substance abuse applies when people do not meet the dependence criteria, but report at least one moderately severe substance-related symptom that puts them at high risk for harming themselves or others and for developing dependence. Dependence requires treatment, and abuse generally results in referral to brief intervention or treatment.
A growing body of neuroimaging studies provides evidence that a physiological basis underlies the clinical experience of SUD chronicity (Fowler et al., 2007). These studies demonstrate that cravings, cue reactivity, tolerance, and withdrawal can be seen in the brain; that they interact with brain development (particularly among adolescents); that they respond to medications as well as social and physical environment; and that chronic substance use is associated with physical changes in the brain that have an impact on brain functioning and emotional states (Chang et al., 2005, 2006; Kufahl et al., 2005; Paulus, Tapert, and Schuckit, 2005; Risinger et al., 2005; Schlaepfer et al., 2006; Volkow, Fowler, and Wang, 2003, 2004).
Epidemiological Indicators of Chronicity
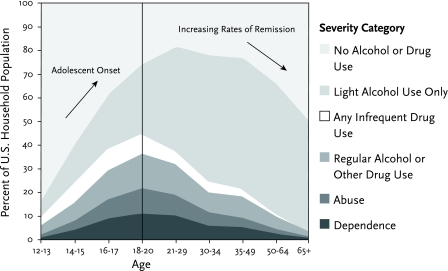
Of the 235 million people aged 12 and over in the U.S. household population in 2001, 5 percent met the criteria for substance dependence, and 4 percent met the criteria for substance abuse in the past year (Office of Applied Studies (OAS), 2002). Epidemiological data affirm that SUDs typically follow a chronic course, developing during adolescence and lasting for several decades. Some 90 percent of all individuals with dependence started using before the age of 18, and half started before the age of 15 (Dennis et al., 2002). In the U.S. population as a whole, the prevalence of dependence and abuse rises through the teen years, peaks at around 20 percent between ages 18 and 20, then declines gradually over the next four decades (Figure 1; OAS, 2002). A significant portion of older nonusers are people in recovery. In studies of community (Dawson, 1996; Kessler, 1994; Robins and Regier, 1991) and treatment (Dennis et al., 2005) populations, between 58 and 60 percent of people who met the criteria for an SUD at some time in their lives eventually achieved sustained recovery—that is, they had no dependence or abuse symptoms for the past year. Most who recover do so only after at least one episode of treatment (Cunningham, 1999a, 1999b).
FIGURE 1.
Substance Use Disorders Begin in Adolescence and Last for Decades
In the U.S. household population in 2001, the percentage of people who reported substance dependence or abuse rose through the adolescent age groups to peak among the 18-to 2o-year-olds, and declined through subsequent age groups (OAS, 2002).
People who enter treatment are a distinct subgroup of substance users whose problems are particularly severe and intractable. Among people in publicly funded addiction treatment in 2002, 62 percent met the diagnostic criteria for dependence; 16 percent met the criteria for abuse; and 22 percent were admitted for other subclinical substance-related problems (e.g., acute intoxication, mental health problems aggravated by substance use; OAS, 2005). Of people admitted to U.S. public programs in 2003, 64 percent were reentering treatment: 23 percent for the second time, 22 percent for the third or fourth time, and 19 percent for the fifth or more time (OAS, 2005). In fact, numerous longitudinal studies have shown that, on average, people reach sustained abstinence only after three to four episodes of different kinds of treatment over a number of years (Anglin, Hser, and Grella, 1997; Dennis et al., 2005; Grella and Joshi, 1999; Hser et al., 1997, 1998; Scott, Dennis, and Foss, 2005; Scott, Foss, and Dennis, 2005). In one longitudinal study with 1,271 patients, the estimated median time from first use to at least 1 drug-free year was 27 years, and the median time from first treatment to 1 alcohol- and drug-free year was 9 years with three to four episodes of treatment (Dennis et al., 2005).
In sum, most patients in publicly funded addiction treatment have SUDs and require multiple treatment episodes over several years to reach stable recovery. For optimal outcomes, treatment systems and interventions should be able to address the long-term aspects and cyclical dynamics of the disorder.
Inside the Cycles of Recovery and Relapse
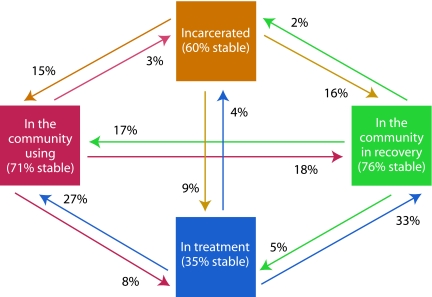
In a recent study, Scott and colleagues provided insight into the factors influencing 448 patients’ transitions between relapse, treatment reentry, incarceration, and recovery (Scott, Dennis, and Foss, 2005). Over 2 years of monitoring, 82 percent transitioned at least once, and 62 percent moved multiple times (Figure 2). In an average quarter, 32 percent of the patients moved from one status to another.
FIGURE 2.
The Pathway to Recovery Is Cyclical
Over a 2-year period, 82 percent of drug users transitioned one or more times between use, incarceration, treatment, and recovery. An average of 32 percent changed every 90 days, with movement in every direction and treatment increasing the likelihood of getting to recovery (Scott, Foss, and Dennis, 2005).
Several variables predicted the transitions. Patients with higher substance use severity and environmental obstacles to recovery—for example, substance use in the home, family problems, and victimization—were less likely to transition from drug use to recovery or treatment (i.e., the individuals most in need of treatment were the least likely to re-enroll on their own). Patients were more likely to transition from use to recovery when they believed their problems could be solved, desired help with their problems, reported high self-efficacy to resist substance use, and received addiction treatment during the quarter.
Scott and colleagues conducted a second study, this time with 1,326 adult patients over a 3-year period, that looked at annual transitions (Scott, Foss, and Dennis, 2005). More than 83 percent of the participants transitioned from one point in the cycle to another during the 3 years (including 36 percent who transitioned twice and 14 percent who transitioned three times). Treatment participation was again a primary correlate of the transition from use to recovery. The odds ratio of transitioning from use to recovery went up 1.14 for every 9 weeks of treatment received during the year. Among patients who started the year in recovery, the major predictor of whether they maintained abstinence was not treatment, but their level of self-help group participation. The odds ratio of relapse went down 0.55 for every 77 days of self-help group attendance.
Factors Affecting the Duration of SUDs
The age at first substance use and the duration of use before starting treatment are related to the length of time it takes people to reach at least 1 year of alcohol and drug abstinence. Scott and colleagues found that the median time of use was significantly longer for people who started before age 15 than for those who started after age 20 (29 vs. 18 years; Scott, Dennis, and Foss, 2005). Patients who began treatment within 10 years of their initial drug use achieved a year or more of abstinence after an average of 15 years, compared with 35 or more years among those who entered treatment after 20 or more years of use. These results clearly establish the need to diagnose and intervene as early as possible, ideally during the first decade of use.
The Impact of Co-Occurring Problems
As clinicians and researchers are aware, individuals with SUDs have high rates of additional health and social burdens that increase the difficulty of treatment: psychiatric problems, HIV risk behaviors, violence, illegal activity and involvement in the criminal justice system, service utilization, homelessness, and a wide range of vocational problems (Center for Substance Abuse Treatment, 2000; Compton, Lamb, and Fletcher, 1995; Epstein, 2002; Grant, 2000; Hasin et al., 1997a, 1997b, Jaffe, 1993; Kessler et al., 1996; Langenbucher, Morgenstern, and Miller, 1995; Lennox, Scott-Lennox, and Bohlig, 1993; Lennox, Scott-Lennox, and Holder, 1992; Lennox, Zarkin, and Bray, 1996; Mark et al., 2001; Regier et al., 1990; Woody, Cottler, and Cacciola, 1993). Patients who abuse multiple substances or have other co-occurring problems are more likely to experience difficulties with treatment/medication adherence, shorter stays, administrative discharges, compromised functional status, difficult community adjustment, reduced quality of life, and worse outcomes (e.g., Brooner et al., 1997; Ford, Snowden, and Walser, 1991; Hien et al., 1997; McLellan et al., 1983; Mueser et al., 1990; Project MATCH Research Group, 1997; Ross, Glaser, and Germanson, 1988; Rounsaville et al., 1982, 1986; Weisner, Matzger, and Kaskutas, 2003; White et al., 2005). Clinical trials have demonstrated that when patients have an SUD combined with one or more non-substance-related disorders, it can be more effective—in terms of both clinical outcome and cost—to provide integrated care (Parthasarathy et al., 2003; Willenbring, 2005).
EMERGING APPROACHES TO RECOVERY MANAGEMENT
Recently, clinicians and researchers have generated several new approaches to improve the long-term management of an SUD by responding to its chronic nature. Underlying the approaches are three strategies:
Improve the continuity of care;
Use monitoring and early reintervention; and
Provide other recovery support.
Improving Continuity of Care
During the years- or decades-long course of an SUD, patients need varying levels of care. In periods of intensified symptoms, a patient may be able to cope best by retreating from the community to a specialized inpatient or intensive outpatient setting. Conversely, reentry into the community at the conclusion of an intensive treatment episode marks the beginning of a new state of risk related to continuing biobehavioral vulnerability and environmental exposures.
Accordingly, the APA (1995), the American Society of Addiction Medicine (2001), and the Department of Veterans Affairs Office of Quality and Performance (www.oqp.med.va.gov/cpg/SUD/SUD_Base.htm) have issued clinical practice guidelines recommending that patients being discharged from intensive levels of addiction treatment be transferred to outpatient treatment for a period of time before leaving the addiction treatment system. A number of studies demonstrate that this practice promotes continuation of abstinence and reduces the likelihood of arrest (e.g., Brown et al., 1994; Donovan, 1998; Gilbert, 1988; Godley et al., 2007; Higgins, Badger, and Budney, 2000; Ito and Donovan, 1986; Kosten et al., 1992; McKay, 2001; McKay et al., 1998; Moos et al., 2001; Moos and Moos, 2003; Ouimette, Moos, and Finney, 1998; Peterson et al., 1994; Ritsher et al., 2002; Ritsher, Moos, and Finney, 2002; Sannibale et al., 2003; Walker et al., 1983). Also, in one of the few economic evaluations of long-term management of chronic SUDs, French and colleagues (2000) found that while the outlay to provide a full continuum of inpatient and outpatient care was greater than that for outpatient treatment alone ($2,530 vs. $1,138; p< 0.05), the cost differential was offset by significantly greater reductions in societal costs over the subsequent 9 months (savings of $17,833 vs. $11,173; p< 0.05).
Despite the benefits associated with continuing care, a study of discharge patterns in 23 states and jurisdictions showed that although 58 percent of patients successfully completed detoxification, hospital, residential treatment, or intensive outpatient programs, only about 17 percent of these individuals proceeded to regular outpatient care (OAS, 2005). Studies focusing on single correctional, drug court, residential, intensive outpatient, and detoxification programs have found, similarly, that 25 to 90 percent of discharged individuals do not successfully access the recommended outpatient continuing care (Godley et al., 2002; Godley, Godley, and Dennis, 2001; Mark et al., 2003; McCorry et al., 2000; McKay et al., 2002; OAS, 2005; Taxman, 2002). Common reasons for low success rates in bridging patients into continuing care include relying on patients’ self-motivation to follow through with discharge recommendations, discharging patients to geographically large catchment areas (particularly from criminal/juvenile justice and adolescent residential programs) where followup services are not easily accessed, and passively linking patients to other organizations or staff without proactive efforts to ensure continuity of care.
Recent studies have evaluated new and more assiduous protocols to improve participation in continuing care (Ciliska et al., 1996; Godley et al., 2002, 2007; McKay et al., 2004; Simon et al., 2004; Slesnick and Prestopnik, 2004; Zhu et al., 1996). As an example, McKay and colleagues (2004, 2005) demonstrated benefits with telephone-based continuing care. The researchers randomly assigned 359 alcohol- or cocaine-dependent adults who had completed a 4-week intensive outpatient program to one of three continuing care protocols: (a) twice weekly standard outpatient treatment for 12 weeks; (b) twice weekly relapse prevention group therapy for 12 weeks; or (c) 4 weeks of relapse prevention group therapy and 12 weeks of therapist-initiated telephone contact. Over the course of the study, the participants who were telephoned had significantly fewer positive cocaine urine tests than those in group b (odds ratio 0.80) or group a (odds ratio 0.26). The results also suggest that telephone delivery of continuing care may be most effective for persons whose SUD is less severe; participants with high dependence levels or co-occurring disorders benefited slightly less than others.
Godley and colleagues (2002, 2004, 2007) developed a protocol called assertive continuing care (ACC) and showed that it improved participation and recovery indicators. Researchers randomly assigned 183 adolescents in residential treatment to either ACC or usual continuing care (UCC). Adolescents in the ACC group worked with a case manager who tried to meet with them once before discharge. Subsequently, the case managers provided in-home outpatient treatment and helped negotiate additional treatment services, school support, probation, and other services to support recovery. All the adolescents in both intervention groups were referred to local outpatient treatment programs and self-help groups, and were given continuing care plans. Over the 90 days following discharge, those who received ACC:
Were more likely than those given UCC to access at least some continuing care services (94 vs. 54 percent);
Received more days of continuing care sessions (median 14.1 vs. 6.3);
Were more likely to engage in 7 or more of 12 activities associated with sustaining abstinence (e.g., self-help, urine testing, relapse prevention work; 64 vs. 35 percent); and
Were more likely to remain abstinent 1 to 3 months after discharge from residential treatment (43 vs. 24 percent),
Which was, in turn, predictive of abstinence 4 to 9 months after discharge (69 vs. 19 percent).
The research team is currently exploring whether contingency contracting can further improve continuing care participation and related outcomes and whether ACC can improve outcomes following outpatient treatment.
On a broader scale, various groups have suggested using performance measurement to improve continuity of care (e.g., Garnick et al., 2002; McCorry et al., 2000; McLellan et al., 2005; www.ncqa.org; www.washingtoncircle.org). One of the largest such initiatives, the Network for the Improvement of Addiction Treatment (NIATx), is a partnership among the Center for Substance Abuse Treatment, the Robert Wood Johnson Foundation, and a number of independent addiction treatment organizations (Capoccia et al., 2007; McCarty et al., 2007; Wisdom et al., 2006). The NIATx mission is to improve the efficiency with which the treatment field uses its capacity and to encourage ongoing improvements in treatment access and retention. NIATx assumes that addiction is a chronic and progressive condition and that interruptions and delays in the continuity of care can seriously exacerbate consequences. Using a process-improvement model, the first 13 NIATx programs were able to reduce the time from an individual’s first contact to treatment entry by 37 percent, and from the first assessment to first treatment episode by 33 percent. They also improved the rate of returning for the second treatment session by 18 percent and the likelihood of staying four or more sessions by 11 percent (McCarty et al., 2007).
Monitoring and Early Reintervention
Ongoing monitoring and early reintervention have improved long-term outcomes for a range of chronic conditions, including asthma, cancer, diabetes, depression, and severe mental illness (Dunbar-Jacob et al., 1995; Engel, 1977, 1980; Huber, 2005; Institute of Medicine, 2001; McLellan et al., 2005; Nicassio and Smith, 1995; Roter et al., 1998; Weisner et al., 2004). Applying this approach to SUDs, Scott and Dennis (2003) developed and tested the recovery management checkup (RMC). With RMC, treatment staff members do not rely on patients to recognize that they need help but instead conduct quarterly checkups to assess patient status. Staff members use motivational interviewing techniques to assist those who have relapsed to resolve their ambivalence about their substance use and commit to treatment or other appropriate care. Staff members also deploy assertive treatment linkage, engagement, and retention protocols to secure patient access to treatment and increase the amount of therapy received.
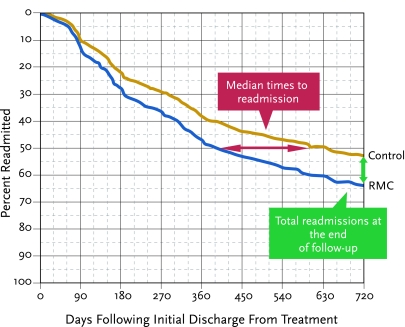
The initial clinical trial of RMC randomly assigned 448 adults, when they first presented for treatment, to post-treatment followup with the checkup intervention or only quarterly monitoring (Figure 3; Dennis, Scott, and Funk, 2003; Scott, Dennis, and Foss, 2005). At the end of 2 years of followup, the results showed that patients in the RMC group:
FIGURE 3.
Time to Readmission to Treatment by Condition.
In the 24 months following discharge from an index episode of care, the rate of readmission was higher (64% versus 51%) and the median time to readmission was shorter (376 vs. 600 days) among patients who the received recovery management checkup intervention, compared to controls. [Adapted from Dennis, Scott, and Funk, 2003; with permission from Elsevier.]
Returned to treatment in greater numbers (60 vs. 51 percent)
Returned to treatment sooner (median 376 vs. 600 days)
Attended treatment on more days (average 63 vs. 40)
Were less likely to be in need of treatment after 2 years (34 vs. 44 percent).
A second clinical trial, with 446 patients, used a modified RMC protocol and produced parallel findings. These two trials indicate that ongoing monitoring and early reintervention can promote positive patient behaviors in long-term substance use.
Other Recovery Support Initiatives
Individuals with an SUD, like those with other chronic conditions, require a variety of support services to help manage their condition during and between episodes of formal treatment. Research demonstrates that active participation in self-help groups during and after treatment promotes lengthier periods of recovery (Brown, 1993; Hsieh, Hoffman, and Hollister, 1998; Humphreys and Moos, 2001; Kyrouz, Humphreys, and Loomis, 2002; McKay et al., 2002; Ritsher et al., 2002; Scott, Dennis, and Foss, 2005). Preliminary evidence also suggests that self-help participation is associated with better outcomes when patients join groups that focus on their particular issues, such as dual diagnoses (Laudet et al., 2000) or adolescent issues (Finch, 2005; Kelly and Myers, 1997; Kelly, Myers, and Brown 2002; White and Finch, 2006). Other recently tested recovery support approaches include telephone-based self-monitoring (Simpson et al., 2005) and Internet-based groups (Klaw, Huebsch, and Humphreys, 2000; Kypri et al., 2005; Toll et al., 2003). A meta-analysis of 24 studies involving 3,739 participants with chronic health conditions (other than SUDs) suggests that Internet-based interventions that allow interactions between patients and staff have a significantly higher impact than sites providing information only (Murray et al., 2004).
Connecticut and other states have begun to add recovery-based performance measures, values, and continuity of care between professional and “peer-based recovery supports” to their recovery initiatives (www.dmhas.state.ct.us/recovery.htm). Similarly, in 2003, the Arizona Department of Health Services embarked on a unique initiative designed to develop a “peer workforce” for persons with SUDs (azdhs.gov/bhs/bhsglance.pdf). Public health systems that provide addiction, mental health, child welfare, and other services in Connecticut, Arizona, and other jurisdictions target key subgroups of people with SUDs to interrupt the cycle of relapse, treatment reentry, and recovery. For example, parents with SUDs can access standardized screening, colocated services, intensive case managers, or recovery coaches to facilitate long-term treatment engagement (e.g., Loveland and Boyle, 2005; Ryan, Louderman, and Testa, 2003).
IMPLICATIONS FOR PRACTICE
Whether a program implements one of the approaches we have described or others yet to be developed, the literature suggests that programs should take their resources and capacities into account when choosing which empirically proven efficacious programs to implement to improve care. Lipsey and colleagues (2001), in a meta-analysis, demonstrated that the thoroughness of implementation can markedly affect the efficacy of evidence-based interventions. The researchers recommended that programs implement the most efficacious program they can implement well, because a highly efficacious program will not yield any better results for patients if it is implemented poorly. Such findings have led the National Institutes of Health to emphasize the need to improve the state of “implementation science” (e.g., grants.nih.gov/grants/guide/pa-files/PAR-06-039.html). Based on a recent review of the implementation science literature, Fixsen and colleagues (2005) suggested that efforts to implement new approaches should generally include implementation strategies at multiple levels, including but not limited to Federal, state, and local stakeholders, and staff across all levels of the provider organizations.
Shifting from an acute care to a chronic care model of recovery has implications for addiction programs, as well as for external stakeholders in those programs, and proper implementation of a chronic care model is crucial to its efficacy.
Organizational Support for a Chronic Care Approach
The philosophical, financial, clinical, and practical implications of moving to a chronic care approach will touch everyone in an addiction treatment organization—its board of directors, management, clinical supervisors and line staff, administrative supports, and clients. Consider what is required, for example, to respond appropriately when a person returns for his or her fourth episode of care: intake and admission procedures must be streamlined to facilitate rapid interruption of crises or relapses; patient and staff assumptions that multiple treatments represent failure must give way to attitudes more aligned with the standards we apply to treating other chronic conditions that need long-term management; and the funding structure will need to provide the necessary financial support.
In addition, as we learn more about the factors that influence patients’ progress in different phases of recovery, we will likely need greater resources and infrastructure to organize this information so that it can support real-time clinical decision making. It may be necessary to modify assessment and other record systems to transfer information readily when patients move between levels of care and to make them accessible to multiple staff on the treatment team. Addressing such issues is likely to be critical for improving the management of SUDs.
Even when staff members favor the change to a chronic care model, they may not have adequate training, education, experience, or resources to address the needs of a particular client comprehensively—ranging, for example, from making psychiatric referrals to helping with housing. Miller and colleagues (2006) suggest that programs need to equip staff with three types of infrastructure before change can happen efficiently:
Preparatory knowledge, which may be inculcated through reading, verbal instruction, or observing competent practice by others;
Practice with feedback—of note, early practice during or right after training without feedback can rein-force bad habits and do as much harm as good; and
Ongoing coaching or supervision, which is essential, because practice will inevitably bring up a wide range of situations and complex scenarios not covered in the basic materials or training.
Even experienced clinicians benefit from opportunities to brainstorm with staff colleagues on ways to handle a new situation or adapt a protocol when necessary. When Miller and colleagues (2004) randomized 140 counselors to a wait list condition or four training conditions (workshop, workshop + practice feedback, workshop + coaching, workshop + feedback + coaching), all training conditions improved knowledge and proficiency, but actual practice changed only when both feedback and coaching were provided. Although this particular study focused on a specific intervention, these three components will likely be important factors when implementing many key changes necessary to move toward a chronic-care model.
Federal, State, and Local Stakeholders
Public payers, government regulators, and accrediting bodies set requirements and impose limits on what publicly funded treatment providers can accomplish in terms of adopting a chronic-care approach to treating SUDs. More than three-quarters of the people accessing addiction treatment receive some kind of public assistance (Substance Abuse and Mental Health Services Administration, 2006); this makes public fund providers the primary purchasers of services and gives them a unique ability to reshape existing structures and policies. As one example of the constructive use of this power, McLellan (2006) recently reported preliminary data from Delaware demonstrating that offering treatment providers performance-based incentives can improve the system of care. The data showed that retention rates from 2002 to 2004 increased 30 days (48 to 69 percent) and 60 days (25 to 42 percent) after admission. The State of Massachusetts implements a continuum of care based on the chronic disease model for its prevention and treatment systems (www.mass.gov/dph/bsas/sa_strategic_plan.ppt). In an attempt to more effectively address the chronic aspects of addiction, Connecticut is reviewing and modifying its regulations, services, and training to focus more on recovery values, recovery-based performance measures, and continuity of care between professional and “peer-based recovery” supports (www.dmhas.state.ct.us/recovery.htm). Although these and other efforts across the United States are encouraging first steps in the change process, adopting a chronic-care approach will require buy-in and active participation from all concerned with reducing the health and social consequences of drug abuse and addiction.
NEXT STEPS
Recent studies suggest some initial approaches to chronic care management. However, the field would benefit from research that investigates (1) the costs of ongoing monitoring and early reintervention; (2) the chronic care model in different populations (e.g., pregnant and postpartum women, offenders leaving prison, and adolescents); (3) the point at which an individual’s recovery history and status warrant transition from quarterly to biannual checkups; (4) the usefulness of more frequent or even continuous monitoring in improving outcomes; (5) the impact of less formal types of care (e.g., recovery coaches or faith-based interventions); (6) modes of service delivery such as telephone and e-mail; and (7) the indirect effects of recovery management on other outcomes such as HIV infection, illegal activity, emotional problems, vocational activity, and quality of life.
This information can help individuals and their families, and treatment staff recognize that addiction is a chronic but treatable condition, that most people with SUDs need help from several sources, that recovery often takes multiple episodes of treatment, and that relapse is common. However, staff members should encourage clients with SUDs and their families by stating that the majority of people do succeed and the likelihood of reaching recovery status is related to continuing care and ongoing recovery support. When relapse occurs, staff should explain the chronic nature of the condition, proactively refer those in relapse to continuing care and other services, and work with patients to ensure that they follow through with recommendations for continuing care, for self-help group meetings, for ongoing urine monitoring, and for services to address other problems.
CONCLUSION
Historically, addiction treatment has been conceptualized as an episodic relationship in which a person seeks treatment, receives an assessment, and then is treated and presumed cured—all in a relatively short time period. Although the field faces numerous challenges in its attempts to manage chronic SUDs more effectively, this review demonstrates that we are making progress. Indeed, it has been argued that addiction treatments appear to be as effective as interventions available for other chronic conditions such as diabetes and hypertension (McLellan et al., 2000). The growing body of empirical evidence demonstrating the chronicity of SUDs, coupled with increasing awareness among various stakeholders about the need for change, represents genuine progress. Formal and informal efforts to address the problems continue to expand; it is hoped that this enhanced awareness will lead to increased dialogue and action among the numerous stakeholders to improve the treatment and long-term management of chronic SUDs.
ACKNOWLEDGMENTS
This work was supported by NIDA grants R37 DA 11323 and R01 DA 15523. The authors would like to thank Joan Unsicker, Stephanie Guetschow, David Anderson, and Eric Sarlin for their assistance in preparing and editing the manuscript, and Ya-Fen Chan, Mark Godley, Susan Godley, Laverne Stevens, Bill White, and several anonymous reviewers for their thoughtful comments. The opinions are those of the authors and do not reflect official positions of the government.
REFERENCES
- American Psychiatric Association. Practice Guidelines for the Treatment of Patients with Substance Use Disorders: Alcohol, Cocaine, Opioids. Washington, DC: American Psychiatric Association; 1995. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. Text Revision, DSM-IV-TR. [Google Scholar]
- American Society of Addiction Medicine. Patient Placement Criteria for the Treatment of Substance-Related Disorders. 2d ed. Chevy Chase, MD: American Society of Addiction Medicine; 2001. [Google Scholar]
- Anglin MD, et al. Drug treatment careers: Conceptual overview and clinical, research, and policy applications. In: Tims F, Leukefeld C, Platt J, editors. Relapse and Recovery in Addictions. New Haven, CT: Yale University Press; 2001. pp. 18–39. [Google Scholar]
- Anglin MD, Hser YI, Grella CE. Drug addiction and treatment careers among clients in the Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive Behaviors. 1997;11(4):308–323. [Google Scholar]
- Brooner RK, et al. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Archives of General Psychiatry. 1997;54(1):71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Brown SA. Recovery patterns in adolescent substance abuse. In: Baer JS, Marlatt GA, McMahon J, editors. Addictive Behaviors Across the Life Span: Prevention, Treatment, and Policy Issues. Newbury Park, CA: Sage; 1993. pp. 161–183. [Google Scholar]
- Brown SA, et al. Correlates of success following treatment for adolescent substance abuse. Applied and Preventive Psychology. 1994;3(2):61–73. [Google Scholar]
- Capoccia VA, et al. Making “stone soup”: Improvement in clinic access and retention in addiction treatment. Joint Commission journal on Quality and Patient Safety. 2007;33(2):95–103. doi: 10.1016/s1553-7250(07)33011-0. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Changing the Conversation: The National Treatment Plan Initiative. Rockville, MD: Department of Health and Human Services; 2000. [Google Scholar]
- Chang L, et al. Additive effects of HIV and chronic methamphetamine use on brain metabolite abnormalities. American journal of Psychiatry. 2005;162(2):361–369. doi: 10.1176/appi.ajp.162.2.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L, et al. Combined and independent effects of chronic marijuana use and HIV on brain metabolites. Journal of Neuroimmune Pharmacology. 2006;1(1):65–76. doi: 10.1007/s11481-005-9005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciliska D, et al. A systematic overview of the effectiveness of home visiting as a delivery strategy for public health nursing interventions. Canadian Journal of Public Health. 1996;87(3):193–198. [PubMed] [Google Scholar]
- Compton WM, Lamb RJ, Fletcher BW. Results of the NIDA treatment demonstration grants’ cocaine workgroup: Characteristics of cocaine users and HIV risk behaviors. Drug and Alcohol Dependence. 1995;37(1):1–6. doi: 10.1016/0376-8716(94)01061-o. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. Resolving alcohol-related problems with and without treatment: The effects of different problem criteria. Journal of Studies on Alcohol. 1999a;60(4):463–466. doi: 10.15288/jsa.1999.60.463. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. Untreated remissions from drug use: The predominant pathway. Addictive Behaviors. 1999b;24(2):267–270. doi: 10.1016/s0306-4603(98)00045-8. [DOI] [PubMed] [Google Scholar]
- Dawson D. Gender differences in the risk of alcohol dependence: United States, 1992. Addiction. 1996;91(12):1831–1842. [PubMed] [Google Scholar]
- Dennis ML, et al. Changing the focus: The case for recognizing and treating cannabis use disorders. Addiction. 2002;97(Suppl 1):4–15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, et al. The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment. 2005;28(Suppl 1):S51–S62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Foss MA, Scott CK. An 8-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Evaluation Review. 2007;31(6):585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26(3):339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan DM. Continuing care: Promoting the maintenance of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. 2d ed. New York: Plenum; 1998. pp. 317–336. [Google Scholar]
- Dunbar-Jacob J, Burke LE, Puczynski S. Clinical assessment and management of adherence to medical regimens. In: Nicassio PM, Smith TW, editors. Managing Chronic Illness: A Biopsychosocial Perspective. Washington, DC: American Psychological Association; 1995. [Google Scholar]
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Engel GL. The clinical application of the biopsychosocial model. American Journal of Psychiatry. 1980;137(5):535–544. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- Epstein JF. Substance Dependence, Abuse and Treatment: Findings from the 2000 National Household Survey on Drug Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2002. DHHS Publication No. SMA 02–3642. [Google Scholar]
- Finch AJ. Starting a Recovery School with CEH Test Hazelden Professional Library: A How to Manual. Center City, MN: Hazelden Foundation; 2005. [Google Scholar]
- Fixsen DL, et al. Louis de la Parte Florida Mental Health Institute, National Implementation Research Network (FMHI Publication No. 231) Tampa, FL: University of South Florida; nirn.fmhi.usfp.edu/resources/publications/Monograph/; 2005. Implementation research: A synthesis of the literature. [Google Scholar]
- Ford L, Snowden LR, Walser EJ. Outpatient mental health and the dual-diagnosis patient: Utilization of services and community adjustment. Evaluation and Program Planning. 1991;14(4):291–298. [Google Scholar]
- Fowler JS, et al. Imaging the addicted human brain. Science & Practice Perspectives. 2007;3(2):4–16. doi: 10.1151/spp07324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French MT, et al. Benefit-cost analysis of residential and outpatient addiction treatment in the state of Washington. Evaluation Review. 2000;24(6):609–634. doi: 10.1177/0193841X0002400603. [DOI] [PubMed] [Google Scholar]
- Garnick DW, et al. Establishing the feasibility of performance measures for alcohol and other drugs. Journal of Substance Abuse Treatment. 2002;23(4):375–385. doi: 10.1016/s0740-5472(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Gilbert FS. The effect of type of aftercare follow-up on treatment outcome among alcoholics. Journal of Studies on Alcohol. 1988;49(2):149–159. doi: 10.15288/jsa.1988.49.149. [DOI] [PubMed] [Google Scholar]
- Godley MD, et al. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. Journal of Substance Abuse Treatment. 2002;23(1):21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- Godley MD, et al. Findings from the assertive continuing care experiment with adolescents with substance use disorders. In: Dewey W, editor. Problems of Drug Dependence, 2003: Proceedings of the 65th Annual Scientific Meeting, The College on Problems of Drug Dependence, Inc. NIDA Research Monograph Series No. 184; Rockville, MD: National Institute on Drug Abuse; 2004. pp. 123–124. [Google Scholar]
- Godley MD, et al. The effect of assertive continuing care (ACC) on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102(1):81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Godley SH, Godley MD, Dennis ML. The assertive aftercare protocol for adolescent substance abusers. In: Wagner E, Waldron H, editors. Innovations in Adolescent Substance Abuse Interventions. New York: Elsevier; 2001. pp. 311–329. [Google Scholar]
- Grant BF. Theoretical and observed subtypes of DSM-IV alcohol abuse and dependence in a general population sample. Drug and Alcohol Dependence. 2000;60(3):287–293. doi: 10.1016/s0376-8716(00)00115-0. [DOI] [PubMed] [Google Scholar]
- Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the National Drug Abuse Treatment Outcome Study. American Journal of Drug and Alcohol Abuse. 1999;25(3):385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- Hasin DS, et al. Alcohol dependence and abuse diagnoses: Validity in community sample heavy drinkers. Alcoholism: Clinical and Experimental Research. 1997a;21(2):213–219. [PubMed] [Google Scholar]
- Hasin DS, et al. Differentiating DSM-IV alcohol dependence and abuse by course: Community heavy drinkers. Journal of Substance Abuse. 1997b;9:127–135. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Hien D, et al. Dual diagnosis subtypes in urban substance abuse and mental health clinics. Psychiatric Services. 1997;48(8):1058–1063. doi: 10.1176/ps.48.8.1058. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Experimental and Clinical Psychopharmacology. 2000;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Hser YI. Drug treatment careers: A conceptual framework and existing research findings. Journal of Substance Abuse Treatment. 1997;14(6):543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- Hser YI, et al. Relationships between drug treatment careers and outcomes: Findings from the National Drug Abuse Treatment Outcome Study. Evaluation Review. 1998;22(4):496–519. [Google Scholar]
- Hser YI, et al. A 33-year follow-up of narcotics addicts. Archives of General Psychiatry. 2001;58(5):503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Hsieh S, Hoffman NG, Hollister CD. The relationship between pre-, during-, post-treatment factors, and adolescent substance abuse behaviors. Addictive Behaviors. 1998;23(4):477–488. doi: 10.1016/s0306-4603(98)00028-8. [DOI] [PubMed] [Google Scholar]
- Huber DL. Disease Management: A Guide for Case Managers. Amsterdam: Elsevier; 2005. [Google Scholar]
- Humphreys K, Moos R. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcoholism: Clinical and Experimental Research. 2001;25(5):711–716. [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Ito J, Donovan DM. Aftercare in alcoholism treatment: A review. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Process of Change. New York: Plenum; 1986. pp. 435–452. [Google Scholar]
- Jaffe J. The concept of dependence: Historical reflections. Alcohol Health and Research World. 1993;17(3):188–189. [Google Scholar]
- Kelly JF, Myers MG. Adolescent treatment outcome in relation to 12-step group attendance. Alcoholism: Clinical and Experimental Research. 1997;21:27A. [Google Scholar]
- Kelly JF, Myers MG, Brown SA. Do adolescents affiliate with 12-step groups? A multivariate process model of effects. Journal of Studies on Alcohol. 2002;63(3):293–304. doi: 10.15288/jsa.2002.63.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. The National Comorbidity Survey of the United States. International Review of Psychiatry. 1994;6:365–376. [Google Scholar]
- Kessler RC, et al. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry. 1996;66(1):17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Klaw E, Huebsch PD, Humphreys K. Communication patterns in an on-line mutual help group for problem drinkers. Journal of Community Psychology. 2000;28(5):535–546. [Google Scholar]
- Kosten TR, et al. Six-month follow-up of short-term pharmacotherapy for cocaine dependence. American Journal of Addictions. 1992;1:40–49. [Google Scholar]
- Kufahl PR, et al. Neural responses to acute cocaine administration in the human brain detected by fMRI. Neuroimage. 2005;28(4):904–914. doi: 10.1016/j.neuroimage.2005.06.039. [DOI] [PubMed] [Google Scholar]
- Kypri K, et al. Innovative approaches to intervention for problem drinking. Current Opinion in Psychiatry. 2005;18(3):229–234. doi: 10.1097/01.yco.0000165591.75681.ab. [DOI] [PubMed] [Google Scholar]
- Kyrouz EM, Humphreys K, Loomis C. A review of research on the effectiveness of self-help mutual aid groups. In: White BJ, Madara EJ, editors. American Self-Help Clearinghouse Self-Help Group Sourcebook. 7th ed. Cedar Knolls, NJ: American Self-Help Clearinghouse; 2002. pp. 1–16. [Google Scholar]
- Langenbucher JW, Morgenstern J, Miller KJ. DSM-III, DSM-IV and ICD-10 as severity scales for drug dependence. Drug and Alcohol Dependence. 1995;39(2):139–150. doi: 10.1016/0376-8716(95)01152-o. [DOI] [PubMed] [Google Scholar]
- Laudet AB, et al. Support, mutual aid and recovery from dual diagnosis. Community Mental Health Journal. 2000;36(5):457–476. doi: 10.1023/a:1001982829359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennox RD, Scott-Lennox JA, Bohlig EM. The cost of depression-complicated alcoholism: Health-care utilization and treatment effectiveness. Journal of Mental Health Administration. 1993;20(2):138–152. doi: 10.1007/BF02519238. [DOI] [PubMed] [Google Scholar]
- Lennox RD, Scott-Lennox JA, Holder HD. Substance abuse and family illness: Evidence from health care utilization and cost-offset research. Journal of Mental Health Administration. 1992;19(1):83–95. doi: 10.1007/BF02521310. [DOI] [PubMed] [Google Scholar]
- Lennox RD, Zarkin GA, Bray JW. Latent variable models of alcohol-related constructs. Journal of Substance Abuse. 1996;8(2):241–250. doi: 10.1016/s0899-3289(96)90282-5. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Chapman GL, Landenberger NA. Cognitive-behavioral programs for offenders. Annals of the American Academy of Political and Social Science. 2001;578(1):144–157. [Google Scholar]
- Loveland D, Boyle M. Behavioral Health Recovery Management Clinical Guidelines. Peoria, IL: Fayette Companies; 2005. Recovery Coach and Recovery Planning Manual. www.bhrm.org/guidelines/addguidelines.htm. [Google Scholar]
- Mark TL, et al. The economic costs of heroin addiction in the United States. Drug and Alcohol Dependence. 2001;61(2):195–206. doi: 10.1016/s0376-8716(00)00162-9. [DOI] [PubMed] [Google Scholar]
- Mark TL, et al. Factors associated with the receipt of treatment following detoxification. Journal of Substance Abuse Treatment. 2003;24(4):299–304. doi: 10.1016/s0740-5472(03)00039-4. [DOI] [PubMed] [Google Scholar]
- McCarty D, et al. The Network for the Improvement of Addiction Treatment (NIATx): Enhancing access and retention. Drug and Alcohol Dependence. 2007;88(2–3):138–145. doi: 10.1016/j.drugalcdep.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCorry F, et al. Developing performance measures for alcohol and other drug services in managed care plans. Journal on Quality Improvement. 2000;26(11):633–643. doi: 10.1016/s1070-3241(00)26054-9. [DOI] [PubMed] [Google Scholar]
- McKay JR. Recent developments in alcoholism: The role of continuing care in outpatient alcohol treatment programs. In: Galanter M, editor. Services Research in the Era of Managed Care. Vol. 15. New York: Plenum; 2001. pp. 357–372. [DOI] [PubMed] [Google Scholar]
- McKay JR, et al. Predictors of participation in aftercare sessions and self-help groups following completion of intensive outpatient treatment for substance abuse. Journal of Studies on Alcohol. 1998;59(2):152–162. doi: 10.15288/jsa.1998.59.152. [DOI] [PubMed] [Google Scholar]
- McKay JR, et al. Evaluation of full versus partial continuum of care in the treatment of publicly funded substance abusers in Washington State. American Journal of Drug and Alcohol Abuse. 2002;28(2):307–338. doi: 10.1081/ada-120002976. [DOI] [PubMed] [Google Scholar]
- McKay JR, et al. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology. 2004;72(6):967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McKay JR, et al. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Archives of General Psychiatry. 2005;62(2):199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Research…for a Change: Impact Through Customer-Oriented Research. Slides presented at the Blending Addiction Science & Practice: Bridges to the Future conference; Seattle, WA. October 16–17; 2006. www.sei2003.com/blendingseattle/tue_pdfs/Tuesday_Plenary_McLellan.pdf. [Google Scholar]
- McLellan AT, et al. Predicting response to alcohol and drug abuse treatments: Role of psychiatric severity. Archives of General Psychiatry. 1983;40(6):620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- McLellan AT, et al. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, et al. Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, et al. A randomized trial of methods to help clinicians learn motivational interviewing. Journal of Consulting and Clinical Psychology. 2004;72(6):1050–1062. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- Miller WR, et al. Disseminating evidence-based practices in substance abuse treatment: A review with suggestions. Journal of Substance Abuse Treatment. 2006;31(1):25–39. doi: 10.1016/j.jsat.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Moos R, et al. Outpatient mental health care, self-help groups, and patients’ one-year treatment outcomes. Journal of Clinical Psychology. 2001;57(3):273–287. doi: 10.1002/jclp.1011. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Long-term influence of duration and intensity of treatment on previously untreated individuals with alcohol use disorders. Addiction. 2003;98(3):325–327. doi: 10.1046/j.1360-0443.2003.00327.x. [DOI] [PubMed] [Google Scholar]
- Mueser KT, et al. Prevalence of substance abuse in schizophrenia: Demographic and clinical correlates. Schizophrenia Bulletin. 1990;16(1):31–56. doi: 10.1093/schbul/16.1.31. [DOI] [PubMed] [Google Scholar]
- Murray E, et al. Interactive health communication applications for people with chronic disease. Cochrane Database of Systematic Reviews. 2004;4:CD0004274. doi: 10.1002/14651858.CD004274.pub2. [DOI] [PubMed] [Google Scholar]
- Nicassio PM, Smith TW, editors. Managing Chronic Illness: A Biopsychosocial Perspective. Washington, DC: American Psychological Association; 1995. [Google Scholar]
- Office of Applied Studies. Results from the 2001 National Household Survey on Drug Abuse: Volume I. Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2002. DHHS Publication No. SMA 02–3758. [Google Scholar]
- Office of Applied Studies. Treatment Episode Data Set (TEDS): 2002. Discharges from Substance Abuse Treatment Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. DHHS Publication No. SMA04–3967. [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. Journal of Studies on Alcohol. 1998;59(5):513–522. doi: 10.15288/jsa.1998.59.513. [DOI] [PubMed] [Google Scholar]
- Parthasarathy S, et al. Utilization and cost impact of integrating substance abuse treatment and primary care. Medical Care. 2003;41(3):357–367. doi: 10.1097/01.MLR.0000053018.20700.56. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Tapert SF, Schuckit MA. Neural activation patterns of methamphetamine-dependent subjects during decision making predict relapse. Archives of General Psychiatry. 2005;62(7):761–768. doi: 10.1001/archpsyc.62.7.761. [DOI] [PubMed] [Google Scholar]
- Peterson KA, et al. Determinants of readmission following inpatient substance abuse treatment: A national study of VA programs. Medical Care. 1994;32(6):535–550. doi: 10.1097/00005650-199406000-00001. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Regier DA, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) study. Journal of the American Medical Association. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Risinger RC, et al. Neural correlates of high and craving during cocaine self-administration using BOLD fMRI. Neuroimage. 2005;26(4):1097–1108. doi: 10.1016/j.neuroimage.2005.03.030. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, et al. Psychiatric comorbidity, continuing care, and mutual help as predictors of five-year remission from substance use disorders. Journal of Studies on Alcohol. 2002;63(6):709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Moos RH, Finney JW. Relationship of treatment orientation and continuing care to remission among substance abuse patients. Psychiatric Services. 2002;53(5):595–601. doi: 10.1176/appi.ps.53.5.595. [DOI] [PubMed] [Google Scholar]
- Robins LN, Regier DA. Psychiatric Disorders in America. New York: Macmillan; 1991. [Google Scholar]
- Ross HE, Glaser FB, Germanson T. The prevalence of psychiatric disorders in patients with alcohol and other drug problems. Archives of General Psychiatry. 1988;45 (11):1023–1031. doi: 10.1001/archpsyc.1988.01800350057008. [DOI] [PubMed] [Google Scholar]
- Roter DL, et al. Effectiveness of interventions to improve patient compliance: A meta-analysis. Medical Care. 1998;36(8):1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, et al. Diagnosis and symptoms of depression in opiate addicts: Course and relationship to treatment outcome. Archives of General Psychiatry. 1982;39(2):151–156. doi: 10.1001/archpsyc.1982.04290020021004. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, et al. Prognostic significance of psychopathology in treated opiate addicts: A 2. 5-year follow-up study. Archives of General Psychiatry. 1986;43(8):739–745. doi: 10.1001/archpsyc.1986.01800080025004. [DOI] [PubMed] [Google Scholar]
- Ryan J, Louderman R, Testa M. Substance Abuse and Child Welfare: Experimenting with Recovery Coaches in Illinois. Urbana, IL: University of Illinois at Urbana-Champaign, Children and Family Research Center; 2003. [Google Scholar]
- Sannibale C, et al. Aftercare attendance and post-treatment functioning of severely substance dependent residential treatment clients. Drug and Alcohol Review. 2003;22(2):181–190. doi: 10.1080/09595230100100624. [DOI] [PubMed] [Google Scholar]
- Schlaepfer TE, et al. Decreased frontal white-matter volume in chronic substance abuse. International Journal of Neuropsychopharmacology. 2006;9(2):147–153. doi: 10.1017/S1461145705005705. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Recovery Management Checkups: An Early Re-Intervention Model. Chicago, IL: Chestnut Health Systems; 2003. [Google Scholar]
- Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug and Alcohol Dependence. 2005;78(3):325–338. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Foss MA, Dennis ML. Pathways in the relapse–treatment–recovery cycle over 3 years. Journal of Substance Abuse Treatment. 2005;28(Suppl 1):S63S72. doi: 10.1016/j.jsat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Simon GE, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: A randomized control trial. Journal of the American Medical Association. 2004;292(8):935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 2002;59(6):538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Simpson TL, et al. Telephone self-monitoring among alcohol use disorder patients in early recovery: A randomized study of feasibility and measurement reactivity. Drug and Alcohol Dependence. 2005;79(2):241–250. doi: 10.1016/j.drugalcdep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik JL. Office versus home-based family therapy for runaway, alcohol abusing adolescents: Examination of factors associated with treatment attendance. Alcoholism Treatment Quarterly. 2004;22(2):3–19. doi: 10.1300/J020v22n02_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. DHHS Publication No. SMA 06-4194. [Google Scholar]
- Taxman F. Supervision—Exploring the dimensions of effectiveness. Federal Probation. 2002;66(2):14–27. [Google Scholar]
- Toll BA, et al. What do Internet-based alcohol treatment websites offer? Cyberpsychology & Behavior. 2003;6(6):581–584. doi: 10.1089/109493103322725351. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ. The addicted human brain: Insights from imaging studies. Journal of Clinical Investigation. 2003;111(10):1444–1451. doi: 10.1172/JCI18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ. The addicted human brain viewed in the light of imaging studies: Brain circuits and treatment strategies. Neuropharmacology. 2004;47(Suppl 1):3–13. doi: 10.1016/j.neuropharm.2004.07.019. [DOI] [PubMed] [Google Scholar]
- Walker R, et al. Length of stay, neuropsychological performance, and aftercare: Influences on alcohol treatment outcome. Journal of Consulting and Clinical Psychology. 1983;51(6):900–911. doi: 10.1037//0022-006x.51.6.900. [DOI] [PubMed] [Google Scholar]
- Weisner C, et al. Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. Rockville, MD: National Institute on Drug Abuse; 2004. [Google Scholar]
- Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98(7):901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- White WL. Pathways from the Culture of Addiction to the Culture of Recovery: A Travel Guide for Addiction Professionals. 2d ed. Center City, MN: Hazelden; 1996. [Google Scholar]
- White WL, et al. It’s time to stop kicking people out of addiction treatment. Counselor. 2005;6(2):12–25. [PMC free article] [PubMed] [Google Scholar]
- White WL, Finch AJ. The recovery school movement: Its history and future. Counselor. 2006;7(2):54–57. [Google Scholar]
- Willenbring ML. Integrating care for patients with infectious, psychiatric, and substance use disorders: Concepts and approaches. AIDS. 2005;19(Suppl 3):S227–S237. doi: 10.1097/01.aids.0000192094.84624.c2. [DOI] [PubMed] [Google Scholar]
- Wisdom JP, et al. Addiction treatment agencies’ use of data: A qualitative assessment. Journal of Behavioral Health Services and Research. 2006;33(4):394–407. doi: 10.1007/s11414-006-9039-x. [DOI] [PubMed] [Google Scholar]
- Woody GE, Cottler LB, Cacciola J. Severity of dependence: Data from the DSM-IV field trials. Addiction. 1993;88(11):1573–1579. doi: 10.1111/j.1360-0443.1993.tb03144.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) Geneva, Switzerland: World Health Organization; 1999. [Google Scholar]
- Zhu S-H, et al. Telephone counseling for smoking cessation: Effects of single-session and multiple-session interventions. Journal of Consulting and Clinical Psychology. 1996;64(1):202–211. doi: 10.1037//0022-006x.64.1.202. [DOI] [PubMed] [Google Scholar]